Asia Pacific


Update
Metro Manila city leaders commit to intensifying HIV response
11 September 2017
11 September 2017 11 September 2017Mayors and other city leaders from the 17 cities that make up the National Capital Region in the Philippines pledged to make the HIV epidemic a public health emergency requiring multisectoral strategies and a full provision of resources. The city representatives recently signed a city HIV resolution during a dinner meeting in Manila hosted by the Secretary of the Department of Health, Paulyn Jean Rosell-Ubial.
A recent UNAIDS report, Ending AIDS: progress towards the 90–90–90 targets, has helped to galvanize this action. The report found that the number of new HIV infections in the Philippines has risen by 140% in the past six years and the country has the fastest growing HIV epidemic in the Asia and the Pacific region. Health authorities say that the 17 cities in the National Capital Region accounted for more than 40% of reported HIV cases in the country.
Ms Rosell-Ubial stated that she had raised this alarm as early as last year, when she took office, calling the situation a national emergency. She appealed to the mayors and city officials of Metro Manila for their help in delivering crucial services to community groups and key populations. The Mayor of Taquig City and Chair of the League of Cities, Laarni “Lani” Cayetano, expressed her support for the initiative and underlined the efforts of Taguig City in providing HIV services.
The Secretary of Health expressed appreciation for the personal support of Eamonn Murphy, UNAIDS Director of the Regional Support Team for Asia and the Pacific, and for the long-term contribution from the UNAIDS country office.
Mr Murphy praised the strong leadership of the Secretary of Health and the commitment by cities in the Manila region and pledged to help mobilize technical support, and is in discussion with development partners regarding these efforts.
The city HIV resolution recognized that the 2030 Agenda for Sustainable Development committed countries to ensuring healthy lives and the well-being of all citizens, as well as ending AIDS by 2030. It commits cities to increasing financial investments and accelerating the implementation of high-impact programmes, including ensuring quick diagnosis and entry into treatment, HIV services tailored to the needs of gay men and other men who have sex with men and innovative prevention programmes, including targeted outreach and pre-exposure prophylaxis. The resolution also promised to eliminate HIV-related stigma and discrimination and other human rights violations that prevent key populations and people living with HIV from accessing services.
Quotes
“We can buy all the drugs that we need. We can buy all the test kits that we need. We can find the government funding to do this, but what we need is for our cities to join with the Department of Health in making sure that we deliver through new and innovative delivery systems. Without this partnership, we won't reach our goals of 90–90–90 and 100% elimination of mother-to-child transmission by 2020.”
“I am confident that all cities in the National Capital Region will heed the call to take the actions necessary to reach our 90–90–90 goals by 2020. As the Chair of the Philippines League of Cities, I call on all cities in the country to join us and act now.”
“The Philippines responded quickly and innovatively in partnership with the community to the first wave of the epidemic, and through strong, pragmatic and committed leadership is showing the nation has the capacity and the resolve to meet the challenges presented by the new wave of growing infections, particularly among young gay men and other men who have sex with men and transgender people.”
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025

Feature Story
China’s community health services are a model for the world
21 August 2017
21 August 2017 21 August 2017The Yuetan Community Health Centre is nestled on a narrow lane in an old residential part of central Beijing, China. Its yard is packed with bicycles, rather than cars—an indication that the centre is serving people close to where they live.
“Through our centre and nine affiliated community health stations, we provide services to 150 000 people living in the Yuetan area,” said Du Xue Ping, Director of Yuetan Community Health Centre. “In addition to providing medicine, we also undertake health promotion, encouraging people to lead a healthy life. We know that prevention is far better than cure.”
The centre blends state-of-the-art Chinese medicine and Western medicine, serving 420 000 patients annually. It supports the community’s rapidly ageing population, overseeing two senior homes and staff who conduct home visits for seniors and people with mobility problems.
