Michel Sidibé UNAIDS Executive Director EXD






Update
Quebec parliamentarians and civil society both vital to the AIDS response
29 November 2017
29 November 2017 29 November 2017During a visit to Canada, on 28 November UNAIDS Executive Director Michel Sidibé met with members of the Government of Quebec, members of parliament and civil society at the National Assembly of Quebec.
In meetings with the Quebec Minister of Health, Gaétan Barrette, and the Deputy Minister for International Relations and the Francophonie, Jean-Stéphane Bernard, Mr Sidibé underlined that it is important that UNAIDS’ work be aligned with that of the Quebec Government and stressed the need to tailor the response to HIV in accordance with the needs of the country or region. He also spoke about the urgent need to make HIV prevention more effective and the importance of investing in HIV prevention and reducing the number of new HIV infections.
Mr Sidibé also discussed Quebec’s AIDS response and visited Point de Repères, a community-based organization that advocates for harm reduction. He met with leaders from MIELS-Québec, a community-based organization working for more than 30 years with people living with HIV, and Ruban en Route, a not-for-profit organization providing prevention education programmes designed to reduce sexual risk behaviours.
During meetings with members of Quebec’s Parliament, including with Jacques Chagnon, President of the National Assembly and President of the Parliamentary Assembly of La Francophonie, Mr Sidibé emphasized the important role that parliamentarians play in the global response to HIV. He also stressed that parliamentarians are critical to advancing the vision of ending AIDS by 2030 through their leadership, advocacy role and ability to authorize and oversee spending on AIDS.
Quotes
“The National Assembly of Quebec is a vital ally for social justice and to guarantee the right to health for all. Together we can end the AIDS epidemic by 2030.”
“The National Assembly of Quebec is pleased to contribute, to the best of its ability, to the exchange of information and experiences on best practices in the response to HIV through the Parliamentary Network for the Fight Against HIV/AIDS, which was created by the Parliamentary Assembly of La Francophonie.”
“In the framework of the 90–90–90 targets, Quebec has mobilized and made a lot of effort. Although the last percentages are the most difficult to reach, we are on the right track. We can count on invaluable partners in this regard, particularly from community organizations, as demonstrated by our recent collaboration in the implementation of supervised injection sites in Montreal.”
Region/country
Related


