West and Central Africa
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025
 Government mitigation measures in Cameroon
Government mitigation measures in Cameroon

09 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
UNAIDS data 2024
02 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
 Empowering youth to lead Togo’s HIV response
Empowering youth to lead Togo’s HIV response

31 October 2024




Feature Story
New model drug law launched in western Africa
12 September 2018
12 September 2018 12 September 2018Unjust laws can prevent people from accessing the services they need to prevent or treat HIV, and people who use drugs need help and care, not punishment—these are two of the messages from the new Model Drug Law for West Africa. Launched on11 September in Dakar, Senegal, the model drug law aims to guide policy-makers in the region on how to better frame their drug laws.
It is increasingly recognized that the current drug laws are not effective and result in enormous costs. The model drug law shows how countries can modify their laws in order protect the health and welfare of people while at the same time allowing law enforcement to focus on the most serious drug offences.
“The risk of acquiring HIV is 23 times higher among people who inject drugs, yet they still face human rights abuses, punitive legal environments and are left out of health and HIV programming,” said Michel Sidibé, Executive Director of UNAIDS. “It is essential that countries take a human rights-based approach that is grounded in scientific evidence and includes critical harm reduction services to protect the health and welfare of people who inject drugs and their communities.”
Drawn up by the West Africa Commission on Drugs, a group convened by Kofi Annan comprising experts from western Africa, the model drug law notes that barriers to accessing health services for people who use drugs need to be removed. People who inject drugs are one of the groups at highest risk of exposure to HIV, but they remain marginalized and often out of reach of health and social services.
The model drug law suggests removing criminal penalties for people who use drugs and making harm reduction measures available. It has been shown that harm reduction works—when harm reduction services are made available, new HIV infections fall sharply. For drug use, and possession of drugs for personal use, the model drug law sets out alternatives to conviction and punishment.
“Our current drug laws stigmatize and penalize drug users. However, pushing them to the fringes of society or locking them up in ever increasing numbers will not solve the problem. On the contrary, it worsens health issues and puts enormous pressure on the already over-stretched criminal justice systems,” said Olusegun Obasanjo, former President of Nigeria and Chair of the West Africa Commission on Drugs.
The model drug law also seeks to enhance access to essential medicines such as morphine and other opioids to manage pain. Many people in western Africa are denied the pain-relieving medicines that they need because doctors and other health professionals are not prescribing opioids for fear of prosecution. The model drug law suggests special protection for medical staff to help remove barriers to accessing pain relief.
Experience around the world has shown that it is possible to change drug laws for the better. The new model drug law is a step towards making such changes in western Africa.
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025



Feature Story
Progress, but still miles to go, to increase HIV prevention and treatment in Central African Republic
03 August 2018
03 August 2018 03 August 2018Some 18 months after the launch of the catch-up plan, the National AIDS Council (CNLS), the Ministry of Health and UNAIDS co-organized a workshop in Bangui, to take stock of the progress and the challenges to accelerate access to treatment for people living with HIV in the Central African Republic. The workshop also served as an opportunity to renew political commitment to the HIV response and to call for urgent action on prevention.
The Prime Minister of the Central African Republic, Simplice Mathieu Sarandji, opened the meeting with 80 stakeholders present, including members of government, civil society organisations, people living with HIV, members of key populations, as well as local governments, traditional and religious leaders.
Key areas of progress since the launch of the catch-up plan in January 2017 included the development of new policies to implement test and treat, and the increase in the number of people on HIV treatment from 25,000 in 2016 to 34,000 in June 2018. Community treatment groups have been delivering HIV treatment to people in remote and insecure regions such as the eastern town of Zemio. In addition, a community treatment observatory is helping monitor access to and quality of HIV care in Bangui.
However, there are miles to go. Less than 35% of people living with HIV in Central African Republic access treatment — this is among the lowest in sub-Saharan Africa. Challenges include an inadequate monitoring and evaluation system, a lack of effective supervision of facilities providing HIV services, limited community engagement to implement HIV testing and treatment, as well as limited financial commitments to reach treatment targets. Most agreed on the need to improve coordination.
As a result, participants identified priorities for the next six months to reach treatment targets for 2019. All stressed that communities, people living with HIV and key populations must be involved every step of the way. In addition, participants stressed the urgent need for increased domestic and donor funding.
A steering committee and technical working groups prepared the two-day workshop based on available data and on-the ground site visits. The groups included representatives from the Ministry of Health, CNLS, community organisations, people living with HIV, international NGOs such as Medécins Sans Frontières and the French Red Cross as well as UNICEF, UNFPA, WHO and UNAIDS.
Quotes
“Our country and government are committed to accelerating the pace of people accessing medicine and to reach the goal of zero new HIV infections. To ensure this, we will fund HIV treatment for an additional 5000 people in 2019. We will also rapidly develop a national HIV prevention plan.”
“It is time to go faster with our catch-up plan. We must change our approaches, build on progress and adapt when necessary to reach our goals. Our objective is to focus on the communities where people are most vulnerable to HIV infection and to provide them with effective services that respect human rights.”
“We will not put more people on treatment and reduce new HIV infections without involving us. Stigma and discrimination remain serious barriers to our efforts. This is why people living with HIV want to play an active role in encouraging HIV testing, prevention and treatment for all.”
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


