Cosponsors


Feature Story
Heads of H6 agencies embrace new results framework
07 May 2018
07 May 2018 07 May 2018Around the world, many women, children and adolescents still have little or no access to quality health services and education, clean air and water, adequate sanitation and good nutrition. And far too many face violence and discrimination, unequal access to power and opportunity, and numerous barriers that harm their physical, mental and emotional health and well-being.
To accelerate change, the executive heads of the H6 partnership met on the sidelines of the United Nations System Chief Executives Board in London, United Kingdom, on 2 May and agreed a new results framework, H6 Results 2020. H6 Results 2020 aims to shape the H6 partnership into a trusted, valued source for technical support, strategic policy advice and best practices for the health and well-being of women, children and adolescents.
Developed under the chairpersonship of UNAIDS Executive Director Michel Sidibé, H6 Results 2020 is closely aligned with the Every Woman Every Child Every Adolescent Global Strategy and the 2020 Every Woman Every Child Partners’ Framework. H6 Results 2020 sets ambitious goals while committing to deliver on a number of concrete results for 2020.
“I am excited about our revitalized H6 partnership. As the technical arm of the Every Woman Every Child movement, we plan to further streamline and simplify the health architecture, coordinating with key partners to leverage political capital, technical expertise and advocacy for results for women, children and adolescents everywhere,” said Mr Sidibé.
Taking forward the vision endorsed by the executive heads in March 2018, H6 Results 2020 builds on the achievements of the H6 to date and reinforces existing mechanisms while strengthening United Nations mechanisms to support countries. It outlines how the H6 will harmonize efforts of the six H6 organizations and with key partners at the country, regional and global levels and will focus on the countries with the highest burdens of maternal, child and adolescent mortality and morbidity for intensified action.
“The H6 partnership plays a critical role in ensuring that countries focus on the health needs of women in an intersectional way, with laser-like focus on gender equality, human rights and other enablers, such as education,” said Phumzile Mlambo-Ngcuka, the Executive Director of UN Women.
By amplifying its added value, the H6 partnership seeks to serve as a living laboratory for United Nations reform—heeding the call of the United Nations Secretary-General for a more country-focused, coordinated, efficient and accountable development system better able to assist countries in implementing the 2030 Agenda for Sustainable Development.
“It is important that the United Nation comes together to focus its technical support on key priorities in a few high-burden countries, and what must drive our focus is results for people,” said Tedros Adhanom Ghebreyesus, the Director-General of the World Health Organization.
While committed to driving progress across a range of priorities for women, children and adolescent health, H6 Results 2020 puts clear emphasis on reaching adolescents. Adolescent girls and boys (aged 10–19 years) remain a particularly underserved population by the health and social programmes of many countries. Ensuring the health and well-being of adolescents is critical to delivering on the mandate of each of the H6 partners.
“The H6 partnership has proven that working in close collaboration and bringing different expertise and experience to the table is not only effective in enabling countries to deliver rights-based quality care for the women and girls left furthest behind, but also ensures strong country ownership,” said Natalia Kanem, the Executive Director of the United Nations Population Fund.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025



Feature Story
A united rallying cry: Time to make health care systems more flexible and innovative
16 April 2018
16 April 2018 16 April 2018Seven months after launching the catch-up plan in western and central Africa, progress on increasing the numbers of people on antiretroviral treatment continues to lag in the region. Many countries will not reach key targets by 2020 if the current systems remain unchanged.
"Overall we saw a 10% percent increase of people on treatment, which is not enough," said UNAIDS Executive Director Michel Sidibé. "Now, there is even more a sense of urgency."
Mr Sidibé, however, pointed to the success in the Democratic Republic of Congo where there was a clear increase in the number of people living with HIV accessing ARVs. The reasons for the positive trend included civil society and political leadership working closely together as well as community HIV testing and the training of 11 000 health care workers.
"More than ever there is a need to rethink health systems and alternatives for people to access health care," he said.