Press Release
On World AIDS Day, UNAIDS warns that men are less likely to access HIV treatment and more likely to die of AIDS-related illnesses
01 December 2017 01 December 2017New report from UNAIDS shows the blind spot in reaching men with HIV services
OTTAWA/GENEVA, 1 December 2017—On World AIDS Day, UNAIDS has released a new report showing that men are less likely to take an HIV test, less likely to access antiretroviral therapy and more likely to die of AIDS-related illnesses than women. The Blind spot shows that globally less than half of men living with HIV are on treatment, compared to 60% of women. Studies show that men are more likely than women to start treatment late, to interrupt treatment and to be lost to treatment follow-up.
“Addressing the inequalities that put women and girls at risk of HIV is at the forefront of the AIDS response,” said Michel Sidibé, Executive Director of UNAIDS. “But there is a blind spot for men—men are not using services to prevent HIV or to test for HIV and are not accessing treatment on the scale that women are.”
In sub-Saharan Africa, men and boys living with HIV are 20% less likely than women and girls living with HIV to know their HIV status, and 27% less likely to be accessing treatment. In KwaZulu-Natal, the province with the highest HIV prevalence in South Africa, only one in four men aged 20–24 years living with HIV in 2015 knew that they had the virus.
In western and central Africa, a region that is struggling to respond effectively to HIV, only 25% of men living with HIV are accessing treatment. When people are not on treatment they are more likely to transmit HIV.
“When men access HIV prevention and treatment services, there is a triple dividend,” said Mr Sidibé. “They protect themselves, they protect their sexual partners and they protect their families.”
The report highlights data from sub-Saharan Africa that show that condom use during sex with a non-regular partner is low among older men, who are also more likely to be living with HIV—50% of men aged 40–44 years and 90% of men aged 55–59 years reported not using a condom. These data are consistent with studies showing a cycle of HIV transmission from older men to younger women, and from adult women to adult men of a similar age in places with high HIV prevalence.
The Blind spot also shows that HIV prevalence is consistently higher among men within key populations. Outside of eastern and southern Africa, 60% of all new HIV infections among adults are among men. The report outlines the particular difficulties men in key populations face in accessing HIV services, including discrimination, harassment and denial of health services.
Men who have sex with men are 24 times more likely to acquire HIV than men in the general population and in over two dozen countries HIV prevalence among men who have sex with men is 15% or higher. However, recent studies suggest that condom use is dropping in Australia, Europe and the United States of America. In the United States, for example, the percentage of HIV-negative gay men and other men who have sex with men who engage in sex without using condoms increased from 35% to 41% between 2011 and 2014.
“We cannot let complacency set in,” said Mr Sidibé. “If complacency sets in, HIV will take hold and our hopes of ending AIDS by 2030 will be shattered.”
The Blind spot shows that around 80% of the 11.8 million people who inject drugs are men and that HIV prevalence among people who inject drugs exceeds 25% in several countries. Condom use is almost universally low among people who inject drugs and the percentage of men who inject drugs using sterile injecting equipment during their last drug injection varies from country to country. In Ukraine, for example, the percentage of men who inject drugs who used a sterile needle at last injection was well over 90%, whereas in the United States only around 35% used a sterile needle.
In prisons, where 90% of detainees are men, HIV prevalence is estimated at between 3% and 8%, yet condoms and harm reduction services are rarely made available to detainees.
While HIV testing has been able to reach women, particularly women using antenatal services, the same entry points have not been found for men, limiting uptake of HIV testing among men.
“The concept of harmful masculinity and male stereotypes create conditions that make having safer sex, taking an HIV test, accessing and adhering to treatment—or even having conversations about sexuality—a challenge for men,” said Mr Sidibé. “But men need to take responsibility. This bravado is costing lives.”
The report shows the need to invest in boys and girls at an early age, ensuring that they have access to age-appropriate comprehensive sexuality education that addresses gender equality and is based on human rights, creating healthy relationships and promoting heath-seeking behaviour for both girls and boys.
The report shows that men visit health-care facilities less frequently than women, have fewer health checks and are diagnosed with life-threatening conditions at later stages than women. In Uganda, some men reported they would rather avoid knowing their HIV status and receiving life-saving treatment because they associated being HIV-positive with emasculating stigma. One study in South Africa showed that 70% of men who had died from AIDS-related illnesses had never sought care for HIV.
The report urges HIV programmes to boost men’s use of health services and to make services more easily available to men. This includes making tailored health services available, including extending operating hours, using pharmacies to deliver health services to men, reaching men in their places of work and leisure, including pubs and sports clubs, and using new communications technologies, such as mobile phone apps.
It also urges a supportive legal and policy environment that addresses the common barriers to accessing HIV services, especially for key populations, and can accommodate the diverse needs and realities of men and boys.
The Blind spot shows that by enabling men to stay free from HIV, get tested regularly and start and stay on treatment if HIV-positive, the benefits will not only improve male health outcomes, but will contribute to declines in new HIV infections among women and girls and to altering harmful gender norms.
In 2016 (*June 2017) an estimated:
*20.9 million [18.4 million–21.7 million] people were accessing antiretroviral therapy
36.7 million [30.8 million–42.9 million] people globally were living with HIV
1.8 million [1.6 million–2.1 million] people became newly infected with HIV
1.0 million [830 000–1.2 million] people died from AIDS-related illnesses
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS CanadaSophie Barton-Knott
tel. +41 79 514 6896
bartonknotts@unaids.org
UNAIDS Geneva
Alinka Brutsch
tel. +41 22 791 1647
brutscha@unaids.org
UNAIDS Communications
communications@unaids.org
Press centre
Download the printable version (PDF)


