UNDP The United Nations Development Programme

Feature Story
Haiti’s HIV successes and challenges acknowledged on World AIDS Day
02 December 2012
02 December 2012 02 December 2012
UNAIDS Executive Director Michel Sidibé (left) participates in a World AIDS Day event in Pétionville, Haiti, along with United States Ambassador to Haiti, Pamela White, and Haiti’s First Lady, Sophia Martelly.
On one level, Haiti’s HIV response parallels its earthquake recovery. Although the task is far from over, national and international stakeholders have collaborated to confront the challenge and important gains have been made.
During a World AIDS Day commemoration in Pétionville, Haiti, hosted by the Ministry of Health, UNAIDS Executive Director Michel Sidibé congratulated the country on its progress toward the vision of “getting to zero:” zero new HIV infections, zero discrimination and zero zero AIDS-related deaths.
Over the past decade, the rate of new HIV infections in Haiti fell by 54%. From 2005 to 2011, there was a 47% national decline in AIDS-related deaths. By 2011, 58% of Haitians living with HIV were accessing antiretroviral therapy. Mr Sidibé expressed optimism that this positive trajectory would continue.
“I was honoured yesterday to meet the President of the Republic and I can tell you that during our conversation, it was obvious that he wanted to put AIDS at the centre of his efforts to ensure that all people have access to the information and support systems necessary for life,” Sidibé said.
These efforts, said Mr Sidibé, must focus on the country’s most vulnerable. An estimated 18% of men who have sex with men and 8% of sex workers in Haiti are living with HIV. Nearly half of young Haitians living in camps do not have adequate knowledge about HIV.
Mr Sidibé urged Haiti’s leaders to boost efforts to reach populations at high risk of HIV infection with prevention and treatment services. He called for the passage of an HIV law that would signal zero tolerance for stigma and discrimination.
I am proud to be working alongside the President of the Republic to guarantee education for all, the strengthening of our health care system, women's empowerment and improved living conditions for the whole population.
First Lady Sophia Martelly
Mr Sidibé also urged the leadership of Haiti to increase domestic investments for the HIV response. Currently, more than 75% of funding for Haiti’s HIV response comes from external sources. By taking greater ownership of its national AIDS response, Haiti would join the worldwide paradigm shift “from charity to global solidarity,” said the UNAIDS Executive Director.
During the World AIDS Day ceremony, Haiti’s First Lady, Sophia Martelly, acknowledged the complex network of social issues that increase people’s risk of HIV. “Wherever educating children is problematic, there will be AIDS. Wherever basic social needs are not met, there will be AIDS. Wherever there is violence and rape, there will be AIDS. That is why there must be an in-depth approach to prevention,” said the First Lady.
“I am proud to be working alongside the President of the Republic to guarantee education for all, the strengthening of our health care system, women's empowerment and improved living conditions for the whole population,” she added.
Speeches
Speeches
- First Lady of Haiti (in French)
Related

Feature Story
Costa Rica to develop HIV strategies to reach male sex workers
06 November 2012
06 November 2012 06 November 2012
UNAIDS Executive Director Michel Sidibé and the Minister of Health of Costa Rica, Dr Daisy Corrales. UNAIDS HQ, Geneva. 6 November 2012. Credit: UNAIDS
The Minister of Health of Costa Rica, Dr Daisy Corrales, aims to strengthen the AIDS response among key populations at higher risk in her country, which is where the epidemic remains concentrated. During a meeting with UNAIDS Executive Director Michel Sidibé on 6 November at the UNAIDS Headquarters in Geneva, Dr Corrales highlighted the focus of her Ministry in developing HIV communications and educational strategies for organizations working with male sex workers.
“We need to develop our strategies to reach male sex workers with HIV information and education that is relevant to their needs and in agreement with their particular work schedules,” said Dr Corrales.
Costa Rica’s HIV prevalence among adults 15 to 49 years of age is 0.3%. The country’s HIV epidemic is concentrated among key populations at higher risk of infection such as the migrant indigenous population, men who have sex with men (MSM), sex workers and their clients. A study conducted in 2010 found HIV prevalence among MSM of 10.9% and 11% among female sex workers.
“It is not always easy to talk about men who have sex with men, sex workers or drug users but we have an obligation to ensure they have access to HIV services that are free from stigma and discrimination,” said Mr Sidibé.
We need to develop strategies to reach male sex workers with information and education that is relevant to their needs and in agreement with their particular work schedules
Minister of Health of Costa Rica, Dr Daisy Corrales
Mr Sidibé also commended the Government of Costa Rica for its efforts in scaling up HIV treatment for people with HIV—an estimated 65% coverage—as well as their success in stopping new HIV infections among children. “Costa Rica’s transmission rate of HIV from mother-to-child is consistently under 2%, a very impressive feat and a bold example for Latin America that an HIV free generation is within our reach.”
Mr Sidibé assured the Minister of Health that UNAIDS will continue providing support to Costa Rica to design its strategy for an effective and sustainable response to AIDS.