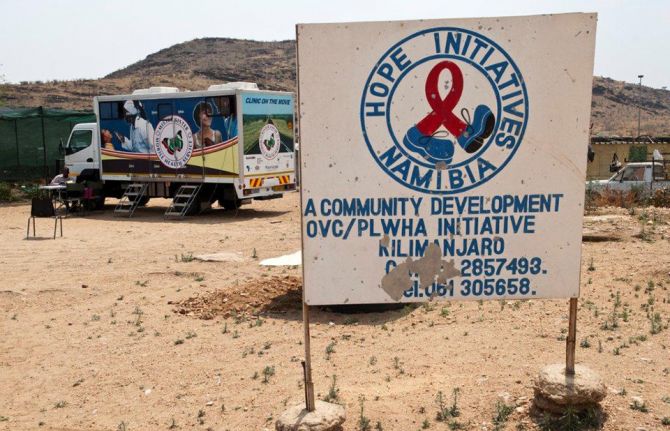
The call to delegate patient care to communities was a major rallying call during AFRAVIH, the international francophone HIV and hepatitis conference held in Bordeaux, France, early April. Mr Sidibé briefly shared the stage at the opening ceremony with the civil society organisation Coalition PLUS. They declared that the key to success in ending AIDS involved joining forces between doctors and community health workers and giving more leeway to communities to respond to the local needs of their own people.
Under the banner, "De-medicalize" the organisation explained that doctors will never be replaced but that there were too few of them and people living with HIV didn't require acute care.
Coalition Plus' recent report states that governments and the medical practitioners should delegate more tasks to nurses and community health workers. In addition to allowing for more targeted prevention and faster access to treatment, delegation of non-medical tasks would lighten the load on overburdened health systems. West and central Africa represent 17% of the total population living with HIV but 30% of deaths in the region are from AIDS-related illnesses. This is a region, according to UNAIDS and its partners, that can truly benefit from community models of care.
What worries Médecins Sans Frontières (MSF) is the risk of a significant drop in resources for treatment will hamper recent improvements in west and central Africa. This concern stems from the fact that Global Fund estimates a 30% drop in fund allocations to the region for 2018 – 2020 compared to signed HIV grants in the previous allocation period. In 2016, MSF was among the first to sound alarm bells regarding the region's high HIV death toll and the up to 80% of children unable to access antiretroviral therapy. MSF HIV Policy Advisor and Advocacy Officer Nathalie Cartier said that they supported the west and central Africa catch-up plan but that it needed to be fully implemented. "Political will has been promising but now it's time to make it a reality on the ground so that people living with HIV can reap the benefits," she said.
Global Fund supported the catch-up plan and works closely with countries in order to maximize the impact of the investments. They believe that leveraging additional domestic financing for health is crucial to increase country ownership and build sustainable programs.
All the more reason to decentralize healthcare systems and capitalize on innovations to keep health costs down. HIV self-testing, new medicines and high impact strategies involving communities are critical to improving efficiencies. "With point-of-care (POC) testing in communities and homes, delays are minimal between diagnosis and initiating treatment," said Cheick Tidiane Tall, Director of Réseau EVA, a network of pediatric doctors specialized in HIV care. “In the long run, that's a lot of people and resources saved,” he added.
Côte d'Ivoire Infectious and Tropical Diseases professor Serge Eholié couldn't agree more. "Flexible health care systems capitalizing on various innovations makes a lot of sense," he said. Turning to the Minister of Health in the Central African Republic, Pierre Somse, he asked, 'How do you respond?'
Mr Somse, also a trained doctor, said, "We doctors will stay doctors. However, there is a need for us to lean on communities and vice versa." He added, "at the heart of the issue are patients and they are and should always be the priority."
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


Feature Story
H6 commits to accelerate results for health
26 March 2018
26 March 2018 26 March 2018The H6 combines the strengths of six international organizations to help countries to realize the United Nations Secretary-General’s Every Woman Every Child strategy. The partnership mobilizes political commitment and resources to transform societies so that women, children and adolescents can realize their rights to the highest attainable standards of health and well-being.
High-level representatives of the six organizations met in New York, United States of America, to shape a shared vision for the H6. During the meeting, which took place on 21 March, health leaders committed to jointly deliver more and faster results in countries.
The Chair of the H6, Michel Sidibé, shared his vision for the partnership, including how it can evolve to meet the demands of the Sustainable Development Goals, including in humanitarian settings, and be a leading platform to advance United Nations reform.
“As a transformative platform, I see the H6 as an outstanding opportunity to rapidly bring United Nations reform to life and deliver results for every woman, child and adolescent on the ground,” said Michel Sidibé, Executive Director of UNAIDS.