Press Statement
World AIDS Day message from UNAIDS Executive Director
24 November 2017 24 November 20171 December 2017
Michel Sidibé
Executive Director of UNAIDS
Under-Secretary-General of the United Nations
This World AIDS Day, we are highlighting the importance of the right to health and the challenges that people living with and affected by HIV face in fulfilling that right.
The right to health is a fundamental human right—everybody has the right to the enjoyment of the highest attainable standard of physical and mental health, as enshrined in the International Covenant on Economic, Social and Cultural Rights.
The world will not achieve the Sustainable Development Goals—which include the target of ending AIDS by 2030—without people attaining their right to health. The right to health is interrelated with a range of other rights, including the rights to sanitation, food, decent housing, healthy working conditions and a clean environment.
The right to health means many different things: that no one person has a greater right to health care than anyone else; that there is adequate health-care infrastructure; that health-care services are respectful and non-discriminatory; and that health care must be medically appropriate and of good quality. But the right to health is more than that—by attaining the right to health, people’s dreams and promises can be fulfilled.
On every World AIDS Day, we look back to remember our family members and friends who have died from AIDS-related illnesses and recommit our solidarity with all who are living with or affected by HIV.
From the beginning, the AIDS response was built on the fundamental right to health and well-being. The AIDS community advocated for rights-based systems for health and to accelerate efforts for the world to understand HIV: how to prevent it and how to treat it.
Too many people—especially those who are the most marginalized and most affected by HIV—still face challenges in accessing the health and social services they urgently need. We all must continue to stand shoulder to shoulder with the people being left behind and demand that no one is denied their human rights.
This year has seen significant steps on the way to meeting the 90–90–90 treatment targets towards ending AIDS by 2030. Nearly 21 million people living with HIV are now on treatment and new HIV infections and AIDS-related deaths are declining in many parts of the world. But we shouldn’t be complacent. In eastern Europe and central Asia, new HIV infections have risen by 60% since 2010 and AIDS-related deaths by 27%. Western and central Africa is still being left behind. Two out of three people are not accessing treatment. We cannot have a two-speed approach to ending AIDS.
For all the successes, AIDS is not yet over. But by ensuring that everyone, everywhere accesses their right to health, it can be.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Press centre
Download the printable version (PDF)
Documents
World AIDS Day 2017 message by UNAIDS Executive Director
28 November 2017
Related
 Keeping up the momentum in the global AIDS response
Keeping up the momentum in the global AIDS response
24 April 2019
 Malawi launches its health situation room
Malawi launches its health situation room
12 April 2019
 Learning lessons on evaluation
Learning lessons on evaluation

02 April 2019
 UNAIDS presents a new plan to create a healthy, equitable and enabling environment for UNAIDS staff
UNAIDS presents a new plan to create a healthy, equitable and enabling environment for UNAIDS staff

01 April 2019
 UN and AU working together for sustainable development
UN and AU working together for sustainable development

27 March 2019
Let’s balance for better
12 March 2019
 International Women’s Day in Ethiopia
International Women’s Day in Ethiopia