Feature Story
Namibia’s City of Windhoek collaborates to strengthen HIV response
30 October 2012
30 October 2012 30 October 2012
The Mister Sister Mobile clinic parked outside the office of Hope Initiative SA—a community-based organization that provides care and support services for orphans and vulnerable children in the informal settlements around Windhoek.
Credit: UNAIDS/T.Figuera
Similar to many other countries, Namibia’s population has been shifting towards towns and cities in search of better opportunities and hoping for a more prosperous life. Urbanization has led to the growth of informal settlements surrounding major cities and towns making it difficult to reach residents with critical health services.
Namibia’s capital City of Windhoek—whose population grew by 38% between 2001 and 2011—has partnered with UNAIDS, UNDP and PharmAccess Foundation to strengthen its overall health and HIV response with innovative options such as mobile clinics.
“The City of Windhoek is committed to delivering efficient and effective municipal health services to all Windhoek residents, in particular underserved populations,” said the Chief of Health Services for the City of Windhoek, Mary-Anne Kahitu. “Through our strategic partnerships—such as with the Ministry of Health and Social Services, PharmAccess Foundation and other key stakeholders—we will endeavor to promote increased access to quality health and HIV services in informal settlements,” she added.
During a period of 18 months, the joint project "Strengthening city responses to HIV/AIDS" explored the city’s urban HIV epidemic and response. Findings included a household survey showing that HIV incidence and prevalence appeared to be higher in the north-western area of Windhoek, which is primarily characterized by informal settlements and low-income formal housing. The study highlighted that these areas had limited access to adequate HIV prevention and treatment services—such as antiretroviral treatment, HIV counselling and testing and services to stop mother-to-child transmission of HIV.
Mobile health services
The findings of the study prompted collaborative action between PharmAccess Foundation, the City of Windhoek and the Ministry of Health and Social Services to provide mobile health services. Twice a month, a mobile clinic visits the informal settlements. Supported through the PharmAccess’ Mister Sister Mobile clinic project, the Ministry provides all medicines for the operation of the clinic free of charge.
The City of Windhoek is committed to delivering efficient and effective municipal health services to all Windhoek residents, in particular underserved populations
Chief of Health Services for the City of Windhoek, Mary-Anne Kahitu
The first mobile clinic was parked outside the office of Hope Initiative SA (HISA), a small community-based organization that provides care and support services for orphans and vulnerable children in the informal settlements around Windhoek.
“It is very important to have a mobile clinic in informal settlements because without it, children and vulnerable people would definitely not have access to medical help,” said Patricia Sola, Founder of Hope Initiative. “Our nearest clinic is more than an hour walk away, not to mention the cost of being seen by a doctor.” For HISA, the clinic also brings an opportunity to give information to patients on access to social grants and birth registration.
The primary health care services provided the same kind of services the Ministry offers in its health care facilities. These include family planning advice and supplies, routine immunizations, child growth monitoring, screening for TB symptoms and referral, diagnosis and treatment of routine communicable disease, HIV testing, and referral and follow up on chronic diseases.

UNAIDS Deputy Executive Director, Management and Governance, Jan Beagle chats with a group of children during her recent visit to Namibia.
Credit: UNAIDS/T.Figuera
In August 2012, PharmAccess began expanding its operations into the rural and remote areas of Khomas and Omaheke regions with two additional mobile clinics. “PharmAccess Namibia is very proud to provide primary health care services to the people who need it most in Windhoek’s poorest informal settlements,” said Ingrid De Beer, Managing Director of Pharm Access in Namibia. “Our partnership with the Ministry of Health and Social Services, supported by Mister Sister Partners and the City of Windhoek, has made this possible. In the coming months, we look forward to collecting the evidence required to inform local policies on primary health service provision in the informal settlements of greater Windhoek,” she added.
In a recent visit to Namibia, UNAIDS Deputy Executive Director, Management and Governance, Jan Beagle, along with representatives of partner organisations involved in the project, commended the City of Windhoek and the Ministry of Health and Social Services for its leadership and commitment to strengthening the city's response to HIV.
Ms Beagle highlighted the excellent partnership between the community, civil society and government to meet the health needs of vulnerable populations in informal settlements around Windhoek and emphasized that “such innovative initiatives should be scaled up and replicated across the country.”
External links
External links
Related
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025
 Status of HIV Programmes in Botswana
Status of HIV Programmes in Botswana

