Feature Story
Photography exhibition aims to reduce HIV stigma and discrimination in Pakistan
07 September 2015
07 September 2015 07 September 2015A photography exhibition portraying the inspirational stories of people living with HIV opened in Islamabad, Pakistan, on 7 September.
A Photo Story on People Living with HIV in Pakistan is a collection of 25 portraits of men and women living with HIV who have taken the decision to share their stories of HIV-related stigma with the public. It is the first exhibition in Pakistan to shine the spotlight on the resilience of people living with HIV. Each photo is accompanied by a short interview in which people express their challenges and concerns, but also their determination to bring about change and eliminate stigma and discrimination.
Nazir Masih, the Chief Executive Officer of the New Lights AIDS Control Society, a non-profit organization dedicated to providing treatment, care and support for people living with HIV, is one of the people portrayed in the exhibition. He said, “HIV is a problem of human beings and it is not an issue of any particular religion or nation. That is why hurdles and threats cannot deter me from the path of helping those in need and will not stop me, come what may, because this is what I have been made for.”
In Pakistan, it has often been difficult to disseminate key HIV information, owing to cultural and social barriers. The aim of this exhibition is to give a human face to the epidemic, with photographs that will have a lasting impact and can be shared on multiple platforms.
“We salute the courage and willingness of the men and women showcased in this exhibition to disclose their status in the hopes of transforming society,” said Steve Kraus, Director of the UNAIDS Regional Support Team for Asia and the Pacific, who inaugurated the exhibition. “Let us embrace our brothers and sisters living with HIV. Only when we reach zero discrimination can we end the AIDS epidemic in Pakistan.”
Stigma and discrimination towards people living with HIV remains a widespread challenge in Pakistan. The country’s People Living with HIV Stigma Index, conducted in 2010, revealed high levels of stigma and exclusion from families and religious activities and discrimination in employment. One third of respondents reported being denied access to health care in the previous 12 months.
Abdul Baseer Khan Achakzai, National Programme Manager, National AIDS Control Programme, said “The Government of Pakistan is committed to scaling up targeted interventions to prevent the rise in HIV prevalence among key and vulnerable populations and to fostering an organized national response to halt new HIV infections, improve the health and quality of life of people with and affected by HIV and initiate community-based HIV testing to bridge the gap between registered and estimated HIV cases.”
The exhibition was produced in collaboration with the National AIDS Control Programme of Pakistan, the United Nations Information Centre and UNAIDS.
Region/country

Feature Story
UNAIDS wins first prize in British Medical Association Book Awards
03 September 2015
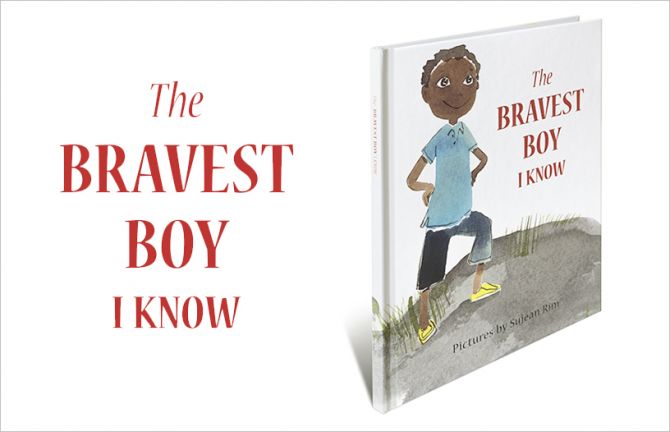
03 September 2015 03 September 2015UNAIDS has been awarded first prize in the Popular Medicine category of the British Medical Association (BMA) Book Awards for its book The Bravest Boy I Know.
The prestigious awards were announced at a ceremony on 3 September at BMA House in London. An annual event, the awards aim to encourage and reward excellence in medical publishing, with prizes given out in categories and an overall BMA Medical Book of the Year award made from the category winners.
The Bravest Boy I Know is about two friends, Kendi and Kayla. Kendi is living with HIV. The story is set in Africa and is a heart-warming tale of how the two friends deal with HIV in a positive way. The book conveys the important message that by taking medicine, children living with HIV can live active and healthy lives, while also explaining that the medicines can make children feel unwell and tired.
The judges noted that the book, “Is a unique offering … and is well-presented and engaging. If used appropriately it could be an important public health tool.”
UNAIDS Director of Communications and Global Advocacy Annemarie Hou, accepting the award on behalf of UNAIDS, said, “This is a tremendous honour and recognition that children everywhere need access to high-quality health information.”
The book, which is beautifully illustrated by celebrated artist Sujean Rim, was launched in May 2014 by UNAIDS and the United Nations World Tourism Organization’s Sustainable Tourism for Eliminating Poverty (ST-EP) Foundation at an event attended by the United Nations Secretary-General Ban Ki-moon and Ambassador Dho Young-shim, Chairperson of the ST-EP Foundation. The book is dedicated to Mr Ban for his work in prioritizing education through the Global Education First Initiative, which aims to put every child in school, improve the quality of learning and foster global citizenship.
Speaking at the launch in 2014, Mr Ban said that, “This book, which will be delivered to schools across Africa through ST-EP’s Small Libraries project, will help everyone understand that young people can live normal and fulfilling lives with HIV.”
Ambassador Dho said at the launch in 2014, “As the UN MDGs Advocate for Education, I firmly believe in the power of education to accelerate the achievement of all UN MDGs by 2015, and particularly Goal 6—aimed at HIV. This meaningful collaboration with UNAIDS is creating synergies that will have a powerful impact on the education and the health of children.”
In addition to winning first prize in the Popular Medicine category, UNAIDS was also Highly Commended for The Gap Report in the Public Health category and for The Cities Report in the Health and Social Care category.
