Asia Pacific




Feature Story
Supporting communities to be involved in the AIDS response in Thailand
20 January 2020
20 January 2020 20 January 2020The UNAIDS Country Office in Thailand, with a small team of three staff members, is located in Bangkok. Orawan Bettenhausen, the Administrative Assistant, has been part of the team for almost 20 years. “Being part of the UNAIDS family has empowered and transformed me into who I am today. I have been very fortunate to have had country directors who have coached me, and great colleagues and peers, both within and outside of UNAIDS, who have assisted, supported and inspired me,” she said.
Ms Bettenhausen recalls meeting a person living with HIV, a representative of the Thai Network of People Living with HIV, in her first weeks with UNAIDS. “I asked him about his life. When he finished talking, I was in tears,” she said. “To my surprise, he told me that neither he nor any other person living with HIV would want me to feel sorry for them. They just wanted to be accepted for who they are. He taught me a huge lesson, and I made a commitment to work for people living with and affected by HIV.”
Throughout the years, she has assisted the Country Director and the team to get communities, civil society organizations and people living with HIV meaningfully involved and engaged in the AIDS response. “As the Administrative Assistant , I do feel that I support our community partners in different ways, such as contributing to the execution of joint projects, facilitating logistic support to make sure communities can attend regional and national events and providing interpretation from Thai to English and vice versa. I feel I am giving community members the opportunity to overcome language barriers, to be present in decision-making spaces to voice their needs and showcase their work outside Thailand,” she explained.
Ms Bettenhausen has witnessed important changes in the AIDS response in Thailand. For example, she remembers UNAIDS implementing projects in collaboration with civil society organizations and facilitating dialogues between policymakers, HIV programme implementers and community representatives at a time when stigma and discrimination against people living with HIV and key populations was a major concern in the country.
Since 2015, Thailand has implemented the 3-by-4 Package for Stigma-Free Health Facilities, with comprehensive programmes to address and remove barriers to accessing health services. In 2019, the country announced the Thailand Partnership for Zero Discrimination, which goes beyond health settings and includes areas such as workplaces and the education system. UNAIDS has been involved since the outset of the initiative by providing technical assistance to formulate the zero discrimination strategy, to develop a monitoring and evaluation plan and to operationalize the strategy in a joint effort with the Thai Government and civil society.
“My contribution to this achievement was to provide continuous support to the Country Director, who played a critical role in linking stakeholders from different sectors and bringing them together, making sure that communities were always involved and enabled to speak up. Now our government counterparts work alongside civil society organizations. All key stakeholders are equal and come together to make decisions and move in the same direction. A true partnership!” said Ms Bettenhausen.
Ms Bettenhausen grew up in northern Thailand. Her passion for the public sector started in early childhood, as she watched her father improve the livelihoods of farmers and their families through his work as an adviser for the German Government and rural development donors. Later, while studying for a master’s degree in management, she realized business was not her calling and made the decision to write her dissertation on the Human Development Center, a nongovernmental organization working in the Klong Toey slum in Bangkok. The two months that she spent working in the slums and collecting data for her dissertation gave her insight into urban poverty, drug use, child abuse and HIV. “After I graduated, I joined the business world for two years, but I felt my vocation was to follow in my father’s footsteps and to work for people. Fate was on my side and I got a position with UNAIDS,” she said.
Ms Bettenhausen’s main challenge at the Country Office is to keep up with the various tasks, as administrative work is often time-consuming. Nevertheless, she believes that everything done with due diligence is contributing to making a difference. Her work is not only critical to ensuring that the UNAIDS Country Office can fulfil its mandate, but also key to achieving the goal of ending AIDS by 2030.