12 March 2019


Update
Deutsche AIDS-Stiftung makes awards for outstanding contributions to the global AIDS response
15 November 2017
15 November 2017 15 November 2017Princess Mabel van Oranje-Nassau and UNAIDS Executive Director Michel Sidibé were presented with the World Without AIDS Award in Berlin, Germany, on 4 November in recognition of their achievements in the global AIDS response.
The awards were made by Deutsche AIDS-Stiftung, the German AIDS foundation, during its annual Benefit Opera Gala, which brought together 2000 guests to raise money for the AIDS response and to speak out against stigma and discrimination.
Princess Mabel van Oranje-Nassau was honoured for her almost 20-year commitment to ending AIDS. She is the Chair and founder of Girls not Brides, the global partnership to end child marriage, which consists of more than 800 civil society organizations in 95 countries.
Mr Sidibé received his award in recognition of his work to achieve the goal of ending AIDS by 2030.
During the gala, which has been raising awareness and funds for people living with HIV since 1994, Mr Sidibé highlighted the growing HIV epidemic in eastern Europe and central Asia, which saw a 60% increase in new HIV infections between 2010 and 2016. He made it clear that the shrinking space for civil society in the region will exacerbate stigma and discrimination and will drive people away from life-saving services.
Germany is a leader in global health and has consistently driven progress in the AIDS response at both the national and international levels. In 2017, the German nongovernmental umbrella organization Deutsche AIDS-Hilfe launched a campaign to end AIDS in Germany by 2020.
Quotes
“If we can keep girls in school and out of marriage and protect them from HIV infection, they will be better educated, healthier and more prosperous. And that’s not good just for those girls, that’s also good for their families, their communities and their countries. So let girls be girls and not brides.”
“We need to make the impossible possible for the most marginalized people.”
“The number of guests here today and their strong engagement proves how relevant our fight against HIV still is.”
Related


