

Feature Story
Interactive TV series about HIV launched in Kyrgyzstan
13 November 2020
13 November 2020 13 November 2020A new television series for young people in the Kyrgyz language, School Elections, was launched online last week. During six 15–20-minute episodes, a girl, Ayana, who is living with HIV, tells her story of bullying, friendship and the fight for human dignity. The producers of the series hope that Ayana’s example will give hope to young people who face similar challenges.
“We have a simple idea to promote: you may differ from others in your health, appearance or level of wealth. But regardless of this, we all deserve respect, friendship, love and happiness. This series is about kindness and acceptance of others as they are,” said Azim Azimov, Head of Production at the Media Kitchen production studio and the main screenwriter of the series.
Starting on 6 November, new episodes will be aired weekly on YouTube and will also be broadcast on television, Instagram and the teens.kg youth project website. Additionally, each series has one to three interactive episodes—the leading actors invite the viewers to look at the problems raised in the series through the viewers’ eyes, experience each situation for themselves and make their own decisions.
According to the United Nations Educational, Scientific and Cultural Organization (UNESCO), more than 30% of students around the world experience various forms of bullying at the hands of their classmates. Students who are perceived as “different” are often subjected to bullying for reasons of appearance, health status, including HIV status, sexual orientation and gender identity, social status or the economic situation of the family.
“This series tells people about the complex issue in simple and understandable language, to show how strong-willed and honest young people can overcome ignorance, indifference, cruelty and injustice, inspire others and change life for the better,” said Tigran Yepoyan, UNESCO Regional Adviser on HIV, Education and Health.
“This series is a powerful new instrument for reducing stigma in our society, it not only shows the difficulties of living with HIV, discrimination and bullying but also motivates our adolescents not to be afraid to fight for dignity and justice and move forward towards their dreams,” said Meerim Sarybaeva, UNAIDS Country Director for Kyrgyzstan.
The official soundtrack of the series, which was supported by the UNESCO Institute for Information Technologies in Education and UNAIDS, was performed by the singer Ayim Ayilchieva.
Related
 Women, HIV, and war: a triple burden
Women, HIV, and war: a triple burden

