Feature Story
Benin adopts positive new law on HIV prevention, care and elimination of stigma and discrimination
20 February 2026
20 February 2026 20 February 2026UNAIDS welcomes the passing into law by the President of Benin Patrice Talon of Law 2026-02 on 9 February 2026. The law focuses on HIV prevention and management of care and will accelerate progress towards ending AIDS in the Republic of Benin.
The new law is the culmination of a process first initiated in 2013 and which resumed in 2020 under the leadership of the Health Program for the Fight against AIDS (PSLS). This revision was made due to the significant limitations of the 2006 law, namely that it was based on a punitive, coercive and stigmatizing approach.
The previous law was incompatible with human rights standards, allowed for numerous violations of confidentiality, criminalized HIV-related behaviors and reinforced the marginalization of key populations. The law was out of step with good public health practices which should be based on prevention, inclusion and respect for human rights.
The 2026 law is now aligned with international human rights standards and more specifically reaffirms the right to non-stigma and non-discrimination. It enhances privacy and data protection, ensures access to HIV care and prevention and services and recognizes key populations including sex workers, men who have sex with men, people who inject drugs, transgender people, migrants and prisoners among others. It improves prisoners’ rights significantly and reduces criminal provisions against people living with HIV by recognizing the strictly voluntary nature of disclosing HIV status.
“The journey to validating Benin’s HIV Law was powered by strong country leadership, exceptional UNAIDS–UNDP collaboration, unwavering support from the UN Regional Coordinator, close technical follow-up with the Ministry of Health, catalytic funding from UNAIDS, UNDP and Expertise France, and close involvement of parliamentarians — turning evidence into political will and political will into transformative legislation’’ said Yayé Diallo, outgoing UNAIDS Country Director for Togo and Benin.
The progress is the result of coordinated advocacy and collaborative partnership actions at all levels involving the UNAIDS Executive Director Winnie Byanyima, who made it a priority of her visit to Benin in September 2024.
UNAIDS Regional Office, the global HIV Legal Network and UNDP provided technical support. The Global Fund and Expertise France provided financial support and the combination of the efforts of various stakeholders at the local level, namely the PSLS, the CNLS-TP(Conseil National de Lutte contre le VIH/Sida, la Tuberculose, le Paludisme, les Hépatites, les Infections Sexuellement Transmissibles et les Épidémie), the parliament and its institutions (IPaB - Institut Parlementaire du Bénin), the caucus of women parliamentarians and parliamentary committees), civil society organizations including networks of people living with HIV and key populations. With this new law and rigorous monitoring of its application, Benin is resolutely committed to its march towards the ending AIDS by 2030.
"UNAIDS, the UN Country Team, and partners including Expertise France applaud Benin’s political resolve and its new, pioneering HIV legislation. By centering the law on vulnerable groups and youth who account for 35% of new infections, Benin is taking a giant leap towards universal access to HIV treatment and the ultimate goal of ending AIDS as a public health threat by 2030." said Christian Mouala, Representative and Director of the UNAIDS Multi-Country Office for Côte d’Ivoire, Togo, and Benin.
Region/country
Related


Feature Story
Strengthening partnerships to sustain the HIV response in Eastern Europe and Central Asia
12 February 2026
12 February 2026 12 February 2026“We’re closely watching developments in both infection rates and funding in Eastern Europe and Central Asia. The challenges are great,” said Anne von Fallois, CEO of Deutsche AIDS-Stiftung (DAS), during a meeting with Eamonn Murphy, UNAIDS Regional Director, in Bonn. “We’re united on the importance of the region—especially Ukraine.”
This is a critical moment for the AIDS response in Eastern Europe and Central Asia (EECA). As global attention shifts to new crises, there is growing concern that the region—where both new HIV infections and AIDS-related deaths are still rising—could be left behind.
Since 2010, AIDS-related deaths in EECA have increased by 34%. Only about half of people living with HIV are on treatment, and viral suppression—at just 42%—is the lowest globally. More than half of new HIV diagnoses occur late, when risks of transmission and mortality are significantly higher.
War, displacement, economic hardship, and migration may be contributing to a more challenging HIV response, with potential implications beyond national borders, including the European Union. While the full impact is still emerging, these pressures could place additional demands on health systems and underscore the importance of sustained, coordinated action.