The participants were united in their ambition to make the H6 a one-stop shop for countries for strategic policy advice, technical assistance and strategic information. Adolescent health, particularly for 10–18-year-olds, was discussed as a key focus area.
“I see an effective H6 partnership as an important way to drive health impact at the country level for all children, including by better addressing gaps in services for the age group from 10 to18 years old, and by planting the seeds of development in humanitarian contexts,” said Henrietta Fore, the Executive Director of the United Nations Children’s Fund.
The participants also committed to ensure policy-making in which communities have a voice and decided to build innovative partnerships with stakeholders beyond the United Nations.
Enhanced transparency and accountability of the H6 and reducing fragmentation and duplication in the United Nations system, as well as between the United Nations and the World Bank, will be key to success, as will a strong focus on joint reporting of results. The H6 will also work in close collaboration with the Global Financing Facility and the Partnership for Maternal, Newborn & Child Health.
“The United Nations Population Fund is strongly committed to the H6 partnership, which has proven that working in close collaboration and bringing different expertise and experience to the table is not only effective in enabling countries to deliver quality care for the women and girls left furthest behind, but also ensures strong country ownership,” said Natalia Kanem, the Executive Director of the United Nations Population Fund.
The H6 principals will now develop a results framework and reconvene in May to review and endorse it. They are aiming to adopt a road map to roll out new ways of working by mid-year.




Feature Story
Africa’s welcome mat: stories of hope and resilience from refugees in Uganda
29 March 2018
29 March 2018 29 March 2018“Right now, I just want to go to a country where there is peace,” says a young student who fled the conflict in his home country, the Democratic Republic of the Congo. His new home is Kyangwali Refugee Settlement Area in the Hoima District of Uganda—the place that will give him a chance to fulfil his dream of a peaceful life.
The Kyangwali Refugee Settlement Area lies on the banks of Lake Albert on the border between southern Democratic Republic of the Congo and northern Uganda. Most of the refugees in Kyangwali are fleeing interethnic conflict in eastern Democratic Republic of the Congo and making the perilous journey into Uganda on fishing boats across Lake Albert. Since January 2018, approximately 59 000 people have made the crossing. On a normal day 500 refugees arrive; on a busy day it can be as many as 2000.
Families arrive with whatever personal belongings they can carry—from mattresses and cookware to valuables, such as solar panels, piled high among the passengers in the boats. The boat ride can take as little as six hours if people travel in a motorized vessel or as much as 12 hours if they travel by canoe. “Boats sometimes run out of fuel in the middle of the lake and Ugandan marine police have to bail them out,” says Bornwell Kantande, Representative of the Office of the United Nations High Commissioner for Refugees in Uganda. “Other boats have capsized from overloading—at the peak of the influx of refugees as many as 200 people would pile onto a single canoe.”
Upon arrival at the Kyangwali reception centre, refugees are registered by aid workers and given a wristband for identification purposes. They receive high-energy biscuits and water and those who need it are given emergency health care. Refugees stay at the reception centre for a day or two before being transported to the settlement area, where they are allocated a small plot of land and material and equipment to build temporary shelter while they establish themselves.
In a recent visit to the reception centre, Michel Sidibé, UNAIDS Executive Director, witnessed first-hand the health services that are offered to newly arrived refugees at its small makeshift clinic. Here refugees obtain access to emergency health care and are informed about the minimum initial service package for reproductive health, which they receive throughout the different phases of new arrival: border crossing; the short stay at the reception centre; before transportation to the settlement area; and during settlement. Services include HIV testing and tuberculosis screening, prevention of mother-to-child transmission of HIV services, provision of HIV and tuberculosis treatment to people already on it and other sexual and reproductive health services.
During his visit, Mr Sidibé listened to the stories of many refugees, who told him not only of the impact that dislocation has had on their health and their lives, but also of their aspirations and dreams to make a better life for themselves and their families. “I heard stories of sadness, but also of hope and resilience,” says Mr Sidibé.
Uganda is home to the largest refugee population in Africa, with a population of almost 1.4 million refugees in 13 refugee settlements across the country. The majority of refugees are from South Sudan and the Democratic Republic of the Congo, the latter of which has close to five million displaced people—almost as many as in the Syrian Arab Republic.