20 February 2025

Feature Story
Zambia learns from Kenya’s experience in developing HIV programmes for key populations at higher risk
17 October 2012
17 October 2012 17 October 2012
Zambian delegation with staff from the Kenya Medical Research Institute, A drop-in Centre at Mtwapa, Mombasa.
South to South learning—or the cooperation between low- and middle-income countries—can help countries understand how to respond to HIV, particularly in politically and culturally sensitive areas such as developing programmes for key populations at higher risk of HIV infection.
From 24- 28 September 2012, members of the National AIDS Council of Zambia, with support from the country’s United Nations Joint Team on AIDS, visited to Kenya to learn about their HIV programmes to reach key populations including sex workers, people who inject drugs, men who have sex with men and transgender people.
Despite both countries having restrictive legal environments which criminalise sex work, same sex sexual relations and drug use, Kenya has long recognized its complex HIV epidemic among key populations—which accounts for 33% of new HIV infections. The country put in place a technical working group within the ministry of health to develop programmes that meet the needs of most at risk populations.
“The Modes of Transmission Study done in 2009 clearly showed that we needed interventions for key populations if we were to have a significant impact on the epidemic,” said Dr Orago, Director of the National AIDS Control Council in Kenya.
Zambia’s National AIDS Strategic Framework has recognized the need to gather more information on the epidemic among key populations. Two studies are currently planned to collect the required information. However, HIV programmers recognize that having this information is just one step towards getting key populations the services they require. It will take much longer to address the stigma and discrimination towards these key populations entrenched in Zambia’s society.
Kenya’s political leadership was seen as a key element that has contributed to focus the AIDS response on key populations despite the existence of a non-supportive social environment. In October 2010, for example, the Minister of special programs Esther Murugi opened the national symposium on “Most at Risk Populations” in the country where she recommended more tolerance and acceptance towards men who have sex with men. Also, prominent parliamentarians have long supported the implementation of programmes focusing on people who use drugs in the coast province. “It is clear from what we have seen in Kenya that we need to organize stakeholders and to establish a mechanism that will help us mobilize political support at the highest levels,” said Harold Witola of the Zambian National AIDS Council.
The cornerstone of the response in Kenya is a partnership framework between Government, NGOs and organized key population groups. Kenya has reached a stage in the response where the Government and its partners are implementing evidence-based HIV programmes that focus on the needs of key populations at higher risk. These include purchasing and distributing condoms and water-based lubricants for men who have sex with men and sex workers; developing HIV prevention information materials specifically for key populations; and designing a programme to make disposable syringes available for people who use drugs.
The Modes of Transmission Study done in 2009 clearly showed that we needed interventions for key populations if we were to have a significant impact on the epidemic
Dr Orago, Director of the National AIDS Control Council in Kenya
The Zambian delegation, which included HIV programmers and decision-makers from different Government departments as well as civil society and UN partners, visited a range of programmes to understand how Kenyan service providers work within the national policy and legal framework to provide an effective package of HIV-related activities for key populations.
They visited two peer support programs for people who use drugs, a government clinic in Nairobi that focus on sex workers and men who have sex with men, an NGO clinic for male and female sex workers, and a peer support group for men who have sex with men. They also met with members of the media to identify ways to leverage its advocacy capacity and support.
The team also held community level discussions with groups of men who have sex with men, sex workers (female and male), people who inject drugs and truck drivers. “What strikes me is the excitement and commitment of everyone that we have met, including Government officials, civil society members and the beneficiaries of these services to respond to the public health needs of these important groups in the response to AIDS,” said Dr Mwango as Team Leader for the Zambia Team.
Focusing on the health needs of key populations is an essential human right, fundamental to protecting the public health and critical to reaching the goal of universal access to HIV prevention, treatment, care and support. The Zambia Team left Kenya with a resolve to make a difference for the lives of Zambians who are at the most risk of becoming infected with HIV. “It is not going to be easy, but we have seen in Kenya that it can be done” said Helen Frary, UNAIDS Country Coordinator for Zambia.
Related
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025
 Status of HIV Programmes in Botswana
Status of HIV Programmes in Botswana

20 February 2025

Feature Story
New handbook to improve design of HIV programmes focusing on men who have sex with men in the Middle East and North Africa region
03 October 2012
03 October 2012 03 October 2012
A new handbook to help design and implement HIV programmes focusing on men who have sex with men (MSM) in the Middle East and North Africa (MENA) was released on 27 September by UNAIDS in Cairo, Egypt. The handbook was presented at a workshop organized by the World Health Organization entitled "HIV Among Key Populations at Increased Risk of Sexual Transmission".
Entitled “HIV and Outreach Programmes with Men who Have Sex with Men in the Middle East and North Africa: From a Process of Raising Awareness to a Process of Commitment”, it aims to provide countries that are currently implementing MSM programmes with additional tools to improve them. It also provides other countries willing to initiate MSM programmes with sufficient elements to do so.
The new publication describes in four modules the whole cycle of a national HIV outreach programme aimed at engaging MSM. These four modules include: Situation analysis; outreach programme conceptualization, outreach approach, and monitoring. Each module contains scientific data and practical steps.
Prevailing taboos hamper the AIDS response
Sexuality and sexually transmitted infections (STIs) are sensitive issues that are rarely discussed in the MENA region and homosexuality and transexuality remain taboo subjects, according to the new report.
This handbook will give a strong theoretical and technical background and support to outreach workers; be it health care providers or peer educators
Elie Aaraj, President of the Regional/Arab Network Against AIDS (RANAA) and Executive Director of MENAHRA
"Most countries in the region criminalise same sex relations making it virtually impossible for this key population to seek or receive the necessary HIV prevention, treatment and care services," said Ali Feizzadeh, Senior Strategic Information Advisor at UNAIDS.
An increasing number of bio-behavioural surveys in the region show that the AIDS epidemic is concentrated within key populations at higher risk—notably MSM. The same surveys reveal that MSM regularly change sexual partners, and may be drug users or sex workers while their knowledge of STIs remains limited.
The new UNAIDS publication stresses that, while the current regional AIDS response is characterized by low coverage of HIV prevention programmes for key populations at higher risk, there is a growing awareness of the need to work with populations such as MSM on HIV prevention in the region. Currently, these efforts are mainly undertaken by non-governmental associations.
"All the countries in the region approved the Human Rights Declaration, however, some sensitive areas of work cannot be undertaken by the present governmental bodies. The role of the Civil Society is to bridge the gap between national support and the actual need,” said Elie Aaraj, President of the Regional/Arab Network Against AIDS (RANAA) and Executive Director of MENAHRA. “This handbook will give a strong theoretical and technical background and support to outreach workers; be it health care providers or peer educators," he added.
The UNAIDS handbook provides useful information, tips and tools to effectively reach MSM communities, establish trust and build relationships through continuous dialogue. The handbook emphasizes the importance of engaging the MSM population in the effective design of HIV outreach programmes.
The handbook is the result of the analysis of existing programmes and fieldwork conducted by partner civil society organizations in nine countries across the region. It complements the recently published WHO Guidelines that focus on good practice recommendations in the area of prevention and treatment of HIV and other STIs among MSM and transgender people.
Related