Access to services remains fragile in all countries of the region. While antiretroviral therapy is officially free in most countries, too many people are still unable to access it. Prevention coverage is even lower: opioid agonist maintenance therapy reaches only a fraction of those who need it, and pre-exposure prophylaxis remains limited. Key populations account for most new infections, yet continue to face stigma, discrimination, and legal barriers rooted in outdated policies.
“We know what works: community-led services are essential to reach people who are otherwise excluded, and partnership with communities is vital in these challenging times,” said Eamonn Murphy. “With continued UNAIDS engagement in the region, sustained, coordinated investment—alongside government commitment and community engagement—is essential to protect progress and prevent further loss of life.”
Through its partnership with UNAIDS, Deutsche AIDS-Stiftung supports HIV work in Germany and internationally, advancing stigma reduction, prevention, social support, and assistance for vulnerable groups.
As funding uncertainties grow, partners stressed the need to strengthen joint resource mobilization and encourage more active engagement from the European Union. Emergency measures can only go so far. The investments required are modest, but the stakes—for the region and for Europe as a whole—could not be higher.


Feature Story
‘I never lacked anything—except answers’ - a young man’s journey of being born with a disease he did not understand
19 January 2026
19 January 2026 19 January 2026For 24-year-old Rakhants’a Lehloibi, growing up in the rural village of Maphutseng, in Lesotho, meant navigating life with a secret he didn’t fully understand. Born with HIV, he spent his earliest years believing the antiretroviral (ARV) treatment he took daily was simply to stop frequent nosebleeds—a story his grandmother told to shield him from the stigma surrounding HIV.
“Life was tough, but my grandmother gave me all the love in the world,” he recalled. “I never felt like I lacked anything—except answers.”
Rakhants’a’s mother died when he was very young, leaving his grandmother to raise him. In 2007, when he was just 4 years old, he became severely ill. Traditional healers were consulted, but their remedies failed. It was only when he was taken to a local clinic that he was tested and diagnosed with HIV.
“Back then, I didn’t even know what HIV was,” he said. “My grandmother told me the pills I was taking were to stop nosebleeds. I believed her.”
In Lesotho—as in much of sub-Saharan Africa—stigma against people living with HIV remains widespread. Many conceal their status to avoid rejection by family and community.
“For years, I took pills but I didn’t understand why. I missed school for clinic visits. I watched my grandmother struggle just to make sure I got my medication,” Rakhants’a said. Eventually, doubting the need for treatment since his nosebleeds stopped, he began skipping doses. “I didn’t know I was putting my life at risk.”
The stigma he faced only deepened his struggle. “Kids at school whispered that I had AIDS. I felt isolated, ashamed and angry. I even thought about running away just to escape the pain. But I kept going. I passed my exams and later moved to the country’s capital Maseru to live with my sister and attend high school.”
UNAIDS country Director for Lesotho, Pepukai Chikukwa, agrees that "Though HIV stigma has reduced over the years, it is still a critical barrier to the AIDS epidemic, obstructing access to life-saving HIV prevention and treatment." Ms Chikukwa adds that it pushes people away from care and increases their risk of infection. Ms Chikukwa noted that “Addressing HIV-related stigma and discrimination requires a coordinated, multi-level, and multi-setting approach involving individuals, communities, organizations and policymakers.”
It was in Maseru that Rakhants’a’s life began to change. At Baylor Clinic, he finally learned the truth about his diagnosis and joined the Teen Club, a support network for young people living with HIV.
“For the first time, I met others like me. I realized I had been born with HIV, passed on from my late mother. That was a turning point.”
Still, the journey was not easy. Poor adherence to HIV treatment meant that Rakhants’a’s viral load was dangerously high. One health worker bluntly told him he was “as good as dead.” Placed on second-line treatment—five pills a day instead of one—he felt overwhelmed.
“At first, it was hard. But instead of giving up, I prayed every day and asked my mother to watch over me. Slowly, things changed. I gained strength, I took my medication properly, and within three months, my viral load was suppressed.”
Today, Rakhants’a uses his voice to fight stigma and inspire others. Through social media and community platforms, he spreads a message of hope and resilience.
“Being HIV positive doesn’t mean your life is over,” he said. “With proper treatment and support, we can live full, healthy lives.”