“It is beyond admirable to selflessly offer refuge to hundreds of thousands of women, children and men who are in need of international protection,” remarked Mr Sidibé. “Uganda’s refugee policy is among the most progressive in the world and is a model for other countries to emulate.”
Region/country
Related


Feature Story
Partnership connects African law schools to the AIDS response
26 February 2018
26 February 2018 26 February 2018Stigma and discrimination, especially against women and girls and key populations, is a major barrier to people using HIV services. Up to 60% of countries report having laws, regulations or policies that deter people in key populations from being able to protect themselves from, or get treatment for, HIV.
There is therefore a need for legal services to challenge stigma and discrimination, but in many parts of the world such services are absent. Since teaching in law schools is often focused on core subjects, such as constitutional, administrative and criminal law, that often do not address legal issues related to HIV, most lawyers lack the specialized knowledge they need to take on HIV-related stigma and discrimination cases.
Academics sometimes need to give advice on key HIVrelated legal issues, such as the criminalization of HIV transmission. It is therefore important that they understand why human rights are essential to the response to HIV.
To respond to this lack of HIV-related legal knowledge, a unique pilot project has been set up with the law schools of the Universities of Dar es Salaam and Dodoma in the United Republic of Tanzania and Makerere University and Uganda Christian University in Uganda. The project will strengthen the legal environment for the response to HIV and give academics and students the skills they need to support human rights-based responses to HIV. It will also increase awareness in order to encourage communities to seek support from legal clinics.
“By training a committed and well-informed future generation of lawyers on HIV and the law and informing people about their rights, UNAIDS hopes to strengthen a human rights-based response to HIV in the United Republic of Tanzania and Uganda,” said Michel Sidibé, Executive Director of UNAIDS.
The project is the result of an agreement signed in 2014 by UNAIDS and the International Development Law Organization (IDLO) to scale up efforts towards zero HIV-related discrimination. The project is part of a collaboration that started in 2009 to strengthen and expand legal services for people living with HIV and key populations.
“HIV is not just a health issue, but a matter of social justice. It’s crucial that we equip the next generation of African lawyers with the knowledge and skills to effectively respond to HIV and end discrimination,” said Irene Khan, Director-General of IDLO.
The project will also see legal handbooks being developed for both the countries, which will serve as guidance on HIV and the law for students, lawyers and community leaders. The handbooks will consider HIV epidemiology in the region, the social and legal factors that contribute to HIV vulnerability, jurisprudence and common legal issues faced by people living with HIV and key populations. They will also give legal and non-legal options to address these issues.
“The project has exposed our students to new skills in responding to the challenges facing people living with HIV. The legal clinic now has the necessary skills to provide services to people living with HIV in Dodoma,” said Nicodemus S. Kusenha, a Lecturer at the University of Dodoma in the United Republic of Tanzania.
A UNAIDS, United Nations Development Programme and IDLO collaboration that started in 2009 has provided technical and financial support to HIV-related legal services in 18 countries and produced a publication on scaling up HIV-related legal services and elearning courses in four languages.
“Through an interaction with people living with HIV and key populations, we have been able to draw links between the theory of health law as we teach it and the beneficiaries of the law. This project has therefore made our teaching of the law more meaningful and with a human face,” said Zahara Nampewo, a Lecturer at Makerere University in Uganda.


Press Statement
UNAIDS welcomes appointment of Henrietta Holsman Fore as Executive Director of UNICEF
23 December 2017 23 December 2017GENEVA, 23 December 2017—UNAIDS warmly welcomes the announcement by the United Nations Secretary-General that Henrietta Holsman Fore has been appointed as the new Executive Director of the United Nations Children’s Fund (UNICEF). Ms Fore is a champion of economic development, education, health and humanitarian assistance and was the first woman to serve as the Administrator of the United States Agency for International Development and as the Director of United States Foreign Assistance.
“We look forward to working closely with Henrietta Holsman Fore and continuing to collaborate with UNICEF on our common goals—stopping new HIV infections among children, ensuring access to HIV treatment and making sure that children living with and affected by HIV get the care and support they need,” said Michel Sidibé, Executive Director of UNAIDS.
UNICEF is a founding Cosponsor of UNAIDS and in 2011 joined UNAIDS, the United States President’s Emergency Plan for AIDS Relief and other partners to develop the Global Plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive. The plan helped to significantly reduce new HIV infections among children in the countries most affected by HIV.