12 September 2025
 Displacement and HIV: doubly vulnerable in Ukraine
Displacement and HIV: doubly vulnerable in Ukraine

11 August 2025




Feature Story
“Someone has to start”: how a Haitian transgender activist is inspiring hope through visibility
09 November 2020
09 November 2020 09 November 2020Haiti’s first safe house for transgender people opened last week. Kay Trans Ayiti launched with the snip of a red ribbon and cheers from a circle of activists and residents. The group took turns taking pictures between bobbing pink and blue balloons tied to the veranda.
The triumphant moment came during a tough time. Asked how transgender people have fared in Haiti during COVID-19, home founder Yaisah Val was emphatic. “When the rest of the population has a cold, the trans community has pneumonia. Just imagine that with the hunger, poverty and meagre resources in Haiti, we are always on the outside,” she says.
In many ways, Ms Val is not as shut out as the people she serves. Haiti’s first publicly open transgender woman introduces herself as a mother of two and a wife. She has a degree in education and clinical psychology. She was a teacher and school counsellor before becoming a full-time community mobilizer, activist and gender identity spokesperson. During what she calls her stealth years, she was easily accepted as a woman.
Born in the United States of America to Haitian parents, she has had the benefit of a stable home, supportive teachers and a wildly loving grandmother.
“If you are going to be a sissy you will be the best sissy there is because you are mine,” her granny told her when she was a boy named Junior.
This is an anomaly. According to the United Caribbean Trans Network, transgender people in the region are far less likely to be supported by family, complete their secondary education and be employed. They are more likely to be homeless, to sell sex to survive and to face extreme violence. All this sharply increases the community’s HIV risk. A recent study found that transgender women in Haiti had an HIV prevalence of 27.6%—14 times higher than the general population.
But notwithstanding her “privileged” life, Ms Val’s 47-year journey has been fraught.
From when she was two or three years old she knew she was a girl. The gender policing from relatives was immediate and incessant: “Straighten up that boy. You can’t let him grow up like that.” At seven she was admitted to Washington Children’s Hospital with self-inflicted wounds to her genitals. Puberty was, “hell … a lot of confusion and self-hate.”
About 20 years ago she became herself during the Haitian Carnival. She braided her hair, slipped into a dress and boarded a loud, colourful tap-tap bus with her friends. One man flirted. He called her pretty and opened doors. She felt like Cinderella.
“That boy eventually found out and beat me within an inch of my life,” Ms Val remembers. “Whether you are upper class or middle class or on the streets, as long as you are trans it does not matter. Once you disclose, all respect is gone … you are just this thing. That one word disarms you of all humanity in people’s eyes.”
Transitioning offered a sort of freedom, “I was living and being seen as who I am, who I had always been.” But the fear of being assaulted or excluded made her identity a stressful secret. Old boyfriends did not know she was transgender until she came out years later. She only disclosed to the man who would become her husband after they had lived together for a year and were on the brink of getting married.
“I don’t recommend people do that,” Ms Val says again and again, referring to transgender people hiding their gender identity from romantic partners. “It can be violent. It can be dangerous.”
In her case it worked out. Her partner decided that she was the same person he knew and loved. Three years ago, the story repeated when she disclosed to her children.
“I was just surprised,” her son, Cedrick said. “I was shocked in a good way. They’d slowly started educating me over the years, so I understood what it meant. Ever since then the whole mother/son bond went to a new level for both of us. It filled in all those gaps. Now everything made sense, like her childhood stories.”
Coming out to those closest to her has opened the floodgates to activism. In 2016, Ms Val became the first person in Haiti’s history to publicly identify as a transgender person. She has been a key partner for UNAIDS Haiti and the island’s lesbian, gay, bisexual, transgender and intersex (LGBTI) people organizations. Last year she participated in a national dialogue on LGBTI rights. Together with her husband she started taking in homeless transgender people. That paved the way for Kay Trans Ayiti, which now houses 10 transgender people. Fundraising is under way for a programme of psychosocial support, hormonal replacement legal advice and job training. One of their employment initiatives is a food cart. Some of their residents are living with HIV. They are supported to remain adherent to their antiretroviral treatment.
Ms Val knows first-hand how terrifying it is to access sexual and reproductive health care as a transgender woman. She recalls the experience of going to a gynaecologist in Haiti to get a check-up related to her vaginoplasty. The doctor did not understand what “transgender” meant. That visit ended with the gynaecologist calling other doctors to gawk.
“I was a YouTube channel, a Google page … anything but a human being. I was upset. I was crying. This is why transgender people do not access health care! We have a lot of transmen with gynaecological issues who make herbal treatments rather than go to the doctor,” Ms Val says.
Her group, Community Action for the Integration of Vulnerable Women in Haiti (Action Communautaire pour l’integration des Femmes Vulnerable en Haiti, or ACIFVH), is working with two HIV clinics to sensitize health-care providers. Combatting the ignorance and conservatism is a tall task. Even after educational sessions some doctors and nurses have tried pushing their religious views on the trainers.
“I was lucky not to be hindered by transphobia and discrimination,” Ms Val reflects. “Imagine if I did not have a supportive grandmother, an education and opportunities. I would not have been the person you see now.
“If you throw a seed on concrete it is not going to thrive. Being trans is not the problem. It is the reaction people have to it: throwing them on the streets, not letting them work, not taking them into schools. We need to have a place in society. It is hard. It will take a while. But someone has to start.”
Our work
Region/country
Related



