Tuberculosis (TB) is caused by bacteria called Mycobacterium tuberculosis. TB infection occurs when a person breathes in droplets produced when someone with active TB disease coughs or sneezes. These droplets can remain infectious in the air for several hours in damp enclosed spaces with little ventilation or direct sunlight, such as overcrowded informal housing or prisons. TB infection does not always result in active TB disease; most healthy people are able to kill or contain the TB bacteria. A person who has TB infection, but no disease, cannot transmit TB. Only someone with active TB of the lung is infectious. Overall, a relatively small proportion (5–15%) of the estimated 2–3 billion people infected with TB will actually develop TB disease during their lifetime. However, if a person’s immune system becomes weakened, the TB bacteria are much more likely to multiply, spread and cause active disease. TB disease typically affects the lungs (pulmonary TB), but can also affect any other part of the body (extrapulmonary TB). HIV infection is the strongest risk factor for TB infection progressing to TB disease. Other risk factors include malnutrition, diabetes, drug use, excessive alcohol use, silicosis, cancer or cancer treatment and old age.
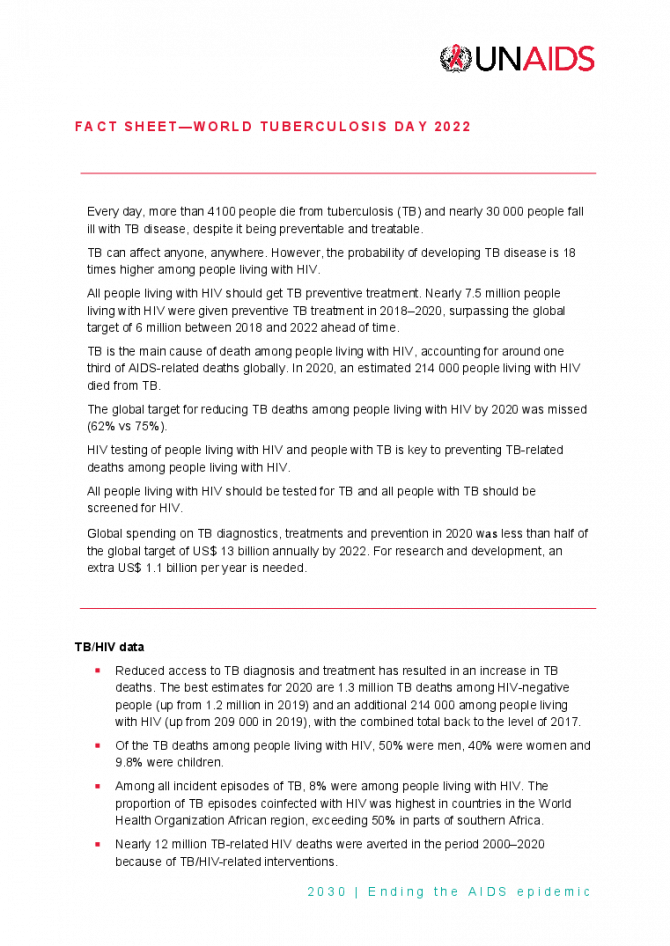
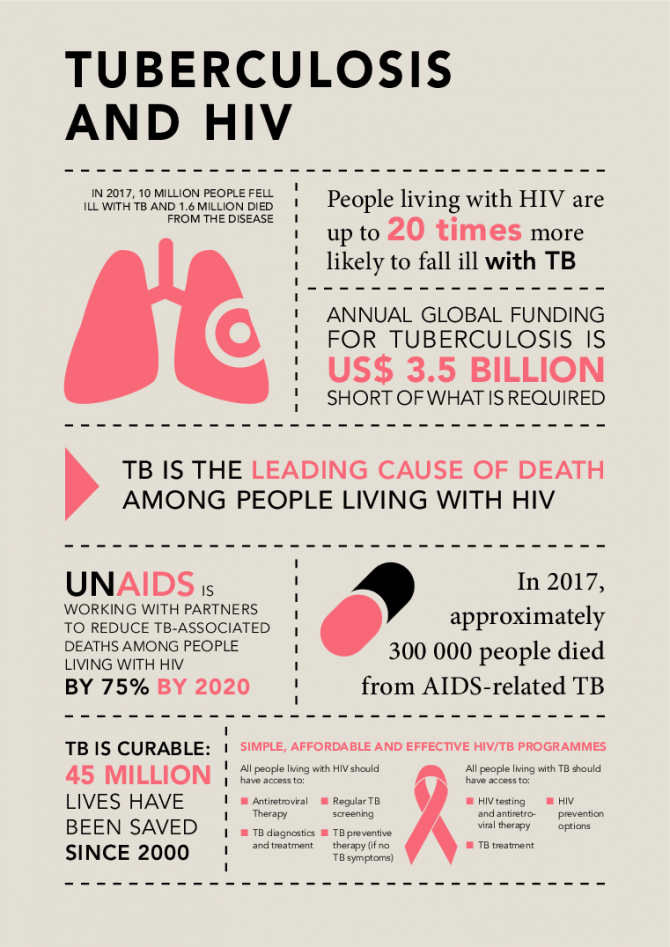
TB is the leading cause of death among people living with HIV, causing more than one third of all AIDS-related deaths in 2015. Almost 60% of the estimated global HIV-related TB cases are not diagnosed and not treated.
New molecular diagnostic tests for TB are increasingly available, which are faster and more accurate than the traditional microscopy tests. They can also detect drug-resistant forms of TB. The lipoarabinomannan (LAM) urine dipstick test can help diagnose TB among people living with HIV with advanced HIV disease (CD4 count <100 cells/mm3). Despite these advances, TB can remain difficult to diagnose in people living with HIV and in children. Clinical algorithms, including X-rays, can be used to determine when presumptive TB treatment is indicated in the absence of a positive TB test.
Without treatment TB is rapidly fatal in a person living with HIV. Treatment of drug-sensitive TB is six months of daily treatment with four antibiotics. It is well-tolerated, effective, relatively low cost (about US$ 100–1000 total cost, depending on the country) and can be safely combined with antiretroviral therapy.
Drug-resistant TB treatment is more complicated and expensive, requiring three to six second-line anti-tuberculous medicines for up to two years, often including painful daily injections. The outcome of treatment is worse than for drug-sensitive disease, owing to side-effects, including permanent hearing loss, and interactions between medicines. People living with HIV are twice as likely to die during TB treatment compared with TB patients who are HIV-negative.
UNAIDS advocates at the global regional and national levels for countries to achieve the 2016 United Nations Political Declaration on Ending AIDS commitment of reducing TB-related deaths among people living with HIV by 75% by 2020 (compared to a baseline of 2010). This is achieved by resource mobilization, technical assistance and ensuring that TB and HIV programmes work closely together to prevent, find and effectively treat HIV and TB.
“The world has made defeating AIDS a top priority. This is a blessing. But TB remains ignored. We can't fight AIDS unless we do much more to fight TB as well”
Nelson Mandela, former President of South Africa