Press Release
UNAIDS announces nearly 21 million people living with HIV now on treatment
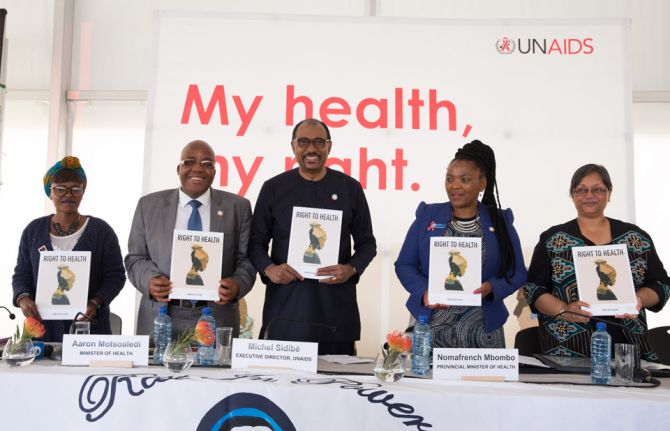
20 November 2017 20 November 2017New report from UNAIDS highlights the right to health as the key to ending AIDS
CAPE TOWN/GENEVA, 20 November 2017—Remarkable progress is being made on HIV treatment. Ahead of World AIDS Day, UNAIDS has launched a new report showing that access to treatment has risen significantly. In 2000, just 685 000 people living with HIV had access to antiretroviral therapy. By June 2017, around 20.9 million people had access to the life-saving medicines. Such a dramatic scale-up could not have happened without the courage and determination of people living with HIV demanding and claiming their rights, backed up by steady, strong leadership and financial commitment.
“Many people do not remember that in 2000 there were only 90 people in South Africa on treatment,” said Michel Sidibé, Executive Director of UNAIDS, speaking in Khayelitsha, South Africa. “Today, South Africa has the biggest life-saving treatment programme in the world, with more than 4 million people on treatment. This is the kind of acceleration we need to encourage, sustain and replicate.”
The rise in the number of people on treatment is keeping more people living with HIV alive and well. Scientific research has also shown that a person living with HIV who is adhering to an effective regime of antiretroviral therapy is up to 97% less likely to transmit HIV. As treatment access has been scaled up for pregnant women living with HIV, new HIV infections among children have been rapidly reduced. From 2010 to 2016, new HIV infections among children were reduced by 56% in eastern and southern Africa, the region most affected by HIV, and by 47% globally.
“In 2001, the first person in Khayelitsha started HIV treatment. Today, there are almost 42 000 people on treatment here. The success of Khayelitsha’s treatment programme is a microcosm of the massive success of South Africa’s HIV programme,” said Aaron Motsoaledi, Minister of Health, South Africa.
The challenges now are to ensure that the 15.8 million people in need of treatment—based on the number of people living with HIV at the end of 2016—can access the medicines and to put HIV prevention back at the top of public health programming, particularly in the countries in which new HIV infections are rising.
The new report from UNAIDS, Right to health, highlights that the people most marginalized in society and most affected by HIV are still facing major challenges in accessing the health and social services they urgently need. However, the report also gives innovative examples of how marginalized communities are responding.
In India, for example, a collective of sex workers has trained sex workers to work as nursing assistants, providing stigma-free health services to sex workers and the wider community. In Uganda, groups of grandmothers are weaving and selling traditional baskets to allow them to pay for schooling for the grandchildren in their care who lost their parents to AIDS.
In 2016, around 1.8 million people were newly infected with HIV, a 39% decrease from the 3 million who became newly infected at the peak of the epidemic in the late 1990s. In sub-Saharan Africa, new HIV infections have fallen by 48% since 2000.
However, new HIV infections are rising at a rapid pace in countries that have not expanded health and HIV services to the areas and the populations where they are most effective. In eastern Europe and central Asia, for example, new HIV infections have risen by 60% since 2010 and AIDS-related deaths by 27%.
References to the right to health are found in international and regional laws, treaties, United Nations declarations and national laws and constitutions across the globe. The right to health is defined in Article 12 of the International Covenant on Economic, Social and Cultural Rights as the right of everyone to the enjoyment of the highest attainable standard of physical and mental health. This includes the right of everyone, including people living with and affected by HIV, to the prevention and treatment of ill health, to make decisions about one’s own health and to be treated with respect and dignity and without discrimination.
UNAIDS’ Right to health report makes it clear that states have basic human rights obligations to respect, protect and fulfil the right to health.
The report gives voice to the communities most affected by HIV—including people living with HIV, sex workers, people who use drugs, gay men and other men who have sex with men and young people—on what the right to health means to them.
“Almost 20 years ago, the struggle was about access to treatment. Now, my struggle is not only about access but about ensuring that I have the support that I need to live a healthy and positive life. That is my right to health,” said Cindy Mguye, civil society representative.
Wherever the right to health is compromised, HIV spreads. In sub-Saharan Africa, for example, 67% of new HIV infections among young people are among young women and girls aged between 15 and 24 years. Studies have shown that a large number of young women and girls in the region contract HIV from older men, demonstrating multiple concerns about the ability of young women and girls to negotiate safer sex, stay in education and access age-appropriate sexual and reproductive health services.
Studies have also shown the difficulties health services face in reaching men with HIV testing and treatment, as well as broader health services, showing the challenge in encouraging men to exercise their right to health. In 2016, men in sub-Saharan Africa were 18% less likely to be accessing treatment and 8% more likely to die from AIDS-related illnesses than women.
The Right to health gives a clear demonstration of the challenges ahead in efforts to end the AIDS epidemic as a public health threat by 2030, as outlined in the 2016 United Nations Political Declaration on Ending AIDS.
The report underscores that to reduce new HIV infections and AIDS-related deaths and ensure access to essential health services, funding for health needs to increase. It gives examples of how to enhance funding, including increasing the share of health spending as a proportion of national economies, making savings through efficiencies and partnering with the private sector. The funding gap for HIV is estimated at US$ 7 billion by 2020.
UNAIDS has set an agenda to Fast-Track the response to HIV by 2020 towards ending the AIDS epidemic as a public health threat by 2030. It will continue to work closely with its Cosponsors and partners to ensure that everyone, everywhere can fulfil their right to health and can access the health and social services they need.
In 2016 (*June 2017) an estimated:
*20.9 million [18.4 million–21.7 million] people were accessing antiretroviral therapy (in June 2017)
36.7 million [30.8 million–42.9 million] people globally were living with HIV
1.8 million [1.6 million–2.1 million] people became newly infected with HIV
1.0 million [830 000–1.2 million] people died from AIDS-related illnesses
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
UNAIDS South AfricaNatalie Ridgard
tel. +27 82 909 2637
ridgardn@unaids.org
UNAIDS Communications
tel. +41 22 791 3873
communications@unaids.org
Related publications
Press centre
Download the printable version (PDF)