From 2010 to 2016 there was a 56% decline in new HIV infections among children in eastern and southern Africa. However, access to treatment for children continues to lag behind. Globally, just 43% of children living with HIV had access to life-saving antiretroviral therapy in 2016, compared to 54% of adults.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
UNAIDS Cosponsors




Feature Story
Early infant diagnosis of HIV: changing lives for mothers and infants
07 December 2017
07 December 2017 07 December 2017Mahabad Asanova’s first daughter was found to be living with HIV after being rushed to hospital with a high fever. For her second pregnancy, Ms Asanova had to wait 18 months before finding out that her son was HIV-negative.
By the time of her third pregnancy, however, things had changed dramatically. Within a month of her birth, Ms Asanova had been told that her daughter was HIV-negative. A revolutionary method of HIV testing of infants, dried blood spot (DBS) testing, had by then been introduced, significantly cutting the time for diagnosis.
“Waiting 18 months to know about the HIV status of my child was terrible,” Ms Asanova said. “I’m so relieved—dried blood spot testing completely changed my life.” Before DBS, children had to wait a year or more to be tested.
DBS is simple: no sophisticated equipment or invasive testing methods are needed. After a prick on the newborn’s heel, a drop of blood is collected on filter paper and dried. The sample is sent to a laboratory for testing and the results are known before the infant is a month old, allowing infants living with HIV to be treated immediately with life-saving antiretroviral medicines.
“Before dried blood spot testing was widely introduced in 2013 in Kyrgyzstan, only around 15% of infants were diagnosed early,” said Edil Tilekov, HIV Programme Officer for the United Nations Children’s Fund (UNICEF). “In 2017, that figure grew to nearly 90%.”
Today, HIV science and diagnostics are becoming ever-more sophisticated. UNICEF is promoting point-of-care HIV diagnostic methods for infants that would yield an HIV diagnosis a mere two hours after collecting blood.
The introduction of DBS and improved training for doctors has helped to defuse some of the stigma against people living with HIV.
“Stigma among medical staff began to decrease as antiretroviral medicines were integrated into the primary health-care system,” Elmira Narmatova, Director of the Osh Oblast AIDS Centre, said. “It became more like a chronic disease, mortality declined.”
Children who are treated early fare better and the more the medicines work, the more confident parents become. Today, in part as a result of DBS, more than 95% of children living with HIV in Osh, Kyrgyzstan, access antiretroviral therapy.
Yet pockets of resistance remain. Despite early diagnosis, not all infants receive the medicines they need. “We are interviewing parents and medical staff to find out why some parents still don’t want to give their infants antiretroviral medicines,” said Mr Tilekov.
Informal conversations already provide clues: resistance may be due to religion, to scepticism about immunization or even to urban myths.
“Although much has been done to provide parents with information and train medical staff, there is still a lack of resources and trained personnel, so some parents will slip through the net and might not be briefed properly about side-effects,” said Mr Tilekov. “So, if their infants lose weight or don’t eat well after starting antiretroviral therapy, parents blame the medicines.”
When an infant or mother is tested for HIV in Osh, the laboratory sends the results to the Osh AIDS Centre, a pleasant house set among trees in a leafy suburb, its gates open in welcome. The hallways are decorated with images of the popular Vitaminka fairy tale, a comic strip that helps health workers and parents explain to children the importance of taking their antiretroviral medicines regularly.
By providing child-friendly spaces and psychosocial support in addition to medical treatment, the centre makes parents feel welcome and encourages them to visit, pick up prescribed medication and get tested regularly.
The centre, upgraded by the Ministry of Health together with UNICEF and UNAIDS with support from the Government of the Russian Federation, now treats more than 200 children and a psychologist provides psychosocial support to children living with HIV.
Away from social pressures and among friends, parents can exchange hopes for the future and find much needed support at the centre.
Ms Asanova looks relaxed as her fingertips touch across her lap, her olive-green dress contrasting with her cream-coloured hijab. Mahabad Asanova isn’t her real name, since she still worries about stigma and discrimination beyond the centre’s walls. But she isn’t afraid anymore, even though she is now expecting another child. Whatever happens, thanks to DBS, she will no longer face painful months of waiting for a diagnosis.