Feature Story
20–50–80 to reach 100 in Ukraine
06 November 2020
06 November 2020 06 November 2020Ukraine has announced that it is now funding 80% of its national HIV response’s HIV prevention, care and support programmes.
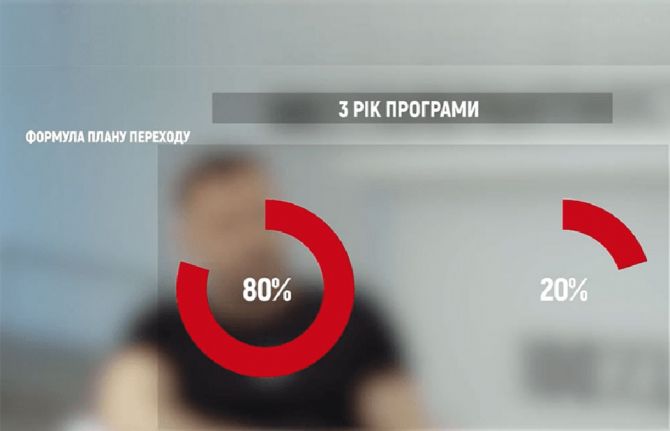
Under its 20–50–80 transition plan, which began in 2018, the government committed to increasing its share of the funding of HIV prevention, care and support programmes, which previously were fully funded by international donors, over three years. In the first year of the transition plan, the state was to finance 20% of those programmes, with the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) providing 80%. In the second year, the ratio was to reach 50/50 and in the third year 80% of funding was to be provided by the state, with 20% from by the Global Fund. This level of funding, which comes from both national and local budgets and is for prevention, care and support programmes within the national HIV and tuberculosis (TB) response and for the procurement of HIV/TB-related services from community organizations, has now been achieved.
The transition plan was proposed by a group of public and community organizations led by 100% Life, formerly called the All-Ukrainian Network of People Living with HIV. Dmytro Sherembey, the Head of the Board of 100% Life, said that most of the funding of the country’s HIV response used to come from donors, primarily the Global Fund. The 20–50–80 formula provided a simple algorithm tied to an agreed timeframe and obliged the government to increase domestic funding, since under the plan donor financing would be stopped if the government failed to meet its obligations.
“It was not an easy decision. It would have been easier to just sign a grant with the Global Fund. But we understood that if the government did not increase its funding, about half a million people who use the services would be left with nothing,” said Mr Sherembey. Also, since the government is unable to provide a wide spectrum of HIV prevention, care and support services on its own, community organizations have stepped in. However, there was a worry that reduced funding for community organizations would result in their being unable to provide such services, resulting in hundreds of thousands of people being deprived of care.
A Strategic Group for the Implementation of the Transition Plan, which included the Public Health Centre of Ukraine’s Ministry of Health, 100% Life, UNAIDS, the ICF Alliance for Public Health, Renaissance and Deloitte, developed new mechanisms through which local community organizations could cooperate with local authorities. The Sumy and Poltava regions of Ukraine were the first to start financing HIV and TB programmes from domestic funding. In 2018, the equivalent of more than US$ 650 000 was allocated to the programmes from Ukraine’s state budget.
“The transition plan provides an opportunity to continuously strengthen links between government and nongovernmental organizations in the provision of quality services to people living with HIV and tuberculosis. Nongovernmental organizations are moving away from their former role of volunteer activists and are starting to carry out professional social work and are accountable for its results. And the state, in turn, purchases their services through the public procurement system,” said Igor Kuzin, the Acting Director of the Centre for Public Health of the Ministry of Health of Ukraine.
With the support of Ukraine’s Ministry of Finance, the implementation of the transition plan progressed. In 2019, about US$ 4 million was allocated, equal to 50% of funding, which reached 25 regions in Ukraine. In 2020, the cost to the government of treatment and other services is expected to be about US$ 12.5 million, which is 80% of funding for such programmes.
“Together with the Public Health Centre of Ukraine’s Ministry of Health, and international and civil society partners, we will carefully monitor and analyse the results of this new model of HIV service delivery in order to ensure its sustainability, effectiveness and consistency,” said Raman Hailevich, the UNAIDS Country Director for Ukraine.
Our work
Region/country
Related