Press Statement
UNAIDS welcomes additional evidence from Cameroon, Côte d’Ivoire, and South Africa on progress towards the 2020 targets
22 July 2018 22 July 2018Results from population-based HIV impact surveys provide insight into where investments are needed
AMSTERDAM/GENEVA, 22 July 2018—Cameroon, Côte d’Ivoire, and South Africa have released new survey data on progress towards the 2020 targets. The Cameroon and Côte d’Ivoire population-based HIV impact assessment (PHIA) surveys and the South African survey all studied knowledge of HIV status, new HIV infections, condom use, voluntary medical male circumcision, antiretroviral therapy coverage, viral suppression and other indicators.
In South Africa, which has the largest HIV epidemic in the world with more than 7 million people living with HIV and the largest treatment programme in the world with 4.4 million people on antiretroviral therapy, the new data combined with similar data from an earlier survey indicate that there has been a 40% reduction in the rate of new adult HIV infections between 2010 and 2017.
“These surveys are incredibly important and play a vital role in helping countries to review and refine their HIV programming to make sure that the right services are reaching people affected by HIV,” said Michel Sidibé Executive Director of UNAIDS.
The survey data confirm UNAIDS estimates which indicate that South Africa has also improved treatment coverage and is very close to reaching the 90-90-90* treatment targets. It found that 85% of people living with HIV knew their HIV status, 71% of people who knew their status were accessing antiretroviral treatment and 86% of people who were accessing treatment had supressed viral loads.
Viral load suppression among all people living with HIV in Cameroon and Côte d’Ivoire however was less than 50% reflecting low treatment coverage. The two countries are far from reaching the 90-90-90 targets at 47%, 91% and 80% and 37%, 88% and 76% respectively.
The largest difference between the southern African country and the two western and central African countries is observed in knowledge of HIV status, indicating that HIV testing services need to be significantly scaled up in west and central Africa.
The PHIA surveys provide key information for identifying characteristics of the populations that are not receiving services. In Cameroon, viral load suppression varied by province from 28% to 63%. In South Africa less than 50% of children and young men (ages 15-34 years) living with HIV had suppressed viral load (compared to 67% among the women aged 15-49). These data will provide critical information to allow programme managers to direct their responses to the populations and locations most in need of services.
The PHIA surveys, were led by Columbia University in collaboration with country governments and supported by the United States President’s Emergency Plan for AIDS Relief. The South African survey was conducted by the Human Sciences Research Council
* 90% of people living with HIV know their HIV status, 90% of people who know their status are receiving antiretroviral treatment, and 90% of people on treatment have suppressed viral loads.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Press centre
Download the printable version (PDF)


