West and Central Africa


Update
Young women more affected by HIV than young men in western and central Africa
18 June 2019
18 June 2019 18 June 2019In western and central Africa, survey data suggest that HIV prevalence among women aged 20−29 years is higher than that among men of the same age in all countries, and between five and nine times higher in some countries, including Côte d’Ivoire, the Gambia and Ghana. However, by the time they are 40−49 years old, men have similar HIV prevalence; exceptions to this are in the Democratic Republic of the Congo, Ghana and Gabon, where HIV prevalence among women is still almost twice as high in that age range.
The difference in HIV prevalence between men and women in the 20−29-year age group in western and central Africa is greater than that observed in eastern, and some southern, African countries. Possible reasons for this difference include the high rates of voluntary medical male circumcision in western and central Africa, which has been shown to have a 60% protective effect on female-to-male HIV transmission. Other possible reasons for the difference in western and central Africa might be the very low use of condoms and low uptake of antiretroviral therapy among men in the region.
Related information
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


Press Statement
UNAIDS congratulates Michel Sidibé on his appointment as Minister of Health and Social Affairs of Mali
08 May 2019 08 May 2019UNAIDS extends its heartfelt thanks to the Executive Director of UNAIDS for his outstanding contribution to the global response to HIV
GENEVA, 8 May 2019—UNAIDS congratulates Michel Sidibé on his appointment as the Minister of Health and Social Affairs of Mali. Mr Sidibé served as the Executive Director of UNAIDS for more than 10 years after being appointed as the second Executive Director of UNAIDS and Under-Secretary-General of the United Nations in January 2009.
A true champion for a people-centred approach to health and development and a strong advocate for social justice, Mr Sidibé has made a remarkable contribution to the AIDS response, helping to save and improve the lives of millions of people around the world.
Since Mr Sidibé took up his position as Executive Director of UNAIDS, there has been a 170% increase in the number of people accessing antiretroviral therapy, from 8 million in 2010 to 21.7 million in 2017. There has also been a 45% drop in AIDS-related deaths—from 1.7 million in 2008 to 940 000 in 2017—and new HIV infections have been reduced by 22%—from 2.3 million in 2008 to 1.8 million in 2017.
“It has been an honour for me to serve UNAIDS as its Executive Director and contribute to the global AIDS response,” said Mr Sidibé. “I would like to thank all UNAIDS partners and staff and especially community members affected by HIV, who have made our successes possible. With their steadfast commitment and resolve, we have been able to bring life-saving services to millions of people. If we stay the course and do the right thing, always—putting people first and delivering results for people—we will succeed in ending AIDS.”
Mr Sidibé’s vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths, and his tireless advocacy to ensure that all people have access to health services, have kept HIV at the top of the global agenda. His calls for global solidarity and shared responsibility have seen resources for HIV increase by more than one third, from US$ 15.9 billion in 2010 to US$ 20.6 billion in 2017 in low- and middle-income countries. His advocacy for country ownership helped to ensure that 56% of HIV resources in low- and middle-income countries now come from domestic sources, promoting long-term sustainable responses to HIV.
His commitment to the concept of universal access to HIV prevention, treatment, care and support meant that the goal of reaching 15 million people living with HIV with antiretroviral therapy by 2015 was achieved seven months ahead of schedule. His focus on the most vulnerable and marginalized has given a voice to the voiceless, including gay men and other men who have sex with men, sex workers, transgender people, people who inject drugs, prisoners and other incarcerated people, and people on the move.
A strong believer that no child should be born with HIV, his leadership in calling for the elimination of new HIV infections among children contributed to a 60% reduction in new paediatric HIV infections since 2009 in the 21 priority countries of the Global Plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive.
During his tenure, Mr Sidibé spearheaded two of the most successful United Nations General Assembly political declarations on HIV, which named key populations and included ambitious regional and global Fast-Track Targets. He has successfully advocated to take AIDS out of isolation, encouraging a holistic human-rights based approach to include HIV as part of sexual and reproductive health and integrate responses to interlinked diseases, including tuberculosis and cervical cancer.
“I would like to thank United Nations Secretary-General António Guterres for his long-standing support to UNAIDS,” said Mr Sidibé. “I am also grateful to the United Nations system for allowing me to develop my career, from when I started as a short-term junior professional in the Democratic Republic of the Congo for the United Nations Children’s Fund in 1987 to becoming Under-Secretary-General of the United Nations some 20 years later—I am eternally thankful for the opportunities I have been given.”
The countries most affected by HIV have rallied behind Mr Sidibé’s call to reach the 90–90–90 targets, whereby 90% of people living with HIV know their status, 90% of people who know their status are accessing treatment and 90% of people on treatment have a suppressed viral load. Some 75% of all people living with HIV now know their HIV status, and focus has been increased on HIV testing and expanding antiretroviral therapy.
His call with partners to establish an HIV prevention coalition led to a new HIV Prevention 2020 Road Map to strengthen and sustain political commitment for primary HIV prevention and establish accountability for delivering services at scale in order to stop new HIV infections.