Related
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025

Feature Story
In Mozambique, five adolescent and young girls receive a special award on World AIDS Day for winning the SMS BIZ/U-Report Girl-to-Girl competition
06 December 2017
06 December 2017 06 December 2017This story was originally published by UNICEF
In Mozambique there has been some progress in the fight against AIDS, notably in preventing mother to child transmission of HIV. But progress in preventing new HIV infections among adolescents (10-19) and improving testing and treatment in adolescent populations are still unacceptably slow.
Around 120,000 adolescents live with HIV (UNAIDS 2017). The data also reveals a worrying gender disparity: according to IMASIDA 2015, HIV prevalence among adolescent girls 15-19 is four times higher than for boys (6.5% vs 1.5%). Prevalence is also higher in urban areas than in rural. Young women have higher odds of HIV infection due to various factors including gender norms, reduced access to information, and age-disparate sex. Additionally, not knowing one’s HIV status and engaging in high risk practices predisposes young people to the risk of contracting HIV. This highlights the need for adolescents and young people to have access to appropriate information as they explore their sexuality.
The AIDS epidemic must remain a global public health concern, according to UNICEF and UNAIDS. Innovative solutions must be adopted to speed up progress in preventing HIV infection of children and adolescents and ensuring those living with HIV get the treatment they need.
In 2015, in the context of the youth-focused Sexual and Reproductive Health (SRH) and HIV prevention Geração Biz (Busy Generation) programme, UNICEF Mozambique partnered with line ministries of Youth and Sports; Health; Education and Human Development; UNFPA and the youth association Coalizão (Youth Coalition) to adapt the SMS-based technology for development platform U-Report and roll out the programme known as SMS BIZ. This was aimed at improving adolescent and young people’s access to comprehensive and personalised SRH and HIV information through SMS (for more information visit http://mozambique.ureport.in/).
SMS BIZ partners set up a counselling hub managed by Coalizão with 24 trained peer counsellors, equipped with ICT facilities and a reference guide on SRH, HIV and Gender-based Violence (GBV) prevention to facilitate their capability to respond to adolescents queries. The counseling service is totally anonymous so neither the counsellors nor users can identify the other. Counsellors respond to about 1,000 questions daily. A total of 350,000 questions were responded to date. Communication and promotion materials were developed to promote the counselling service while advocacy sessions were held in selected provinces in order to create synergies with different stakeholders. Partnerships with the three Telecom Operators allowed SMS BIZ partners to count on free un-limited SMS for the period of 2017-2020.
In only two years, SMS BIZ/U-Report, has exceeded expectations with over 110,000 active adolescents and youth registered by September 2017, using the services for information on topics relevant to them.
Adolescents and young people registered have been engaged in discussions addressing misconceptions about SRH, HIV prevention and treatment, and increasing uptake and linkages to HIV and GBV services. Results from a poll show positive results, with 65% of adolescents and young people that responded to the poll were referred and adhered to health facilities during the counselling session for additional individual face-to-face counselling, consultation or treatment.
However, until recently, the challenge has been attracting as many girls as boys to the platform with a ratio of 60% boys - 40% girls. Raima Francisco Manjate, one of the SMS BIZ/U-Report stellar peer counsellors officially launched the Girl-to-Girl invite system on the International Day of the Girl Child on October 11th, with an intervention at the National Girls Conference organized in the context of the UN Joint programme Action for Girls, funded by the Swedish Government. The results have been outstanding: in 72 hours, more than 8,600 girls were successfully registered, the girls' user population grew from 4% to 44%, with five girls registering more than 50 friends and winning the competition.
Today, the total number of SMS BIZ/U-Report users reached 130,000.
The five adolescent and young girls, winners of the competition, have been awarded today at the World AIDS Day Celebrations, in Maputo and in the provincial capitals of Quelimane, Nampula and Beira in recognition of their efforts in mobilising friends to adhere to this important counselling service.
Neima Muianga, 20 years old and Cristina Djive, 18 years old, both from the capital Maputo, were the two girls awarded today at the WAD ceremony, by the following high-level dignitaries such as Mr. Carlos Agostinho do Rosario, Mozambique Prime Minister, Mr. Luiz Loures, UNAIDS Deputy Executive Director, Ms. Nazira Abdul, Health Minister and Ms. Clarisse Machanguana, UNICEF National Ambassador.