The facility is part of China’s highly regarded multitiered medical system, which has successfully brought life-saving services to people across the country. In this system, major diseases are handled in large hospitals and routine services are treated in community health centres. According to Chinese data, in 2015 there were more than 34 000 similar community health clinics providing essential health services to 706 million people in China. “Community health centres are the first line of defence in protecting people’s health,” said Michel Sidibé, Executive Director of UNAIDS. “The family-centred interface and clear bond between staff and patients exemplifies people-to-people connections.”
Mr Sidibé visited the community health centre to learn more about its holistic and comprehensive approach and how China’s community health system could help to inform the 2 million community health workers initiative, which was recently endorsed by the African Union.
In the 1970s, China’s community-based doctors dramatically improved access to health care in rural communities and were an inspiration to many other countries. China exported the model, sending teams of doctors and nurses to Africa.
“I know from my own personal experience the contributions China has made to primary health care in Africa,” said Mr Sidibé. “Chinese doctors provided crucial medical services to people in Mali where I am from.”
“The world can learn a lot from the Chinese experience,” said Mr Sidibé. “I am very impressed by the professionalism I witnessed here today.”
Region/country
Related

Update
China’s Belt and Road initiative to play a key role in overcoming global health challenges
21 August 2017
21 August 2017 21 August 2017Michel Sidibé, the Executive Director of UNAIDS, has urged international health leaders to prioritize health development. While giving his keynote address at the opening ceremony of the Belt and Road High Level Meeting for Health Cooperation: Towards a Health Silk Road, Mr Sidibé also expressed to the Vice-Premier of China, Liu Yandong, his appreciation for China’s efforts through the Belt and Road initiative to create greater cooperation for better health and highlighted the ongoing work to strengthen China–Africa health connections.
More than 20 ministers and deputy ministers of health and the Director-General of the World Health Organization, Tedros Adhanom Ghebreyesus, attended the meeting, which was held in Beijing, China, on 18 and 19 August. The meeting looked at ways to collaborate across shared health goals, including innovation and technology, vaccine safety, nutrition, maternal and child health and human resources for health.
A communiqué issued at the end of the meeting commits China to support UNAIDS in its work in related fields and includes concrete actions and deliverables, including the creation of a public health cooperation network and an alliance for sustainable health development.
China’s Vice-Minister of Commerce, Wang Shouwen, commended UNAIDS’ contribution to supporting China’s engagement with Africa and committed to strengthening cooperation with UNAIDS.
UNAIDS and the National Health and Family Planning Commission of China adopted a memorandum of understanding that enhances cooperation on the implementation of the Belt and Road initiative and the 2030 Agenda for Sustainable Development and aims to enhance the effectiveness of the global response to the AIDS epidemic. Both parties agreed to use the Belt and Road initiative as a catalyst and accelerator for the Sustainable Development Goals and achieving the global Fast-Track targets by 2020, including reducing new HIV infections and AIDS-related deaths to fewer than 500 000 globally and eliminating HIV-related stigma and discrimination. The five-year agreement includes an annual US$ 1 million contribution to UNAIDS.
Quotes
“Health is the common pursuit of all mankind and also the eternal theme echoing in the ancient Silk Road for thousands of years. We hope to strengthen cooperation with the international community and contribute more Chinese wisdom to the development of human health.”
“The Belt and Road initiative is about inclusiveness and connecting the dots across borders, issues and agendas for mutual benefit and development. It is a people-centred approach. Without this there can be no transformation in health.”
“The Belt and Road initiative contains the fundamentals to achieve universal health coverage, access to medicines, human resources and a platform to share experience and promote best practices.”
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025




Update
Grassroots hero: thinking out of the box by mixing health and fun
15 August 2017
15 August 2017 15 August 2017There is a quiet hum in the room from the mostly young men sitting in chairs, eyeing their smartphones and chatting. Suddenly, a cheerful figure bursts into the executive lounge of the high-rise building in Taguig City, Philippines.