According to UNAIDS, there are 260,000 people living with HIV in Lesotho and 3200 people became newly infected with HIV in 2024. There were 6,400 children aged between 0 to 14 years, living with HIV. Nonetheless, 97% of people living with HIV know their status, of those, 97% are receiving HIV treatment and 99% of those are virally suppressed. In 2023, 11.3% of women and 18.5% of men aged 15 – 49 years old reported discriminatory attitudes toward people living with HIV.
Region/country
Related


Feature Story
UN Deputy Secretary-General reaffirms commitment to a responsible UNAIDS transition and UN commitment to the AIDS response at Board meeting
22 December 2025
22 December 2025 22 December 2025The United Nations Deputy Secretary-General, Amina Mohammed, joined the 57th meeting of the UNAIDS Programme Coordinating Board (PCB) in Brasilia, bringing a clear message: the UN will stand with governments and communities until AIDS is ended as a public health threat.
In her remarks to the Board, the Deputy Secretary-General commended the inclusive and constructive nature of the deliberations and reaffirmed that the ongoing UN80 reform process will strengthen – not diminish – the global AIDS response. She stressed that reform must be deliberate and protect what works. “There is a sense of urgency, but let me underscore here, we are not in a hurry to fail... We must achieve common ground around all the concerns that the PCB and civil society have aired over the last few weeks in particular,” she said.
Ms. Mohammed warned of growing financial pressures on countries and donors, highlighting the strain on domestic resources in low- and middle-income countries, driven by debt and the cost of debt servicing. “Governments, even if they wanted to prioritize HIV and AIDS as a budget spend, quite frankly are taking away from education, taking away from health, because they cannot meet that [cost],” she said. “Part of what we have to do today with this strategy and with the transitions that we offer in UN80 – and UNAIDS is one of them – is how to convince the international community to come back.”
The UN80 initiative aims to make the UN development system more coherent, integrated, and fit for purpose in a rapidly changing world. For UNAIDS, this means a two-phase transition that preserves its core functions and highest-value contributions to the global AIDS response – leadership and advocacy, convening and coordination, accountability and data, and community engagement.
During its meeting, the PCB adopted landmark decisions that will shape the next phase of the HIV response:
- Global AIDS Strategy 2026–2031: A bold, evidence-informed roadmap grounded in human rights, gender equality, and community leadership. The strategy will guide preparations for the 2026 UN General Assembly High-Level Meeting on AIDS and negotiations for the political declaration.
- UNAIDS and UN80 transition: The Board reaffirmed its commitment to a responsible, inclusive transition of the UNAIDS Joint Programme within the wider UN development system. A PCB Working Group will be established in early 2026 to ensure the process is orderly, transparent, and safeguards UNAIDS’ core functions.
“I have seen many across the agencies that I chair in the UN Sustainable Development Group … This is a really good one. Why? Because it has so much clarity, it has so much of a division of labour, but I think that in this particular case, what has helped it is this nature of inclusion that you have had, and demonstrated, in the PCB, with civil society having such a strong voice,” said Ms Mohammed.
The PCB meeting also featured a one-day thematic discussion on long-acting antiretrovirals, highlighting their potential to transform HIV prevention and treatment. With political will, financing, and partnerships, these innovations can dramatically reduce new infections and accelerate progress toward ending AIDS.
“Ending AIDS remains achievable,” she concluded. “But only if resources match our ambition.”



Feature Story
Multisectoral resilience to funding cuts in Guatemala
22 December 2025
22 December 2025 22 December 2025This story first appeared in the recently released World AIDS Day report 2025.
In 2025, cuts in international support for the HIV response in Guatemala and a reduced HIV allocation from the Global Fund caused immediate challenges for the HIV response. Some services were curtailed or discontinued altogether in clinics affected by the cuts, and remaining service providers struggled to absorb clients who had lost their service access. Furthermore, a substantial portion of the personnel at HIV comprehensive care units and community outreach workers that help facilitate and maintain access to services for people from key populations were also affected as their work had long been funded by external donors.
In response to these cuts in external funding, the Ministry of Health stepped in to ensure continuity of care by covering the salaries of 81 staff members, thereby sustaining the operation of numerous comprehensive care units and guaranteeing service delivery to thousands to clients across the country. This intervention was critical to maintain access to lifesaving HIV treatment and preserve the integrity of the national HIV response.