Related

Feature Story
More focus on populations and places most in need as United States updates its National HIV/AIDS Strategy
05 August 2015
05 August 2015 05 August 2015The United States of America (US) released an updated AIDS strategy on 30 July which sets the course for its domestic response to HIV over the next five years. The National HIV/AIDS Strategy: Updated to 2020 sets ambitious targets which put particular focus on the people and places most in need.
The US strategy mirrors many of the goals of UNAIDS Fast-Track approach. It calls for 90% of people living with HIV to be aware of their status, aims to increase the percentage of people living with HIV who are retained in medical care to at least 90% and to ensure that 80% of all people diagnosed with HIV have a suppressed viral load which reduces the likelihood of transmitting the virus by around 96%.
Commenting on the new strategy President Obama said that it seized upon rapid shifts in science and policy as more had been learned about the disease. He also said it focused on making sure that every American could get access to life-extending care, no matter who they were, where they lived or how much money they had.
The strategy recommends that efforts be concentrated on people who are being left behind in the response to HIV, namely, gay men and other men who have sex with men, especially African American men, heterosexual African American men and women, young people, people who inject drugs and transgender women. It calls for full access to comprehensive pre-exposure prophylaxis (PrEP) services for those for whom they are appropriate and desired. The strategy also prioritizes certain geographic areas where HIV incidence is high and linkage to, and retention in care is low, including the southern US and specific major metropolitan areas, like Washington, DC.
“I commend President Obama on the bold, new goals set in the updated US strategy which align with the UNAIDS ‘Fast-Track’ approach. The United States joins other nations in pursuit of key prevention, testing and treatment targets that, if met by 2020, put the world on course to end AIDS as a public health threat by 2030,” said Michel Sidibé, Executive Director of UNAIDS.
According to the latest data available from the Centers for Disease Control and Prevention (CDC), there are an estimated 1.2 million people living with HIV in the US, of whom 1 in 8 are unaware of their HIV status. CDC also estimates that 50% of Americans who are diagnosed with HIV are not retained in medical care and that only 37% are accessing life-saving HIV treatment.
At the event to launch the revised strategy, which was held in Atlanta, Georgia, it was also announced that Mayor Kasim Reed had signed the Paris Declaration—Fast-track cities: Ending the AIDS epidemic. In signing the declaration, the mayor has committed to putting Atlanta on the Fast-Track to ending the AIDS epidemic through a set of commitments. Those commitments include achieving the UNAIDS 90–90–90 targets, which will result in 90% of people living with HIV knowing their HIV status, 90% of people who know their HIV-positive status on antiretroviral treatment and 90% of people on treatment with suppressed viral loads, keeping them healthy and reducing the risk of HIV transmission.
The Fast-Track Cities Initiative is supported by its core partners, namely, the City of Paris, the International Association of Providers of AIDS Care (IAPAC), UNAIDS and the United Nations Human Settlements Programme (UN-Habitat).
Region/country









Feature Story
Aquatics world championships in Kazan promotes AIDS awareness
30 July 2015
30 July 2015 30 July 2015At the 16th FINA World Championships in aquatics, visitors, athletes and volunteers are learning more about HIV. The event, being held from 24 July to 9 August in Kazan, Russia, is promoting Dive safely!, an initiative to raise awareness about HIV and encourage people to learn their HIV status.
Located in the Dive safely! pavilion in the FINA Water World park, the initiative provides HIV prevention materials and offers free, confidential HIV tests to its visitors during the two week championship.
Opening the pavilion, the President of FINA, Dr Julio Maglioni said, "It is an unexpected gift for me to be here today. The AIDS response is very important for the health of our world. It is very important now to unite in order to stop this disease in the name of sport.”
Alexander Zhukov, President of the Russian Olympic Committee, invited all young people at the FINA World Championship to visit the Dive safely! pavilion and take an HIV test. “Every young person should know about HIV and know their status," said Mr Zhukov.
Alexander Zhukov confirmed that the Russian Olympic Committee will soon increase its cooperation on HIV prevention through a new agreement with UNAIDS, and will expand its HIV prevention projects during upcoming international sporting events in Russia, such as the World Football Championship in 2018.
A social media campaign for the FINA World Championships led by the UNAIDS Regional Youth Red Ribbon Team—a group of young celebrities from Eastern Europe and Central Asia—was launched on Twitter, Instagram and Facebook, encouraging people to learn about HIV and to post photos and messages with the hashtag #divesafely.
Since the pavilion was opened, more than 500 people have visited every day, with more than 200 people being tested onsite each day for HIV. The tests are carried out by doctors from the Republican AIDS Center of Tatarstan and any positive results are referred to the AIDS Center in Kazan.
Dilyara Vagapova, spokesperson for the #divesafely campaign, called on people to know their HIV status. "Together we can end AIDS in our countries. To be fashionable means to know your HIV status!"
Dive safely! (Легкой воды! in Russian) is a joint initiative of the Ministry of Health of the Republic of Tatarstan, the Executive Directorate for Sports Projects, the local non-governmental organization New Century (“Novyi Vek”), the Tatarstan Republican AIDS Centre and UNAIDS.
Region/country
Related











Feature Story
Postcards from China’s first AIDS RIDE
29 July 2015
29 July 2015 29 July 2015Liu Jiulong is the first person in China to complete an AIDS RIDE. This fundraiser and HIV awareness raising bicycling event has been popular in other countries like the USA for many years. However, in China, fear of stigma and discrimination has kept many people living with HIV from taking part in public events.
“Cycling promotes a healthy lifestyle and the AIDS RIDE is a good way to promote correct knowledge about HIV prevention to the general public,” said Liu Jiulong.