Feature Story
A tale of two Jamaican clinics during COVID-19
03 November 2020
03 November 2020 03 November 2020A woman living with HIV is at the Centre for HIV Research and Education Services (CHARES) in Kingston, Jamaica. She normally gets a three-month allotment of her antiretroviral medicines. But not this time. The doctor warns her that, since April, state pharmacies have only been dispensing a one-month supply.
About a 20-minute drive away at the Comprehensive Health Clinic, a client waits for his name to be called. He doesn’t use one of the wooden benches allocated for sexual health patients. Instead, he finds a nearby seat and listens intently.
HIV service providers in Jamaica have been challenged this year with responding both to new challenges caused by COVID-19 and long-standing service delivery stumbling blocks. The UNAIDS Country Director, Manoela Manova, wanted to get a better understanding of the issues on the ground, so she visited both treatment sites to speak with everyone, from adherence counsellors to doctors.
The University Hospital of the West Indies’ CHARES has been a best practice model for HIV treatment in Jamaica. For the island as a whole, 79% of those on treatment were virally suppressed last year. At CHARES, however, an impressive nine in every 10 clients are virally suppressed and therefore keep healthy and are unable to transmit the virus.
But even for this accomplished programme, COVID-19 has presented significant challenges.
Laboratory support has been diverted toward COVID-19 and there has been a backlog in receiving viral load testing results.
CHARES had been used to writing three-month prescriptions for stable clients, but since COVID-19, state-run pharmacies have been dispensing only a one-month supply. This is part of the government’s strategy to avoid stock-outs given the supply chain challenges at this time, but it means that those on treatment need to go out to get their medicines more often. CHARES has begun home deliveries, particularly for older people, who are more reluctant to venture out given the novel coronavirus risk.
COVID-19 containment measures have increased the need for mental health support. Income loss, school closures and curfews have placed an added strain on thousands of Jamaican households, including many people living with HIV. But when clients are referred to psychiatric support in the main hospital they rarely go for fear of experiencing discrimination. Further, since the hospital in which CHARES is located is a designated COVID-19 treatment site, some clients have opted to stay away.
“We need closer monitoring and evaluation to address the challenges around patient management at this time,” said CHARES Programme Director Racquel Brown. “Optimally we would like to hire someone with responsibility for analysing patient data to make more strategic decisions around care and treatment.”
The Comprehensive Health Centre serves a number of people living with HIV alongside those infected with other sexually transmitted infections. Here, too, multimonth dispensing has not been possible during COVID-19. Patients’ need for nutrition support has been high during this period. Some have had their antiretroviral medicines but no food with which to take them.
But other challenges came before COVID-19. Two out of five clients are lost to follow-up. Patients have given service providers wrong addresses. And the clinic’s viral suppression rate stands at 70%, below the national average. Some come off their treatment against their doctor’s advice.
Ms Manova said many of the challenges at both clinics are linked to self-stigma and discrimination, which is the main issue facing Jamaica’s HIV response. For the country as a whole, just 43% of all people living with HIV were on treatment in 2019 despite the island’s relatively high testing coverage.
“Before and during COVID-19, our results are undermined by shame, fear and prejudice,” she noted. “For an effective public health response, we have to be deliberate and consistent about building trust with communities and combatting all forms of stigma and discrimination that block people from accessing care.”
“It was inspiring and sobering to spend time with these health-care providers,” Ms Manova said. “Jamaica has correctly treated community health-care employees as essential workers. Staff including community facilitators, social workers, adherence counsellors and case managers are just as needed as doctors and nurses. Their work is critical at this time to address the individual needs and emotions that could affect treatment outcomes.”
Our work
Region/country
Related
 Multisectoral resilience to funding cuts in Guatemala
Multisectoral resilience to funding cuts in Guatemala