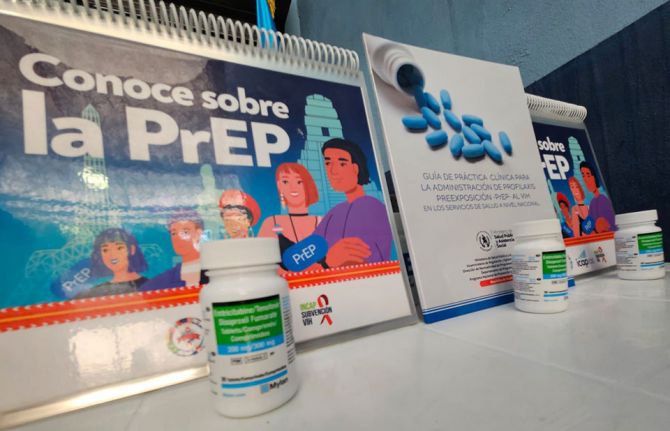
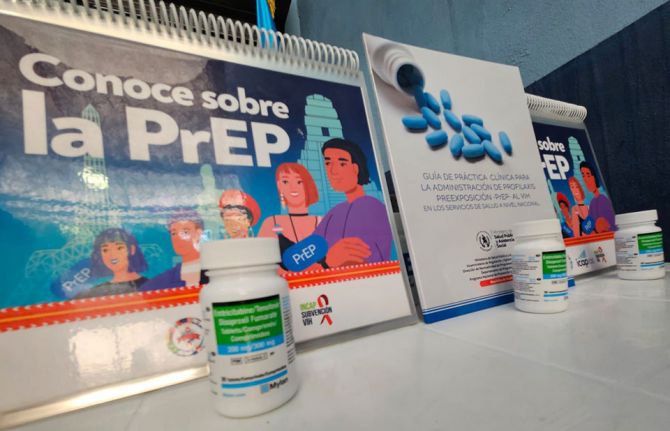
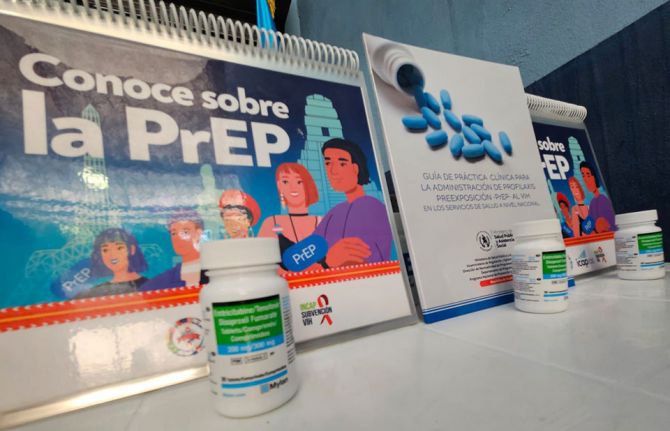
The Government also intervened to fill the gap when a key implementer and PrEP provider lost its financing. In 2025, Guatemala moved to quantify PrEP needs, develop targets for scale-up and launch access to PrEP in three departments. However, gaps persist with respect to HIV prevention programmes for people from key populations.
Community-led responses have also stepped into the breach created by the loss of international assistance. Colectivo Amigos contra el Sida (CAS), an organization focused on HIV prevention among gay men and other men who have sex with men and transgender women, moved to assume responsibility for supporting PrEP delivery to clients of a large PrEP programme that lost its funding. CAS collects voluntary donations for services from clients who can afford to pay, which helps to co-finance operational costs that are no longer covered by international donors.
Community-led responses play a critical role in the efforts to end AIDS as a public health threat. For that reason, Guatemala, with the support of UNAIDS, is working to ensure communities have access to financial and technical support. UNAIDS is collaborating with the Global Fund to help build the knowledge and capacity of civil society organizations to lobby more effectively for greater domestic resources.
Planning for the sustainability of the HIV responses is an urgent priority for many countries including Guatemala. Now that the Global Fund is set to phase out its support given Guatemala’s status as an upper-middle-income country, UNAIDS is collaborating with the Ministry of Health and the national AIDS programme to roll out the UNAIDS Rapid AIDS Financing Tool, aimed at facilitating decision-making and actions to effectively respond to the AIDS epidemic amidst a resource-limited environment.