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025





Feature Story
Turning the tide of the HIV epidemic in Thailand
17 January 2020
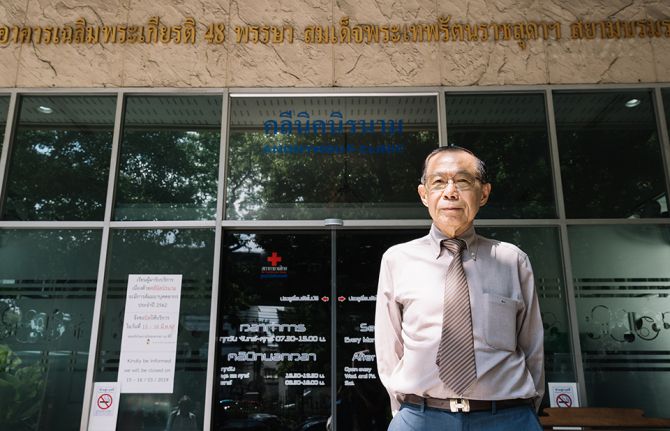
17 January 2020 17 January 2020It is a morning like any other at the Thai Red Cross AIDS Research Centre, a civil society organization operating under the umbrella of the Thai Red Cross Society. In a building in the heart of Bangkok, nurses, doctors, counsellors and peer educators are busy with their daily work, providing HIV services for the 200 people who attend the Thai Red Cross Anonymous Clinic every day for medical check-ups, HIV tests and HIV prevention services, including condoms and pre-exposure prophylaxis (PrEP).
When he was 35 years old, Praphan Phanuphak―the Director of the centre, which he co-founded in 1989―discovered the first case of HIV in Thailand. “It happened by accident. A patient was referred to me to investigate why he had a recurrent fungal skin infection,” he recalled. “In February 1985, this patient was admitted with pneumocystis pneumonia. During that month, another man was referred to the hospital with generalized cryptococcus infection. Both were diagnosed with HIV. Since then, I have devoted my life to treating people living with HIV and developing solutions to expand access to HIV services in the country.”
Mr Praphan remembers that in the early days of HIV the response in Thailand faced several challenges. At the time, Thai law required hospitals to report the names of people diagnosed with HIV to the Ministry of Public Health, which contributed to increasing stigma and discrimination against people living with HIV. In response, the Thai Red Cross established the Thai Red Cross Anonymous Clinic, Asia’s first anonymous clinic, and advocated with the Thai Government to remove the reporting law. The Anonymous Clinic remains the most renowned centre providing voluntary HIV testing in the country.
“Until the beginning of 2000, antiretroviral medicines were not available through public health facilities in Thailand, and many people living with HIV could not afford to buy them,” said Mr Praphan. He said that in 1996 the Thai Red Cross AIDS Research Centre was the first to provide free antiretroviral medicines as part of its clinical trials through the HIV Netherlands–Australia–Thailand Research Collaboration.
“After years of despair, a time of hope finally came. For that, I want to thank Her Royal Highness Princess Soamsawali, who stood by our side by setting up a fund for the prevention of mother-to-child transmission of HIV in 1996, several years before the Thai Government started its successful prevention programme,” said Mr Praphan.
The AIDS response in Thailand has changed dramatically over the years. In 2006, Thailand integrated its HIV services, including antiretroviral therapy, into its universal health coverage scheme. Since 2014 Thailand has provided antiretroviral therapy for all regardless of their CD4 level. Everyone can access treatment for free, and people living with HIV are offered treatment immediately after diagnosis.
However, many people are starting antiretroviral therapy late. “We have the medicines, but many people are not being diagnosed fast enough,” warned Mr Praphan. Despite tremendous progress, the HIV epidemic is not yet over in Thailand. HIV remains concentrated among key populations: almost 50% of new HIV infections in 2018 were among gay men and other men who have sex with men. Low uptake of HIV testing among key populations is related to the acceptability of services and stigma and discrimination, which hinder access to HIV diagnosis, prevention and care.
“From our experience, helping key populations to reach their peers and bring them to HIV drop-in centres, where they can be tested, is the best way to detect and diagnose people living with HIV early enough,” said Mr Praphan, who successfully advocated to amend Thai law to allow certified lay providers from key populations to provide a number of HIV services.
The Thai Red Cross AIDS Research Centre’s approach focuses on undertaking pilot projects to generate evidence to inform national planners and policymakers. That evidence provides a foundation for national acceptance and the roll-out of innovation on a national scale.
Taking the lead in reaching out to key populations, the centre has been offering PrEP to people at substantial risk of HIV since 2014 through projects such as the Princess PrEP Programme. In October 2019, Thailand introduced PrEP under its universal health coverage benefits package as a pilot phase in efforts to scale up PrEP nationwide.
