



Feature Story
First-ever Jamaica transgender strategy looks beyond health
08 January 2021
08 January 2021 08 January 2021Imagine using a health-care system that has no concept of you as a person, or of your unique needs. Nurses might not ask important questions. Doctors might overlook the solutions you really require. You might feel unwelcome.
That has always been the reality for transgender people in Jamaica. A new strategy seeks to change this.
With support from UNAIDS and the United Nations Population Fund (UNFPA), TransWave Jamaica has launched the Trans and Gender Non-Conforming National Health Strategy, the first of its kind in the English-speaking Caribbean. The five-year plan is a rights-based road map for how the health and well-being of transgender people can be advanced. It moves beyond recommendations for the health-care system to the structural and societal changes necessary to achieve equitable access to services and opportunities for the transgender community.
“Too many transgender people stay home and suffer or change who they are to access public health-care spaces,” explained TransWave Associate Director of Policy and Advocacy, Renae Green. “We need improvement to basic services, including psychosocial support. And we need transgender people to be able to access public health services as their authentic selves.”
Through the Unified Budget, Results and Accountability Framework Country Envelope for Jamaica, UNAIDS collaborated with UNFPA to support a robust year-long process of research, community engagement and strategy development, including a monitoring and evaluation framework. The strategy development process was informed by a multisectorial steering committee composed of civil society organizations, international cooperation partners and government authorities.
HIV is a major priority for the Jamaica transgender community. Around 50% of transgender women participants in two recent studies were living with HIV. But there are other pressing concerns. Two surveys found that around half of transgender respondents were unemployed. One third skip meals. One in ten sells sex to survive. Research conducted in 2020 by TransWave found that half of respondents had been physically assaulted in the past year, with 20% reporting sexual assault. More than 80% had been verbally abused.
“The needs go beyond HIV and health care. Other factors affect people’s ability to be safe, to be adherent or to remain HIV-negative. We should take into account the whole person, not just a part,” said Denise Chevannes-Vogel, HIV and AIDS Officer for the UNFPA Sub-Regional Office for the Caribbean.
“We value the fact that we were able to bring together the community to have a discussion about their needs beyond HIV,” said Ms Green.
The TransWave team led the community needs assessment. Some community requests, such as hormone replacement therapy or gender assignment surgery, are unique. But others are common to all people. They want access to health care and housing, education and employment. And they want to see themselves represented in the civil society spaces where many access care and support.
“We will not reach any AIDS-related targets if we do not prioritize transgender health as a whole. People are dying because of violence, living on the streets, lack of jobs and lack of opportunities. Even the HIV prevention knowledge that most people would acquire through formal education settings is not available to transgender people when they are bullied and forced to drop out. So this process was about reflecting on the impact indicators. What would it take for them to live longer, better lives?” said Ruben Pages, UNAIDS Jamaica’s Community Mobilization Adviser.
But what chance does this comprehensive and forward-thinking strategy have of succeeding in a country famed for its social conservatism? The partners are optimistic. On one hand, the approach calls for longer-term goals, including law reform around issues such as gender identity recognition and decriminalizing sex between same-sex partners. But the strategy is also a practical guide for transgender inclusion in systems and frameworks that are already in place. With targeted action there can be quick wins.
Manoela Manova, the UNAIDS Country Director for Jamaica, said the strategy will help the country accelerate progress to end AIDS.
“Going forward, there will be renewed focus on ensuring that excellent prevention, testing and treatment outcomes are achieved across all communities, especially key and vulnerable populations,” Ms Manova said. “This is an opportunity to make good on our commitment to leave no one behind.”
Our work
Region/country
Related