Region/country




Feature Story
The impact of donor cuts on community-led responses in Tajikistan
08 December 2025
08 December 2025 08 December 2025Takhmina Haidarova and Pulod Jamalov are among the very few HIV activists in Tajikistan living openly with HIV. For years, they have been the public faces of courage—challenging stigma, supporting others and ensuring no one faces HIV alone. Through their organizations, the Tajikistan Network of Women Living with HIV and Spin Plus, they have built lifelines for people living with HIV and people from key populations, including people who use drugs.
Now, those lifelines are at risk of disappearing. Recent funding freezes and cuts to international HIV assistance threaten to close community-led programmes across the country. “People are panicking,” says Takhmina. “If our support services shut down, women affected by HIV, families with children living with HIV, and people from key populations will have nowhere to turn.”
Tajikistan is a small, mountainous, landlocked country in central Asia, bordered by Afghanistan, China, Kyrgyzstan and Uzbekistan. Despite economic growth, it remains the poorest country in the region, with nearly a third of its gross domestic product coming from remittances. It faces deep social and structural challenges—a fragile health system, restrictive laws, gender inequality, and powerful traditional and religious norms that fuel stigma and discrimination.
For people living with HIV, these challenges can be overwhelming. Nearly 97% of women living with HIV in Tajikistan conceal their HIV status, even from family members, and 64% report discrimination, including from health-care providers.
For Takhmina, the fight is personal. She acquired HIV from her husband, a labour migrant in the Russian Federation, and was rejected by the family after his death. “I did not even know HIV existed in Tajikistan,” she says. “I had no knowledge, no support, no one to turn to.” Now, through the Tajikistan Network of Women Living with HIV, she helps other women navigate the isolation she once faced.
“Community groups like ours are the only ones people trust,” says Pulod Jamalov, Director of Spin Plus. “We go where the system does not reach—into prisons, remote villages and migrant families. Without us, many people will simply be left behind.”
Until now, international partnerships have made real progress possible. HIV-related mortality has halved since 2020 in Tajikistan, and vertical transmission dropped to 0.8% in 2024, with only one such case recorded that year.
But this progress is fragile. About 60% of the HIV response in Tajikistan depends on international donors, of which about 20% was funded by the United States President’s Emergency Plan for AIDS Relief (PEPFAR) until January 2025. Around 37% of the national programme is now financed domestically, marking a step towards sustainability. The Government covers all costs for prevention of vertical HIV transmission, including HIV testing for pregnant women. In 2025, for the first time, the Government of Tajikistan allocated national funds to procure 10% of the country’s antiretroviral (ARV) medicines.
National authorities estimate that even a 10–20% reduction in funding could trigger a 135% increase in the number of new HIV infections and a 5% increase in mortality, erasing years of gains.
In January 2025, two major community health centres providing stigma-free care were closed, and outreach, testing and counselling stopped altogether. When these centres temporarily resumed their operations, they recorded a noticeable decline in the number of clients seeking or referred for services. Community-led monitoring, once a key accountability tool, has been completely discontinued.
Tajikistan has shown what is possible with targeted support. But unless donors, governments and international partners act quickly to protect community-led services, those gains will be reversed.
Watch: Funding cuts disrupt HIV response in Tajikistan
Region/country


Feature Story
Innovative high-level leadership to strengthen and sustain the HIV response in Uganda
16 December 2025
16 December 2025 16 December 2025This story first appeared in the recently released World AIDS Day report 2025
Across eastern and southern Africa, men and boys are less likely to test for HIV, initiate antiretroviral therapy or remain engaged in care. As a result, although HIV prevalence is higher among women and girls, the number of AIDS-related deaths is higher among men and boys in the region.
One leader recognized the challenge and decided to use his influence to create positive change. In the traditional kingdom of the Buganda people within present-day Uganda, the King, His Majesty Mutebi II, has championed health and well-being over the course of his reign, including through a series of campaigns that aim to instil healthy social norms and health-seeking behaviours. Previous campaigns have focused on promoting polio immunization, blood donation, maternal and child health and physical exercise. Buganda is home to 12 million of the 49 million people living in Uganda.