22 December 2025

Feature Story
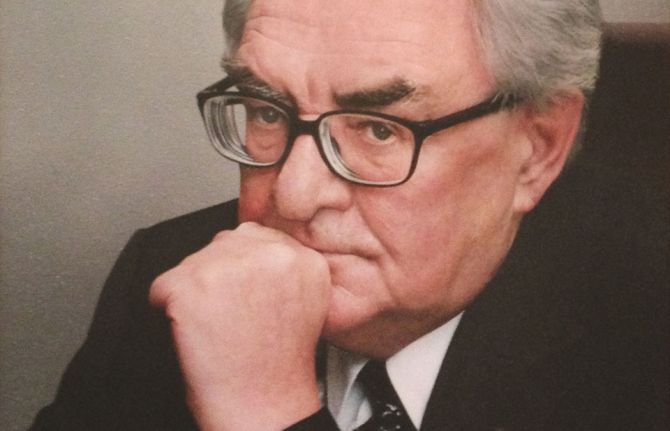
UNAIDS saddened by the death of Valentin Pokrovsky, a Russian leader on HIV, medicine and pandemic preparedness
30 October 2020
30 October 2020 30 October 2020By Alexander Goliusov, Director, Regional Support Team for Eastern Europe and Central Asia
When I was a young epidemiologist working at the Soviet Ministry of Health, Valentin Pokrovsky was respected as someone who was bigger than life—a living legend. He was already respected as the Director of the Central Research Institute of Epidemiology, the leading centre in the Soviet Union for research and expertise on responding to epidemiological outbreaks.
In the mid-1980s, when growing numbers of AIDS cases were being reported in other countries, some hoped that HIV would never reach the Soviet Union. I remember Mr Pokrovsky speaking out publicly, reminding officials, health workers and the public that we all needed to treat HIV as a serious risk to health. In 1987, he led the medical team that diagnosed the first person with AIDS in Moscow. His public insistence that this was just the first diagnosed case of AIDS was critical to mobilizing the early response to HIV across the Soviet Union.
Even after the end of the Soviet Union, I remember how Russian health workers and policymakers still looked to Mr Pokrovsky for training, leadership and expertise. Epidemiologists who studied under him at the Institute of Epidemiology always inspired admiration and perhaps even a little jealousy. They were always some of the best trained epidemiologists in the Russian Federation. They were ready to be at the forefront of investigating outbreaks of HIV, anthrax or diphtheria. During each of these outbreaks, Mr Pokrovsky encouraged health workers, the Ministry of Health and local officials to follow the science, collect the data and save lives. During this period of transition, he was called on to lead the first Russian Academy of Medical Sciences, from 1992 to 2006. Long after many colleagues from his generation had already retired from official roles and research, he continued to run the Institute of Epidemiology, now part of the Russian Federal Service for Surveillance on Consumer Rights Protection and Human Wellbeing (Rospotrebnadzor).
During his 47 years of leadership at the Institute of Epidemiology, Mr Pokrovsky pioneered many areas of research and prevention, including the prevention of nosocomial infections. Long before HIV, hepatitis C, staphylococcus or COVID-19 were highlighted as high risks for hospital-based infections, he pioneered the national programme on the prevention of nosocomial infections.
When I got the sad news this morning that Mr Pokrovsky had passed away at the age of 91 years, I immediately remembered how generations of Soviet and Russian health professionals and people living with HIV benefitted from his wisdom and dedication. He maintained his advocacy and leadership on HIV, always pushing doctors and officials to collect data and advance research that would have a practical impact on saving lives. In my last conversation with him two years ago, he reminded me that there is no room for complacency:
“Now is not the time to doze off. We have to work much harder to get the HIV epidemic under control.” Valentin Pokrovsky, 1929–2020
Region/country
Related