“Thank you, thank you,” said Ronivin (Vinn) Garcia Pagtakhan, the Executive Director and Founder of LoveYourself, a community-based organization providing health and empowerment services to men who have sex with men and transgender people. The team were wrapping up after a major event promoting HIV testing.
Mr Pagtakhan, with his shock of brown hair, frosted with a light green tint, bounced from one group to the next, joking and repeating his thanks.
Almost everyone here is a volunteer,” explained Mr Pagtakhan. “I get really moved when I talk about my volunteers. I owe everything to them.”
LoveYourself provides HIV testing and treatment services, as well as oral pre-exposure prophylaxis (PrEP) and tuberculosis screening. It has 25 staff members, who are supported by around 800 volunteers. Mr Pagtakhan founded LoveYourself in 2011, modelling it on a lesbian, gay, bisexual and transgender youth centre he volunteered in while living in San Francisco, United States of America.
“At the time, I felt there was a real problem with the way we were handling HIV prevention among the gay community in the Philippines,” said Mr Pagtakhan. “It was all about fear. I wanted something more optimistic and encouraging. I wanted a place that was lively, where people would want to hang out.”
He was only 25 years old at the time. “As they say, I know my market, because I am part of the community.”
He graduated from nursing school in the Philippines when he was 18 and got the fourth highest score on the national nursing board examinations. “This meant that I was in high demand by other candidates as a teacher helping to prepare people for their licensing exams. I travelled around the Philippines giving classes and I used social media to reach out to students as well,” said Mr Pagtakhan.
He became a celebrity on social media, with 600 000 followers on Twitter, and won the prestigious international Twitter Shorty Awards as the Nurse of the Year. The prize money helped start LoveYourself.
“The first three years, it was like sending your child off to college. I basically supported the organization on my earnings. We didn’t have any donors,” said Mr Pagtakhan. “I like to think out of the box and I had a particular vision. I didn’t want grants to dictate what we did or became. I wanted to create ripples of positive change in the community. LoveYourself isn’t just about HIV, but rather about increasing a person’s self-worth.
The organization has three community centres in the Manila, Philippines, area offering HIV testing and other services. Anyone can drop in, even on the weekends and in the evenings, for free health services.
LoveYourself tested about 20 000 people in 2016 and diagnosed around 1500 new HIV infcetions, which represent around 50% of the newly diagnosed HIV cases reported by the Department of Health in Manila. LoveYourself also works with companies and schools to help them develop HIV policies and to conduct on-site HIV tests.
In July, the organization began piloting PrEP and with support from UNAIDS and the World Health Organization plans to start a demonstration project offering self-testing before the end of the year.
In just six years, LoveYourself has grown to become an important HIV service provider in Manila. Mr Pagtakhan is proud of the organization’s achievements and has bigger ambitions. “We are still renting. I want LoveYourself to own a place, which is a community centre, where we can have health services but also original events and activities,” he said.
For more information on LoveYourself, go to http://www.loveyourself.ph.
Resoures
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025



Feature Story
UNAIDS Goodwill Ambassador Pia Alonzo Wurtzbach ramps up HIV advocacy efforts
09 August 2017
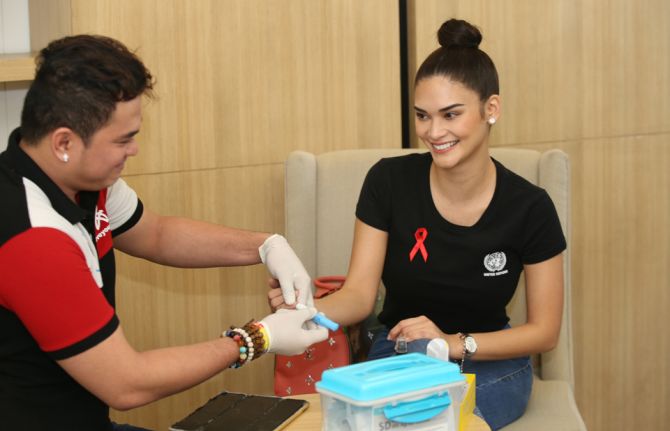
09 August 2017 09 August 2017Miss Universe 2015 and UNAIDS Goodwill Ambassador for Asia and the Pacific, Pia Alonzo Wurtzbach has launched an HIV awareness campaign with a public HIV screening. On 9 August, the model and actress, along with Mayor Lani Cayetano of Taguig City in the Philippines undertook the screening which was conducted by the community organization LoveYourself in Taguig City.