Mr Praphan believes that policymakers and programme implementers should understand that, “We cannot continue to do business as usual. In Asia and the Pacific, several countries are still either sceptical or conservative in terms of promoting the necessary approaches to change the course of the HIV epidemic.” He thinks that the region cannot achieve the 90–90–90 targets by 2020 at the current pace. “We need to think out of the box and look at what other countries are doing that can be taken as a model. This is how we can move faster on our way towards ending AIDS as a public health threat.”
Region/country
Related


Press Release
Sri Lanka eliminates vertical transmission of HIV and syphilis
13 December 2019 13 December 2019GENEVA/BANGKOK, 13 December 2019—UNAIDS congratulates Sri Lanka for achieving the elimination of vertical transmission of HIV and congenital syphilis. “Sri Lanka’s remarkable achievement gives me hope and shows that change is possible. It is clear that when a country ensures that services are accessible and stigma-free for women, including for women living with or affected by HIV, results follow that benefit women’s health, their children’s health and society as a whole,” said Winnie Byanyima, UNAIDS Executive Director.
According to the Ministry of Public Health of Sri Lanka, in 2018 all pregnant women diagnosed with HIV started antiretroviral therapy and 97% of pregnant women diagnosed with syphilis received treatment. The country has not reported any case of mother-to-child transmission of HIV since 2017 and the rate of congenital syphilis has been reduced to less than 50 cases per 100 000 live births in 2017 and 2018.
“The elimination of mother-to-child transmission of HIV is the result of strong political commitment, a successful multisectoral integrated approach built upon the foundations of the public health system and technical expertise,” said Anil Jasinghe, Director General of Health Services in Sri Lanka.
Sri Lanka becomes the fourth country in the Asia–Pacific region after Thailand, Malaysia and the Maldives to be validated for eliminating vertical transmission of HIV and congenital syphilis.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS GenevaAnne-Claire Guichard
tel. +41 22 791 2321
guicharda@unaids.org
UNAIDS Bangkok
Michela Polesana
tel. +66 9445194092
polesanam@unaids.org
UNAIDS Media
tel. +41 22 791 42 37
communications@unaids.org
Press centre
Download the printable version (PDF)
Region/country
Documents
The response to HIV in Asia and the Pacific — Global AIDS update 2019
16 July 2019
Asia and the Pacific boasts some of the earliest successes in responding to the HIV epidemic. The region’s response, however, is highly uneven, and several national HIV programmes are not keeping pace with their growing HIV epidemics. Creeping complacency in other countries risks squandering gains made thus far.
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment
Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment

21 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
UNAIDS data 2024
02 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024


Feature Story
Fear of the unknown
12 August 2019
12 August 2019 12 August 2019When her husband came home with a positive HIV test, Jokapeci Tuberi Cati decided that she wanted to get tested too.
“Fear of the unknown, of the stigma associated with HIV and of rejection were all going through my mind before the test,” she said.
Once she got tested in Lami, Fiji, she sighed and said to herself, “done and dusted.”
But she had a nagging thought that her test would be positive and she started thinking about a coping mechanism. She kept playing over and over the same scenario, with one question: how will she live from this point onward?
“In fact, little happened in reality,” Ms Cati said. She recounted that an experienced doctor treated her with the utmost care when he informed her of her HIV-positive status.
She returned home and decided that she and her husband would bear the diagnosis together as a couple. No one needed to know anything.
With time, Ms Cati learned to cope with her new status and vowed to accept her new life. She now wanted to help people to understand the issue so that they would not go through the same experience.
But first she had to let people know.
“The moment I decided to disclose my HIV status to my family and friends, there was a different magnitude of support,” she said. Thinking back to 20 years ago, she still cannot forget how people reacted with such warmth.
That emboldened her to become much more proactive and share her story with a greater number of throughout the country. She is now a programme manager at the Fiji Network for People Living with HIV. Despite losing her husband, Ms Cati is thankful she found out about her status, because with medication she did not transmit HIV to her children.
“Better to know than not know—the benefits are huge,” she said.