His mission was to use the challenge to eliminate ignorance, misunderstanding, fear and discrimination against people living with HIV. His odyssey began on 4 May in Nanchang city, his home town. He rode his bike for 3 000 km, cycling through 27 cities. He completed his journey in Beijing 43 days later. Liu Jiulong hosted 30 outreach events during his trip, reaching 16 million people online.
Speaking about his accomplishment after crossing the finish line, he said, “There were so many people involved and I enjoyed the mutual support we gave each other.”
Life was anything but great in 2007 when Liu Jiulong was diagnosed with HIV. He was working at an advertising company in Beijing. “I thought I wasn’t going to live to be 35 years old. I felt worthless and also very guilty and bad towards my family,” said Liu Jiulong. He also experienced stigma and discrimination when people stoppedspeaking to him after learningabout his status.
He felt so desperate that he even tried to commit suicide. Eventually, with the support of caring doctors, nurses and volunteer supporters at the Beijing Youan Hospital he made it through those dark days and decided to move back to his home town. He founded an organization called “Love Service Station” to support people living with HIV in Nanchang City.
Liu Jiulong started taking antiretroviral treatment for HIV in 2009 and said it has changed his life, “With life-saving treatment, I’m in a good situation. I can complete the 3 000 km AIDS RIDE.”
Liu Jiulong wants other people living with HIV to know that with effective self-management of HIV and by taking antiretroviral treatment, they can improve the quality of their life. He is proud of his recent achievement, “It’s a great feeling.”
Region/country
Related
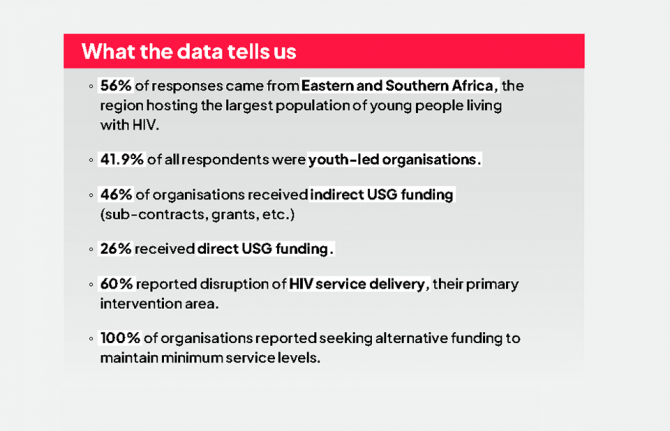
 Multisectoral resilience to funding cuts in Guatemala
Multisectoral resilience to funding cuts in Guatemala

22 December 2025


Feature Story
Global scientific leaders explore strategies to achieve the 90-90-90 target
22 July 2015
22 July 2015 22 July 2015Leading HIV researchers describing results from multiple clinical trials in sub-Saharan Africa report that innovative service delivery models are achieving results across the HIV treatment cascade that approach or exceed the 90–90–90 target.
Study results were presented at an all-day workshop hosted by the British Columbia Centre for Excellence in HIV/AIDS and the Division of AIDS at the University of British Columbia, prior to the opening of the 8th International AIDS Society Conference on HIV Pathogenesis, Treatment and Prevention in Vancouver, Canada. The studies are being undertaken in a number of high-burden countries in sub-Saharan Africa, including Botswana, Kenya, Malawi, South Africa, Swaziland, Uganda and Zambia.
“These exceptional clinical trial results show yet again how innovation is driving progress in the AIDS response,” said UNAIDS Executive Director Michel Sidibé. “The results demonstrate that the 90–90–90 target is more than a dream. It is entirely feasible.”
Diane Havlir, of the University of California, San Francisco, presented interim results from the Sustainable East Africa Research for Community Health (SEARCH) trial in more than 30 rural communities in Kenya and Uganda. Having enrolled more than 334 000 people, the SEARCH trial is evaluating a multicomponent programme, including use of community-centred, multidisease campaigns to provide HIV testing and link HIV-positive individuals to immediate initiation of antiretroviral therapy.
At a population level, the SEARCH programme has achieved 90% knowledge of HIV status. Among participants living with HIV, more than 90% of people in Uganda and 83% in Kenya are receiving antiretroviral therapy. At 24 weeks, 92% of trial participants who have initiated antiretroviral therapy have achieved viral suppression.
Similarly encouraging, although preliminary, results were reported from the PopART trial by Richard Hayes of the London School of Hygiene and Tropical Medicine. Working in 21 communities, the trial is evaluating a combination HIV prevention package that includes repeated rounds of community-level HIV testing and immediate initiation of antiretroviral therapy for all people who are diagnosed HIV-positive. Among more than 115 000 community members enumerated in the trial, 90% of all men living with HIV and 92% of all women living with HIV were aware of their HIV status following the PopART programme. Among people with an HIV diagnosis, 62% of men and 65% of women were receiving antiretroviral therapy, highlighting the need to further strengthen linkage to care for people living with HIV. Data on rates of viral suppression among PopART participations will be available next year.
Max Essex, of the Harvard University School of Public Health, presented baseline findings for the Botswana Combination Prevention Protocol. Mr Essex and his colleagues have found that 79% of all people living with HIV in Botswana knew their HIV status as of mid-2015, 86% of adults who have been diagnosed with HIV were receiving antiretroviral therapy and 96% of people receiving antiretroviral therapy had achieved viral suppression.
Comparably impressive results have been achieved by a Médicins Sans Frontières (MSF) programme in the District of Chiradzulu in Malawi, according to David Maman of MSF. In Chiradzulu, 77% of all people living with HIV know their HIV status, 84% of people with an HIV diagnosis are receiving antiretroviral therapy and 91% of people receiving antiretroviral therapy have achieved viral suppression.