His commitment to improving the lives of women and girls galvanized action for Security Council resolution 1983 in 2011, which focused on ensuring access to HIV prevention and treatment for women and girls, on the prevention of, and response to, sexual violence related to conflict and on post-conflict peacebuilding.
Mr Sidibé’s strong belief in the power of communities has paved the way for community-led responses to HIV, which have proved to be a gamechanger in increasing the uptake of HIV services and in creating support networks to improve adherence to treatment and quality of life for people living with HIV.
His undeterred commitment, dedication and passion has allowed Mr Sidibé to engage heads of state, people living with HIV, affected communities, donors, first ladies, parliamentarians, Mayors, civil society, scientists, young people and HIV programme leaders alike, bringing everyone around the same table to galvanize action to end AIDS by developing focused and sustainable solutions that leave no one behind.
Mr Sidibé has been an inspirational leader of UNAIDS and for the global response to HIV, and UNAIDS extends its heartfelt thanks for his years of dedicated service. Mr Sidibé will take on his new role as Minister of Health and Social Affairs of Mali with immediate effect and will be replaced ad interim by UNAIDS Deputy Executive Director, Management and Governance, Gunilla Carlsson.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
Sophie Barton-Knotttel. +41 22 791 1697 / +41 79 514 6896
bartonknotts@unaids.org
UNAIDS Media
tel. +41 22 791 42 37
communications@unaids.org
Press centre
Download the printable version (PDF)
Region/country




Feature Story
Urgent action needed to address HIV in Haut-Mbomou, Central African Republic
15 April 2019
15 April 2019 15 April 2019On the border between South Sudan and the Democratic Republic of the Congo, Haut-Mbomou is the province worst hit by HIV in the Central African Republic, with HIV prevalence at 11.9% compared to a national average of 4%.
Initially spared by the conflict that engulfed the country in 2013 and 2014, since 2018 Haut-Mbomou has seen fighting between rival armed groups, continued insecurity and a large-scale displacement of people. More than 47 000 people have been displaced by insecurity and violence in the province, adding to a population of some 3500 refugees from South Sudan and the Democratic Republic of the Congo.
Alerted by accounts of persistent medicine stock-outs, substandard care for people living with HIV and barriers to access to HIV and health services owing to insecurity, a joint mission of the Central African Republic Ministry of Health, the National AIDS Council, the World Health Organization, the Office of the United Nations High Commissioner for Refugees and UNAIDS visited Haut-Mbomou from 8 to 12 April. Located 1000 km from the capital, Bangui, the province is among the most underserved by health and social services. Half of the health facilities in the province are closed owing to a lack of personnel or rundown facilities.
In the towns of Obo and Zemio, the mission met with local authorities, health-care providers, religious and community leaders, internally displaced people, refugees and people living with HIV. “This joint mission brings together the breadth of national and United Nations expertise to offer practical solutions to the challenges of HIV and health in this critical province,” said Patrick Eba, UNAIDS Country Director for the Central African Republic.
The mission noted the impact of insecurity on the population and on access to health and other services. The main routes of supply are closed and violence outside the urban centres greatly limits access to medicines, food and other essential commodities.
The Obo District Hospital, the main health-care facility in the province, lacks basic laboratory testing equipment, including for blood safety or tuberculosis screening. Access to antiretroviral medicines is greatly limited by regular stock-outs. The absence of CD4 count measurement, viral load testing and other biological tests for people on antiretroviral therapy limits the quality of care for host populations and refugees. The mission was also concerned by the absence of HIV prevention and sensitization efforts, including the unavailability of condoms.
“How can we live in dignity when we face constant stock-outs of antiretroviral therapy and the hospital staff treat us badly? Many people who are on treatment are sick with opportunistic infections, but the hospital cannot give us anything,” lamented a frail, middle-aged woman living with HIV in Obo, who also bravely spoke out against discrimination.
Access to food is increasingly a problem because insecurity limits farming, fishing and hunting and hinders the ability of humanitarian agencies to deliver nutritional support. For vulnerable people living with HIV, including refugees and displaced people, access to food and nutritional support is essential for antiretroviral medicine adherence and effectiveness.
In Zemio, the mission spoke with members of community groups established by Médecins Sans Frontières as part of an innovative programme to facilitate access to antiretroviral medicines. Group leaders collect and dispense antiretroviral medicine to members who live far from hospitals. The group members highlighted that barriers to their access to medicines included roadblocks, insecurity and extortion by armed groups. The mission held a dialogue with communities and leaders of the main armed group in Zemio to emphasize the need for unhindered access to health-care facilities.
The mission showed the complex nature of the challenges facing the HIV response in a context such as that in the Central African Republic, which is characterized by insecurity, population displacement and a collapsed health-care system. Those challenges call for urgent attention and action on the part of the government, the United Nations and others to address emerging and chronic health and HIV challenges. “Addressing these challenges is essential to show that these populations are not forgotten” said Wilfrid Sylvain Nambei, the Minister Coordinateur of the National AIDS Council. “Swift action following this mission will reinforce confidence in the government and its partners and it will advance our efforts to build peace, reconciliation and reconstruction that leaves no one behind.”
