
Update
90–90–90: good progress, but the world is off-track for hitting the 2020 targets
21 September 2020
21 September 2020 21 September 2020In 2016, the United Nations General Assembly’s Political Declaration on Ending AIDS committed countries to the 90–90–90 targets, which aim to bring HIV testing and treatment to the vast majority of people living with HIV by the end of 2020 and to reduce the amount of HIV in their bodies to undetectable levels, so they keep healthy and to prevent the further spread of the virus.
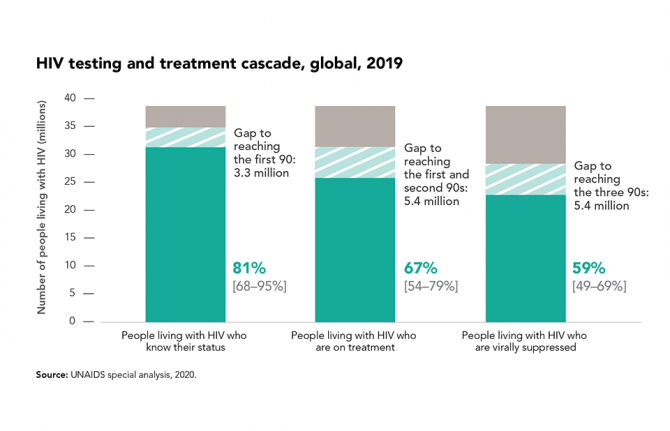
Globally, there have been remarkable gains across the HIV testing and treatment cascade. At the end of 2019, 81% of people living with HIV knew their HIV status, and more than two thirds (67%) were on antiretroviral therapy, equal to an estimated 25.4 million of the 38.0 million people living with HIV—a number that has more than tripled since 2010.
Gains in treatment effectiveness, as well as increases in the number of people who know their status and are on treatment, are reflected in the fact that viral load suppression levels among all people living with HIV increased by 18 percentage points between 2015 and 2019. Almost 59% of people living with HIV globally had suppressed viral loads in 2019. However, achieving the 90–90–90 targets results in a minimum of 73% of people living with HIV having suppressed viral loads, so the global target for the end of 2020 is unlikely to be met.
The COVID-19 pandemic also could have an impact on viral load. Early modelling showed that a severe disruption in HIV treatment could result in additional AIDS-related deaths in sub-Saharan Africa. Some countries have reported reductions in medicine collections of up to 20% in some areas and there have been multiple reports of people living with HIV not having enough antiretroviral medicine for a lockdown of more than 60 days, as well as reports of people having abandoned their HIV treatment due to a lack of food. However, monthly data from January to June 2020 reported by countries to UNAIDS have not shown substantial declines in the numbers of people currently on treatment over the six-month period.
Related


Update
How are babies becoming infected with HIV in Africa?
11 February 2020
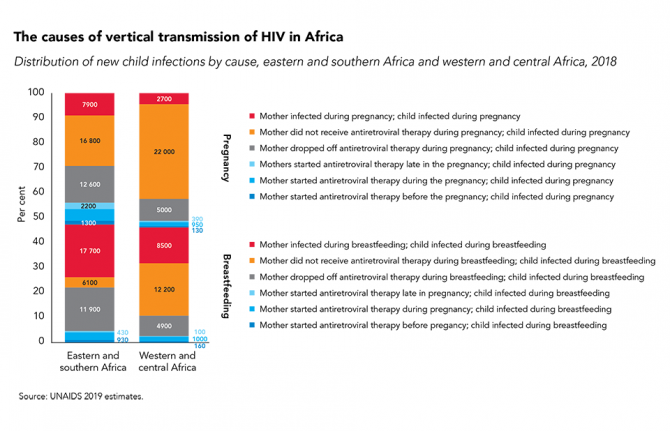
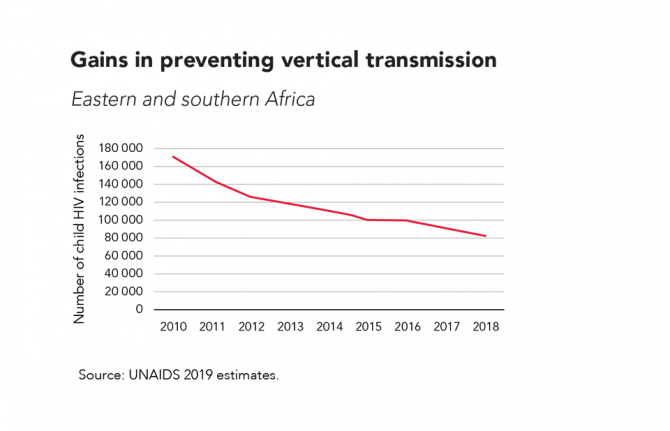
11 February 2020 11 February 2020In Africa, where a pregnant woman living with HIV lives has a big influence on whether her baby will be born HIV-free, and, if not, how her infant will acquire HIV.
There are a many reasons for vertical (mother-to-child) transmission of HIV, including: women not receiving antenatal and prevention of vertical HIV transmission services during pregnancy or breastfeeding; women starting antiretroviral therapy but falling out of care during pregnancy or breastfeeding; and women becoming infected with HIV during breastfeeding or pregnancy. However, not all countries face the same challenges, and to make rapid progress in eliminating vertical transmission it is crucial to know which means of transmission is contributing to the most new HIV infections among children in a country or region.
While the causes of vertical transmission of HIV in different regions vary, one thing is sure: far too many babies are still becoming infected with HIV.
Related