François Dabis, of the Bordeaux School of Public Health, described preliminary results from a separate trial in the Hlabisa district in KwaZulu-Natal, South Africa, of a test-and-treat initiative that includes six-month rounds of community-level testing and establishment of antiretroviral treatment sites in all communities in the study. Among more than 26 000 people in the study communities, 85% know their HIV status. Among HIV-diagnosed people reached by the programme, 86% are receiving antiretroviral therapy. Study results indicate that linkage to care remains suboptimal and an important focus of further work and innovation.
Several important themes emerged from these study findings. Researchers emphasized the importance and value of engaging and collaborating with local communities in developing programme approaches tailored to local needs and circumstances. Most of the studies have also taken multidisciplinary approaches to the development, monitoring and evaluation of programmes, involving social scientists, economists and community representatives as well as clinicians and biostatisticians.


Feature Story
Vancouver delegates call for greater innovation in HIV diagnostics
22 July 2015
22 July 2015 22 July 2015Innovation in HIV diagnostics is urgently needed if the world hopes to achieve the 90–90–90 target for access to antiretroviral therapy, leading scientific experts advised this week. The call for intensified effort and innovation on HIV diagnostics occurred during two sessions at the 8th International AIDS Society Conference on HIV Pathogenesis, Treatment and Prevention, held in Vancouver, Canada.
“It is clear that we can’t accept business as usual when it comes to HIV diagnostics,” said UNAIDS Deputy Executive Director Luiz Loures, who moderated a special satellite session on enhancing diagnostic access. “We must do things differently if we are to reach the 90–90–90 target.”
Global experts focused on three key diagnostic challenges: ensuring timely diagnosis of HIV among children, rapidly increasing knowledge of HIV status among adults living with HIV and scaling up essential viral load testing. These three focus areas are key priorities for the Diagnostics Access Initiative, a multi-stakeholder global initiative that aims to fully leverage the potential of laboratory medicine to lay the groundwork to end the AIDS epidemic as a public health threat.
Diagnosing children living with HIV
Unlike adults, who can be diagnosed with HIV through a simple antibody test, very young children require more expensive molecular tests, which use centralized laboratories that are remote from clinical sites. This creates substantial delays in diagnosing HIV-exposed children and also increases both costs and the risks that specimens or results will be lost. Even when early infant diagnostic services are available, many HIV-exposed children only receive their HIV test results after the time when peak mortality occurs, at six to eight weeks old, according to Trevor Peter, of the Clinton Health Access Initiative (CHAI).
Relatively simple, point-of-care diagnostic tests for early infant diagnosis are now emerging, Mr Peter reported, and these will need to be rapidly scaled up. In addition, mobile health technologies have the potential to reduce delays in the communication of test results and help ensure that test results for HIV-exposed children are actually received at the clinical site. At the Vancouver conference, UNAIDS and its partners in the Diagnostics Access Initiative announced with Roche Diagnostics a 35% decline in the global price for early infant diagnostic testing.
Ensuring 90% knowledge of HIV status among adolescents and adults living with HIV
UNAIDS sponsored a separate session at the conference on democratizing HIV testing to reach the 90–90–90 target. Joseph Amon of Human Rights Watch advised that all people should feel empowered to choose where, when and how they want to be tested for HIV. Consistent with this human rights approach, there is growing interest in HIV self-testing tools.
New international guidelines on HIV testing services, launched by the World Health Organization (WHO) in Vancouver this week, indicate that WHO envisages widespread access to self-testing as an important component of a comprehensive HIV testing effort. Several countries in different regions currently allow HIV self-testing, but most countries have yet to adapt their laws and regulatory frameworks to permit it.
The new WHO guidelines on HIV self-testing emphasize the importance of moving testing access closer to communities. In particular, the new guidelines recommend steps to enable lay workers to administer HIV tests. Results from the Sustainable East Africa Research for Community Health (SEARCH) trial in more than 30 rural communities in Kenya and Uganda indicate that population-level knowledge of HIV status approaching or exceeding 90% can be achieved through community-owned, multidisease testing campaigns.
Presenting modelling work, John Stover of Avenir Health said that 90% knowledge of HIV status is achievable more broadly through a strategic combination of testing strategies, such as provider-initiated testing in diverse health settings, outreach to key populations, fixed centres for HIV testing and counselling, and various community-based approaches, such as HIV self-testing, mobile testing and door-to-door, home-based efforts.
Ensuring universal access to viral load testing
Conference participants also heard urgent calls to expand access to viral load testing. Not only is access to viral load testing essential for monitoring the 90-90-90 target, but viral load testing is an essential clinical tool to detect early treatment failure and permit intervention to improve treatment adherence. However, projections by CHAI indicate that current trends in the uptake of viral load testing are insufficient to ensure achievement of the 90–90–90 target.
During the diagnostics-focused sessions, several ways forward were suggested to close the viral load testing gap. Partners in the Diagnostics Access Initiative, along with the Government of South Africa, last year concluded an agreement with Roche Diagnostics to reduce the price of viral load testing by 40% worldwide. In addition, steps need to be taken to maximize the effective use of the viral load platforms that presently exist, as many viral load technologies are severely under-utilized at present.
Related
 “Who will protect our young people?”
“Who will protect our young people?”

02 June 2025

Feature Story
UNFPA, WHO and UNAIDS: Position statement on condoms and the prevention of HIV, other sexually transmitted infections and unintended pregnancy
07 July 2015
07 July 2015 07 July 2015Condoms are a critical component in a comprehensive and sustainable approach to the prevention of HIV and other sexually transmitted infections (STIs) and are effective for preventing unintended pregnancies. In 2013, an estimated 2.1 million people became newly infected with HIV[i] and an estimated 500 million people acquired chlamydia, gonorrhoea, syphilis or trichomoniasis.[ii] In addition, every year more than 200 million women have unmet needs for contraception,[iii] leading to approximately 80 million unintended pregnancies.[iv] These three public health priorities require a decisive response using all available tools, with condoms playing a central role.