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025



Feature Story
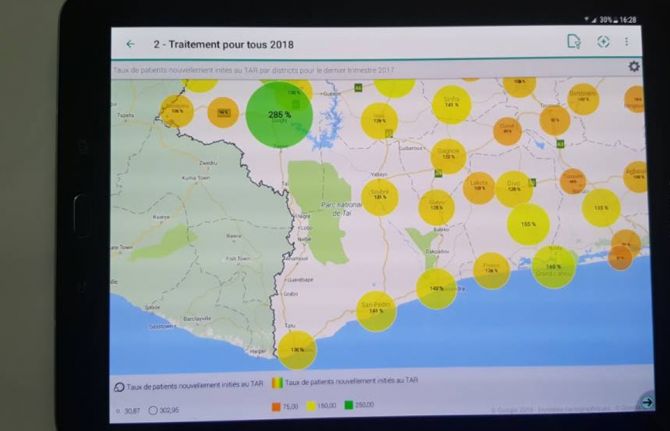
Côte d’Ivoire signals renewed will to tackle issue of user fees for HIV services
16 April 2019
16 April 2019 16 April 2019The Government of Côte d’Ivoire has signalled its commitment to stop people being charged for accessing HIV testing and treatment services, declaring that it will strictly apply previously announced decisions to prevent people living with or affected by HIV being asked to pay user fees.
A note circulated by the Ministry of Health has reminded all service providers that costs for HIV testing and treatment services should not be charged to people accessing those services. The directive applies for all services for pregnant and breastfeeding women, all HIV testing services, tests for viral load suppression and the prescription of antiretroviral medicines for people living with HIV.
The directive also reminds service providers that children under the age of 15 years should have free access to health services and that young women aged 15–24 years should have free access to primary health care, HIV testing and family planning services.
In several countries, the issue of user fees has been identified as a major barrier to testing people for HIV, to treating people living with HIV and to retaining people in treatment and care.
The renewed commitment of Côte d’Ivoire to confront the issue of user fees followed discussions between the President of Côte d'Ivoire, Alassane Ouattara, and the former President of Botswana, Festus Mogae, who visited the country in March in his capacity as Chairperson of the Champions for an AIDS-Free Generation in Africa.
Following their discussions, the government also announced its intention to increase domestic funding for the AIDS response by US$ 10 million in the next budget.
During his meeting with the President, Mr Mogae congratulated Mr Ouattara and the First Lady, Dominique Ouattara, for their personal commitment to ending the AIDS epidemic as a public health threat by 2030. Ms Ouattara is UNAIDS Special Ambassador for the Elimination of Mother-to-Child Transmission and the Promotion of Paediatric Treatment of HIV.
At the conclusion of his mission, Mr Mogae underlined the importance of accelerating the response to the epidemic. “We cannot be complacent and allow the huge improvements that we have made so far to be lost. If we stop now, we will lose everything we have already invested and achieved. The entire nation must be mobilized to ensure that no one is left behind,” he said.
There were 500 000 people living with HIV in Côte d’Ivoire in 2017, with around 46% accessing HIV treatment.
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


Feature Story
Liberia’s catch-up plan takes shape
27 March 2019
27 March 2019 27 March 2019The HIV epidemic continues to have a profound humanitarian and public health impact in western and central Africa, a region that risks being left behind in the global response to ending the AIDS epidemic. In July 2017, the African Union endorsed a regional catch-up plan for western and central Africa that seeks to rapidly accelerate access to HIV treatment and close the gap between African regions. National catch-up plans have been established in 18 countries in western and central Africa, including in Liberia.
It is estimated that in 2017, 40 000 people were living with HIV in Liberia, including around 3000 children aged 0–14 years. Fewer than one in three adults aged 15–49 years who are living with HIV have access to medicines that would keep them well and stop them passing on the virus to other people. For children, the situation is even more challenging, with just 18% on treatment.
However, there are encouraging signs that Liberia is scaling up its response to the HIV epidemic and adopting best practice programmes and policies to ensure the delivery and take-up of HIV testing, treatment and prevention services. Under the leadership of the Ministry of Health and the National AIDS Commission of Liberia, a Fast-Track plan for 2019–2020 has been developed that identifies high-impact programmes to accelerate the response, the urgent need for adjustments to existing programmes and barriers that must be removed in order to ensure better service delivery. It also recognizes that prevention measures must be reinforced and that stigma and discrimination associated with the virus must be reduced.
The Liberia catch-up plan seeks to triple the country’s test and treat figures, whereby people who test positive for HIV are immediately referred for treatment. The catch-up plan is guided by a location–population approach, with a service delivery bias towards the three counties with the highest unmet need for HIV testing, treatment and care services, urban areas and some other locations. Services are oriented towards adults aged 15–49 years, especially to pregnant women and to groups at higher risk, such as gay men and other men who have sex with men, sex workers, people who inject drugs, prisoners and mine workers. Infants exposed to the virus during pregnancy and breastfeeding are also a priority.
The plan also aims to tackle the low take-up of services by men.
“We are designing interventions that will encourage more men to test and know their status. Of those tested so far, 80% are women,” said the National AIDS Commission of Liberia Chair, Theodosia Kolle. “Stigma remains a major issue in Liberia.”