Beginning in 2016, Uganda decided to harness the influence of traditional leadership to encourage men and boys to test for HIV, and for those who test positive to start and stay on treatment. This national effort, which the King carried forward in Buganda, is premised on the conviction that social influencers such as the King are uniquely well positioned to change the attitudes and social norms of men and boys. In 2017, UNAIDS appointed the King as a UNAIDS Goodwill Ambassador on ending AIDS in eastern and southern Africa to support and highlight the King’s leadership to improve HIV outcomes among men and boys in the kingdom.
To undertake his health promotion campaigns, the King leverages his influence to obtain financial support for campaigns and to maximize their reach and effectiveness. The King has been able to attract financial support for the health campaigns from private-sector partners such as Airtel Uganda and DFCU Bank to contribute to the health campaign focused on men and boys.
The King’s HIV advocacy campaign, Abaami Munyenye (“Men are Stars”), focused on men and boys aged 15–49 years living in districts with a high HIV burden. The campaign used innovative means to generate resources and reach men and boys with key messages, including at major sporting events, such as a marathon to celebrate the King’s birthday, which attracted 50 000–60 000 participants (85% male), and the Malaza football cup, which attracted 20 000–30 000 fans. In addition to leveraging these events to reach tens of thousands of men and boys with health promotion messages, the fees paid by event participants raised funds to support health services for men and boys.
The advocacy campaign has had a clear positive impact on HIV outcomes in Buganda. From 2016 to 2020, the percentage of people living with HIV who knew their HIV status rose from 89% to 94%, HIV treatment coverage increased from 64% to 92%, and the number of new HIV infections declined by 52%.
The King’s previous health promotion campaigns typically ran for three years each, but there was consideration in 2025 to replace the HIV campaign. With donor cutbacks potentially jeopardizing national momentum towards HIV epidemic control, the King determined that now was not the time to move on from the HIV response. As a result, the campaign to improve HIV outcomes is now continuing across the kingdom.
2025 World AIDS Day report
Region/country


Feature Story
UNAIDS releases updated guidelines for conducting National AIDS Spending Assessments
14 November 2025
14 November 2025 14 November 2025UNAIDS is releasing an updated version of its guidelines for conducting National AIDS Spending Assessments (NASA). The guidelines are aimed at NASA implementers and HIV programme managers utilizing HIV expenditure data to influence budgetary, policy and programmatic decisions.
NASA is a comprehensive, systematic approach to tracking HIV expenditures and analyzing financial resources dedicated to the HIV response within a country. NASA results can identify which programmes and interventions are most underfunded and require prioritization, as well as those dependent on external sources and thus most vulnerable to external shocks. By providing this granular view, NASA data supports sustainability planning and integration into broader health financing systems, while also identifying potential inefficiencies and cost-saving opportunities, increasing evidence for allocative efficiency measures and fostering a performance-based financing culture aligned with value-for-money principles.
Importantly, the NASA approach allows for the tracking of resources being directed to, and used by, the community-led response, and for all community-based interventions. Without the detailed expenditures collected via NASA or through a similar approach, it would be difficult to monitor progress towards the global targets regarding community-leadership in the HIV response, as well as other country and global targets, including co-financing commitments.
These detailed expenditure data are critical to sustainability planning by providing an updated picture of the financial landscape which helps countries identify future trends and potential funding gaps, to inform their resource mobilization options and measure their progress towards sustainability of their HIV responses.
The NASA framework has been developed by UNAIDS in collaboration with partners and country stakeholders, evolving over more than two decades to provide a globally accepted, standardized and comparable approach to tracking the multisectoral resources invested in the HIV response. It aligns with the System of Health Accounts developed by the World Health Organization and is based on the triaxial framework of accounting (refer to figure below). NASA’s classification system allows for the detailed matching of the spending against the priorities outlined in countries’ national HIV strategic plans (NSPs) and the Global HIV Strategy. Since the late 2000s, over 80 countries have undertaken at least one NASA, with many countries undertaking assessments routinely, mostly in low and middle-income countries (LMICs). UNAIDS also offers an expanded range of resource tracking approaches to best suit country needs - including NASA-basic for resource constrained settings, requiring less time and fewer resources (typically 4–6 weeks) and NASA-plus for deeper dives into community-led response or TB tracking.
UNAIDS provides capacity building, technical tools and guidance, as well as technical support to countries for their routine expenditure data collection, analysis, and dissemination. UNAIDS also continues to support the strengthening of public expenditure systems, and HIV resource tracking within these, to improve governments’ ability to track and manage all their HIV and health-related expenditures, linking these to performance indicators, to achieve optimal outcomes with their available resources.