Male and female condoms are the only devices that both reduce the transmission of HIV and other sexually transmitted infections (STIs) and prevent unintended pregnancy.
Laboratory studies show that condoms provide an impermeable barrier to particles the size of sperm and STI pathogens, including HIV.[v] [vi] Condoms, when used consistently and correctly, are highly effective in preventing the sexual transmission of HIV. Research among serodiscordant couples (where one partner is living with HIV and the other is not) shows that consistent condom use significantly reduces the risk of HIV transmission both from men to women and women to men[vii] [viii] [ix] Consistent and correct use of condoms also reduces the risk of acquiring other STIs and associated conditions, including genital warts and cervical cancer.[x] With a failure rate of about 2% when used consistently and correctly, condoms are very effective at preventing unintended pregnancy.[xi] [xii]
Condoms have played a decisive role in HIV, STI and pregnancy prevention efforts in many countries.
Condoms have helped to reduce HIV transmission and curtailed the broader spread of HIV in settings where the epidemic is concentrated in specific populations.[xiii] Distribution of condoms has been shown to reduce rates of HIV and other STIs in sex workers[xiv] [xv] [xvi] and men who have sex with men.[xvii] In India[xviii] [xix] and Thailand[xx] increased condom distribution to sex workers and their clients in combination with other prevention interventions were associated with reductions of transmission of both HIV and other STIs. Zimbabwe[xxi] and South Africa are two high-prevalence countries where increased condom use was found to contribute to reductions in HIV incidence.[xxii]
A recent global modelling analysis estimated that condoms have averted around 50 million new HIV infections since the onset of the HIV epidemic.[xxiii] For 2015, 27 billion condoms expected to be available globally through the private and public sector will provide up to an estimated 225 million couple years protection from unintended pregnancies.[xxiv] [xxv]
Condoms remain a key component of high-impact HIV prevention programmes.
Recent years have seen major scientific advances in other areas of HIV prevention. Biomedical interventions including antiretroviral therapy (ART) for people living with HIV can substantially reduce HIV transmission. While the success of ART may alter the perception of risk associated with HIV, studies have shown that people living with HIV who are enrolled in treatment programmes and have access to condoms report higher condom use compared to those not enrolled.[xxvi]
Condom use by people on HIV treatment and among serodiscordant couples is strongly recommended. [xxvii] Only when sustained viral suppression is confirmed and very closely monitored, and when the risk of other STIs and unintended pregnancy is low, it may be safe not to use condoms.[xxviii] [xxix] [xxx]
Oral pre-exposure prophylaxis (PrEP)—where antiretroviral drugs are used by HIV-negative people to reduce their risk of acquiring HIV—is also effective in preventing HIV acquisition, but is not yet widely available and is currently only recommended as an additional tool for people at higher risk, such as people in sero-discordant relationships, men who have sex with men and female sex workers, in particular in circumstances in which consistent condom use is difficult to achieve.[xxxi] Voluntary medical male circumcision (VMMC) can reduce the risk of HIV acquisition by 60% among men, but because protection is only partial, should be supplemented with condom use. [xxxii]
Hence, condom use remains complementary to all other HIV prevention methods, including ART and PrEP, in particular when other STIs and unintended pregnancy are of concern. The roll-out of large-scale HIV testing and treatment, VMMC and STI control programmes, and efforts to increase access to affordable contraception all offer opportunities for integrating condom promotion and distribution.
Quality-assured condoms must be readily available universally, either free or at low cost.
To ensure safety, efficacy and effective use, condoms must be manufactured according to the international standards, specifications and quality assurance procedures established by WHO, UNFPA and the International Organization for Standardization[xxxiii] [xxxiv] and made available either free or at affordable cost. Condom use in resource-limited settings is more likely when people can access them at no cost or at subsidized prices.[xxxv] [xxxvi]
Most countries with high HIV rates continue to heavily depend on donor support for condoms. In 2013, only about 10 condoms were made available to every man aged 15-64, and on average only one female condom per eight women in sub- Saharan Africa. HIV prevention programmes need to ensure that a sufficient number and variety of quality assured condoms are accessible to people who need them, when they need them. Adequate supplies of water based-lubricants also need to be provided to minimize condom usage failure, especially for anal sex, vaginal dryness and in the context of sex work.[xxxvii]
Despite generally increasing trends in condom use over the past two decades, substantial variations and gaps remain. Reported condom use at last sex with non-regular partners ranges from 80% use by men in Namibia and Cambodia to less than 40% usage by men and women in other countries, including some highly affected by HIV. Similarly, among young people aged 15 to 24 years, condom use at last sex varies from more than 80% in some Latin American and European countries to less than 30% in some West African countries.[xxxviii] This degree of variation highlights the need for countries to set ambitious national and subnational targets and that in many settings there are important opportunities for strengthening demand and supply of condoms.
Programmes promoting condoms must address stigma and gender-based and socio-cultural factors that hinder effective access and use of condoms.
Effective condom promotion should be tailored for people at increased risk of HIV and other STIs and/or unintended pregnancy, including young people, sex workers and their clients, injecting drug users and men who have sex with men. Many young women and girls, especially those in long-term relationships and sex workers, do not have the power and agency to negotiate the use of condoms, as men are often resistant to using condoms. Within relationships, the use of condoms may be taken to signal a lack of trust or intimacy.
However, few programmes adequately address the barriers that hinder access and use of condoms by young people,[xxxix] key populations[xl] and men and women in relationships. In some contexts, sex workers are forced to have unprotected sex by their clients.[xli] [xlii] and carrying condoms is criminalized and used as evidence by police to harass or to prove involvement in sex work[xliii] [xliv] These practices undermine HIV prevention efforts and governments should take actions to end these human rights violations.[xlv] Condom programmes should ensure that condoms and lubricants are widely available and that young people and key populations have the knowledge, skills and empowerment to use them correctly and consistently.[xlvi] Condoms should also be made available in prisons and closed settings,[xlvii] [xlviii] and in humanitarian crises situations.[xlix]
Adequate investment in and further scale up of condom promotion is required to sustain responses to HIV, other STIs, and unintended pregnancy.