UNAIDS played a significant role in helping to draft the catch-up plan, mobilizing stakeholder involvement and ensuring that people living with HIV, civil society and members of key populations were included in order to shape its design. Around 70 people took part in a special two-day workshop in March to craft the necessary political and programmatic measures to improve service delivery, enhance community mobilization, increase funding and enable a more efficient use of existing resources and an improved monitoring and evaluation system.
The workshop was also an opportunity to validate the Global AIDS Monitoring (GAM) report for 2019 for Liberia. GAM is the world’s most extensive data collection on HIV epidemiology, programme coverage and finance and publishes the most authoritative and up-to-date information on the HIV epidemic—vital for an effective AIDS response.
“With teamwork we can reach the 2020 Fast-Track Targets as long as we prioritize and implement high-impact programmes,” said Miriam Chipimo, UNAIDS Country Director for Liberia.
The 90–90–90 targets included in the Fast-Track approach are that, by 2020, 90% of all people living with HIV will know their status, 90% of all people living with HIV will have access to antiretroviral therapy and 90% of all people on antiretroviral therapy will have viral suppression.
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025




Feature Story
The road to NAIIS: UNAIDS’ role in better understanding Nigeria’s HIV epidemic
22 March 2019
22 March 2019 22 March 2019After six months of data collection and three months of data analysis, the President of Nigeria, Muhammadu Buhari, announced the results of the Nigeria HIV/AIDS Indicator and Impact Survey (NAIIS) in March 2019. Costing approximately US$ 100 million and covering more than 200 000 people, 185 survey teams collected data for the NAIIS, the largest HIV-specific survey in the history of the global response to the epidemic.
In Nigeria, three types of survey have been conducted by the Federal Ministry of Health HIV/AIDS Division to determine HIV prevalence and to monitor the trends of the HIV epidemic in the country:
- The HIV Sentinel Survey (HSS), which is conducted typically every two to three years among women attending antenatal clinics, which determines HIV prevalence among pregnant women.
- The National Reproductive Health Survey (NARHS), which is conducted every five years among the general population.
- The Integrated Biological and Behavioural Surveillance Survey (IBBSS), which is mostly used to monitor prevalence and behavioural trends among key populations.
The last HSS and IBBSS took place in 2014, while the last NARHS took place in 2012. These data sources have served as the main survey data sources for the AIDS response in the country.
Between 2012 and 2014, significant progress was made in the AIDS response in Nigeria. The number of antiretroviral therapy sites doubled, prevention of mother-to-child transmission sites increased eightfold and HIV counselling and testing sites increased fourfold. According to government data, 6.7 million adults were counselled and tested for HIV in 2014, a 65% increase from the previous year. HIV testing among pregnant women also doubled in 2014 compared to 2013. Similarly, the number of people living with HIV on antiretroviral therapy increased significantly.
However, despite this progress, there was no commensurate improvement in the statistics on the coverage of antiretroviral therapy among people living with HIV. National achievements in the AIDS response were poor compared to the targets, and programme implementers reported difficulties in identifying people living with HIV in need of services. It was therefore suggested that the HIV burden was not as high as was estimated using the available HIV prevalence data.
Former UNAIDS Country Director Dr Bilali Camara was a longstanding advocate for an expansion of the surveillance of the country’s epidemic.
“Working as UNAIDS Country Director in Nigeria, I realized early on that we did not have the full picture of the country’s AIDS epidemic,” said Dr Camara. “I was pushing for surveillance to be expanded for a long time―I am very happy that with this new survey we now have a better understanding of the AIDS epidemic in Nigeria and that it will allow us to better respond to the areas and people in most need.”
Dr Camara’s persistence indeed paid off.
In July 2015, the National Agency for the Control of AIDS (NACA), under the leadership of its then Director-General, Professor John Idoko, decided that it was imperative to better understand Nigeria’s HIV epidemic. The NACA set up a National Stakeholder Committee, comprising the head of the National AIDS and STI Control Programme, the UNAIDS Country Director, the World Health Organization (WHO) representative, the United States President’s Emergency Plan for AIDS Relief (PEPFAR) Coordinator, civil society and others, which decided to conduct a triangulation of data from various sources.
“The need for the survey was first initiated under my leadership, but we had overwhelming support from Dr Camara. UNAIDS headquarters was even willing to send its Strategic Information Director to Nigeria at the time,” said Professor Idoko.
Many countries have shifted to a location–population approach, which helps to ensure that HIV services reach the people and geographic areas with the greatest need. Location–population approaches require granular-level data, which were not typically available in Nigeria. In 2016, the UNAIDS Nigeria Strategic Information Team, led by Dr Gatien Ekanmian, was tasked to develop an evidence-informed methodology to estimate the HIV burden at the local level. During this process, a closer analysis of the results from the various surveys highlighted a series of issues with the HSS surveys:
- The sentinel sites were too limited in number to ensure nationally representative geographic coverage based on the demographics of the country.
- Urban sites were oversampled.
- Rural sites were usually under-sampled.
- There were often more urban sites than rural sites in many states, thus the HSS results reflect more the urban HIV epidemic than the rural epidemic among pregnant women.