Update
Violence faced by key populations
27 January 2020
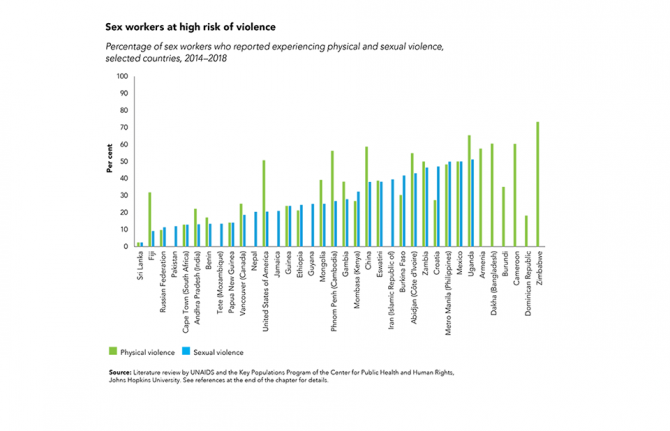
27 January 2020 27 January 2020Gains have been made against HIV-related stigma and discrimination, but discriminatory attitudes remain extremely high in far too many countries. Discrimination can manifest in criminal laws that give license to discrimination, aggressive law enforcement, harassment and violence, pushing key populations to the margins of society and denying them access to basic health and social services, including HIV services.
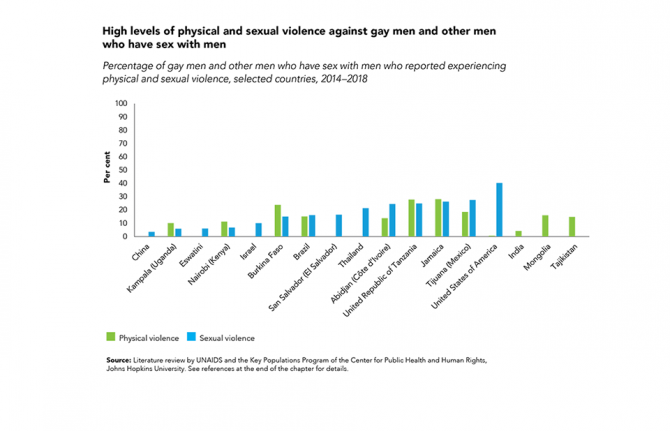
Surveys and studies across regions show that large percentages of key populations are victims of physical and sexual violence: among 36 countries with recently available data, more than half of sex workers in eight countries reported experiencing physical violence, and in two countries, at least half reported experiencing sexual violence.
In four of 17 countries with recently available data, more than one in five gay men and other men who have sex with men reported experiencing sexual violence.
Related information