Despite the low cost of condoms, international funding for condom procurement in sub-Saharan Africa has stagnated in recent years.[l] Collective actions at all levels are needed to support the efforts of countries that depend on external assistance for condom procurement, promotion, and distribution and to increase domestic funding and private sector investment in condom distribution and promotion.[li]
Although condoms are part of most national HIV, STI and reproductive health programmes, condoms have not been consistently distributed nor promoted proactively enough.[lii] National condom distribution and sales can be strengthened by applying a total market approach that combines public sector distribution, social marketing and private sector sales.[liii] [liv] Administrative barriers that prevent programmes and organizations from providing sufficient quantities of condoms for distribution need to be removed. In high-HIV prevalence locations condom promotion and distribution should become systematically integrated in community outreach and service delivery, and in broader health service provision.
[i] UNAIDS. 2014. World AIDS Day Report 2014.
[ii] WHO, Dept. of Reproductive Health and Research. Global incidence and prevalence of selected curable sexually transmitted infections.
[iii] UNFPA/Guttmacher Institute. 2012. Adding It Up: Costs and Benefits of Contraceptive Services.
[iv] Sedgh G et al. Intended and Unintended Pregnancies Worldwide in 2012 and Recent Trends. Studies in Family Planning, 2014, Vol 45. 3, 301–314, 2014.
[v] Carey RF et al. Effectiveness of latex condoms as a barrier to human immunodeficiency virus-sized particles under conditions of simulated use. Sex Transm Dis 1992;19:230-4.
[vi] WHO/UNAIDS. 2001. Information note on Effectiveness of Condoms in Preventing Sexually Transmitted Infections including HIV.
[vii] Holmes K et al. Effectiveness of condoms in preventing sexually transmitted infections. Bulletin of the World Health Organization, 2004, 82 (6).
[viii] Weller S et al. Condom effectiveness in reducing heterosexual HIV transmission. Cochrane Database Syst Rev. 2002;(1):CD003255.
[ix] Smith DK et al. Condom effectiveness for HIV prevention by consistency of use among men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2015 Mar 1;68(3):337-44.
[x] Also see: http://www.cdc.gov/condomeffectiveness/brief.html
[xi] Trussell J. Contraceptive efficacy, in: Hatcher RA et al., eds., Contraceptive Technology: Twentieth Revised Edition, New York: Ardent Media, 2011, pp. 779–863.
[xii] Kost K et al. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception, 2008; 77:10-21.
[xiii] Hanenberg RS et al. Impact of Thailand's HIV-control programme as indicated by the decline of sexually transmitted diseases. Lancet, 1994, 23;344(8917): 243-5.
[xiv] Ghys PD et al. Increase in condom use and decline in HIV and sexually transmitted diseases among female sex workers in Abidjan, Cote d’Ivoire, 1991–1998. AIDS, 2002, 16(2):251–258.
[xv] Levine WC et al. Decline in sexually transmitted disease prevalence in female Bolivian sex workers: impact of an HIV prevention project. AIDS, 1998, 12(14):1899–1906.
[xvi] Fontanet AL et al. Protection against sexually transmitted diseases by granting sex workers in Thailand the choice of using the male or female condom: results from a randomized controlled trial. AIDS, 1998, 12(14):1851–1859.
[xvii] Smith D et al. Condom efficacy by consistency of use among MSM: US. 20th Conference on Retroviruses and Opportunistic Infections, Atlanta, abstract 32, 2013.
[xviii] Boily M-C et al. Positive impact of a large-scale HIV prevention programme among female sex workers and clients in South India. AIDS, 2013, 27:1449–1460.
[xix] Rachakulla HK et al. Condom use and prevalence of syphilis and HIV among female sex workers in Andhra Pradesh, India - following a large-scale HIV prevention intervention. BMC Public Health, 2011; 11 (Suppl 6): S1.
[xx] UNAIDS. 2000. Evaluation of the 100% Condom Programme in Thailand, UNAIDS Case Study.
[xxi] Halperin DT et al. A surprising prevention success: Why did the HIV epidemic decline in Zimbabwe? PLoS Med. 2011. 8;8(2).
[xxii] Johnson LF et al. 2012. The effect of changes in condom usage and antiretroviral treatment coverage on human immunodeficiency virus incidence in South Africa: a model-based analysis, Journal of the Royal Society Interface. 2012, 7;9(72):1544-54.
[xxiii] Stover J. 2014. Presentation. UNAIDS Global Condom Meeting, Geneva, November 2014.
[xxiv] In line with standard assumptions, 120 condoms are required for 1 couple year of protection. Projected condom sales for 2015 cited based on: Global Industry Analysts. 2014. Global Condoms Market. May 2014.
[xxv] Stover J et al. Empirically based conversion factors for calculating couple-years of protection. Eval Rev. 2000 Feb; 24(1):3-46.
[xxvi] Kennedy C et al. Is use of antiretroviral treatment (ART) associated with decreased condom use? A meta-analysis of studies from low- and middle-income countries (LMICs). July 2014 h International AIDS Conference. Melbourne, WEAC0104 - Oral Abstract Session.
[xxvii] Liu H et al. Effectiveness of ART and condom use for prevention of sexual HIV transmission in sero-discordant couples: a systematic review and meta-analysis. PLoS One. 2014 4;9(11):e111175.
[xxviii] Swiss AIDS Federation Advice Manual: Doing without condoms during potent ART. Swiss AIDS Federation, 2008.