The conclusion of the UNAIDS Nigeria epidemiological analysis was that the HSS and NARHS were no longer giving sufficiently precise epidemiological information. It was recommended that a comprehensive review of the HIV surveys being conducted in Nigeria be carried out in order to address the shortcomings in the existing survey approaches and methodology.
Thereafter, the UNAIDS country office met with various stakeholders, including the Development Partners’ Group on HIV, and presented these observations and recommendations, effectively utilizing the Development Partners’ Group on HIV to galvanize support from PEPFAR and the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) in particular.
In June 2016, the Director-General of the NACA raised an objection to the latest estimate of 3.5 million Nigerians living with HIV, believing that the figure was an overestimation. He had the opportunity to discuss his concerns with UNAIDS country directors, Dr Erasmus Morah and Dr Alti Zwandor at the International AIDS Conference in Durban, South Africa, in 2016. In July 2016, after advocacy from the UNAIDS country office, the new Minister for Health, Professor Isaac Adewole, and the new Director-General of the NACA, Dr Sani Aliyu, agreed on the need for an epidemiologically robust population-based HIV survey in Nigeria. They approved the recommendations for a population-based survey and committed to mobilize resources for it.
“When I resumed as Director-General of the National Agency for the Control of AIDS, a recurring issue that came up at every introductory meeting with partners was the difficulty in finding new cases. It was obvious that there was a problem with case-finding. Was this because we were looking in the wrong places? I had doubts on the quality data we had … and we can’t achieve epidemic control if we don’t even know where we are. Hence, the number one priority of my administration was born―establishing the true prevalence of HIV in Nigeria by employing the best scientific and technical survey tools available in the shortest possible time,” said Dr Aliyu.
In November 2016, a review and triangulation of HIV data in Nigeria was commissioned by the NACA, in collaboration with UNAIDS, the findings of which gave further support for a national survey to develop more precise estimates of HIV prevalence. Firm support for the survey came from the Government of the United States of America (the Centers for Disease Control and Prevention, PEPFAR, USAID and the Department of Defense) and the Global Fund, which committed funding to the NAISS.
“It was easy to see that getting the data situation in Nigeria right was not only the right thing to do but also the dream of so many people. Fortunately, Nigeria had great partners to help turn this dream into reality. Programming and accounting for HIV results in the country will never be the same,” said Dr Morah, the current UNAIDS Country Director for Nigeria.
The United Nations system’s contributions in the NAIIS Technical Committee were anchored by UNAIDS, WHO and the United Nations Children’s Fund. Before the results of the survey were announced, Peter Ghys, UNAIDS Director of the Strategic Information Department, led a multi-group technical mission to Nigeria. The team gave advice on the use of the survey results, on the trends and the geographic locations of the epidemic, at the national and subnational levels. They also gave technical guidance to national partners on data management and governance, including on a strategy for country ownership and leadership of the survey results and support on how to communicate the changes in the epidemiological profile of HIV in the country.
“The road to NAIIS is a wonderful and brilliant story to tell, because it actually tells the story of the HIV response in Nigeria,” said Professor Adewole.
This feature is adapted from an article written by Erasmus U. Morah, Gatien K. Ekanmian and Doris, A.Ogbang
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025







Feature Story
Helping the forgotten generation
02 April 2019
02 April 2019 02 April 2019Towering over a throng of young people, Christine Kafando peppers the crowd with questions.
“Do you feel pressure from other boys and girls?” “Do you feel abandoned because of poverty?” “Do you have all the information you need regarding your health and HIV? If not, ask me, ask your partners, ask! Okay!”
The 40 boys and girls nod and shrug. They have come for a workshop run by the Association Espoir pour Demain (AED) in Bobo-Dioulasso, Burkina Faso, which aims to create a space for young people to learn about sexual health and to train some to become peer educators.
“After having seen a number of young students come to us pregnant, we felt a need to start these workshops,” Ms Kafando, the founder of AED, said.
Issa Diarra said the workshop enabled a dialogue. “In our society, we really don’t talk that much about sex and, I would add, health issues, but here we really had the chance to discuss all that,” he said. Another attendee of the workshop, Roland Sanou, agreed, “Sex today remains taboo for young people, but I don’t want it to stay that way.”
Many of them say times have changed and that the way they think is different from the way their parents thought. “Currently, we young people are aware and we know what we want and we know that being sick can keep us from realizing our dreams, so that’s why we are rallying,” said Baba Coulibaly.
At the beginning, AED helped women living with HIV to access treatment. It then grew to help mothers and their babies born with HIV. Fifteen years later, many of those children are now teenagers and still drop by. Reflecting on her two decades as an HIV advocate, Ms Kafando said, “For so many years, women have been the face of HIV, but it’s key to include men and boys to raise their awareness.”
Jacinta Kienou, a nurse who has been at the association since it was founded, said that there were two big challenges: a number of young people living with HIV no longer take their treatment regularly and many young people are unsure about how to deal with relationships.
“Because they live with HIV, and they are young, lots of problems bubble up concerning affection and acceptance by others with regard to their HIV status,” she said. “Often relationships end because of someone’s HIV status. We council them and their parents at that time,” she added.