Region/country
Related


Feature Story
Indonesia commits to piloting PrEP
15 July 2019
15 July 2019 15 July 2019Indonesia has decided to pilot pre-exposure prophylaxis (PrEP) in four cities with high levels of HIV prevalence. PrEP is a way for people who do not have HIV but who are at substantial risk of getting it to prevent HIV infection by taking a pill every day. It is hoped that the pilot project will pave the way for a wider roll-out across the country.
The commitment to piloting PrEP came during the 1st Indonesian Symposium on PrEP, which was organized by UNAIDS at the end of June. The two-day event brought together around 150 clinicians, public health officials and representatives of key populations, who shared their experiences of PrEP research and implementation strategies across the Asia-Pacific region. The pilot in Indonesia will be conducted in close collaboration with the Ministry of Health.
PrEP is a highly effective prevention choice for people who are at high risk of HIV infection such as sex workers, people who use drugs and gay men and other men who have sex with men. It is having a big impact in reducing new HIV infections in Australia and its availability is increasing in New Zealand, Thailand and Viet Nam. China, India, Malaysia and Philippines have also initiated pilot projects.
Prevention efforts are vital to strengthening the HIV response in Indonesia and PrEP would be a significant addition to the country’s combination prevention approach. Indonesia had 46000 new HIV infections in 2018 and has one of the fastest growing epidemics in the Asia Pacific region. In 2018 there were 640000 people living with HIV in the country and only 17% had access to treatment.
The discussions at the symposium helped to disperse some of the common misconceptions regarding PrEP, both among communities and services working to reduce new HIV infections. Civil society activists expressed their strong support for PrEP roll-out.
“PrEP will become a necessity for sex workers,” said Rito Hermawan of the Indonesian Sex Workers Network, “As well as using condoms, they can get additional protection by using PrEP. We must educate people about PrEP to stop any misconceptions.”
Other civil society activists echoed their support.
“The more I learn about the benefits of PrEP, the more I wonder why it is not available here,” said Mr. Riunaldi from Intermedika Prana Foundation, “I am hopeful that more people will understand how important PrEP is for our country.”
Participants in the symposium said that many people were already accessing PrEP online, indicating a growing demand in Indonesia.
“It is incumbent on policy makers, health professionals, researchers and civil society organizations to ensure that those at risk of HIV infection have access to the information and resources needed to make informed decisions regarding their health” said Tina Boonto, UNAIDS Country Director for Indonesia.
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025


Feature Story
Pakistan: bringing services closer to communities affected by the HIV outbreak
03 July 2019
03 July 2019 03 July 2019A newly refurbished paediatric centre is to open in Ratodero, Pakistan, to serve families affected by the recent HIV outbreak in the district of Larkana. It is expected that the centre will be operational by mid-July.
Alia (not her real name), the mother of a two-year old girl, lives in the village of Mirpur Bhutto, in Ratodero Taluka in Larkana district. Alia’s world has been turned upside down since her family was caught up in the HIV outbreak in the area.
“My daughter was diagnosed with HIV just a few days ago, but she became so weak so quickly. She couldn’t eat anything we gave to her,” says Alia. After Sameera’s (not her real name) diagnosis, she was referred to Sheikh Zayed Children Hospital in Larkana to start antiretroviral therapy. The hospital is more than 50 kilometres away from the family home.
“I got these dispersible tablets for Sameera and some fever medicine, and since she started her treatment, I have seen some improvements in my daughter’s health. Her fever has gone and before there was diarrhoea from which she also recovered,” explains Sameera’s mother.
Alia’s husband is a farmer and earns less than two dollars a day. “We can hardly support our family of ten members,” she explains.
Poor road conditions and economic constraints make it difficult for Alia and her daughter to travel from their village to the district capital Larkana, currently the nearest health facility where her daughter can receive the treatment she needs.
Since the HIV outbreak was first reported in Larkana at the end of April, UNAIDS, UNICEF, the World Health Organization, the Sindh AIDS Control Programme and other partners have been calling for a new paediatric treatment centre in Ratodero to bring HIV services closer to the affected communities. As a result of these efforts and in the framework of the “Sindh HIV Outbreak Response Plan, May 2019-Apr 2020,” UNICEF is refurbishing the paediatric HIV treatment centre at Taluka Headquarters hospital in Rotadero, ensuring that treatment will be available in the area where Alia and her daughter live. When the new centre opens, HIV treatment services for Sameera will be less than 10 kilometres away.