“As the UNAIDS Goodwill Ambassador for Asia and the Pacific, I wanted to start my HIV advocacy here at home in the Philippines,” said Ms Wurtzbach. “It’s important because the country has the fastest growing HIV epidemic in the region.”
A recent UNAIDS report has found that new HIV infections in the Philippines increased 140% between 2010 and 2016. Taguig City is one of the 17 cities in the Metro Manila area, which account for 40% of new infections in the country. Mayor Cayetano is the national chairperson of the League of Cities in the Philippines and promised to encourage other cities to scale-up HIV testing.
“The city of Taguig will always be here to support you Pia,” said Mayor Cayetano.
Ms Wurtzbach unveiled the project Progressive Information Awareness campaign, or the PIA project which aims to inform young people about HIV through social media, youth-friendly and informative videos, as well as promote policies which will enable young people, particularly from key populations to access HIV and other key health services. The PIA project is also working with a coalition of government, non-profit organizations and business partners on a major fundraising and award World AIDS Day Gala.
“With the PIA Project we hope to see an increase in HIV awareness, spread love for people living with HIV, and make HIV testing among Filipinos a normal part of their health and wellness routine,” said Ms Wurtzbach.
Across Asia and the Pacific young people from key populations are at higher risk of HIV.
“The HIV movement among young people that Pia is lighting up here in the Philippines will resonate around the Asia-Pacific region,” said Eamonn Murphy, Director, UNAIDS Regional Support Team for Asia-Pacific.
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025


Feature Story
Quezon City’s HIV programme becomes a model for other cities
13 July 2017
13 July 2017 13 July 2017The 2030 Agenda for Sustainable Development takes to scale what the AIDS response has been working towards for 30 years—a multisectoral, rights-based, people-centred approach that addresses the determinants of health and well-being. The individual stories in this series highlight the linkages between HIV and related Sustainable Development Goals (SDGs), each told from the personal perspective of people affected by HIV. The series paints a picture of how interconnected HIV is with the SDGs and how interdependent the SDGs are with each other. Most importantly, the stories show us the progress we have achieved with the AIDS response and how far we have left to go with the SDGs.
Klinika Bernardo, popularly known as the Sundown Clinic, is located along a bustling highway. It operates from 15:00 until 23:00, allowing a maximum number of clients to visit. “We cater to men who have sex with men from all over the Philippines,” said Leonel John Ruiz, head physician at Klinika Bernardo. “Only 40% of our clients are from Quezon City.”
In 2012, Quezon City became the first city in the Philippines to open a clinic providing services for men who have sex with men and transgender people. From the start, demand for services at the Sundown Clinic was high. Almost 250 HIV tests and pre- and post-test counselling services were carried out in its first two months of operation, and 18 people tested positive for HIV.
Although same-sex relationships are legal in the Philippines, there is a high degree of stigma and discrimination towards men who have sex with men. Fear of being outed and ostracized prevents many men from accessing traditional health services. Studies by city health officials show that two-thirds of men who have sex with men in Quezon City have never had an HIV test.
“This is my first HIV test. I do not know what to expect,” said one young man while filling out registration forms. “I tried to read up on HIV so I would have some background information, but it took me a while to gather the courage to come here.” The young man found the staff supportive and skilled at calming his nerves. People who test positive for HIV receive counselling on antiretroviral medicines and are accompanied by staff through their initial months of HIV treatment, which is free in the Philippines.