Update
United Nations Deputy Secretary-General and Geneva-based leaders discuss the future of global health in 2030 Agenda
15 November 2017
15 November 2017 15 November 2017What do we need to do differently to reach the ambitious health-related targets in the 2030 Agenda for Sustainable Development? This was the question at the heart of a dynamic exchange of views between United Nations Deputy Secretary-General Amina Mohammed and Geneva-based global health leaders on realizing the vision of health in the 2030 Agenda.
The event was hosted by Tedros Adhanom Ghebreyesus, Director-General of the World Health Organization, and Michel Sidibé, Executive Director of UNAIDS, and was chaired by Valentin Zellweger, Permanent Representative of Switzerland to the United Nations Office and other International Organizations in Geneva. Engaging ambassadors, international organizations, civil society and private sector stakeholders based in Geneva, the meeting sought to identify gaps in the global health agenda and generate concrete, shared solutions for accelerating country-level impact.
In her remarks, Ms Mohammed highlighted health as central to sustainable development and challenged the participants to identify how health can be a guiding light and integrative force for action across the 2030 Agenda. She emphasized the need for more robust data to better understand current health trends and bring programmes to scale.
Ms Mohammed further called for a mapping of the determinants of health to demonstrate to political leaders the urgent need for stronger multisectoral action. She urged participants to consider how health can showcase collective action and results in the context of United Nations reform.
The Sustainable Development Goals (SDGs) have vastly expanded the health agenda, bringing to the fore a range of issues that account for a significant burden of morbidity and mortality, but have not yet been embraced as global health priorities. The participants drew attention to a number of SDG targets that continue to have inadequate political commitment and investment, such as those on mental health, noncommunicable diseases, antimicrobial resistance, air pollution, violence against women and the health of migrants.
During the event, the participants provided a number of proposals on leveraging the unique capacity of Geneva-based institutions, including incubating partnerships on peace, health and trade, building on human rights expertise to address the social determinants of health, encouraging the engagement of ministers beyond health in global health discussions and influencing the global funding architecture to support community-driven solutions and responses.
The participants emphasized the potential for global health to be a forerunner in United Nations reform and to bring new ways of working across the agenda for country-level impact.
Quotes
“The Secretary-General and I place great emphasis on prevention. Investing in prevention to keep people healthy will bring the largest dividend. To do that means addressing social determinants with a myriad of stakeholders in politics, education, trade, civil society, the investor community and beyond.”
“Not only is Geneva the capital of global health, with its critical mass of technical expertise, it also embodies the spirit of collective action, where stakeholders, including international agencies, Member States, civil society, academia and the private sector, can forge innovative partnerships to deliver results for people.”
“Achieving the Sustainable Development Goals is about speed, scale and quality. Are we moving fast enough? Are our efforts and investments ambitious enough? And are we delivering quality health services for all? But above all, the 2030 Agenda for Sustainable Development is a political document. Universal health coverage is a political choice. As technical agencies, we must strengthen our ability to play political roles.”
“Health can be a major entry point for implementing United Nations reform by simplifying and streamlining the health architecture through one inclusive country platform, one implementation plan and one data hub for planning, monitoring and accountability. This will help the United Nations system to be more focused, more aligned and more effective in its support to countries.”
Related