Feature Story
Civil society builds a coalition to accelerate results in western and central Africa
15 May 2018
15 May 2018 15 May 2018Western and central Africa has faced many challenges, from conflicts and humanitarian crises to political instability and the devastating Ebola epidemics. At a time when the global response to HIV is accelerating, millions of people in the region are being left behind. Globally in 2016, 70% of all people living with HIV knew their HIV status, 53% of all people living with HIV were accessing treatment and 44% of all people living with HIV were virally suppressed. In contrast, the western and central African region lags behind, achieving only 42%, 35% and 25%, respectively, in 2016. The gap is considerable in that region: 4.0 million people living with HIV are not receiving treatment and 310 000 adults and children died from AIDS-related illnesses in 2016.
In order to share experiences, challenges and information on successful programmes, representatives of civil society organizations involved in the AIDS responses across western and central Africa gathered in Somone, Senegal, from 7 to 10 May. Technical and financial partners also took part in the discussions.
“Eighty civil society leaders from 17 countries in western and central Africa are eager to take up a central role in the implementation of the western and central Africa catch-up plan as actors of social change and political transformation,” said Patrick Brenny, the Director of the UNAIDS Regional Support Team for Western and Central Africa.
The participants developed innovative solutions to overcome barriers to national AIDS responses and to improve the unity and collaboration of local civil society organizations. They examined progress and setbacks in the implementation of national catch-up plans and shared experiences of violations of human rights related to HIV status and stigma and discrimination.
Consensus emerged that efforts should be focused on bridging the gaps in paediatric care and treatment, in particular in the context of the lack of social protection schemes for orphans and other children made vulnerable by AIDS. The region has seen a worrying trend in increasing mortality among adolescents living with HIV. Lack of access to comprehensive sexuality education, a high age of consent to access sexual and reproductive health information, services and treatment without parental agreement and taboos around youth sexuality were raised as some of the obstacles to be overcome.
Successful innovations and programmes with key populations and other vulnerable groups were shared. There was wide consensus about the role of community health systems to reach remote populations and vulnerable groups, while protecting confidentiality.
“It is high time that we increase investments to guarantee access to antiretroviral medicines, have better paediatric medicines, implement family testing approaches and scale up social protection programmes to protect all vulnerable mothers and children,” said Christine Kafando, Coordinator of the Hope for Tomorrow Association in Burkina Faso.
The participants will build on the progress made by organizing national dialogues around the catch-up plan for the region. The development of a regional platform for advocacy and technical support will be further discussed to enable stronger and more resilient civil society to play roles in national AIDS responses and other global health challenges.
“Each stakeholder gathered here plays a central role in their respective national AIDS response. Each brings invaluable experience to the table. We need to build on this energy to renew our commitment to work together for much needed breakthroughs for the region to bring HIV under control,” said Daouda Diouf, the Executive Director of ENDA Santé in Senegal.
Region/country