Feature Story
Homophobia and punitive laws continue to threaten HIV responses and human rights
28 August 2012
28 August 2012 28 August 2012
Nearly eighty countries have laws that criminalize same-sex sexual relations. UNAIDS Infographic: I am Gay--5 things I fear.
In many regions of the world, punitive laws and practices against lesbian, gay, bisexual and transgender and intersex (LGBTI)[1] individuals continue to block effective responses to HIV. A range of human rights violations have been documented, from denial of health services and freedom of association to harassment, violence and murder.
Last week, a youth organization in Cameroon is reported to have held an anti-LGBT rally; the news followed a series of arrests and detentions in recent years of Cameroonian men who have sex with men based on their sexual orientation.
In Zimbabwe, where sex between men is illegal, police officers arrested and later released 44 members of the organization Gays and Lesbians Zimbabwe (GALZ) on 11 August 2012 following the launch of a GALZ report documenting human rights violations of LGBT individuals.
In Europe, a report on the human rights situation of LGBTI people—published in May 2012 by the European Region of the International Lesbian, Gay, Bisexual, Trans and Intersex Association (ILGA-Europe)—documented many cases of violence, hatred and discrimination against LGBTI people.
Human rights violations based on people's real or perceived sexual orientation, gender identity or expression sanction the climate of hate and fear that keeps LGBTI people further in the closets. Such violations discourage health-seeking behaviour, deny access to key health services and sustain the increasing incidence of HIV infection among men who have sex with men and transgender people.
Human rights advocate Joel Nana, Executive Director of the non-profit organization African Men for Sexual Health and Rights (AMSHeR)
Studies in the United States, Canada, Europe and Australia have documented high levels of homophobic bullying in schools and lack of support from school authorities. A recent study conducted in the United States, for example, found that more than 84% of young LGBT learners had been called names or threatened, 40% had been pushed or shoved, and 18% had been physically assaulted at school.
Several cities in the Russian Federation recently passed laws prohibiting public information on sexual orientation and gender identity. Similar legislation is pending before the Ukrainian parliament. UNAIDS believes such laws discriminate against LGBT people by curtailing their freedoms of assembly and speech, threaten HIV outreach organizations supporting them, and may be used to justify homophobic bullying and violence.
A ‘climate of hate and fear’
Evidence and experience have shown that punitive laws and practices drive sexual minorities away from HIV services. A study conducted in Senegal, for example, found that prosecutions and harassment of LGBT individuals in 2008 led to “pervasive fear and hiding” among members of these groups. According to the study, some health providers suspended their HIV prevention work with men who have sex with men out of fear for their own safety; those who continued to provide health services noted a sharp decline in participation by men who have sex with men.
"Human rights violations based on people's real or perceived sexual orientation, gender identity or expression sanction the climate of hate and fear that keeps LGBTI people further in the closets,” said human rights advocate Joel Nana, Executive Director of the non-profit organization African Men for Sexual Health and Rights (AMSHeR). “Such violations discourage health-seeking behaviour, deny access to key health services and sustain the increasing incidence of HIV infection among men who have sex with men and transgender people," he added.
High HIV prevalence among men who have sex with men, transgender people
In many regions of the world, men who have sex with men and transgender people experience high HIV prevalence and low coverage of HIV prevention, treatment, care and support services.
Recent studies from sub-Saharan Africa show that HIV prevalence among men who have sex with men ranges from 6% to 31%. In Asia, the odds of men who have sex with men becoming infected with HIV are nearly 19 times higher than in the general population. In Latin America, an estimated half of all HIV infections in the region have resulted from unprotected sex between men.
Studies among transgender people have shown disproportionately high HIV prevalence ranging from 8% to 68%. Without access to HIV information and services free of fear, criminal sanction and homophobia, these trends cannot be addressed.
“World leaders are increasingly speaking out against discrimination and criminalization on the basis of sexual orientation and gender identity,” said Susan Timberlake, Chief of the Human Rights and Law Division at the UNAIDS Secretariat. “In launching its report in July, for example, the Global Commission on HIV and the Law issued a strong call for decriminalization of LGBT people and their protection in the context of the AIDS response.”
Some positive developments
Despite setbacks, there are some encouraging developments in favour of equality, non-discrimination and access to health services for sexual minorities.
On 12 July 2012, the President of Chile signed into law an anti-discrimination law that punishes hate crimes, including against LGBT people. Introduced some seven years ago, the adoption of the anti-discrimination law gained momentum following the brutal murder of Daniel Zamudio, a 24-year-old homosexual man.
On the International Day Against Homophobia and Transphobia, 17 May 2012, the European Region of Education International, the European Trade Union Committee for Education (ETUCE), the European Trade Union Confederation (ETUC) and ILGA-Europe committed to strengthen their collaboration to prevent and combat homophobia and transphobia at national and European levels in school, the workplace and society.
In February 2010, the Government of Fiji became the first Pacific Island nation to formally decriminalize sex between men. Fiji’s new Crimes Decree removes previous references to “sodomy” and “unnatural acts” and uses gender neutral language when referring to sexual offences.
In 2009, the High Court of Delhi held that criminalization of same-sex relations is unconstitutional and that it “pushes gays and men who have sex with men underground,” leaving them vulnerable to police harassment and impeding access to HIV services.
UN advocacy and action
In March 2012, the UN High Commissioner for Human Rights presented a report at the 19th session of the UN Human Rights Council documenting discriminatory laws and practices and acts of violence against LGBT individuals based on their sexual orientation and gender identity. The report called on all countries to decriminalize consensual same-sex relations and to ensure that individuals can exercise their rights to freedom of expression, association and peaceful assembly in safety and without discrimination.
At last year’s UN General Assembly High Level Meeting on AIDS, UN Member States committed to reviewing laws and policies that adversely affect the “successful, effective and equitable delivery of HIV services.” UNAIDS encourages all countries to translate this commitment into action to protect the human rights and health needs of LGBT people.
[1] The acronym “LGBTI” is used as an umbrella short-hand for groups and/or individuals whose sexual orientation or gender identity differ from heterosexuality and who may be subject to discrimination, violence and other human rights violations on that basis. Information and data presented in this article may not apply equally to all the groups represented by this acronym. [Back to top]
Related
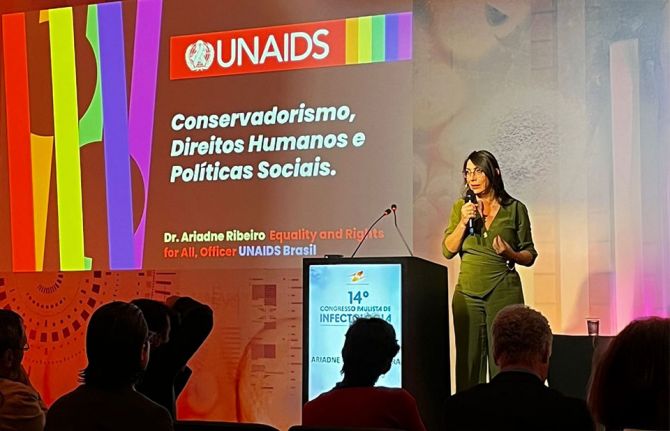 Upholding dignity for everyone: Ariadne Ribeiro Ferreira
Upholding dignity for everyone: Ariadne Ribeiro Ferreira
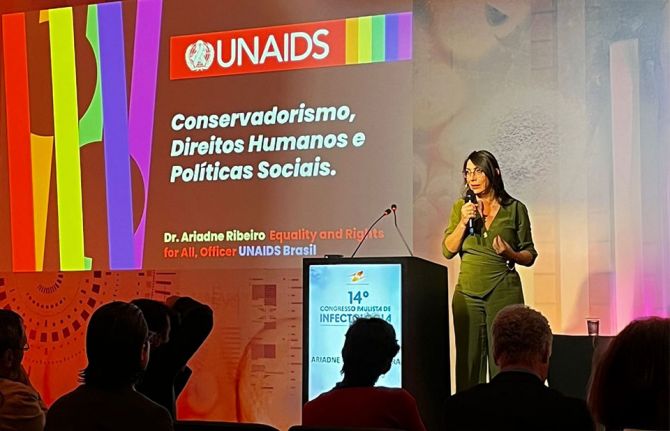
21 November 2024
 Evelyn Siula: A journey of strength and solidarity
Evelyn Siula: A journey of strength and solidarity
18 November 2024