Update
Young people and men less likely to know their HIV status
17 December 2019
17 December 2019 17 December 2019It is vital that people living with HIV know their HIV status. If people know they are HIV-positive, they can access treatment to keep themselves heathy. And when their treatment has reduced their viral load to an undetectable level, they can’t pass on the virus to their sexual partners. However, there are often large disparities in knowledge of HIV status, both geographically and by subpopulation.
In eastern and southern Africa, for example, young people and men living with HIV are much less likely to be aware of their status: while 90% of women living with HIV aged 25 years and above knew their status in 2018 (thanks in large part to the success of efforts to prevent mother-to-child transmission of HIV), that was the case among only 80% of men of the same age, 66% of young women (aged 15–24 years) and 50% of young men (aged 15–24 years). In western and central Africa, the gaps are even larger.
Resources
Related
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025

Update
Barriers to PrEP must be removed
09 December 2019
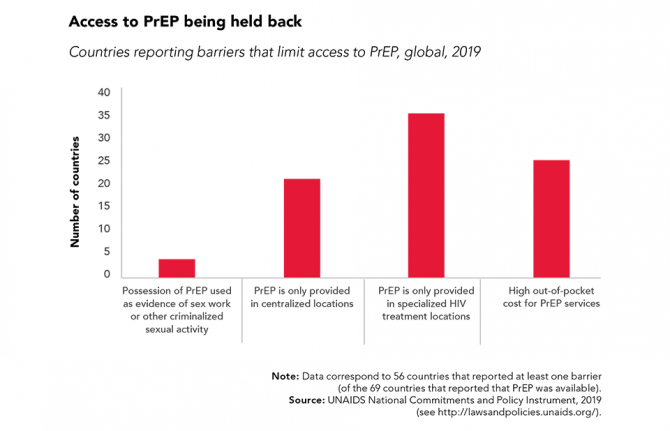
09 December 2019 09 December 2019Oral pre-exposure prophylaxis (PrEP) has shown considerable impact in reducing new HIV infections when provided as an additional HIV prevention choice to gay men and other men who have sex with men, transgender people and sex workers.
PrEP is now being rolled out in sub-Saharan Africa for serodiscordant couples and adolescent girls and young women who are at higher risk of HIV infection. Uptake is high when community-level stigma and misconceptions are addressed, when women and girls are provided with accurate and relevant messaging about PrEP and when PrEP is framed as an empowering prevention method and a positive life choice.
However, further global expansion of PrEP requires countries to address regulatory issues and other barriers that are stopping people who want to use PrEP from doing so.


Update
HIV treatment numbers continue to rise
02 December 2019
02 December 2019 02 December 2019For people living with HIV, being on treatment has two advantages: they stay healthy and, if their viral load is suppressed to undetectable levels, they can’t pass on the virus to their sexual partners.
The number of people living with HIV who are on treatment continues to rise, with an estimated 24.5 million on antiretroviral therapy in mid-2019—more than double the number on treatment in 2012. However, treatment scale-up is still not on track to meet the target by the end of 2020 of 30 million people living with HIV on treatment, and with 37.9 million people living with HIV at the end of 2018, the unmet need for treatment is still worryingly large.
Related


Update
Sex workers often not accessing HIV prevention services
18 November 2019
18 November 2019 18 November 2019Despite the availability of a widening array of effective HIV prevention tools and methods—and a massive scale-up of antiretroviral therapy in recent years—there has been insufficient progress in reducing global new HIV infections, which have fallen by only 16% since 2010.
The United Nations General Assembly’s 2016 Political Declaration on Ending AIDS calls on countries to ensure that 90% of those at risk of HIV infection are reached by comprehensive prevention services by 2020. However, sex workers―and other key populations―often haven’t been accessing the prevention services they need. Country data reported to UNAIDS within the last three years show a widely varying coverage of combination HIV prevention services.
With female sex workers having a 21 times higher relative risk of HIV acquisition compared to the general population, access to suitable HIV prevention options is vital.
Related
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025


Update
HIV-related discrimination far too high
12 November 2019
12 November 2019 12 November 2019In the early days of the HIV epidemic, pervasive stigma and discrimination against people at higher risk of HIV infection and people living with HIV nearly paralysed the AIDS response. HIV-related discrimination stops people accessing the HIV services they need to stay healthy and can affect incomes and livelihoods and a whole range of other aspects of people’s lives.
Discriminatory attitudes towards people living with HIV remain extremely high in far too many countries. Across 26 countries with recent population-based survey data, the percentage of people aged 15–49 years with discriminatory attitudes towards people living with HIV ranged from 16.9% in South Africa to 80% in Guinea.