Feature Story
A united rallying cry: Time to make health care systems more flexible and innovative
16 April 2018
16 April 2018 16 April 2018Seven months after launching the catch-up plan in western and central Africa, progress on increasing the numbers of people on antiretroviral treatment continues to lag in the region. Many countries will not reach key targets by 2020 if the current systems remain unchanged.
"Overall we saw a 10% percent increase of people on treatment, which is not enough," said UNAIDS Executive Director Michel Sidibé. "Now, there is even more a sense of urgency."
Mr Sidibé, however, pointed to the success in the Democratic Republic of Congo where there was a clear increase in the number of people living with HIV accessing ARVs. The reasons for the positive trend included civil society and political leadership working closely together as well as community HIV testing and the training of 11 000 health care workers.
"More than ever there is a need to rethink health systems and alternatives for people to access health care," he said.
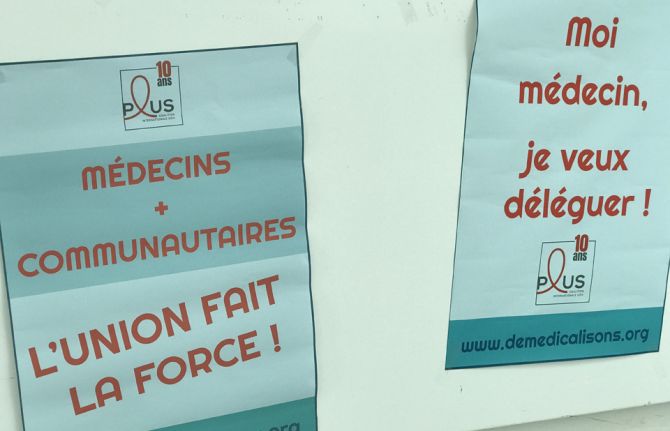
The call to delegate patient care to communities was a major rallying call during AFRAVIH, the international francophone HIV and hepatitis conference held in Bordeaux, France, early April. Mr Sidibé briefly shared the stage at the opening ceremony with the civil society organisation Coalition PLUS. They declared that the key to success in ending AIDS involved joining forces between doctors and community health workers and giving more leeway to communities to respond to the local needs of their own people.
Under the banner, "De-medicalize" the organisation explained that doctors will never be replaced but that there were too few of them and people living with HIV didn't require acute care.
Coalition Plus' recent report states that governments and the medical practitioners should delegate more tasks to nurses and community health workers. In addition to allowing for more targeted prevention and faster access to treatment, delegation of non-medical tasks would lighten the load on overburdened health systems. West and central Africa represent 17% of the total population living with HIV but 30% of deaths in the region are from AIDS-related illnesses. This is a region, according to UNAIDS and its partners, that can truly benefit from community models of care.
What worries Médecins Sans Frontières (MSF) is the risk of a significant drop in resources for treatment will hamper recent improvements in west and central Africa. This concern stems from the fact that Global Fund estimates a 30% drop in fund allocations to the region for 2018 – 2020 compared to signed HIV grants in the previous allocation period. In 2016, MSF was among the first to sound alarm bells regarding the region's high HIV death toll and the up to 80% of children unable to access antiretroviral therapy. MSF HIV Policy Advisor and Advocacy Officer Nathalie Cartier said that they supported the west and central Africa catch-up plan but that it needed to be fully implemented. "Political will has been promising but now it's time to make it a reality on the ground so that people living with HIV can reap the benefits," she said.
Global Fund supported the catch-up plan and works closely with countries in order to maximize the impact of the investments. They believe that leveraging additional domestic financing for health is crucial to increase country ownership and build sustainable programs.
All the more reason to decentralize healthcare systems and capitalize on innovations to keep health costs down. HIV self-testing, new medicines and high impact strategies involving communities are critical to improving efficiencies. "With point-of-care (POC) testing in communities and homes, delays are minimal between diagnosis and initiating treatment," said Cheick Tidiane Tall, Director of Réseau EVA, a network of pediatric doctors specialized in HIV care. “In the long run, that's a lot of people and resources saved,” he added.
Côte d'Ivoire Infectious and Tropical Diseases professor Serge Eholié couldn't agree more. "Flexible health care systems capitalizing on various innovations makes a lot of sense," he said. Turning to the Minister of Health in the Central African Republic, Pierre Somse, he asked, 'How do you respond?'
Mr Somse, also a trained doctor, said, "We doctors will stay doctors. However, there is a need for us to lean on communities and vice versa." He added, "at the heart of the issue are patients and they are and should always be the priority."
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025



Update
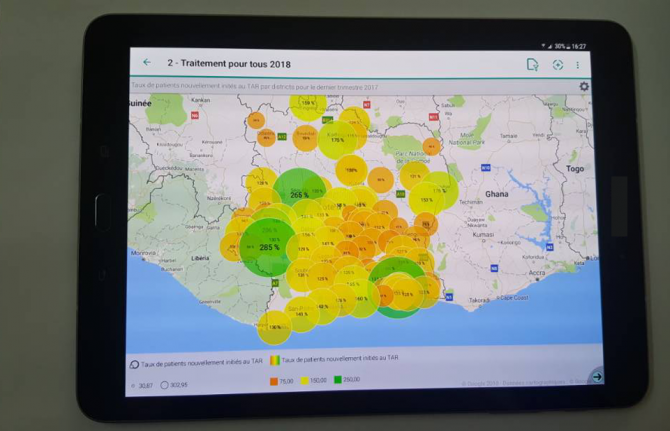
Launch of HIV situation room in Côte d’Ivoire
27 March 2018
27 March 2018 27 March 2018Côte d’Ivoire has become the first francophone country, and the first in western and central Africa, to launch an HIV situation room, a software platform designed to support informed decision-making.
This innovative tool strengthens national information systems through real-time visualization of information from multiple data sets. It will enable leaders and programme managers to make timely decisions to improve health programmes to achieve the 90–90–90 targets, whereby 90% of people living with HIV know their HIV status, 90% of people who know their HIV-positive status are accessing treatment and 90% of people on treatment have suppressed viral loads, by 2020.
The situation room is the result of a collaboration between the Côte d’Ivoire Ministry of Health and Public Hygiene, the United States President’s Emergency Plan for AIDS Relief through the Centers for Disease Control and Prevention, and UNAIDS. It was launched by Raymonde Goudou Coffie, the Minister of Health and Public Hygiene of Côte d’Ivoire, and Michel Sidibé, Executive Director of UNAIDS, on 26 March in Abidjan.
Quotes
“The situation room will allow the use of epidemiological data, strategic information and community-based data in real time to assist decision-making.”
“The Ebola epidemic was only ended in Côte d’Ivoire thanks to a real-time information system. The development of health in the future will depend on our ability to show information in real time and the local level.”
“I congratulate UNAIDS for the situation room, which will help to improve the response in order to achieve the 90–90–90 targets.”
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