Feature Story
Sex workers demand respect for their fundamental rights in a parallel summit to the AIDS 2012
25 July 2012
25 July 2012 25 July 2012
Sex worker initiative Veshya Anyay Mukti Parishad (VAMP) give a performance at the opening of the Sex Workers’ Freedom Festival in Kolkata, India.
Credit : UNFPA/J.Cabassi
As thousands of delegates gather for the XIX International AIDS Conference (AIDS 2012) in Washington, D.C. this week, a parallel satellite hub, the Sex Worker Freedom Festival, is taking place in Kolkata, India, from 22-26 July.
The event brings together over 600 sex workers, international and national partners from more than 40 countries. The Freedom Festival has been organized by sex workers as a response to extensive visa regulations for sex workers and people who use drugs, which may have prevented many from attending the International AIDS Conference event in Washington DC. The five-day festival gives participants the opportunity to be part of the Washington event through video-conferencing link up with major conference sessions and with the Global Village.
“The Sex Worker Freedom Festival is an alternative event for sex workers and our allies to protest our exclusion and ensure the voices of those excluded are heard in Washington.” said Ruth Morgan the Global Coordinator of the Global Network of Sex Work Projects (NSWP) and Co-Organizer of the Kolkata event.
Speaking at the opening of the Kolkata hub, United Nations Secretary General’s Special Envoy on AIDS in Asia and the Pacific, Prasada Rao, stressed that freedoms and rights of sex workers are being denied on a daily basis.
“Aspects of sex work are criminalized in 116 countries around the world. Laws in many countries conflate adult consensual sex work with human trafficking. Routine police raids, often in the name of anti-trafficking, lead to arrest and harassment of adult consenting sex workers,” said Mr Rao. “These discriminatory practices drive sex workers to social exclusion and into a socially disadvantageous position, accentuating their vulnerability to HIV,” he added.
Despite progress made in reducing the spread of HIV within sex work communities, sex workers are still at increased risk of HIV infection. In the Asia-Pacific region for example, while a number of countries have reduced their HIV infection rates with intensive HIV prevention programmes among people who buy and sell sex, hotspots of high prevalence remain. Surveys of female sex workers in India show prevalence of 18% in Maharashtra and 41% in Pune—the overall adult level in the country is an estimated 0.3%.
Sharing experiences, driving progress
The Sex Worker Freedom Festival programme is structured around fundamental freedoms; human rights that all people are entitled to. These include freedom of movement; freedom to access quality health services; freedom to work and choose occupation; freedom to unionise; freedom to be protected by the law; freedom from violence; and freedom from stigma and discrimination.The Festival aims to facilitate the sharing of experiences as well as dialogue around key issues and priorities for the sex work community and HIV programming.
“Without the right to organize and unionize the sex worker community cannot advance our rights,” stated Bharati Dey, General Secretary, Durbar Mahila Samanwaya Committee (DMSC), co-organizer of the Kolkata Hub.
Discriminatory practices drive sex workers to social exclusion and into a socially disadvantageous position. This accentuates vulnerability to HIV
United Nations Secretary General’s Special Envoy on AIDS in Asia and the Pacific, Prasada Rao
The stigma and discrimination experienced by sex workers was identified as a major obstacle to an effective response to AIDS. “Every day and in every location, we have to battle against stigma and discrimination,” said Lakshmi, a sex worker and the Director of Programmes at the Ashodaya sex worker initiative in Mysore, India, said. “We have found a way to be part of the solution. Our team of HIV positive sex worker volunteers has built an effective partnership between communities and health services. This has changed attitudes of health care providers and has created community confidence to access health services.”
Annah Pickering, a sex worker and Manager of the Auckland Region, New Zealand Prostitutes Collective, underlined the multiple benefits of decriminalization of sex work in her country, both for sex worker rights and the HIV response. “We appreciate many legal freedoms. We can report corrupt officials who demand free sex. We don’t hide our condoms in our bras or behind the picture or in the thermos flask. We can put up signs and promote safe sex and insist on it. Does decriminalising sex work prevent the transmission of HIV? I strongly believe so. When you put all these elements together they contribute significantly to support sex workers in preventing the transmission of HIV,” she said.
A central theme of discussions at the Kolkata Hub has been the widespread experiences of violence faced by sex workers around the globe on a daily basis. Sessions have underlined how documentation of sex workers’ experience of violence is critical to ensuring evidence is used to inform effective responses. A sex worker led research project being conducted in Sri Lanka, Myanmar, Nepal and Indonesia by the Center for Advocacy on Stigma and Marginalization (CASAM), the Asia Pacific Network of Sex Workers (APNSW), UNFPA, UNDP, UNAIDS and Partners for Prevention was highlighted as an important initiative in better identifying the risks and factors that help protect sex workers’ from violence.