Quezon City now operates three Sundown Clinics and in the past few years has significantly increased investments in its HIV programmes. With nearly 3 million residents, Quezon City is the Philippines’ most populous urban centre and has made stopping a burgeoning AIDS epidemic a top priority. Mayor Herbert Bautista has encouraged city residents to know their HIV status, and he has taken an HIV test in public. The city’s effort to scale up HIV testing among men who have sex with men has proven successful, with such tests increasing 30 times. Forty per cent of the city’s HIV tests take place in Sundown Clinics, effectively proving that removing barriers increases access to services.
“Since we have been operating, the perspective has definitely changed,” says Leonel. “Before, we would have a hard time inviting people for testing. Now, most of our clients are walk-ins. People are personally and actively seeking information.” Several other local city governments are starting to adapt the Quezon City model and establish their own clinics.
The Sundown Clinic staff speak proudly of their achievements, but they look forward to closing shop one day. “I pray before sleeping,” says Adel, the only female peer educator at Klinika Bernardo. “I hope that one day there will be no one in need of our services. That’s what I am working for.”
SDG 17: Strengthen the means of implementation and revitalize the global partnership for sustainable development
Early in the AIDS response, in the absence of treatment options and the overwhelming scale of people affected by HIV, it was clear that a purely clinical response to the epidemic was not sufficient. Relatives, faith-based organizations and alliances of people affected by HIV stepped in to do what they could to help people die with dignity, to support the orphans, spouses and dependants left behind and to fight for a new way of doing things. Groups of vastly different people linked by the shared experience of the fear and stigma and horror of HIV and AIDS came together to demand that the response go beyond clinics, hospitals and the formal health service.
Embracing and expanding the concept of partnership was revolutionary, not for AIDS but also in the broader development sphere. Partnerships continue to be central to the AIDS response. Coordination and collaboration across a wide range of partners, including sex workers, scientists and social workers, helps to identify and use expertise more effectively, overcome barriers more quickly and allocate resources more efficiently. Partnerships increase awareness and knowledge and create a critical mass of power and support that help to influence policy-makers and spur stakeholders to take action.
The story of the Sundown Clinic in Quezon City in the Philippines embodies SDG 17—strengthen the means of implementation and revitalize the global partnership for sustainable development. The success of the original clinic and the subsequent addition of two more clinics demonstrate how inclusivity continues to define the AIDS response and provide the inspiration for successful partnerships between a wide diversity of stakeholders.
Learn more about SDG Goal 17
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025


Update
Braving the Kokoda trail to raise HIV awareness in Papua New Guinea
03 July 2017
03 July 2017 03 July 2017The Kokoda trail winds through the Owen Stanley Range in Papua New Guinea and is billed as one of the world’s most challenging treks. Nearly 100 km long, the track goes through rugged mountainous terrain and hikers are buffeted by hot and humid days followed by intensely cold nights. Carol Habin is a member of the national organization of people living with HIV in Papua New Guinea, called Igat Hope Inc., and she decided to raise HIV awareness by hiking the trail in June. She joined a group of around 20 people from Australia, which also included HIV-positive people.
“As a woman who works in HIV advocacy programmes, I have come to realize that women are vastly underrepresented in my country,” said Ms Habin. “Violence against women in Papua New Guinea is extremely high. I wanted to walk the trek to not only raise awareness about HIV stigma and discrimination, but also to empower women living with HIV and to make sure their voices are heard.”
The initiative Ms Habin joined was led by the HIV Foundation of Queensland under the Kokoda+Stronger Than You Think project. UNAIDS supported the mobilization of resources for Ms Habin’s participation in the trek. The team was led by Ji Wallace, who is an Australian living with HIV and an Olympic athlete.
“With a lot of work, we can change the attitude of the community,” said Mr Wallace. “It may not happen overnight, but we have the power within us to change.”