In Burkina Faso, young people make up more than 60% of the population and data show that many of them do not know their HIV status. UNAIDS Strategic Information Officer André Kaboré describes two gaps concerning young people. “Despite high-quality treatment being readily available, there are children out there who don’t know they’re living with HIV. Worse, many of those who do know that they are living with HIV aren’t accessing treatment,” he said.
In the country, 94 000 people are living with HIV, 9400 of whom are children under the age of 15 years. While 65% of adults living with HIV are on life-saving antiretroviral therapy, only 28% of children living with HIV whose status is known, about 3500, are on treatment. Ms Kafando calls them the forgotten generation. “They fell through the cracks because until now they had never been sick or needed attention and thus were never tested for HIV,” she said.
The head of the National AIDS Council for Bobo-Dioulasso and the surrounding region, Suzanne Sidibé, said, “We lost sight of children born with HIV. Our aim, with the help of the Association Espoir pour Demain, is to fan out to families through health mediators.”
Hoho Kambiré, who is living with HIV, has four children, two of whom are living with HIV. As an AED health mediator, she speaks about the benefits of knowing one’s status to all who will listen. She visits families, accompanies women to clinics and provides support.
“It is necessary to test all the children to know who is sick and who is not sick and follow up to keep them healthy,” she said. AED has now more than 50 health mediators, mostly women like Ms Kambiré, who originally came to the association seeking health services herself.
The United Nations Children’s Fund (UNICEF) and UNAIDS both support AED financially. Mireille Cissé, a UNICEF HIV specialist, said that the United Nations in Burkina Faso had identified the top priorities for the AIDS response in the country, including working with civil society.
“We agreed that a community link needed to be established, because they are our entry into families,” she said. UNICEF formalized the health mediators’ contribution by providing a stipend for their work and works hand in hand with the regional office of the Ministry of Health.
“A real victory for us was to have the health mediators integrated into the health teams of the districts,” Ms Cissé said. “That buy-in really facilitated the role of the health mediators and has raised their profile.”
UNAIDS has reinforced the capacity of the health mediators to widen their scope of work, which ranges from psychosocial counselling to training on treatment adherence. “To maintain our progress in the HIV response and end AIDS depends a lot on civil society like the Association Espoir pour Demain,” Job Sagbohan, UNAIDS Country Director, said. “We really hope for maximum impact.”
Special page
Region/country





Feature Story
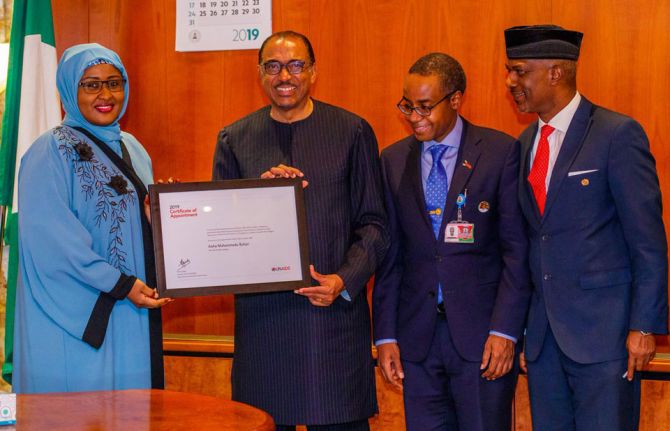
Nigeria adapts strategy to end the AIDS epidemic
20 March 2019
20 March 2019 20 March 2019Nigeria has adopted its Revised National HIV and AIDS Strategic Framework 2019–2021 to guide the country’s future response to HIV. It follows the results of a new survey that shows that HIV prevalence in the country stands at 1.4%. Previous estimates had indicated Nigeria’s HIV prevalence at 2.8%.
The results of the Nigeria National HIV/AIDS Indicator and Impact Survey (NAISS) were unveiled at a special event held in Abuja, Nigeria, on 14 March that was attended by the President of Nigeria, Muhammadu Buhari, and the Executive Director of UNAIDS, Michel Sidibé. During his speech, Mr Sidibé commended the president’s leadership in guiding the country’s response to the HIV epidemic. Nigeria has tripled the number of people on HIV treatment since 2010 and adopted a test and treat policy in 2016.
The improved understanding of the country’s epidemic based on the survey results will allow for more efficient investments in the response to HIV and a more effective planning for the provision of HIV prevention, care and treatment services. It will permit the adoption of a population–location approach to deliver services to the people in the areas where they are needed the most.
During his three-day visit to Nigeria, Mr Sidibé met the Minister of Health, Isaac F. Adewole, to discuss progress, gaps and challenges in the AIDS response and pledged UNAIDS’ support to Nigeria in the implementation of the new framework. This was further underscored when Nigeria’s Minister of Foreign Affairs, Geoffrey Onyeama, and Mr Sidibé signed a new cooperation agreement to strengthen the relationship between UNAIDS and Nigeria.