UN Secretary General’s Special Envoy for AIDS in Asia and the Pacific Mr Prasada Rao speaks at the opening of the Sex Workers’ Freedom Festival in Kolkata, India.
Credit: UNAIDS
“This research is designed to generate quality data, that ensures sex workers’ lived experiences are used to advocate for better policy and programmes to prevent and respond to violence,” said Meena Seshu, Director of the Sampada Gramin Mahila Sanstha (SANGRAM) sex worker peer education project.
The importance of increasing sex workers’ access to quality, integrated, health services has also been a key issue of emphasis. Kay Thi Win, Director of the Targeted Outreach Programme (TOP) initiative in Myanmar, which provides peer-to-peer HIV prevention and support for sex workers said: “There are few sex worker friendly clinics. When TOP started, there was no comprehensive sexual health intervention in Myanmar for sex workers. However through our work we have been able to increase the linkages by providing a comprehensive sexual and reproductive health package that also includes HIV services.”
The Kolkata Hub is hosted by Durbar Mahila Samanwaya Committee (DMSC), and is co-organized with the Global Network of Sex Workers (NWSP) and the All India Network of Sex Workers (AINSW). It is supported by the Open Society Foundation’s Sexual Health and Rights Program, UNAIDS, the Dutch Ministry of Foreign Affairs, UNFPA, HIVOS (the Humanist Institute for Development Cooperation), AIDS Fonds (a Netherlands-based HIV project funder) and the AIDS 2012 conference secretariat.
External links
Publications
Publications
- HIV in Asia and the Pacific: Getting to Zero (UNAIDS, 2011)
Related
 Evelyn Siula: A journey of strength and solidarity
Evelyn Siula: A journey of strength and solidarity
18 November 2024