Feature Story
Bringing HIV and COVID-19 testing services to hard-to-reach areas in Uzbekistan
30 October 2020
30 October 2020 30 October 2020The Russian Federation has donated a mobile clinic to Uzbekistan to provide primary health care for people in remote and hard-to-reach regions of the country, including testing for HIV, COVID-19 and other diseases.
The mobile clinic is equipped with the latest medical equipment and diagnostic systems, including for HIV and COVID-19, and is ready to provide people with access to integrated HIV testing and counselling and other forms of medical diagnostics and treatment.
“Thanks to this programme, the citizens of Uzbekistan living in different regions of the country will be able to receive timely information about the symptoms and ways of transmission of infectious diseases, which has become more important than ever,” said Botirjon Asadov, Uzbekistan Ambassador to the Russian Federation.
The clinic was donated as part of a technical assistance programme supported by the Russian Government that is being implemented by UNAIDS in partnership with the Federal Service for Surveillance on Consumer Rights Protection and Human Wellbeing (Rospotrebnadzor) and the nongovernmental organization AIDS Infoshare.
The programme aims to strengthen health systems, ensure better epidemiological surveillance of HIV and promote the scale-up of HIV prevention programmes among populations at higher risk in Armenia, Belarus, Kyrgyzstan, Tajikistan and Uzbekistan.
“Our work in today’s coronavirus pandemic is more relevant than ever. We continue our cooperation to fight COVID-19 and fully support the efforts of the Uzbek authorities to normalize the epidemic situation in the country as soon as possible, and assure that the Russian Federation is ready to provide the necessary assistance,” said Irina Bragina, Deputy Head of Rospotrebnadzor.
To date, 12 mobile clinics have been donated—four to Tajikistan, three to Armenia and five to Kyrgyzstan. Apart from the primary health-care services and a range of HIV screening services, the clinics provide tests for COVID-19, viral hepatitis and sexually transmitted infections and obstetrics, gynaecology, cardiology and urology care. All the mobile clinics offer services free of charge. So far, more than 1.6 million people have used the services provided by the clinics.
“Mobile clinics today not only continue providing primary health-care services, including HIV testing, but also have come to the forefront to combat a new threat—COVID-19,” said Aleksandr Goliusov, Director, a.i., of the UNAIDS Regional Support Team for Eastern Europe and Central Asia.
Our work
Region/country
Related



Feature Story
Community-led campaign encourages people living with HIV to start treatment
21 October 2020
21 October 2020 21 October 2020A new community-led public information campaign, It is in Your Power to, aimed at encouraging people living with HIV to start antiretroviral therapy has been launched in the four largest areas of the Russian Federation.
The campaign’s website has 12 “capsules” with inspiring stories told by people living with HIV. By “opening” the capsule, visitors can find out about people’s lives, find facts on antiretroviral therapy, ask questions and get help from peer counsellors on HIV-related issues.
All the stories deliver a message that being diagnosed with HIV does not define a person and that if people living with HIV start treatment they can live a long and productive life.
The campaign covers four major Russian areas—the Novosibirsk, Sverdlovsk and Chelyabinsk regions and the city of Saint Petersburg—where, according to the Federal AIDS Center of the Russian Federation, 200 000 people are living with HIV, about 20% of all registered HIV cases in the country.
“In the Sverdlovsk region, some people do not start treatment because they do not believe that HIV exists, some can’t accept their diagnosis, some are afraid of the side-effects of antiretroviral therapy and some have doubts about the effectiveness of the drugs. But the biggest obstacle is the fear of discrimination, fear of losing their job, fear of isolation. We believe we can address this by telling true stories of people living with HIV on treatment,” said Vera Kovalenko, Head of the New Life civil society organization.
The campaign was initiated and developed by several community-led civil society organizations, including Humanitarian Action (Saint Petersburg), the Humanitarian Project (Novosibirsk), Light of Hope (Chelyabinsk) and New Life (Sverdlovsk), with the support of a regional SOS_project funded by the Global Fund to Fight AIDS, Tuberculosis and Malaria and in close cooperation with other partners in the Russian Federation.
Denis Kamaldinov, Head of the Humanitarian Project, invited people to get help. “If you know you are HIV-positive but are not receiving treatment, please contact us for help. We will help with the registration at the AIDS centre. And the treatment is provided free of charge at the expense of the state,” he said.
“Our mission is to fight for every life, to give hope to everyone,” said Alexei Tananin, Head of Light of Hope.
Our work
Region/country
Related
 Women, HIV, and war: a triple burden
Women, HIV, and war: a triple burden