The trekkers took eight days to complete the hike. They conducted HIV awareness sessions with people living in villages along the track.
“I was surprised to find out how little the villagers knew about HIV,” said Ms Habin. “This initiative was very helpful in getting them to understand people living with HIV. I think also thanks to media coverage we have helped transform the way the public views HIV-positive people. I’ve shown everyone that as a woman living with HIV I can do anything, even hike one of the world’s toughest trails.”
Papua New Guinea has the largest HIV epidemic in the Pacific Islands. In 2015, there were 40 000 people living with HIV in the country and 2700 new HIV infections. The country is one of the few in the Asia and the Pacific region in which women are at higher risk of HIV than men, with 56% of new HIV infections occurring among women.
“I particularly want young women to understand they can say no to sex and stand up for their rights,” said Ms Habin.
The hikers completed the hike in late June and returned to Port Moresby for a celebration. UNAIDS Papua New Guinea Country Director David Bridger congratulated the team.
“Papua New Guinea has made immense progress in its HIV response,” said Mr Bridger. “But until the fear that generates misconceptions and breeds stigma is overcome, the AIDS epidemic will continue to claim lives. The Kokoda+Stronger Than You Think initiative is an innovative way to help break down misconceptions and celebrate the strength of people living with HIV. I congratulate your efforts.”
Ms Habin plans to build on the initiative and work with the Government of Papua New Guinea to encourage more people to take HIV tests and adapt HIV prevention to the needs of young women.
Region/country
Related


Feature Story
How do you do it? Australian HIV campaign puts emphasis on a combination of ways
05 April 2017
05 April 2017 05 April 2017Meet Tom, Dick and Harry. Sydney-based health promotion organization ACON’s current campaign singles out different men who “do it”, but who opt for different ways of protecting themselves. Australia’s largest lesbian, gay, bisexual, transgender and intersex (LGBTI) people organization aims to stay in step with its community by redefining HIV prevention.
“We all have notions of what safe sex means, but we wanted to reflect actual behaviour among gay men and other men who have sex with men,” said ACON Chief Executive Officer Nicolas Parkhill.
Safer sex now means condoms, pre-exposure prophylaxis (PrEP), an undetectable viral load or a mix, he explained.
“ACON’s challenge was going from the tried and true condom reinforcement only image to a much more complex combination prevention message,” Mr Parkhill said.
The campaign also stresses the importance of respecting a partner’s choice. “There should be no shaming of people who still use condoms,” Mr Parkhill said. In addition, he says, the combination prevention message speaks to people who are HIV-negative and people living with HIV.
In the campaign video, three men explain how they practise safer sex. One “does it all the time” and opts for condoms, while another says he “does it daily” by taking antiretroviral medicines and achieving an undetectable viral load. A third “does it every day” by taking a daily dose of PrEP.
The scenarios are based on men within the community, but ACON gave them the Tom, Dick and Harry placeholders of unspecified people. The AUS$ 500 000 #YouChooose campaign includes posters, billboards, videos, on-the- ground events and materials distributed to health clinics.
In existence for more than 30 years, ACON’s aim is to end HIV transmission among gay men and other men who have sex with men and promote the health of LGBTI people and people living with HIV. The organization is primarily funded by the New South Wales Government and works closely with the New South Wales Ministry of Health.
“The government values the voice of the lesbian, gay, bisexual, transgender and intersex community in helping define what the HIV response needs to look like,” Mr Parkhill said.
UNAIDS Deputy Executive Director Luiz Loures agrees. “Communities need to be at the centre of initiatives for success in HIV prevention and ACON in Australia is putting key populations exactly at the centre,” he said.
And by having the community involved, Mr Parkhill says, the campaign goes beyond posters on bus shelters. “We are building a movement for gay men and the broader lesbian, gay, bisexual, transgender and intersex community that believes we can put HIV behind us, and we have the science and technology available to do that.”