Feature Story
TB and HIV integration discussed at AIDS 2012
22 July 2012
22 July 2012 22 July 2012
Ms Jan Beagle, UNAIDS Deputy Executive Director, Management and External Relations, spoke during the show and reiterated UNAIDS’s commitment to working with partners in support of the global target to halve TB deaths in people living with HIV by 2015.
Credit: UNAIDS
Tuberculosis (TB) remains one of the leading causes of death among people living with HIV globally, yet TB is mostly preventable and curable. Reducing TB deaths in people living with HIV by 50% by 2015 is one of the 2015 global AIDS targets.
To give voice to TB and HIV affected communities around the world by sharing their experience and views on the way forward in the fight against the two diseases, a live web casted talk show took place during the International AIDS Conference entitled “Tuberculosis + HIV: Protecting the Vulnerable”.
The talk show was hosted by Jeanne Meserve, former CNN and ABC reporter, and Gerry Elsdon, the International Federation of Red Cross and Red Crescent Societies (IFRC) TB Goodwill Ambassador and a South African TV personality who suffered from tuberculosis in the past. The show brought together a dynamic group of women and young people who have suffered from tuberculosis and HIV, as well as the representatives of multilateral organizations such as the Stop TB Partnership, WHO, IFRC, the Global Fund to fight HIV/AIDS, TB and Malaria, and UNAIDS.
The talk show also featured video addresses by Archbishop Tutu, who himself is a former TB patient and Jorge Sampai, UN Secretary-General Special Envoy for Tuberculosis.
Panelists took the opportunity to highlight the need for a closer collaboration between HIV and TB programmes, and about the urgent need for better investment in TB research. They also emphasized the need to invest more in integrating TB screening, treatment and care into antenatal care and maternal and child health services in general. Children most frequently get TB infection from a close relative, usually their mother, thus preventing, diagnosing and treating TB in women will reduce the risk of TB infection and disease in children.
Ms Jan Beagle, UNAIDS Deputy Executive Director, Management and External Relations, spoke during the show and reiterated UNAIDS’s commitment to working with partners in support of the global target to halve TB deaths in people living with HIV by 2015. She underscored that “UNAIDS advocates for TB service providers to reach many who are the most vulnerable and at risk, but who have the greatest problems in accessing services – migrants, indigenous people, prisoners, sex workers and women and children affected by poverty, violence, stigma and discrimination.“
The talk show was organized by the Stop TB Partnership and the International Federation of Red Cross and Red Crescent Societies.
Multimedia
Multimedia
External links
External links
Related

Feature Story
More effective AIDS coordination at country level discussed at AIDS 2012
22 July 2012
22 July 2012 22 July 2012
L to R: UNAIDS Deputy Executive Director, Management and Governance, Ms Jan Beagle, Minister of Public Health, Democratic Republic of Congo, HE Felix Kabange, and the UNAIDS Director, Regional Support Team for Eastern and Southern Africa, Sheila Tlou.
Evidence indicates that coordination and governance of the HIV response have posed significant challenges for many countries. To review lessons learned and establish key principles for more effective coordination of the AIDS response, a meeting took place during the International AIDS Conference entitled Fit for purpose: striving for more effective AIDS coordination at country level.
The meeting brought together representatives of National AIDS Commissions, civil society organizations, regional bodies and development partner organizations to reflect and re-direct energies to explore what a truly country owned and accountable public sector governance body for HIV should look like.
Participants at the meeting took the opportunity to debate about the future of coordination of the AIDS response and to agree on key principles for a framework of effective response coordination, through shared responsibility and global solidarity.
The principles presented focused on, amongst other things, the need for governments to take the lead of the AIDS response in the context of shared responsibility and global solidarity, inclusion of multiple stakeholders in the AIDS response, cross learning between other areas of health, development and HIV programming, and development of AIDS programmes based on country priorities and local experience of what works to achieve maximum accountability.
Ms Jan Beagle, UNAIDS Deputy Executive Director, closed the meeting by urging the participants to celebrate the successes they have achieved so far in tackling AIDS, while also looking to what more can be done in order to ‘get to zero’ new infections, AIDS related deaths and AIDS related stigma and discrimination, using actions and mechanisms that will be sustained and owned by national stakeholders. She emphasized that the positive lessons from the last decade of AIDS coordination need to be brought into the discussion, especially how coordination structures and processes have boosted greater transparency, inclusion of non-governmental stakeholder and emphasized equity and human rights.
The meeting was organized by UNAIDS, together with the World Bank, the United Nations Development Program, the World Health Organization, the German Agency for International Cooperation and the Global Fund to Fight AIDS, TB and Malaria.
Related
 Building country-led sustainable HIV responses
Building country-led sustainable HIV responses

20 December 2024
 Cambodia social protection for people living with HIV
Cambodia social protection for people living with HIV