“I know my Sameera will be fine and that she will get married and have children. This is what the doctor told me. For this to happen she must continue her treatment forever. I will follow the doctor’s instructions because this is what will save my daughter’s life,” says Alia.
By the end of June, 877 people had been newly diagnosed with HIV in the Larkana district. More than 80% of the new cases are among children aged under 15 years old. A total of 721 people had already been registered in care programmes and 482 people (365 of them children under the age of 15) were on treatment.
“UNAIDS is working closely with the government, civil society organizations, the association of people living with HIV, UN agencies and all other partners to ensure that both the immediate response to the HIV outbreak and longer-term programmatic measures will be implemented and sustained,” said Maria Elena Borromeo, UNAIDS Country Director for Pakistan and Afghanistan.
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025


Feature Story
A powerful voice for the AIDS response
25 June 2019
25 June 2019 25 June 2019In September 2018, on the sidelines of the Forum on China-Africa Cooperation (FOCAC) summit in Beijing, China’s First Lady, Professor Peng Liyuan, and her fellow First Ladies from Africa lit up a Reb Ribbon at the centre of the meeting hall, officially launching the Joint Initiative of the China-Africa Thematic Meeting on HIV/AIDS Prevention and Control.
The 2018 FOCAC summit gathered together over 20 African Heads of State and First Ladies to discuss closer partnership between China and African countries, including on health-related matters. During the thematic meeting, Professor Peng announced a three-year HIV prevention campaign among adolescents to begin in 2019 as well as a community health promotion programme involving China, several African countries and international organizations, including UNAIDS.
For more than 10 years, Professsor Peng has had a particular interest in reducing the impact of HIV among children and adolescents, especially among children orphaned by AIDS. In 2016, she hosted the China-Africa Children Summer Camp that brought together children living with or affected by HIV from China, Ghana, South Africa and Zimbabwe. During the camp, the First Lady helped launch the Chinese version of the Bravest Boy I Know, a book which helps children understand the issues surrounding HIV and reduce the stigma and discrimination faced by children affected by the virus.
In 2015, Professor Peng attended a meeting of the Organization of African First Ladies against HIV/AIDS (OAFLA) in Johannesburg, South Africa, where she underlined the importance of four key issues critical to ending AIDS by 2030: universal access to HIV treatment; public information and education; educational opportunities for adolescents and economic development to eliminate poverty.
Together with national Red Ribbon Ambassadors, Professor Peng has for many years visited communities across China, including schools and universities, to raise awareness about HIV prevention and to reduce the stigma and discrimination associated with the virus.
An acclaimed soprano singer, Professor Peng has proven to be a powerful voice for those living with or affected by HIV.
She has been a World Health Organization Goodwill Ambassador for Tuberculosis and HIV/AIDS since 2011. In 2017, she was awarded a UNAIDS Award for Outstanding Achievement in recognition of her contribution to the response.
“A caring heart is our best weapon against AIDS,” she said in accepting the award. “We can save lives if we take action. We must succeed and we will succeed.”
Focus on
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025


Feature Story
Virtual communities power HIV services in China
21 June 2019
21 June 2019 21 June 2019According to national estimates, an estimated 1.25 million people are living with HIV in China, with almost 400 000 unaware of their status. China’s epidemic is concentrated among key populations at higher risk of HIV, including men who have sex with men. That’s why it’s crucial to meet these communities where they socialize, including in virtual spaces such as gay dating applications.
Danlan Public Welfare is a nongovernmental organization that advocates for lesbian, gay, bisexual and transgender rights. It is also behind the largest gay dating application in China, Blued, which today has more than 28 million users. It has incorporated community-driven HIV prevention messaging into the application and includes basic facts about the virus, as well as information on prevention, testing and treatment options and how and where to contact related services. Interactive quizzes test users’ knowledge about HIV.
As well as this powerful virtual tool, Danlan also operates free HIV rapid testing outreach projects in partnership with the Municipal Centres for Disease Control and Prevention. People can take a free HIV test and get their results in just 10 to 15 minutes.