Mr Sidibé also paid a courtesy call on the wife of the country’s president, Aisha Buhari, to formalize and extend her appointment as the UNAIDS Special Ambassador for the Elimination of Mother-to-Child Transmission of HIV and the Promotion of Treatment for Children Living with HIV in Nigeria.
Ms Buhari thanked UNAIDS for extending her mandate and reiterated her commitment to achieving an AIDS-free generation of children.
“This will enable me to contribute more towards ensuring that no child is born with HIV in Nigeria,” said Ms Buhari.
Representatives of the Network of People Living with HIV/AIDS in Nigeria also met with Mr Sidibé to voice their concerns about the gaps and challenges in the country’s AIDS response.
The network’s national coordinator, Abdulkadir Ibrahim, said services were too often not reaching the people in the greatest need. He asked for UNAIDS’ help in strengthening community responses to the HIV epidemic and to ensure that people living with HIV, particularly young people, were involved in creating policies and programmes that affected their health and well-being.
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


Press Release
New survey results indicate that Nigeria has an HIV prevalence of 1.4%
14 March 2019 14 March 2019Expanded data collection and analysis provides better understanding of HIV epidemic in Nigeria
ABUJA/GENEVA, 14 March 2019—Results released today by the Government of Nigeria indicate a national HIV prevalence in Nigeria of 1.4% among adults aged 15–49 years. Previous estimates had indicated a national HIV prevalence of 2.8%. UNAIDS and the National Agency for the Control of AIDS estimate that there are 1.9 million people living with HIV in Nigeria.
Speaking in Abuja, Nigeria, the President of Nigeria, Muhammadu Buhari, welcomed the news that there are fewer people living with HIV in the country than previously estimated and launched the Revised National HIV and AIDS Strategic Framework 2019–2021, which will guide the country’s future response to the epidemic. Nigeria has made good progress in scaling up HIV treatment and prevention services in recent years.
"For the first time, the end of AIDS as a public health threat by 2030 is truly in sight for our country,” said H.E. Muhammadu Buhari, President of Nigeria. “I urge all of us not to relent but to increase the momentum. Let us work collectively and push for the last mile.”
The data from the Nigeria National HIV/AIDS Indicator and Impact Survey (NAIIS) are based a revised and enhanced methodology. The survey provides a clearer understanding of Nigeria’s HIV epidemic and shines a light on progress and the remaining gaps and challenges.
The Executive Director of UNAIDS, Michel Sidibé, welcomed the new estimates and said the improved understanding of the country’s HIV epidemic would allow Nigeria to better reach people living with HIV and people at higher risk of acquiring HIV.
“I commend the Government of Nigeria and its partners for conducting this ambitious survey, which provides us with a much better understanding of the country’s HIV epidemic,” said Mr Sidibé. “While it is fantastic news that there are fewer people living with HIV in Nigeria than previously thought, we must not let down our guard. Let us use the results of this survey to better focus our delivery of HIV prevention, treatment and care services to the people in the greatest need and ensure that Nigeria gets on track to end the AIDS epidemic by 2030.”
While Nigeria’s national HIV prevalence is 1.4% among adults aged 15–49 years, women aged 15–49 years are more than twice as likely to be living with HIV than men (1.9% versus 0.9%.) The difference in HIV prevalence between women and men is greatest among younger adults, with young women aged 20–24 years more than three times as likely to be living with HIV as young men in the same age group. Among children aged 0–14 years, HIV prevalence according to the new data is 0.2%. Significant efforts have been made in recent years to stop new HIV infections among children.
At the national level, viral suppression among people living with HIV aged 15–49 years stands at 42.3% (45.3% among women and 34.5% among men). When people living with HIV are virally suppressed they remain healthy and transmission of the virus is prevented.
The improved understanding of the country’s HIV epidemic will allow for more efficient investments in the response to HIV and more effective planning for the provision of HIV prevention, care and treatment services, including a focus on key populations, such as female sex workers. It will permit the adoption of a population–location approach to deliver services to the people and areas where they are most needed.
The new data differentiate HIV prevalence by state, indicating an epidemic that is having a greater impact in certain areas of the country. The South-South zone of the country has the highest HIV prevalence, at 3.1% among adults aged 15–49 years. HIV prevalence is also high in the North Central zone (2.0%) and in the South East zone (1.9%). HIV prevalence is lower in the South West zone (1.1%), the North East zone (1.1%) and the North West zone (0.6%).
“The Nigeria National HIV/AIDS Indicator and Impact Survey (NAISS) findings provide Nigeria with an accurate national HIV prevalence measure of 1.4%. NAIIS also showed we are able to effectively provide antiretroviral treatment,” said Isaac F. Adewole, Nigeria’s Minister of Health. “Everyone infected with HIV needs to get treatment so they can achieve viral suppression, especially pregnant women. We must ensure pregnant women have access to antenatal services and are tested during every pregnancy. We know we can support HIV-positive mothers, hence ensuring the next generation is free from HIV.”
Nigeria has shown steady progress on increasing access to treatment for people living with HIV, with the adoption of a test and treat policy in 2016. This measure has further accelerated referrals to treatment facilities for people who test positive for the virus. From 2010 to 2017, the country almost tripled the number of people living with HIV having access to antiretroviral therapy, up from 360 000 people in 2010 to more than 1 million people in 2018. However, the new estimates released today indicate that more than half of people living with HIV still do not have suppressed viral loads.