15 December 2023

Feature Story
Global Commission on Law urges countries to make the law work for HIV, not against it
11 July 2012
11 July 2012 11 July 2012
L to R: United States Congresswoman and member of the Global Commission on HIV and the Law, Barbare Lee; UNAIDS Executive Director Michel Sidibé; Deputy Secretary-General of the United Nations Jan Eliason; UNDP Administrator Helen Clark; and His Excellency Festus Mogae, former President of Botswana and member of the Global Commission on HIV and the Law.
Credit: D.Lowthian
The Global Commission on HIV and the Law launched its landmark report on 9 July 2012 at UN Headquarters in New York. The new report denounces the detrimental impact that punitive laws have on human rights and the HIV response and makes bold recommendations for addressing them.
“Never before has there been such an examination of the role of law in HIV,” said Festus Mogae, Former President of Botswana and member of the Commission. “What we have found is an epidemic of bad laws that is costing lives. We must end the epidemic of bad laws and enact laws based on evidence, common sense and human rights,” added Mr Mogae.
Stigma, discrimination and punitive legal approaches have long been recognized as barriers to the HIV response. They heighten vulnerability to HIV especially among key populations at higher risk of infection and make it difficult for individuals and communities to access HIV prevention, treatment, care and support services. UNAIDS has long called for the removal of punitive laws and their replacement with protective ones. Yet, countries across the world still maintain laws, policies and practices that infringe upon human rights, fuel discrimination and prevent global and national efforts to address HIV.
Speaking at the launch of the report, UNAIDS Executive Director Michel Sidibé noted that “the strength of this report is that it goes beyond a superficial description of stigma and discrimination to question the legal and structural fabrics that sustains inequality, injustice and human rights violations in the context of HIV”.
The report titled “HIV and the Law: Risks, Rights and Health” is a result of a two-year consultative process during which the Commission received more than 1 000 submissions from people affected by laws, law enforcement and access to justice issues in the context of HIV. The report took into account recommendations from 7 regional dialogues involving governments and civil society, and the input from a Technical Advisory Group of experts on HIV and the law.
Punitive laws increase risk of HIV infection
The Commission—an independent group of political and social leaders from around the world—pointed out that women in many parts of the world are governed by plural legal systems where traditional and customary law perpetuates their social and economic inequality. This situation makes women vulnerable to relationships and/or sexual violence which put them at risk of HIV infection. The Commission described the realities of many pregnant women living with HIV who face discrimination in health care including forced sterilization, even though simple and inexpensive medicine can prevent mother-to-child HIV transmission and keep mothers alive.
In the report, Commissioners called on governments to use the law to protect women from inequality and violence. They also urged governments to end legal barriers that prevent young people from accessing HIV information and services, as well as sexuality education—all necessary to avoid HIV infection.
The Commission also called for the removal of laws that criminalize people on the basis of their sexual orientation and gender identity, possession of drugs for personal use, and engagement in adult consensual sex work. It cited extensive evidence of how such criminal laws exacerbate risk of HIV infection among men who have sex with men, transgender people, people who use drugs and adults who sell and buy sex. According to the report, such laws drive people underground and into the margins of society away from health and HIV services. Furthermore, if convicted and sent to prison, the risks of contracting HIV, TB and Hepatitis C are very high because, in many countries, laws prohibit the provision of health and HIV prevention services and commodities in prisons.
We must end the epidemic of bad laws and enact laws based on evidence, common sense and human rights
Festus Mogae, Former President of Botswana and member of the Global Commission on HIV and the Law
Nick Rhoades from the Center of HIV Law and Policy spoke against the criminalization of HIV exposure and transmission, having himself been convicted in the United States of America, even though he had used condoms, had an undetectable viral load and did not transmit HIV. Citing the many HIV specific criminal laws, he said: “People have hands and can hit each other with their fists, but you don’t see a law specifically criminalizing a hand as a ‘deadly weapon’ like HIV is.” The Commission has called for the criminal law to be strictly limited to the malicious and intentional acts of actual transmission of HIV.
Participants at the launch highlighted how punitive legal approaches are undermining the investment in HIV prevention and treatment that is finally beginning to show the real possibility of halting and reversing the epidemic. They underlined that the persistence of punitive laws and practices is a serious concern at a time when the world has stabilized new HIV infections, increased its knowledge on effective HIV prevention and is preparing to harness the full potential of expanded HIV treatment. “It is outrageous that in 2012, when we have everything we need to beat this epidemic, we still must fight prejudice, discrimination, exclusion and bad laws,” said Mr Sidibé.
Law as an instrument to protect individuals
Commissioners at the launch underlined that there are many positive examples of countries that have used the law as an instrument to protect individuals, to create an environment that addresses stigma and violence thus encouraging access to HIV services. Other countries have used the law to challenge overly broad and stringent intellectual property regimes to reduce the cost of essential HIV medicines and to ensure their availability including through the production of generics.
“Law reform is complex, but countries can do much more,” said UNDP Administrator Helen Clark. “The task before us is to ensure better laws are adopted and enacted,” she added.
The Commission and its work have started dialogues across the world on issues that are difficult, controversial and complex. They are also issues that are central to human dignity, health and social justice. These dialogues are part of what Governments committed to do in the 2011 Political Declaration on AIDS where they pledged to review laws and policies that “adversely affect the successful, effective and equitable delivery of HIV services and consider their review”.
“We now have a powerful tool for advocacy and engagement to ask governments to uphold human rights for all people vulnerable to HIV,” said Ebony Johnson of the Athena Network. “This report should not be shelved.”
The Global Commission on HIV and the Law is an independent body, convened by the United Nations Development Programme (UNDP) on behalf of the Joint United Nations Programme on HIV/AIDS (UNAIDS). The Commission was supported by a Technical Advisory Group, which reviewed and analyzed existing public health and legal evidence and also commissioned original analysis. Additional information on the Commission, its processes and work is available at www.hivlawcommission.org.