Feature Story
Aisha Muhammadu Buhari to ensure that no child is born with HIV in Nigeria by 2020
26 March 2018
26 March 2018 26 March 2018The wife of the President of Nigeria, Aisha Muhammadu Buhari—the new UNAIDS Special Ambassador for the Elimination of Mother-to-Child Transmission of HIV and the Promotion of Treatment for Children Living with HIV in Nigeria—has vowed to end mother-to-child transmission of HIV in the country.
“It is with a great sense of responsibility and humility that I accept the honour to serve as a UNAIDS Special Ambassador. I am looking forward to using my voice to help ensure that no child is born with HIV in Nigeria by 2020,” said Ms Buhari, upon commencement of her new role.
Nigeria has one of the highest rates of new HIV infections among children in the world. In 2016, an estimated 37 000 [22 000–56 000] children were newly infected with HIV and 24 000 [14 000–37 000) children died of AIDS-related illnesses. Around 270 000 children [180 000–380 000] children were living with HIV in 2016, and just 32% of pregnant women living with HIV had access to antiretroviral medicines to prevent transmitting the virus to their child.
“I am privileged to announce Aisha Muhammadu Buhari’s acceptance of the appointment as UNAIDS Special Ambassador for Nigeria. The trust and respect that she commands in the country will help us to quicken the pace of stopping new HIV infections among children as well as ensuring treatment for all children living with HIV,” said Michel Sidibé, the Executive Director of UNAIDS.
The appointment of Ms Buhari will reinforce recent efforts to scale up the response to HIV in Nigeria. In December 2016, the President of Nigeria, Muhammadu Buhari, launched a Fast-Track plan that includes using domestic resources to maintain 60 000 people living with HIV on treatment and to ensure that an additional 50 000 people can access treatment each year.
“We are delighted that her excellency has accepted this important role of UNAIDS Special Ambassador. The goal of eliminating mother-to-child transmission of HIV in Nigeria is a laudable one. It must be achieved,” said Pauline Tallen, the Board Chairperson of the National Agency for the Control of AIDS, Nigeria.
Ms Buhari is a passionate advocate for the rights of vulnerable women and girls. During her one-year tenure, she will advocate for increased access to antenatal care services and HIV testing for all pregnant women and their linkage to adequate treatment and care. She will also advocate for an increase in domestic resources for the HIV response at the federal and state levels.
“My three lovely children are all HIV-free because I benefited from prevention of mother-to-child transmission of HIV services. All pregnant women living with HIV in Nigeria deserve children who are born free from the virus, and the new UNAIDS Special Ambassador’s voice can help us make a huge difference. She is now in a strong position to advocate for free prevention of mother-to-child transmission of HIV services in the country,” said Lucy Attah Enyia, a beneficiary of prevention of mother-to-child transmission of HIV services.
A formal ceremony to commemorate Ms Buhari’s acceptance of her appointment will take place during the visit of Mr Sidibé to Abuja, Nigeria, in April 2018.
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025