To promote transparency and accountability, UNAIDS and the Equitable Financing Practice synthesizes NASA and Global AIDS Monitoring (GAM) financial indicators making them publicly available and empowering stakeholders to interpret and advocate for improved resource allocation: https://hivfinancial.unaids.org/hivfinancialdashboards.html#
The findings from NASA will be instrumental in shaping the future direction of the HIV response in any given country. They will also support the broader goals of achieving universal access to HIV prevention, treatment, care and support services, and ultimately, in ending the AIDS epidemic as a public health threat by 2030.
Related resources




Feature Story
A decade of promoting workplace equality for people living with HIV in Spain
12 November 2025
12 November 2025 12 November 2025A nationwide campaign in Spain is raising awareness of the labour rights of people living with HIV, while strengthening the commitment of businesses, public administrations and civil society to combat stigma and discrimination.
Led by the non-profit association Trabajando en Positivo, the #YoTrabajoPositivo initiative is marking its tenth anniversary this year. For a decade, the initiative has travelled across Spanish cities raising awareness and advocating for the labour rights of people living with HIV, connecting companies, trade unions and institutions in this effort.
Medical advances have transformed the outlook for HIV. With timely diagnosis and proper treatment, people living with the virus can enjoy life expectancies and quality of life comparable to those of the general population. Nevertheless, stigma and discrimination remain real barriers to labour inclusion.
According to Spain’s Ministry of Health, 19% of the population report feeling uncomfortable at the idea of sharing a workplace with someone living with HIV. Similarly, the International Labour Organization’s Global Survey on HIV-related Discrimination in the World of Work (2021) revealed that a significant proportion of respondents (59.6%) supported measures that violate human rights, such as mandatory HIV testing for employment, highlighting the need to strengthen training and awareness. A further study, Experience of Stigma among People Living with HIV in Spain (Social Pact for Non-Discrimination and Equal Treatment Associated with HIV, 2024), reveals that many people with HIV still fear losing their jobs or being treated differently by colleagues if their status were known.
In this context, the initiative operates on three complementary fronts: providing evidence-based information, showcasing personal testimonies, and promoting good business practices. Together, these elements aim to dispel medical myths and transform workplace attitudes and organizational cultures.
Campaigns such as the #YoTrabajoPositivo Route play a vital role in spreading key messages that help to end stigma in workplaces including:
- HIV is not ordinarily transmitted in work environments.
- People living with HIV can perform any job with the same ability as anyone else.
- With effective treatment, people living with HIV can expect to live a normal lifespan and have full work capacity.
- There is no legal obligation to disclose HIV status in the workplace.
These messages are disseminated through public events, educational materials, and activities in public spaces, bridging the gap between scientific evidence and people's everyday experiences.
The initiative is also part of broader corporate social responsibility and equality promotion efforts in employment. Participation by companies in the Business Initiative Committed to HIV (Empresas Comprometidas con el VIH) has led to the development of internal policies that ensure HIV status does not negatively affect recruitment, retention or promotion processes. These policies also foster training and awareness among staff.
Over the past ten years, the #YoTrabajoPositivo initiative has created public spaces for dialogue on the right to work free from discrimination. It has brought scientific knowledge closer to the general public and fostered cross-sector collaboration.
Building on Spain’s commitment within the Global Partnership for Action to Eliminate All Forms of HIV-Related Stigma and Discrimination, the initiative shows how strong country leadership — combined with evidence, visibility, and collaboration — can transform attitudes and create fairer, more inclusive workplaces.
Campaign website
Region/country





Feature Story
South Africa charts a new frontier by rolling out a twice-yearly injection which is almost 100% effective in preventing HIV
24 October 2025
24 October 2025 24 October 2025South Africa has taken a decisive step towards stopping new HIV infections. The South African National AIDS Council (SANAC) and the National Department of Health, in collaboration with UNAIDS, convened a two-day national meeting on access to a new, and potentially groundbreaking medicine (lenacapavir) which is set to be rolled out in South Africa in early 2026.