12 September 2025
 Displacement and HIV: doubly vulnerable in Ukraine
Displacement and HIV: doubly vulnerable in Ukraine

11 August 2025


Feature Story
COVID-19’s impact on HIV vertical transmission services reversed
27 October 2020
27 October 2020 27 October 2020Recent data collection has shown that the COVID-19 pandemic has had a significant impact on HIV testing services, but the impact on HIV treatment has been less than originally feared. The impact on services for the prevention of vertical transmission of HIV (from mother to child) is mixed—by April, countries generally saw a decline in the number of women tested for HIV at their first antenatal clinic visit, but by June that decline had been reversed.
As of August 2020, the UNAIDS, World Health Organization and United Nations Children's Fund data collection exercise to identify national, regional and global disruptions of routine HIV services caused by COVID-19 had collected data on the prevention of vertical transmission of HIV from 43 countries, of which 17 countries reported data that enable the identification of trends.
To measure the impact of COVID-19 on vertical transmission of HIV services, a ratio was calculated relative to January—for example, if the number of women reached in April was the same as in January, the ratio is 1; if there was a decline, the ratio is less than 1.
All countries except Mozambique and Jamaica experienced declines in women tested for HIV at their first antenatal clinic visit in April compared to January. By June or July, 14 of the 17 countries were back to the February level of testing (all except Indonesia, Botswana and Sierra Leone).
Among the 15 countries reporting on treatment among pregnant women living with HIV, all but five have recovered to the February numbers of women receiving treatment (except Botswana, South Africa, Sierra Leone, Togo and Guatemala).