Community organizations look to UNAIDS for leadership and direction. The 90–90–90 targets provided ACON with the political leverage needed in Australia to engage with members of parliament to reshape and reenergize the direction of HIV testing, treatment, care and support. This provided it with the evidence and information that laid the foundation of its campaign to end AIDS.
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025

Feature Story
New survey finds high levels of HIV discrimination in Republic of Korea
22 June 2017
22 June 2017 22 June 2017N.C. Cho started feeling run down, with muscle aches and a high fever, in 2014. At the time, he was 32 years old and working in the fashion industry in Seoul, Republic of Korea.
“I went to several hospitals, but nobody could come up with a diagnosis,” said Mr Cho. “Finally, I went to see a third doctor, who did a whole series of tests.”
Little did he know that among the battery of blood work, he was also being tested for HIV.
“I was really angry when the doctor came back and told me I had HIV,” said Mr Cho. “I was educated enough to know that such tests should not be conducted without my consent. “The doctor basically told me you may be able to stay healthy, but you could also get very sick, lose a lot of weight and then die. He gave me some medicine for a cold and made it pretty clear that I should not come back.”
Mr Cho was active in Seoul’s gay community and could turn to peers who introduced him to quality HIV services. He was able to access HIV treatment shortly after his diagnosis and is now feeling fine.
A new survey conducted by the Korean Network of People Living with HIV/AIDS (KNP+) finds that Mr Cho’s experience is far too common for people living with HIV in the Republic of Korea. The Korean People Living with HIV Stigma Index, which is the first peer-led survey in the country to detect and measure how HIV-positive people experience stigma and discrimination, was released on 22 June. Its development was supported by the Global Network of People Living with HIV, the International Community of Women Living with HIV and UNAIDS.
The survey, which was conducted from March to June 2016, found that 62% of people questioned reported that they were tested for HIV without their knowledge. This is high compared to other countries in Asia that have conducted similar peer-led surveys. In Viet Nam, 13% of people living with HIV reported similar experiences and in Nepal the figure was 9%. In addition, 17% of people surveyed in the Republic of Korea said their status was disclosed by medical staff to others without their consent.
“For too long, the voices of people living with HIV have been absent in policy-making,” said Son Mun Soo of KNP+. “This study documents their experiences and shows that the government, employers, health-care workers and communities must do much more to guarantee the rights of people living with HIV. A comprehensive anti-discrimination law must be enacted to protect their rights.”
UNAIDS and the World Health Organization strongly recommend that HIV testing only be undertaken with a person’s informed consent.
“Health-care settings should be stigma-free environments that ensure people living with HIV not only stay healthy, but their loved ones and community are also protected from HIV,” said Steve Kraus, Director of the UNAIDS Regional Support Team for Asia and the Pacific. “It is imperative that we have protective laws and empowered communities.”
The study found that while the general level of education of survey respondents was slightly higher than that of the general population, their employment was more precarious. Only 43% of respondents were full- or part-time employees and 42% were living on less than the Republic of Korea’s minimum household income. About one in 10 respondents who were full- or part-time employees said they had disclosed their HIV status to their employer and about half reported discriminatory reactions.
The survey found that while most respondents disclosed their HIV status to their families out of a sense of obligation, almost 40% reported isolating themselves from loved ones because of their HIV status. Self-stigma was also high among respondents, with 75% feeling self-blame and more than a third experiencing suicidal thoughts.
As the first research of its kind into the stigma and discrimination experienced by people living with HIV in the Republic of Korea, KNP+ views the Korean People Living with HIV Stigma Index as a positive step forward to ensuring that the rights and needs of people living with HIV are protected and met. The study calls for more research on how to strengthen anti-discrimination protection in the workplace and demands training for health-care providers that emphasizes the rights of patients, as well as strong measures and penalties to prevent patient privacy violations.
Mr Cho participated in the study as a peer educator and found the experience empowering.