[xxix] Fakoya A et al. British HIV Association, BASHH and FSRH guidelines for the management of the sexual and reproductive health of people living with HIV infection. HIV Medicine, 2008, 9: 681-720, 2008.
[xxx] Marks G et al. Time above 1500 copies: a viral load measure for assessing transmission risk of HIV-positive patients in care. AIDS 2015, 29:947–954.
[xxxi] WHO. 2015. Technical update on Pre-exposure Prophylaxis (PrEP), February 2015. WHO/HIV/2015.4.
[xxxii] WHO. 2007. New Data on Male Circumcision and HIV Prevention: Policy and Programme Implications. WHO/UNAIDS Technical Consultation on Male Circumcision and HIV Prevention: Research Implications for Policy and Programming Montreux, 6 – 8 March 2007 Conclusions and Recommendations.
[xxxiii] WHO, UNFPA and Family Health International. 2013. Male Latex Condom: Specification, Prequalification and Guidelines for Procurement, 2010 revised April 2013.
[xxxiv] International Organisation for Standardisation. 2014. ISO 4074:2014 Natural rubber latex male condoms -- Requirements and test methods. http://www.iso.org/iso/catalogue_detail.htm?csnumber=59718.
[xxxv] Charania MR et al. Efficacy of Structural-Level Condom Distribution Interventions: A Meta-Analysis of U.S. and International Studies, 1998–2007. AIDS Behav, 2011, 15:1283–1297.
[xxxvi] Sweat MD et al. Effects of condom social marketing on condom use in developing countries: a systematic review and meta-analysis, 1990–2010. Bulletin of the World Health Organization 2012, 90:613- 622A. doi: 10.2471/BLT.11.094268.
[xxxvii] Use and procurement of additional lubricants for male and female condoms: WHO/UNFPA/FHI360 Advisory note. 2012.
[xxxviii]Source: Data from a database of Demographic and Health Surveys (DHS) available at statcompiler.com (verified January 2015).
[xxxix] Dusabe J, et al. “There are bugs in condoms”: Tanzanian close-to-community providers’ ability to offer effective adolescent reproductive health services. J Fam Plann Reprod Health Care 2015;41:e2.
[xl] Key populations are defined groups who, due to specific higher-risk behaviours, are at increased risk of HIV irrespective of the epidemic type or local context. Also, they often have legal and social issues related to their behaviours that increase their vulnerability to HIV. These guidelines focus on five key populations: 1) men who have sex with men, 2) people who inject drugs, 3) people in prisons and other closed settings, 4) sex workers and 5) transgender people. In consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations. World Health Organization 2014.
[xli] Global Commission on HIV and the Law. Risks, Rights & Health. 2012
[xlii] UNAIDS. 2014. The Gap report.
[xliii] Open Society Foundations. 2012. Criminalizing condoms. How policing practices put sex workers and HIV services at risk in Kenya, Namibia, Russia, South Africa, the United States and Zimbabwe. http://www.opensocietyfoundations.org/reports/criminalizing-condoms.
[xliv] Bhattacharjya, M et al. The Right(s) Evidence – Sex Work, Violence and HIV in Asia: A Multi-Country Qualitative Study. Bangkok: UNFPA, UNDP and APNSW (CASAM). 2015.
[xlv] WHO; UNFPA; UNAIDS; NSWP; World Bank. 2013. Implementing comprehensive HIV/STI programmes with sex workers: practical approaches from collaborative intervention. 2013.
[xlvi] Vijayakumar G et al. A review of female-condom effectiveness: Patterns of use and impact on protected sex acts and STI incidence. International Journal of STD and AIDS, 2006, 17(10):652-659.
[xlvii] UNODC/WHO/UNAIDS. 2006. HIV/AIDS Prevention, Care, Treatment and Support in Prison Settings A Framework for an Effective National Response.
[xlviii] UNODC/ILO/UNDP/WHO/UNAIDS. 2012. Policy brief. HIV prevention, treatment and care in prisons and other closed settings: A comprehensive package of interventions.
[xlix] Inter-Agency Standing Committee (IASC). 2003. Guidelines for HIV/AIDS interventions in emergency settings. Task Force on HIV/AIDS in Emergency Settings.
[l] UNFPA. 2015. Contraceptives and condoms for family planning and STI/HIV prevention. External procurement support report 2013.
[li] Foss AM et al. A systematic review of published evidence on intervention impact on condom use in sub-Saharan Africa and Asia. Sex Transm Infect 2007, 83:510–516.
[lii] Fossgard IS et al. Condom availability in high risk places and condom use: a study at district level in Kenya, Tanzania and Zambia. BMC Public Health 2012, 12:1030.
[liii] UNFPA-PSI. 2013. Total Market Approach Case Studies Botswana, Lesotho, Mali, South Africa, Swaziland, Uganda. http://www.unfpa.org/publications/unfpa-psi-total-market-approach-case-studies
[liv] Barnes, J et al. 2015. Using Total Market Approaches in Condom Programs. Bethesda, MD: Strengthening Health Outcomes through the Private Sector Project, Abt Associates.
Related
 Multisectoral resilience to funding cuts in Guatemala
Multisectoral resilience to funding cuts in Guatemala

22 December 2025













Feature Story
Promoting greater focus on HIV in humanitarian emergencies
06 July 2015
06 July 2015 06 July 2015AIDS strategies and efforts must give greater priority to humanitarian emergencies and the millions of people affected by them, members of the UNAIDS governing body agreed at the thematic segment of the 36th meeting of the UNAIDS Programme Coordinating Board (PCB), which took place in Geneva, Switzerland, on 2 July.
New data presented at the thematic session by the Office of the United Nations High Commissioner for Refugees (UNHCR), the World Food Programme (WFP) and UNAIDS Secretariat estimate that of the 314 million people affected by humanitarian emergencies in 2013, 1.6 million people--or 1 in 22-- are living with HIV, and many thousands more are at risk.