Minister of Health Dr Aaron Motsoaledi affirmed government’s commitment to make lenacapavir “a public good - accessible, affordable and locally produced”. He emphasised the importance of prioritising adolescent girls and young women. There are around 8 million people living with HIV in South Africa and every week around 1000 adolescent girls and young women become newly infected with HIV.
“The introduction of lenacapavir marks the beginning of a new phase in HIV prevention, one grounded in collaboration between government, communities, our partners like the Global Fund and UNAIDS and the private sector,” said Dr Motsoaledi. “This partnership must be accountable, transparent and inclusive if we are to achieve our national targets.”
South Africa is among nine countries globally selected to roll out the medicine under the Global Fund to Fight AIDS, TB and Malaria’s financial commitment to reach 2 million people across low- and middle-income countries.
“Science continues to offer us new tools, but innovation alone is not enough,” said Eva Kiwango, UNAIDS Country Director for South Africa. “Equity must follow. Communities, especially young women and key populations, have waited too long for HIV prevention they can trust and use with dignity.”
Through a US$ 29 million grant, South Africa will receive enough medicine to provide HIV prevention to 450 000 people at high risk of HIV during a rollout in 23 high-incidence districts across six provinces. The aim is to reach adolescent girls, young women, sex workers, men who have sex with men, people who use drugs and other at risk populations.
“We are not gathered merely to discuss a medicine, but to reaffirm our collective commitment to justice and equality,” said Steve Letsike, Deputy Minister for Women, Youth and People living with Disabilities. “No young woman, no queer person, no person with a disability must be left behind in the promise of HIV prevention.”
Across both days, a common message resonated: partnership is South Africa’s greatest strength. Dr Thembisile Xulu, SANAC CEO, called for unity of purpose noting, “We must move from conversation to coordination, and from coordination to action.”
Yvette Raphael, Co-founder of the Advocacy for Prevention of HIV and AIDS in South Africa emphasised the need to take the message to communities, saying, “Civil society must be given the tools for demand creation to provide research literacy in the way that we and communities understand.”
The evidence and the promise
Presenting findings from the PURPOSE 1 and 2 trials, Professor Linda-Gail Bekker, CEO of the Desmond Tutu Health Foundation reported 100 % efficacy among cisgender women and 96% efficacy among men, transgender and non-binary participants. She highlighted that long-acting prevention tools such as lenacapavir expand choice, strengthen agency, and promote equity, offering new hope to those who need discreet and durable protection.
Professor Helen Rees, from WITS RHI, emphasised the issue of misinformation and disinformation as South Africa prepares to roll out lenacapavir next year. She said that all stakeholders, “Must underscore the importance of science because if there is mistrust in science, people will not trust new products. As we roll out lenacapavir we must have our ears on the ground for misinformation and disinformation.”
Gilead Sciences, developer of lenacapavir, represented by Country Manager, Wendy Cupido affirmed its commitment to ongoing dialogue and partnership with the Government of South Africa and stakeholders to ensure affordable, equitable access. She noted that the manufacturer of lenacapavir Gilead remains ready to engage with the country and partners as they explore local manufacturing readiness.
Speaking during a panel discussion, young Shout Out Now ambassador, Lerato explained the impact of missing one day of oral PrEP means putting yourself at risk of acquiring HIV. She said, “I am looking forward to lenacapavir to reduce my monthly visits to the clinic to access medication and all the relevant screenings to keep myself safe from HIV. It will make my life easier.”
Dr Yogan Pillay, Director HIV and TB delivery at the Gates Foundation underlined how collaboration is transforming affordability. Recent landmark agreements secured by Unitaid, CHAI, Wits RHI and Gates will make generic lenacapavir available at a cost of US$ 40 a year in 120 low- and middle-income countries starting in 2027. “Sustainability isn’t imported -it’s built,” he said, noting the importance of local manufacturing and data-driven delivery.
The meeting entitled Lenacapavir Access and Sustainability was held in Johannesburg on 14 and 15 October, 2025. Over 100 participants participated in person and 130 joined virtually. The consultation marked the launch of the rollout of Lenacapavir in South Africa which is set to start in 2026.
Region/country
Related
 Multisectoral resilience to funding cuts in Guatemala
Multisectoral resilience to funding cuts in Guatemala
22 December 2025
 Lower prices needed for new HIV prevention medicine in Brazil
Lower prices needed for new HIV prevention medicine in Brazil

09 September 2025