Feature Story
Navigating Lesotho’s legal system to address gender-based violence
08 March 2021
08 March 2021 08 March 2021When Lineo Tsikoane gave birth to her daughter, she was inspired to intensify her advocacy for gender equality to give Nairasha a better life as a girl growing up in Lesotho.
“I think a big light went off in my head to say, “What if the world that I’m going to leave will not be as pure as I imagine?” I ask myself, “What kind of world do I want to leave my daughter in?”” she says.
As a result, Ms Tsikoane champions for women’s social, economic and legal empowerment at her firm, Nairasha Legal Support. It offers legal support for women in small and medium enterprises and women who are survivors of sexual and gender-based violence.
“Our main focus is gender-based violence, because this happens to be a country that has one of the highest incidences of rape and intimate partner crime in the world,” she says.
Even before the COVID-19 outbreak, violence against women and girls had reached epidemic proportions globally.
According to UN Women, 243 million women and girls worldwide were abused by an intimate partner in the past year. In Lesotho, it is one in three women and girls.
Less than 40% of women who experience violence report it or seek help.
As countries implemented lockdown measures to stop the spread of the coronavirus, violence against women, especially domestic violence, intensified—in some countries, calls to helplines increased fivefold.
In others, formal reports of domestic violence have decreased as survivors find it harder to seek help and access support through the regular channels. School closures and economic strains left women and girls poorer, out of school and out of jobs, and more vulnerable to exploitation, abuse, forced marriage and harassment.
The United Nations Population Fund (UNFPA) works together with UNAIDS, the United Nations Children’s Fund and the World Health Organization on 2gether4SRHR, a joint programme funded by the Swedish International Development Cooperation Agency, to address HIV and sexual and reproductive health in Lesotho.
During Lesotho’s lockdowns, UNFPA worked with Gender Links, the Lesotho Mobile Police Service and others to support efforts to prevent and respond to incidences of gender-based violence.
“We are ensuring that a helpline, where people experiencing gender-based violence can call, is in place and is working and we are also providing relevant information through various platforms for people to access all the information they need on gender-based violence,” says Manthabeleng Mabetha, the UNFPA Country Director for Lesotho.
Mantau Kolisang, a local policeman from Quthing, Lesotho’s southernmost district, characterized by rolling hills and vast landscapes, says one reason why gender-based violence is prevalent in Lesotho is because the law is not heeded in the rural areas.
“It’s difficult to implement the law since these are remote areas,” he says, adding that while he has made arrests, he has no transport to access far-flung areas in the small mountainous region.
Lesotho’s law states that a girl can marry at the age of 16 years. However, Mr Kolisang says cultural practices, coupled with contraventions of the law, has made some men believe a 13-year-old girl “can be a wife”, exposing Basotho girls to violence.
“Men don’t regard it as a crime,” he says, adding that girls have been abducted from the mountains for forced marriages.
Between 2013 and 2019, 35% of adolescent girls and young women in sub-Saharan Africa were married before the age of 18 years. Girls married before 18 years of age are more likely to experience intimate partner violence than those married after the age of 18.
Because of poverty, gender inequality, harmful practices (such as child, early or forced marriage), poor infrastructure and gender-based violence, girls are denied access to education, one of the strongest predictors of good health and well-being in women and their children.
In Lesotho’s legal system, women are regarded as perpetual minors. This categorization infantilizes women, Ms Tsikoane says. A man who abuses a woman can often walk away unscathed from the justice system if he says the woman in question is his “wife”, she adds.
“This makes women vulnerable to commodification because a child can be passed around,” she says.
Ms Tsikoane says there is a direct link between the minority status of women and HIV infection in Lesotho. In 2019, there were 190 000 women 15 years and older living with HIV in Lesotho, compared to 130 000 men.
Adolescent girls and young women between the ages of 15 and 24 years are particularly vulnerable. They accounted for a quarter of the 11 000 new HIV infections in Lesotho in 2019.
“My hypothesis is women cannot negotiate safe sex,” says Ms Tsikoane.
The dangerous reality that Basotho women live in worries Mr Kolisang. But due to a lack of institutional support and resources, he feels his actions have limited effect.
“I feel for these children. I feel for these women. I do feel for them. I can help, but the problem is how?” he laments.
Ms Tsikoane says she finds “trinkets of opportunities” for her and her colleagues to help their clients and navigate a legal system that is not favourable towards women.
“So, if you are not being well assisted at a police station, if you feel like someone is dragging your case and you are struggling to get an audience, we are there. We will support you and we will fight with you,” she says.
Our work
Region/country