As the Blued dating application becomes popular around the world, Danlan is extending its HIV prevention programme to Belt and Road Countries. Since March 2019, users in Indonesia have been able to access the “Blued Help Center". The service is provided in cooperation with a local civil society organization called "VictoryPlus”, which allows users to post their concerns regarding HIV-related issues and receive an immediate answer. Blued’s “We Care” programme also offers virtual information on HIV services close by.
In Thailand, Danlan worked together with a civil organization called "Impulse" to advocate for HIV prevention programmes and provided free rapid HIV testing services. Danlan has also cooperated with Mahidol University on HIV-related risk behaviour research.
In April 2019, the chief executive officer of Danlan, Geng Le, received an award for “Outstanding Innovative Model” by the Confederation of Trade Unions of Chaoyang, Beijing. It is estimated that community-based organizations like Danlan are responsible for finding 30% of all new HIV cases in the city.
“We are doing our best to use science and technology to improve the lives of lesbian, gay, bisexual and transgender communities, including their health,” says Geng Le. “Our vision is that all young people should be able to live with dignity, be free of stigma and discrimination and love who they want to no matter where they come from, what their sexual orientation is and what their HIV status is.”
Blued is more than just a dating application now. It is also a virtual healthcare resource centre that provides support to the wellbeing of the LGBT community.
Focus on
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025




Feature Story
UNAIDS continues to support the response to the HIV outbreak in Pakistan
18 June 2019
18 June 2019 18 June 2019UNAIDS is continuing its support to Pakistan in responding to the outbreak of HIV in Larkana, during which more than 800 people have been newly diagnosed with the virus. More than 80% of the new cases are among children aged under 15, with most among children aged under 5. By 17 June, 396 people had been referred to treatment.
At a press conference on June 14 the authorities presented the findings of a preliminary investigation into the outbreak. It concluded that poor infection control practices, including a lack of sterilization and the re-use of syringes and intravenous drips, are the most significant factors behind the rise in new infections.
“There is a huge amount of work that needs to be done to improve infection control and support the affected children and their families,” said UNAIDS regional director, Eamonn Murphy, during the press conference held in Karachi, Pakistan. “UNAIDS will continue to facilitate and coordinate within the United Nations system and with other partners to ensure that the required support is provided effectively and efficiently,” added Mr Murphy.
As well as improving infection control procedures, the preliminary investigation found that strengthening community education is critical to raise awareness about HIV prevention and to tackle stigma and discrimination. The conclusions of a rapid assessment on HIV-related knowledge presented at the press conference found that information about HIV is very limited among the affected communities. Many parents and caregivers learnt about HIV only on the day their children were diagnosed or because of media reports about the increase in cases. A lack of accurate information created panic and some families with children diagnosed with HIV have been shunned and isolated.
In response, UNAIDS in partnership with UNICEF, UNFPA, the World Health Organization and the JSI Research and Training Institute have been supporting national partners to develop a community response plan to promote health education and reduce stigma and discrimination. The Sindh AIDS Control Programme, together with UNAIDS and UNICEF, has started to train health workers on paediatric case management and health education sessions are being organized with the involvement of community led organizations and religious leaders. Training sessions for local media on responsible HIV reporting are also being carried out.
UNAIDS has been working closely with the federal and provincial governments to provide on-site technical support to help respond to the crisis and mitigate its impact. Sindh’s Ministry of Health has increased its efforts to prevent unlicensed and informal medical practices from operating and, as a result, 900 health clinics and unlicensed blood banks have been closed.
The preliminary investigation was led by the World Health Organization, in partnership with organizations including the Sindh AIDS Control Programme, Aga Khan University, the Field Epidemiology and Laboratory Training Programme, the Dow Medical University in Karachi, the Microbiology Society of Infectious Disease and UN agencies, including UNAIDS, UNICEF and UNFPA.
With 20 000 new HIV infections in 2017, Pakistan has the second fastest growing AIDS epidemic in the Asia Pacific region, with the virus disproportionately affecting the most vulnerable and marginalized, especially key populations. UNAIDS continues to work with the government and partners in Pakistan to strengthen the response in the country.
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025