“There is a lot of self-stigma among people living with HIV,” said Mr Cho. “So I try to portray a positive outlook. I want others to feel positive about their life and to know that they can be HIV-positive but continue to live their life to the fullest.”
UNAIDS is working to empower people living with, at risk of and affected by HIV to know their rights and to access justice and legal services to prevent and challenge violations of human rights.
Related






Feature Story
Community groups are reducing stigma in health-care settings in Asia
26 May 2017
26 May 2017 26 May 2017Dy Sokha has a ready smile and calls out friendly greetings to doctors, nurses and patients as she walks through the bustling hallways of the Khmer Soviet Friendship Hospital in Phnom Penh, Cambodia. She is brightly dressed in a peach pink shirt and is a full-time counsellor with the ARV Users Association (AUA), a community-based organization providing services to people living with HIV.
“Sometimes at the beginning of a counselling session, the client won’t look at my face,” said Dy Sokha. “They put their face down; they scratch their fingernails. They are so shy. For these difficult cases, I must open up about myself.”
Dy Sokha was diagnosed with HIV about 20 years ago and began taking antiretroviral medicine in 2004. The HIV treatment improved her health significantly and now gives her the strength to lead a busy life as a counsellor.
“I have become a role model for my clients, as they can see I am successful and they understand that just because you have HIV, it does not mean you have to disappear from society,” she said.
AUA, which is active in seven hospitals in two provinces, is one of a few community-based HIV organizations in Cambodia whose staff work directly alongside health-care providers. While the organization provides a range of services, such as counselling on treatment adherence and HIV prevention, it places a particular focus on preventing stigma and discrimination in the hospitals in which it works.
Eighty-five per cent of AUA’s 40 staff members are people living with HIV and so they know first-hand how discrimination can lead to social isolation and negatively affect a person’s health and well-being. The group facilitates connections between clients and health-care providers and holds regular meetings with hospital staff to provide feedback.
“We coordinate with different stakeholders to meet and encourage communication between people living with HIV, service providers and civil society,” said Sienghorn Han, Executive Director of AUA.
In 2015, AUA was trained by Asia Catalyst to document human rights violations in health-care settings. The cooperation was part of a study that Asia Catalyst conducted in four countries in Asia, which found discrimination evident in many areas, from denial of services and segregation to arbitrary additional fees for health services.
When AUA receives a discrimination case, it acts as a mediator, trying to find a solution that is acceptable to both health-care workers and clients.
“We keep good contact with all levels of the hospital,” said Dy Sokha. “The staff and I sit together—the doctor, the client and myself—to understand the problem in order to help the doctor do his or her best.”
AUA also holds counselling sessions with clients that aim to give them accurate information, as well as empower them to advocate for their rights and negotiate with health-care providers.
Bopha, who prefers to use a pseudonym and is living with HIV, found that AUA was especially helpful when she became pregnant in 2013. “AUA explained everything, especially how to take care of my pregnancy and how to disclose my HIV status to my doctor so that I could access antiretroviral medicines to prevent the transmission of HIV to my daughter,” she said.
Cambodian health officials acknowledge that AUA provides services that help busy health-care workers. Ngauv Bora, Deputy Chief, Technical Bureau of the National Centre for HIV/AIDS, Dermatology and STDs, said, “For clients, AUA staff are like friends and they trust them more than the hospital counsellors. AUA is helping to create an enabling environment.”
The organization is one of more than a dozen community groups that, along with health officials and international experts from 12 countries, participated in the first Asia Regional Consultation on Addressing HIV-Related Stigma and Discrimination in Healthcare, which took place on 25 and 26 May in Bangkok, Thailand.
The regional consultation provided a platform for countries to achieve tangible objectives, with technical assistance from partners. Community organizations were recognized as crucial partners in the drive to eliminate stigma and discrimination.
UNAIDS is working with countries to empower people living with, at risk of and affected by HIV to know their rights and to access justice and legal services to prevent and challenge violations of human rights.
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025