Feature Story
Targeting sex workers is not the answer
08 June 2020
08 June 2020 08 June 2020When the Government of Cameroon ordered everyone to stay at home as part of the COVID-19 response, Marie-Jeanne Oumarou (not her real name) rushed to buy groceries and to gather her three children and move them the countryside.
With her children in safe hands, she hoped she could still work.
“I didn’t realize how hard it would be during confinement,” she said. “It doesn’t make sense for us sex workers.”
Ms Oumarou has learned the ins and outs of the couloirs—the avenues of small hotels where sex workers work—in Cameroon’s capital city, Yaoundé, over the past 10 years. Abandoned with her young children, she became a sex worker in 2010. She has grown to know the various older women, former sex workers themselves, who she pays to access safe places to work. COVID-19 changed her life overnight, though.
“Hotels closed, clients were rare, the police constantly around, I cannot survive,” she said.
Denise Ngatchou, Executive Director of Horizons Femmes, a nongovernmental organization that helps vulnerable women, said she was shocked to see how sex workers suddenly became a target.
“Police arrested and held women, disclosing zero information,” she said. “We felt powerless because the government had the upper hand with all the COVID-19 measures.”
Rosalie Pasma, a manager at one of the Horizons Femmes drop-in health centres, shrugged her shoulders in agreement during a Skype interview.
“Everything became much more complicated during COVID-19,” she said. “From women missing health check-ups because of transport issues to our legal expert not being able to access the police stations to defend arrested female sex workers, we felt the confinement in more ways than one.”
Ms Ngatchou piped in, saying that there was no reason to give up. Horizons Femmes vowed to stay open. A skeletal staff with condensed hours still provided HIV testing and other services by respecting preventive measures.
“People told us to stop all our on-the-ground awareness visits, but we held on as long as we could, giving coronavirus tips to women so they knew of the potential dangers,” she said.
They also kept handing out masks and started a crowdfunding project to purchase more protective gear. What really bothers Ms Ngatchou is how so many things happened before their eyes and they could do so little.
“Easing laws against sex work and ending arbitrary arrests of sex workers would really make an impact,” she said.
In the end, she believes that chastising sex workers only worsens the situation.
“Don’t you think that if sex workers hide they are more likely to work and infect themselves or become infected than if there was an infrastructure to help them?” she asked.
Reflecting on what she said, she added that this applies to COVID-19 as well as HIV.
In early April, UNAIDS and the Global Network of Sex Work Projects sounded the alarm on the particular hardships and concerns facing sex workers globally. They called for countries to ensure the respect, protection and fulfilment of sex workers’ human rights.
“Authorities have got to understand that we are not promoting sex work, we are promoting good health,” Ms Ngatchou said. “That’s the priority.”
Our work
Region/country
Related

Update
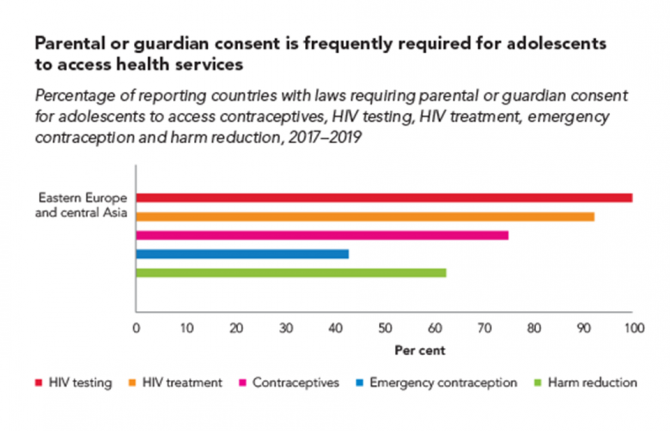
Parental consent undermines the right to health of adolescents
16 March 2020
16 March 2020 16 March 2020Many countries have laws or policies that prevent adolescents from accessing essential health services without the consent of a parent or guardian. The original intention may have been to protect minors, but these stipulations often have the opposite effect and increase the risk of HIV and other health problems among adolescents.
A large proportion of countries across all regions restrict access to HIV testing and treatment for adolescents. In 2019, for instance, adolescents younger than 18 years needed explicit parental consent in 105 of 142 countries in order to take an HIV test. In 86 of 138 reporting countries, they needed such consent to access HIV treatment and care. These kinds of laws and policies also may complicate or hinder adolescent access to pre-exposure prophylaxis (PrEP), a highly effective prevention tool.
Research in sub-Saharan Africa shows that in countries where the age of consent is 15 years or lower, adolescents are 74% more likely to have been tested for HIV in the past 12 months compared with countries where the age of consent is 16 years or higher—with girls especially benefiting from the easier access.
Country-level details on which countries have consent laws can be viewed on the UNAIDS Laws and Policies Analytics web page.
Resources