Update
Many prisoners are lacking basic HIV services
28 October 2019
28 October 2019 28 October 2019Environmental, social, cultural, human rights and biological factors all lead to a greatly increased risk of contracting tuberculosis and HIV in prisons.
Risk behaviours such as sharing of used needles and syringes, unprotected sex, sexual violence and lack of access to comprehensive HIV prevention and harm reduction services put people in prisons at heightened risk of HIV and other infections. Globally, HIV prevalence among people in prison is much higher than among the general population, with incarcerated people on average five times more likely to be living with HIV compared with adults outside. Key populations―people who inject drugs, sex workers and, in some countries, transgender people and gay men and other men who have sex men―tend to be overrepresented among incarcerated populations.
Despite the relative ease of reaching people within prisons, HIV services are not provided in prisons in many countries. Across the last three years of country reports to UNAIDS, very few countries reported programme data on the provision of condoms (32 countries), opioid substitution therapy (24 countries) and sterile injecting equipment (three countries) in prisons, but 74 countries reported programme data on antiretroviral therapy coverage and 83 countries reported HIV testing in prisons.
Related
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025

Update
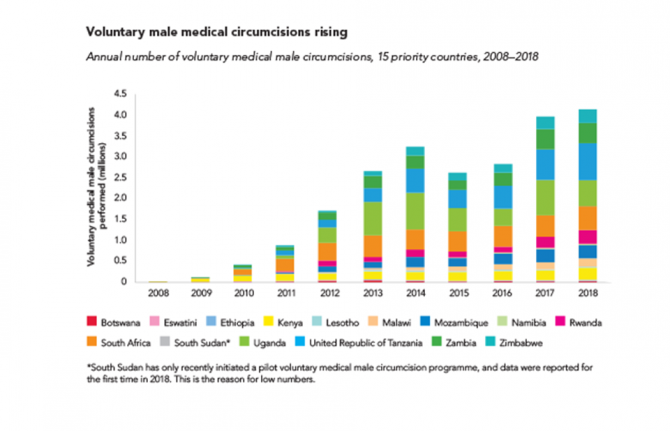
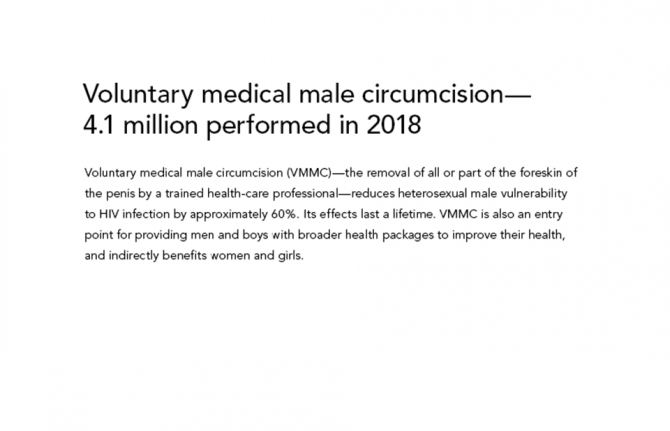
Voluntary medical male circumcision―4.1 million performed in 2018
21 October 2019
21 October 2019 21 October 2019Voluntary medical male circumcision (VMMC)―the removal of all or part of the foreskin of the penis by a trained health-care professional―reduces heterosexual male vulnerability to HIV infection by approximately 60%. Its effects last a lifetime. VMMC is also an entry point for providing men and boys with broader health packages to improve their health, and indirectly benefits women and girls.
VMMC can have a major impact on HIV epidemics in high-prevalence settings. VMMC services incorporate a package of prevention interventions, including safer sex education, education on and provision of condoms, HIV testing and the management of sexually transmitted infections.
About 11 million VMMCs have been performed in 15 priority countries in eastern and southern Africa since the beginning of 2016. In 2018 alone, about 4.1 million voluntary circumcisions were performed among males of all ages, a slight increase from the 4 million carried out in 2017.
There has been progress towards the target of 25 million additional circumcisions for HIV prevention from 2016 to 2020. However, at the end of 2018, when 15 million circumcisions should have been performed, the world was off-target by 4 million circumcisions.
Related
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025