“We are talking about incredible numbers of people and multiple layers of vulnerability. This is too big a scale and impact to ignore. We have to ensure that HIV prevention and treatment services are systematically integrated into emergency responses,” said Mr Michel Sidibé, Executive Director of UNAIDS.
The thematic session contemplated the vast and complex issue of HIV in emergency contexts, including the delivery of health and HIV services in the context of conflict situations, natural disasters, public health emergencies, displacement and migration. On protection issues, vulnerability to HIV due to sexual violence, human rights violations, restrictions, punitive laws and policies were topics of discussion. On resilience, participants talked about the need for community building and preparedness.
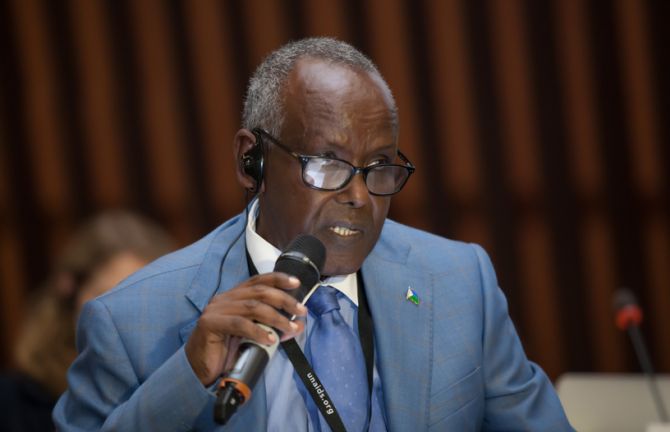
Panelists from a wide range of countries including Burundi, Central African Republic, Djibouti, Haiti, Lebanon, Liberia, Nepal, Nigeria, Sierra Leone and Ukraine told of the realities on the ground. They spoke of barriers and opportunities and gave examples of successful government and civil society efforts to address HIV in the wide variety of humanitarian emergency contexts.
In his keynote speech, former refugee Mr Noé Seisaba from Burundi, who founded the Stop SIDA organization that brings key HIV initiatives to refugee camps and settings, called for the community of people living with HIV to be involved in all aspects of planning and implementation. “I faced a lot of discrimination, but I broke my silence on HIV to try to make working on HIV a community issue and to show that we can intervene as refugees because we have a true understanding of the challenges and realities,” he said. “I am happy to see we are all talking about this issue, but I want to see concrete action.”
Many participants echoed that community involvement and empowerment of people living with and most affected by HIV are critical to achieve results for people in such difficult contexts. “If we are going to end the AIDS epidemic by 2030, we have to shine light on root causes of vulnerability in humanitarian settings and increase action to promote respect for rights and basic humanitarian dignity,” said Mr George Okoth-Obbo, Assistant High Commissioner for Operations at UNHCR.
Cross-regional strategies were encouraged to enable maximum impact and coverage of people. The challenge of sexual violence in emergency settings and gender inequalities was highlighted as a fundamental issue to be given greater focus, action and investment.
36th meeting of the PCB



Feature Story
2015 UNODC World Drug Report: drug use must be addressed as a pressing public health issue
26 June 2015
26 June 2015 26 June 2015The use of illicit drugs needs to be understood as a social and health condition requiring sustained prevention, treatment and care. This is one of the major conclusions emerging from the 2015 World Drug Report, published on 26 June by the United Nations Office on Drugs and Crime (UNODC).
Launched to coincide with the International Day against Drug Abuse and Illicit Trafficking, the report gives a detailed snapshot of the latest developments in drug use, production, trafficking and consequences for health. It finds that some 27 million people are dependent on drugs, half of whom inject; that an estimated 1.65 million people who inject were living with HIV in 2013 (around 13.5%) and that women who inject drugs, though fewer in number, are often much more likely to become infected than men.
In a specific chapter on HIV, it is also noted that there is a major issue in access to antiretroviral therapy and harm reduction programmes among people who inject drugs and that only one in six of all users suffering from drug use disorders or drug dependence benefit from such programmes, which include needle and syringe programmes and opioid substitution therapy. The report acknowledges that some progress has been made in lowering HIV transmission among people who inject drugs: newly diagnosed cases of HIV in this group fell by roughly 10% between 2010 and 2013. However, the international community is far off the global target of reducing transmission by 50% by 2015, set in the 2011 United Nations Political Declaration on HIV and AIDS.
The public health implications of illicit drug use highlighted in the report were explored at length during a special briefing in Geneva hosted by UNODC, UNAIDS and World Health Organization (WHO). During the event, UNODC Deputy Executive Director Aldo Lale-Demoz stressed the need for a multipronged approach which goes beyond disrupting criminal networks. “More also needs to be done in promoting the importance of understanding and addressing drug use as a social and health condition requiring sustained prevention, treatment and care,” he said.
Luiz Loures, UNAIDS Deputy Executive Director, stressed that a people-centred approach was required to reach people who use drugs. "We have the knowlege and technology to end the AIDS epidemic but access has been selective. The difference is determined by good or bad policy. Human rights should be guaranteed and health be at the centre of the response."
According to Shekhar Saxena, Director of WHO’s Department of Mental Health and Substance Abuse, national health care systems often lack the capacity to provide effective treatment and care to drug users. He added that WHO would continue to offer guidance and assistance to countries, “to strengthen health-care systems to reach the ultimate goal of the UN Drug Conventions – to protect the health and welfare of humankind.”
People who inject drugs account for some 30% of new HIV infections outside sub-Saharan Africa and two subregions have notably high rates of HIV infection among people who inject drugs: an estimated 29% in south-west Asia and around 23% in eastern and south-eastern Europe—a region with approximately 40% of the global number of such users living with HIV, mainly residing in the Russian Federation and Ukraine.