Update
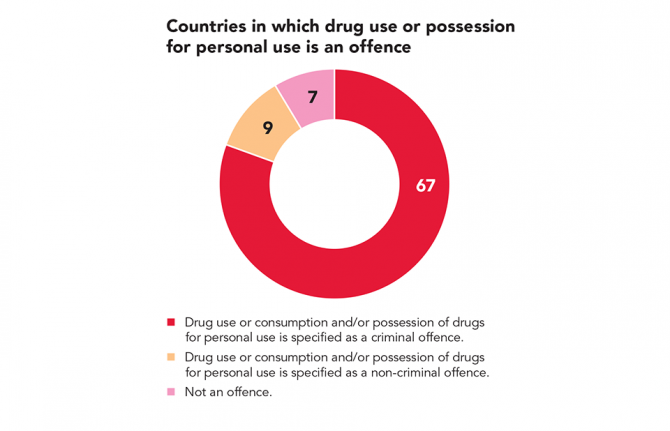
Decriminalization works, but too few countries are taking the bold step
03 March 2020
03 March 2020 03 March 2020With the United Nations Commission on Narcotic Drugs meeting this week in Vienna, Austria, diplomatic attention is once again being given to drugs. In 2018, people who inject drugs accounted for 12% of worldwide new HIV infections.
Laws that criminalize key populations or discriminate against people living with HIV undermine efforts to prevent new HIV infections and AIDS-related deaths in dozens of countries across all regions. Decriminalization of drug use and possession for personal use reduces the stigma and discrimination that hampers access to health care, harm reduction and legal services. In countries where drug use is decriminalized and comprehensive harm reduction is available, HIV prevalence and transmission tend to drop sharply among people who use drugs.
Czechia, the Netherlands, Portugal and Switzerland are among a handful of countries that have decriminalized drug use and possession for personal use and that have also invested in harm reduction programmes. Consequently, diagnoses among people who inject drugs in those countries are low.
With drug use or consumption and/or possession of drugs for personal use a criminal offence in at least 67 countries, it’s time for countries to take the bold step towards decriminalization.
Related information
Related


Feature Story
“We carry on”
28 February 2020
28 February 2020 28 February 2020“For five years I have been subjected to harassment and threats—rape threats, murder threats, vilification, character assassination, phone calls to my family, to my mom,” said Lebanese television anchor Dima Sadek.
To raise public awareness about sexual harassment and bullying in Lebanon, particularly against female journalists during the recent protests, the Arab Foundation for Freedoms and Equality—UNAIDS’ regional partner on rights and health—has produced a video that sheds light on this human rights abuse committed against many women in the country.
Made in partnership with the HIVOS Women Empowered for Leadership (WE4L) programme, with funding from the Dutch Ministry of Foreign Affairs, the video highlights cases of harassment and assault—reporters whose bodily autonomy has been violated, whose personal telephone numbers have been leaked and who subsequently received rape threats and pornography and who have been verbally and physically attacked while live on television.
“You don’t expect that someone could be this hurtful or that they could say such things. You don’t know them and they don’t know you, but because you differ on politics, they feel they are allowed to talk to you in this way,” said Layal Saad, a reporter.
Since similar attacks, including online bullying and harassment both online and offline, have also been reported by female protesters, the video also seeks to raise awareness about the everyday sexual harassment, bullying and violence that women in general are subjected to, emphasizing the need for policies that allow women to become leaders.
Diana Moukalled, a journalist, explained that legal protection against sexual harassment is needed, since at present there are no laws that criminalize sexual harassment in Lebanon. “Lebanese women are among the most politically marginalized in the world, not just in the region. We see women present on many levels, yet there is a sharp discrepancy between the role of Lebanese women and their representation,” she said.
The video’s title is We Carry On, echoing the sentiment of the many women who watched and reacted to it—a feeling of resilience in the face of adversity and a determination to achieve the social justice demanded by women in Lebanon.
Region/country


Feature Story
United Republic of Tanzania lowers age of consent for HIV testing
29 November 2019
29 November 2019 29 November 2019The United Republic of Tanzania has approved a change to the law that lowers the age of consent for HIV testing from 18 years to 15 years. The amendment to legislation also makes self-testing for HIV legal, also from the age of 15 years.
“These amendments will significantly accelerate our intention to meet the 90–90–90 goals, which aim at ending the AIDS epidemic by 2030,” said Ummy Mwalimu, Minister of Health, Community Development, Gender, Elderly and Children. The ministry was instrumental in tabling the amendments to the legislation.
The 90–90–90 targets are ambitious treatment targets to help end the AIDS epidemic. They aim to ensure that, by 2020, 90% of all people living with HIV will know their HIV status, 90% of all people who know their HIV status will be on antiretroviral therapy and 90% of all people on antiretroviral therapy will be virally suppressed.
The changes to the law will contribute to improved access to HIV testing for adults aged 15 years and over.
At the end of 2018, the progress on the 90–90–90 targets in the United Republic of Tanzania was 78–92–87. In 2018, there were 72 000 new HIV infections in the country. While this is a 13% reduction from 2010, it is below the 28% reduction across eastern and southern Africa.
“I congratulate the Government of the United Republic of Tanzania on its leadership and high-level political commitment to the AIDS response. UNAIDS will continue to work hand-in-hand with all our partners to ensure that access to HIV testing and treatment continues to expand,” said Leo Zekeng, UNAIDS Country Director in the United Republic of Tanzania.
Region/country
Related