Neima was thrilled when she discovered she had won the competition: “I feel happy about it. I have sent various SMS to contact numbers on my list, my neighbours, church members and even girls or young women I would bump into in the streets. SMS BIZ is very important for us. I don’t feel comfortable speaking with my parents about sexuality as this is taboo in Mozambique”.
"It is an excellent example of how young people can empower each other through technologies and innovative projects. Girl-to-Girl (G2G) is the kind of innovation that has an essential role for gender equality and health as we work to leave no one behind in implementing the sustainable development goals," said Luiz Loures, UNAIDS Deputy Executive Director, Assistant Secretary-General of the United Nations.
Now that the SMS BIZ/U-Report initiative has been scaled up at national level, SMS BIZ partners expect to reach and engage approximately 400,000 adolescents and young people by 2020. According to Cristina “this initiative cannot stop. So far, it has been a great experience for us.”
Region/country
Related


Press Release
West and Central Africa left behind in global HIV response
05 December 2017 05 December 2017New report highlights urgent need for an improved HIV response for children and adolescents
ABIDJAN/DAKAR/NEW YORK/GENEVA, 5 December 2017 – More than four decades into the HIV epidemic, four in five children living with HIV in West and Central Africa are still not receiving life-saving antiretroviral therapy, and AIDS-related deaths among adolescents aged 15-19 are on the rise, according to a new report released today.
While acknowledging progress in several areas, the report Step Up the Pace: Towards an AIDS-free generation in West and Central Africa, jointly published by UNICEF and UNAIDS, shows that West and Central Africa is lagging behind on nearly every measure of HIV prevention, treatment and care programmes for children and adolescents. In 2016, an estimated 60,000 children were newly infected with HIV in West and Central Africa.
“It is tragic that so many children and adolescents today are not receiving the treatment they need just because they have not been tested,” said Marie-Pierre Poirier, UNICEF’s West and Central Africa Regional Director. “We need to make better use of innovations to increase early diagnosis and improve access to HIV treatment and care for children. For example, the point-of-care technology diagnostic brings testing closer to where children attend health services and self-testing can be a good option for adolescents who may be more comfortable with it.”
The region’s coverage of life-saving antiretroviral therapy among children living with HIV is the lowest in the world because many countries have limited capacity to perform the tests needed for early infant diagnosis of HIV. Without knowing a child’s HIV status, his or her family is less likely to seek the treatment that could prevent the tragedy of a child’s death from AIDS-related illnesses.
The situation is worse among adolescents. The annual number of new HIV infections among those aged 15–19 years in the region now exceeds that of children aged 0-14 years. These new infections occur mostly through unprotected sexual contact and among adolescent girls. Equally concerning, according to the report, is that West and Central Africa has recorded a 35 per cent increase in the annual number of AIDS-related deaths among adolescents aged 15-19 years — the only age group in which the number of AIDS-related deaths increased between 2010 and 2016.
With the region’s youth population expected to grow significantly within the coming decades, especially in countries like the Democratic Republic of the Congo and Nigeria, the numbers of children and adolescents becoming infected with HIV and dying from AIDS is likely to remain high, unless the HIV response – both prevention and treatment – improves dramatically.
The report highlights that the 24 countries that make up the West and Central Africa region are home to 25 per cent of children aged 0–14 years living with HIV worldwide.
“Leaders of the region have endorsed a Catch-Up plan aiming to triple the number of people on treatment in the region – including children – by the end of 2018, the key issue now is to accelerate implementation,” said Luiz Loures, UNAIDS Deputy Executive Director. “Countries should urgently put in place more effective strategies for early infant diagnosis of HIV, and start reducing inequity in children’s access to treatment.”
The report proposes key strategies that will enable countries to accelerate progress in curbing the spread of disease. These include:
- A differentiated HIV response focusing on unique epidemiological and local contexts in each country and community.
- The integration of HIV services into key social services including health, education and protection.
- Community ownership and local governance of the HIV response including working with families, better placed to help reduce stigma, access prevention and treatment.
- Investment in innovations to remove barriers to scale-up including new diagnostic and biomedical approaches such as point of care diagnostics, HIV self-testing and pre-exposure prophylaxis.
UNICEF announced last week that at the current pace of progress, the global 2020 Super-Fast-Track targets to end AIDS among children will not be achieved.