Update
Engaging France's First Lady on education and HIV
25 October 2017
25 October 2017 25 October 2017During a visit to Paris, UNAIDS Executive Director met with France's First Lady at the Elysée Palace to discuss the links between education and HIV.
Mr Sidibé explained that in sub-Saharan Africa, three in four new HIV infections in 15-19 year olds are among girls. And HIV is the third leading cause of death among young women aged 15-29 globally.
The causes vary but lower access to education along with gender inequalities erode women and girls' ability to negotiate safe sex and have control over their bodies. In addition, most young people lack the knowledge to protect themselves from HIV. In sub-Saharan Africa, surveys from 35 countries showed that only 36% of young men and 30% of young women correctly identified the ways of preventing the sexual transmission of HIV.
Mr Sidibé stressed that when girls stay in school they are less vulnerable to HIV. He also emphasized that age-appropriate comprehensive sex education for girls and boys is a cornerstone to end the AIDS epidemic.
Acknowledging Mrs Macron's vast experience in education as a teacher and educator, Mr Sidibé offered support to organize an event on girls’ education on the sidelines of the Dakar financing conference of the Global Partnership for Education in February 2018. Senegal and France are co-hosting the event to raise funds for teachers' trainings and to promote scientific and computer education in schools.
UNAIDS has invited the First Lady of France at its Geneva headquarters in the coming year and to join the First Ladies of Africa at next year's General Assembly in New York.
Quotes
"It is key to strengthen synergies between education and the HIV response including through comprehensive sexuality education. France's leadership is as necessary as ever to end the AIDS epidemic by 2030."
Region/country
Related
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025

Update
UNAIDS urges United Republic of Tanzania to implement HIV Prevention 2020 Road Map
19 October 2017
19 October 2017 19 October 2017In the United Republic of Tanzania, new HIV infections declined by 18% between 2010 and 2016, falling to an estimated 55 000 new HIV infections in 2016. While this is steady progress, the country needs to do more to stop new HIV infections, particularly among adolescent girls and young women, who accounted for an estimated 18 000 new HIV infections in 2016, and among populations at higher risk of HIV. In 2016, there were more AIDS-related deaths among adult men than women, pointing to the need to reach men with HIV testing and treatment services.
During a visit to mainland Tanzania and Zanzibar, the Executive Director of UNAIDS, Michel Sidibé, called on the government and civil society to spearhead the implementation of the recently launched HIV Prevention 2020 Road Map. If implemented, the road map will Fast-Track progress to reduce new HIV infections globally by 75%—from 2.2 million in 2010 to 500 000 by 2020.
During his visit, Mr Sidibé met with the President of Zanzibar as well as a number of ministers and senior government officials in both mainland Tanzania and Zanzibar. He congratulated the United Republic of Tanzania on its commitment to achieve the Fast-Track Targets by 2020. He added that in order to reach those targets, the United Republic of Tanzania will need to prioritize HIV prevention strategies to dramatically reduce new HIV infections. He emphasized the importance of leaving no one behind in access to health and HIV services, including key and vulnerable populations.
During his meeting with the President of Zanzibar, Ali Mohamed Shein, Mr Sidibé encouraged the President to achieve the elimination of mother-to-child transmission of HIV by 2020, which is well within reach in both mainland Tanzania and Zanzibar.
Mr Sidibé also met with civil society organizations during his visit. Civil society play a critical role in responding to HIV in the United Republic of Tanzania, serving on the board of the national AIDS council and ensuring that the AIDS response is multisectoral, inclusive of people living with HIV and reaches people at higher risk of HIV infection.
Mr Sidibé emphasized civil society’s important role in strengthening community responses to HIV and made a call to ensure that its work is integrated into national HIV responses and adequately funded through domestic and international investments.
On 10 October 2017, UNAIDS, UNFPA and partners launched the HIV prevention 2020 road map as part of efforts to reduce new HIV infections by 75% by 2020.
Quotes
“I am pleased with the progress thus far. HIV infections are being reduced, but we need to sustain the gains. We are committed to the African Union global solidarity and shared responsibility agenda.”
“The challenges to ending AIDS here are similar to those in many other places—being able to reach the people most affected by HIV and ensuring they have access to HIV prevention, testing and treatment services.”
“Being part of the Zanzibar Association of People Living with HIV/AIDS gives me a home to interact with my peers and discuss common challenges, the ability to gain skills and an opportunity to speak on behalf of my community at a high level, both nationally and internationally.”
Region/country
Related
Related
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
55th meeting of the UNAIDS Programme Coordinating Board
10 December 2024
 To end AIDS, communities mobilize to engage men and boys
To end AIDS, communities mobilize to engage men and boys

04 December 2024