Update
Criminalization of same-sex sexual relationships decreasing
07 October 2019
07 October 2019 07 October 2019Fifty years after the Stonewall riots in New York, United States of America―a major milestone in the modern struggle to recognize the human rights of lesbian, gay, bisexual, transgender and intersex people―more people are benefiting from the rights that the Stonewall protesters campaigned for. The number of people living in countries that criminalize consensual same-sex sexual relationships has steadily declined since 1969.
In June 2019, Botswana became the latest country to decriminalize same-sex relationships, but Africa still accounts for about half of the world’s population living in countries with anti-homosexuality laws. In 2018, the proportion of the world’s population that lives in countries that criminalize same-sex sexual relations plummeted from about 40% to 23% following the Indian Supreme Court’s decision that decriminalized all consensual sex among adults. This was the largest annual decline since China decriminalized same-sex sexual relationships in 1997.
Prohibitive laws and policies against key populations increase their vulnerability to HIV. It is therefore vital to ensure the full respect of the human rights of all people, regardless of their sexual orientation and gender identity, including through repealing laws that prohibit sex between consenting adults in private, enforcing laws to protect people from violence and discrimination and addressing homophobia and transphobia.
Consensual same-sex sexual relations remain criminalized in at least 67 countries and territories worldwide.
Related information


Feature Story
Mapping HIV laws and policies
31 July 2019
31 July 2019 31 July 2019A new website that enables people to identify national laws and policies related to the AIDS response has been launched by UNAIDS.
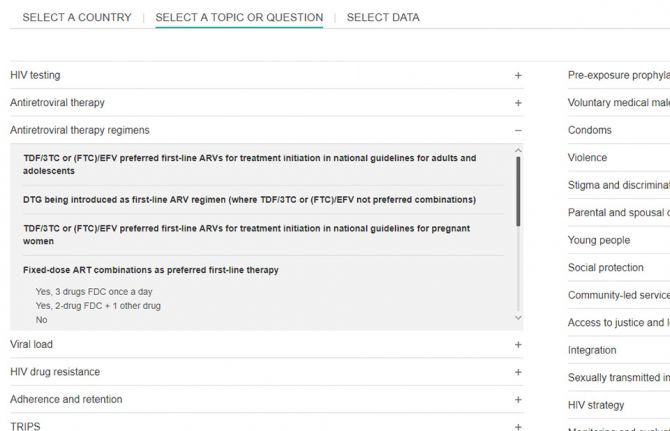
Covering areas as diverse as a country’s ability to diagnose HIV among young babies, the existence of laws that discriminate against transgender people and whether people are prosecuted for carrying condoms, the Laws and Policies Analytics website aims to give a full overview of a country’s laws and policies related to the HIV response. It also allows to view policy data jointly with other data on the HIV epidemic and response.
“We must better understand legal and policy environments to drive effective responses to the HIV epidemic. This new tool will provide access to data on national laws and policies and allow for joint analysis with data on the epidemic and response, so that we can drive more deeply-informed decision-making,” said Shannon Hader, UNAIDS Deputy Executive Director, Programme.
Under the 2016 United Nations Political Declaration on HIV and AIDS, countries committed to accelerate efforts to significantly increase the availability of high-quality data on HIV. The information used on the new website was reported since 2017 and most recently in 2019 through the National Commitments and Policy Instrument (NCPI), a part of the Global AIDS Monitoring mechanism through which countries report their progress against the commitments they made in the 2016 Political Declaration.
Data were provided by national authorities, civil society organizations and other nongovernmental partners engaged in the AIDS response. Data on HIV-related laws and policies compiled from other external official documents complement the nationally supplied data. UNAIDS carries out a thorough validation of all policy data included to ensure their accuracy. Data will be updated annually.
The website hosts data from over 140 countries. Users can search by country or region through an interactive map or can select a specific topic.
Through making policy data widely available, UNAIDS seeks to promote transparency and an increased use of policy data in analyses of the HIV epidemic and the response to HIV in countries worldwide.
The Laws and Policies Analytics website can be accessed at lawsandpolicies.unaids.org.


