Feature Story
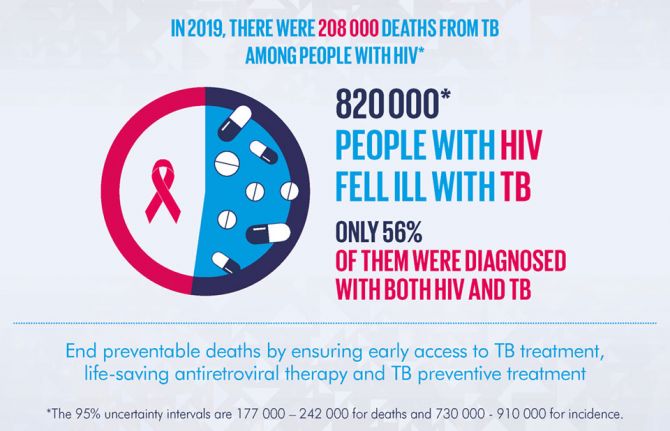
51st Union World Conference on Lung Health opens today as gains in reducing TB deaths risk being set back by COVID-19
20 October 2020
20 October 2020 20 October 2020The 51st Union World Conference on Lung Health opened today under the theme “Advancing Prevention”. In light of the COVID-19 pandemic, the conference is taking place virtually for the first time in its 100-year history. The event will feature cutting edge science around tuberculosis (TB), air pollution and tobacco control, but also deliver special sessions dedicated to COVID-19 and its intersection with lung health and infectious diseases. Speakers include Her Imperial Highness Crown Princess Akishino of Japan, President Bill Clinton, Shannon Hader, UNAIDS Deputy Executive Director and Divya Sojan—a nurse and TB survivor—among others.
According to the World Health Organization (WHO) Global Tuberculosis Report 2020, there has been an encouraging 63% reduction in tuberculosis deaths among people living with HIV since 2010. This is approaching the 75% global target reduction adopted in the 2016 United Nations Political Declaration on Ending AIDS. However, the report also shows that TB remains the leading cause of death among people living with HIV, resulting in just over 200 000 deaths in 2019—30% of all AIDS-related deaths.
Less than half of the estimated 815 000 people living with HIV who developed tuberculosis disease in 2019 were found, diagnosed and reported to national programmes as receiving treatment for both conditions. The remainder are either missed by programmes, not diagnosed or treated appropriately, or their treatment is incorrectly reported. Once diagnosed however, at least 90% of people with tuberculosis knew their HIV status in over 80 countries and territories and 88% of people living with HIV on TB treatment received lifesaving antiretroviral therapy.
Tuberculosis is curable and preventable. Tuberculosis preventive treatment has been recommended by WHO since 2004 for all people newly diagnosed with HIV. It prevents tuberculosis disease and save lives. Until recently, coverage had been woefully inadequate. However, a combination of advocacy, political commitment, increased availability of shorter, more acceptable treatment options, adequate funding and community engagement has led to an impressive increase in the number of people living with HIV who received TB preventative treatment.
In 2019, WHO reported that 3.5 million people living with HIV started TB preventative treatment – compared with 1.8 million in 2018. The total for 2018 and 2019—5.3 million—already represents 88% of the 6 million target set for 2022 in the 2018 United Nations Political Declaration on Tuberculosis; suggesting that this target could be achieved ahead of schedule.
“It took decades to overcome health worker and community doubts, mobilize specific funding for TB preventative treatment and to invest in research for shorter, more effective and more acceptable treatment regimens,” said Shannon Hader, Deputy Executive Director of UNAIDS, “Now we should raise the target and increase access to and use of the best TB preventative treatment regimens for all in need.”
COVID-19 is already disrupting TB and HIV services, adding to the dual stigma that prevents people from accessing services; lockdown measures that are a further barrier to people being tested or collecting their treatment for TB and HIV and diverting human, financial and laboratory resources away from tuberculosis and HIV.
It has been estimated that globally, a three-month lockdown and a protracted 10-month restoration could lead to an additional 6.3 million people falling ill with TB and an additional 1.4 million TB deaths over the next five years. That would result in a setback of at least five to eight years in the fight against TB – bringing 2021 global TB incidence and deaths to levels not seen since 2013 and 2016 respectively – due to the COVID-19 pandemic.
“Now, more than ever, is the time for the HIV and TB communities to team up and call for investment in shorter treatment and prevention regimens and better infection control, supported by the socioeconomic and human rights protections people need,” said Shannon Hader, UNAIDS Deputy Executive Director. “Overcoming COVID-19, TB, HIV and future pandemics requires global solidarity. Together we must develop and equitably distribute combination prevention, including vaccines, and treatment to all—true universal access that prioritizes those who need it most.”
Our work
Shannon Hader's Opening remarks at the 2020 Lung Health conference
Related


Feature Story
COVID-19’s impact on HIV treatment less severe than feared
16 October 2020
16 October 2020 16 October 2020While recent data collection has shown that the COVID-19 pandemic has had a significant impact on HIV testing services, the impact on HIV treatment is less than originally feared.
As of August 2020, the UNAIDS, World Health Organization and United Nations Children's Fund data collection exercise to identify national, regional and global disruptions of routine HIV services caused by COVID-19 had collected treatment data from 85 countries, of which 22 countries reported data over a sufficient number of months to enable the identification of trends.
To measure the impact of COVID-19 on HIV treatment services, a ratio was calculated relative to January—for example, if the number of people on treatment in April was the same as in January, the ratio is 1; if there was a decline, the ratio is less than 1.
Only five countries reported monthly declines in the number of people on treatment after April—these include Zimbabwe in June, Peru and Guyana in July, the Dominican Republic in April, and Sierra Leone in May through to July. The remaining 18 countries did not show a decline and some countries showed a steady increase (e.g. Kenya, Ukraine, Togo and Tajikistan).
One challenge in interpreting trends in the number of people currently on treatment is that many countries have a three-month lost-to-follow-up definition. This means that people who disengaged from treatment in April may only be counted as not on treatment in July.
Among the 22 countries with trend data on numbers newly initiating treatment, all countries except Jamaica showed declines for at least one month or more relative to January. Only around eight of those countries showed a rebound in the number of people newly initiating treatment between January and July.