Feature Story
Leveraging education to improve health and end AIDS
02 February 2018
02 February 2018 02 February 2018During the Global Partnership for Education meeting on 2 February, hosted by Senegal and France, UNAIDS Executive Director Michel Sidibé discussed the importance of education and health. “Integrating education and health is key for our success in controlling the epidemic among young people. Without effective, quality and sustainable health and education systems we are failing young people”, Mr Sidibé said. Credit: UNAIDS/B. Deméocq.
The First Lady of Senegal, Marieme Faye Sall, and the First Lady of France, Brigitte Macron, inaugurate a cardio-paediatric centre that provides surgical treatment for children affected by cardiologic diseases. The centre, funded by the Cuomo Foundation in Monaco, supports women and children in Senegal. Credit: UNAIDS.
Preventing mother-to-child transmission of HIV is crucial, as is community involvement, stressed Mr Sidibé during his meeting with Ms Sall. The western and central Africa region lags behind in access to treatment and prevention, which is why UNAIDS and partners launched a western and central Africa catch-up plan. Credit: UNAIDS/B. Deméocq.
Mr Sidibé also met with the Minister of Health and Social Action of Senegal, Abdoulaye Diouf Sarr, stressing that no matter who you are or where you are from, everyone has the right to health, the right to an education, the right to equal opportunities and the right to thrive. Credit: UNAIDS/B. Deméocq.
The Secretary General of the Organisation Internationale de la Francophonie, Michaëlle Jean, will raise the issue of counterfeit medicines at the upcoming World Health Assembly in May. Credit: UNAIDS/B. Deméocq.
Minister of International Development of Norway, Nikolai Astrup, and Mr Sidibé met on the sidelines of the meeting. Credit: UNAIDS/B. Deméocq.
Mr Sidibé, along with the Ambassador of Luxembourg, Nicole Bintner. Luxembourg has been an active participant and donor in the western and central Africa catch-up plan. Credit: UNAIDS/B. Deméocq.
Good health enables a girl to thrive, to grow, to think, to explore and to contribute to her community. Knowledge of how to stay healthy and access to quality health services enable her to prevent illness, to eat well, to manage her sexual health, to have healthy babies when and if she chooses to and to nurture her own well-being. Education and health are two of the most transformative elements of a girl’s life. Credit: UNAIDS/B. Deméocq.
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


Feature Story
Becoming an activist to overcome discrimination
28 February 2018
28 February 2018 28 February 2018Thrown out of the house by his parents when they found out he was gay, Ezechiel Koffi didn’t give up.
“My parents said I shamed them and that I lived the life of a sinner,” the young man from Côte d’Ivoire said. What hurt him the most were his mother's insults, saying he had no respect for their religious values. He begged them to understand that he was their son and that they should accept him as he was.
Mr Koffi, 24 years old at the time, stayed for a while at Alternative, a lesbian, gay, bisexual, transgender and intersex (LGBTI) people nongovernmental organization in Abidjan, Côte d’Ivoire, where he had started volunteering three years earlier. He kept going to classes, although admits that at times he went on an empty stomach. Psychologically he felt beaten. “It was hard, but I couldn't hide anymore,” he said.
With the help of his older sister, his parents let him move back home after six months. Although he now had a steady roof over his head and regular meals, Alternative became his second home. He has been dedicated to it ever since. Now an HIV educator and community health worker, he proudly showed his certificates on his mobile phone.
Alternative’s project coordinator, Philippe Njaboué, describes Mr Koffi’s tireless energy. “You can call him at whatever time, day or night, he always lends a hand and he often goes out of his way to include people who have been shunned.” When asked about being a substitute family for many LGBTI people, Mr Koffi gave a hesitant smile.
The many discussion groups and support groups have helped, he said, allowing him to share his experience and help others. The once shy boy has emancipated himself. He also no longer shies away from revealing his HIV status. “It’s been 10 years now that I have been living with HIV,” he said.
Looking back, he explained, in the beginning he couldn’t always negotiate the use of a condom. He now makes a point of telling everyone that HIV is a reality. “Use condoms, there is help, you are not alone,” he exclaimed.
He described feeling fully alive among the city’s tight-knit LGBTI crowd. “I am at ease, I can express myself and it’s fulfilling,” he said. His brow furrowed, however, when he mentioned the constant discrimination he and his peers lived with. On top of the taunting and the finger pointing, Mr Koffi said social media was rampant with homophobic comments.
“We deserve the same rights as everyone else and that’s what keeps me motivated,” Mr Koffi said.
Mr Njaboué remarked that society, religion and the state all play a big part in keeping homosexuality taboo in Côte d’Ivoire. “A recent speech by Alternative’s director was tagged by a website as “The king of the homosexuals speaks”, which led to countless death threats,” he said.
Noting that this case was one of many, he believes the situation can only change if the government tackles human rights.
“Most of the population doesn’t know their rights or the law, including a lot people in charge of state security,” Mr Njaboué said. “Not only does the government need to educate people, it should also condemn unlawful behaviour,” he added.
For Mr Koffi, his visibility puts him at risk, he said, but he forges ahead. “I want to live in a world where there is no discrimination based on one’s race, one’s religion or one’s sexuality.”