The new data are more accurate as they are based on an expanded surveillance system and a revised and enhanced methodology. In recent years, there has been a significant expansion in the country’s response to HIV. The number of sites providing treatment has more than tripled, the number of sites providing services to prevent mother-to-child transmission of HIV has increased eightfold and the number of HIV counselling and testing sites has increased fourfold. A total of 11.3 million adults were counselled and tested for HIV in 2016, four times as many as in 2012.
“It is important that all people living with HIV get treatment and achieve viral suppression. To halt the epidemic, we need to act now,” said Sani Aliyu, Director-General of the National Agency for the Control of AIDS. “As a government working with our partners, we have what it takes to support people who are HIV-positive, to provide treatment, to protect their families and to help people live long and healthy lives.”
The NAIIS was led by the Government of Nigeria through the Federal Ministry of Health and the National Agency for the Control of AIDS. UNAIDS, the United States President’s Emergency Plan for AIDS Relief and the Global Fund to Fight AIDS, Tuberculosis and Malaria provided support for the work on the survey, which was overseen by the United States Centers for Disease Control and Prevention and implemented by the University of Maryland, Baltimore, with a scope that included all 36 states and the Federal Capital Territory of Nigeria. The survey reached around 220 000 people in about 100 000 households. Fieldwork was conducted between July and December 2018.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Federal Ministry of Health (FMOH)
Federal Ministry of Health is one of the Ministries in the Federal Republic of Nigeria. It is concerned with the formulation and implementation of policies related to health. The Ministry has several departments focusing on different aspects of health care. The Department of Public Health’s National HIV and STI Control Program (NASCP) participated in the conduct of NAIIS and guided its implementation. More information can be found at http://www.health.gov.ng/
National Agency for the Control of AIDS (NACA)
The National Agency for the Control of AIDS was established to coordinate the various activities of HIV/AIDS in the country. The Agency among several functions coordinate and sustain advocacy by all sectors and at all levels for HIV/AIDS/STDs Expanded Responses in Nigeria. The Agency in collaboration with the FMoH guided the implementation of NAIIS. More information can be found at https://naca.gov.ng/ for more information about NACA.
Contact
UNAIDSMichael Hollingdale
tel. +41 22 791 5534 / +41 79 500 21 19
hollingdalem@unaids.org
UNAIDS Media
tel. +41 22 791 42 37
communications@unaids.org
Press centre
Download the printable version (PDF)
Region/country

Feature Story
Burkina Faso piloting PrEP
08 April 2019
08 April 2019 08 April 2019For the past four months, Benjamin Sana has been regularly attending the Oasis Clinic in Ouagadougou, Burkina Faso, where he sees a doctor who gives him a full check-up.
The doctor and peer educators also check whether Mr Sana has any questions regarding his pre-exposure prophylaxis (PrEP) regimen. PrEP is taken by people who are HIV-negative but at higher risk of infection, and has proved to be very effective at keeping people free from HIV.
“Two plus one plus one,” answers Mr Sana, referring to when he needs to take the pills—two pills two hours before sex, then one the day after and one again the following day or one a day until his last sexual encounter. After his check-up, the 34-year-old gay man said, “PrEP protects me and I feel reassured.” He still uses condoms and lubricant, but when he doesn’t he said he feels safer.
Mr Sana is one of 100 men taking part in the PrEP pilot project at the Oasis Clinic, run by the Association African Solidarité (AAS). Health clinics in Côte d’Ivoire, Mali and Togo are also taking part in the pilot project, which has been running since 2017.
Camille Rajaonarivelo, a doctor at AAS, said that PrEP is part of a combination prevention approach that also involves trained peers from his community. The project will gauge adherence to treatment and whether participants take PrEP correctly, she explained.
“The final aim of this pilot project is to scale up and roll out PrEP nationally once the authorities give the green light,” she said.
The study aims to evaluate whether the preventive option gains traction and how feasible it would be to roll it out nationally and regionally. Financed by the French National Agency for Research on AIDS and Expertise France in partnership with Coalition PLUS and three European health institutes, the pilot project will provide data and ascertain if the treatment lowers the number of new HIV infections among gay men and other men who have sex with men.
Burkina Faso does not penalize homosexuality, but stigma against it is high. As a result, gay men and other men who have sex with men often hide their sexuality and tend to avoid health services. HIV prevalence in Burkina Faso among gay men and other men who have sex with men stands at 1.9%, more than double the rate among the general population.
The first definitive results of the PrEP pilot project in Ouagadougou should be available in 2020. Mr Sana said that many of his friends had shown interest in taking PrEP. “Because the pilot project has limited participants, a lot of people have been turned away,” he said.
He believes that PrEP will save lives, especially those of young men. “Nowadays, young men take a lot more risks and they don’t protect themselves,” Mr Sana said. Ms Rajaonarivelo agreed and added that this applies to young men and young women. “I am stunned to see new cases of HIV every week,” she said. “We have to beef up HIV prevention and awareness again.”
Special page
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025