***
Key facts from the report:
- Prevention of mother-to-child transmission of HIV coverage has increased 2.5-fold between 2010 and 2016 (from 21 per cent to 49 per cent), with some countries such as Benin, Burkina Faso and Cabo Verde now providing these services to more than 80 per cent of the pregnant women living with HIV.
- West and Central Africa has the lowest paediatric antiretroviral treatment coverage in the world, with only 21 per cent of the 540,000 children (0-14) living with HIV receiving antiretroviral treatment in 2016 – compared to 43 per cent globally.
- Today, West and Central Africa accounts for 37 per cent of the world’s AIDS-related deaths among children: about 43,000 AIDS-related deaths occurred among children in West and Central Africa in 2016, a decrease of 31 per cent compared to 2010.
- There were 62,000 adolescents (15-19) newly infected with HIV in 2016, unchanged compared to 2010.
- Adolescent girls and young women continue to be the most affected, with women making up nearly three out of five of all adolescents aged 10-19 years living with HIV across West and Central Africa.
Note to editors:
The Report is available at: https://www.unicef.org/publications/index_101480.html
More information is available at: www.childrenandaids.org
About UNICEF
UNICEF works in some of the world’s toughest places, to reach the world’s most disadvantaged children. Across 190 countries and territories, we work for every child, everywhere, to build a better world for everyone. For more information about UNICEF and its work for children, visit www.unicef.org
About UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube. For more information about UNAIDS and its work, visit www.unaids.org
Contact
UNICEF West and Central Africa (at ICASA)Anne-Isabelle Leclercq Balde
tel. +221 77 740 69 14
aleclercqbalde@unicef.org
Gbolayemi Lufadeju
UNICEF New York
tel. +1 917 213 4034
glufadeju@unicef.org
Aminata Ouattara
UNAIDS (at ICASA)
tel. +221 77 498 1753
ouattaraa@unaids.org
Charlotte Sector
UNAIDS (at ICASA)
tel. +41 79 500 8617
sectorc@unaids.org
Resources
Press centre
Download the printable version (PDF)
Region/country

Feature Story
Living with HIV but dying from tuberculosis
03 November 2017
03 November 2017 03 November 2017Global progress to End TB not fast enough to reach global TB and HIV targets
Tuberculosis (TB) retains its undesirable status as the leading infectious cause of death globally. According to the latest WHO Global Tuberculosis Report 2017 launched this week, global progress in reducing new tuberculosis (TB) cases and deaths is insufficient to meet the global targets for TB and HIV, despite most deaths being preventable with early diagnosis and appropriate treatment of tuberculosis and HIV.
As part of global efforts to advance the response to TB is now being pushed higher up the global development agenda with hundreds of global leaders attending the first WHO Global Ministerial Conference on Ending TB in Moscow from 14-17 November and a dedicated United Nations General Assembly High-Level Meeting on TB in 2018.
“We have an unprecedented opportunity to shine the political spotlight on the inequalities that drive the epidemics of TB and HIV,” said Michel Sidibé, UNAIDS Executive Director, “The return on investment in TB and HIV is more than just dollars, it's in voices heard, rights protected and lives saved.”
In 2016, the risk of developing TB disease among the 37 million people living with HIV was around 21 times higher than the risk in the rest of the world population. There were more than one million TB cases among people living with HIV—10% of all global TB cases in 2016. People living with HIV are much more likely to die from TB disease than HIV-negative people, and one in five (22%) TB deaths occurs among people living with HIV. In 2016, there were 374 000 TB deaths among people living with HIV, which represents almost 40% of all AIDS-related deaths.
TB disease and deaths can be avoided with TB preventive therapy but most people living with HIV who can benefit are not receiving it. In 2016, fewer than 1 million people newly enrolled in HIV care were started on TB preventive treatment. South Africa accounted for the largest share of the total (41%), followed by Mozambique, Zimbabwe and Malawi.
The global burden of drug-resistant tuberculosis continues to rise with an estimated 600,000 cases requiring treatment but only one in five were enrolled on treatment in 2016.
Global TB incidence is only falling at about 2% per year and 16% of TB cases die from the disease; by 2020, these figures need to improve to 4–5% per year and 10%, respectively, to reach the first (2020) milestones of the WHO End TB Strategy. Major gaps remain in global funding for TB prevention and treatment (US$2.3 billion) and TB research into new drugs, vaccines, and diagnostics (US$1.2 billion) for 2017.