

Feature Story
“We must ensure that HIV treatment adherence is not compromised”—keeping people in Pakistan on HIV treatment
29 April 2020
29 April 2020 29 April 2020It was a rainy night when Asghar Satti, the National Coordinator of the Pakistan Association of People Living with HIV (APLHIV), went home after spending a busy day at the office.
That day, he had received a call from a man in Karachi, Pakistan, who is living with HIV. He was worried that he was running low on his supply of antiretroviral therapy, with only nine days of treatment left. That call was one of many such calls that he had received since the beginning of the lockdown put in place after the first case of COVID-19 was identified in Pakistan in late February.
“We need to do something that really benefits the community, we must ensure that HIV treatment adherence is not compromised,” Mr Satti thought.
In order to do just that, the APLHIV set up its Emergency Response Cell (ERC) in March. The ERC is working to ensure that everyone on HIV treatment gets an adequate supply of antiretroviral therapy, often delivered to their door.
Developed by the APLHIV, together with UNAIDS and Pakistan’s National AIDS Control Programme Common Management Unit for AIDS, TB and Malaria, the ERC’s Costed Contingency Plan groups all people living with HIV who are on treatment into three groups: red (people with a supply of antiretroviral therapy for less than two weeks); yellow (people with a supply of antiretroviral therapy for a month); and green (people with a supply of antiretroviral therapy for more than a month). These groups are then used to prioritize who receives packages of antiretroviral therapy, provided by the National AIDS Control Programme, through APLHIV and the Provincial AIDS Control Programme. The National AIDS Control Programme, through its Procurement and Supply Management Unit, provides packages of antiretroviral therapy to APLHIV, which are delivered by APLHIV through courier services to the doorsteps of people living with HIV who are unable to reach treatment centres.
As well as ensuring HIV treatment, other services provided by APLHIV include education for people living with HIV and key populations on COVID-19—more than 70 000 short messages in the local language on how to prevent COVID-19 were sent during the first four weeks of the lockdown. APLHIV, in close collaboration with the Provincial AIDS Control Programme, is also monitoring the 45 centres nationwide that provide antiretroviral therapy, checking that they have sufficient stocks of treatment and that people living with HIV are being provided with services without stigma and discrimination.
With a grant from the Global Fund to Fight AIDS, Tuberculosis and Malaria, APLHIV has provided nutritional support to more than 3200 people living with HIV in need. “You can never imagine what this support means to me, when I don’t have a single penny to feed myself or my siblings. The help we reached is a blessing from God,” one of the recipients said.
APLHIV, which has more than 15 000 people living with HIV from across Pakistan in its network, has also linked around 4000 people living with HIV with one of the social protection programmes launched by the government to support people in need during the COVID-19 pandemic.
“APLHIV will continue operating the Emergency Response Cell until the COVID-19 pandemic ends in the country,” Mr Satti said.
“Working with the community with APLHIV is always fulfilling. The work almost always centres around finding local solutions to effectively respond to the evolving needs of the people, of the community. It is not always easy, but with constant dialogue, innovative ideas are born and then nurtured. This multimonth antiretroviral therapy dispensing and the simple use of different colours to depict level of antiretroviral therapy available, which people can easy understand, is another home-grown innovation we are proud of,” said Maria Elena Filio Borromeo, UNAIDS Country Director for Pakistan and Afghanistan.
Resources
Region/country


Feature Story
COVID-19 responses must uphold and protect the human rights of sex workers
24 April 2020
24 April 2020 24 April 2020The Global Network of Sex Work Projects (NSWP) and UNAIDS recently released a joint statement calling on countries to take immediate, critical action to protect the health and rights of sex workers during the COVID-19 pandemic.
The pandemic, as with other health crises, is exposing existing inequalities and disproportionately affecting people already criminalized, marginalized and living in precarious health and economic situations, often outside social protection mechanisms.
Around the world, sex workers are being forgotten in government responses to the COVID-19 crisis. As sex workers and their clients self-isolate, sex workers are finding themselves unprotected, increasingly vulnerable and unable to provide for themselves and their families. In Ecuador, the Colectivo Flor De Azalea (the Association of Women Sex Workers) has highlighted the sudden lack of support and access to basic services that sex workers face. “Women sex workers have suffered a great impact due to the health emergency. We take to the streets with great fear and we are afraid of being violated. We do not have money for food, rent, medicine; health services are closed. There is no access to condoms—colleagues have died due to COVID-19.”
“Human rights law mandates that human rights are inalienable, universal, interdependent and indivisible,” said Winnie Byanyima, Executive Director of UNAIDS. “Ensuring that this is a reality for all—especially the most vulnerable among us—is essential during this pandemic, but will also build the resilient communities we need to emerge from it.”
As sex workers report interruptions to condom supplies owing to the pandemic, sex workers living with HIV say they are losing access to essential medicines as well. In Eswatini, Voice of Our Voices report that, “for those who are on HIV treatment, it is hard to meet their visit days as there is no transport. For prevention commodities, it is hard to reach them.”
With sex work criminalized in almost every country, sex workers are also more vulnerable to punitive measures linked to the enforcement of COVID-19 regulations. Increased policing can expose sex workers to more harassment and violence, and in several countries has already led to home raids, compulsory COVID-19 testing and the arrest and threatened deportation of migrant sex workers. For those who are driven to the streets by homelessness, as has become the case for many brothel and migrant sex workers, the lack of support means little safety or means to follow through on government requirements.
The criminalization of sex work in most countries also poses particular challenges for accessing government support. In the United States of America, SWOP-Tucson (the Sex Workers Outreach Project) explained that, “many of these schemes require proof that employment has been lost or reduced as a result of COVID-19. Because sex work is criminalized, it’s not possible to provide necessary paperwork and proof of unemployment or hardship. Thus, sex workers can’t get rent/mortgage relief, utility payment abatements or unemployment checks.”
Even in countries where sex work is legalized to some degree, many sex workers are finding that the system of benefits extended to workers in the formal sector does not include them. This is the case in Germany, for example, where sex workers highlight the barriers to accessing support for anyone living outside of the system. “While the government has provided a package for (registered) freelance workers, sex workers have not been in any way addressed in particular, and there is no potential for anyone living here illegally to access money from them.”
As the global crisis deepens, sex workers are increasingly faced with the difficult choice of isolation with no income or support or working at a risk to their own health and safety. Another problem has been that the majority of affordable short-term housing opportunities have closed while sex workers struggle to pay rent or pay hotel room fees. This disappearance of short-term housing, coupled with the shuttering of workplaces, has resulted in sudden homelessness for sex workers in several countries, a situation that is especially aggravated for migrant sex workers, many of whom are also finding themselves stranded by border closures.
Despite the continued exclusion of sex worker communities from emergency public health planning groups, sex workers have begun coordinating their own responses to the crisis. Several mutual aid and emergency fundraising campaigns have been created, enabling sex workers and sex worker organizations to access and distribute funds and essential items. One such initiative was undertaken by And Soppeku, a sex worker-led organization in Senegal, which distributed food packages and hygiene kits to members in three regions (Dakar, Thies and Kaolack). Similar initiatives are being developed around the world in the absence of government action and support.
However, the self-organization of individuals and groups must not be considered a substitute for urgently needed government support. Governments are bound by international human rights law to respect, protect and fulfil human rights, without discrimination, even in times of emergency.
Sex workers and sex worker organizations are calling for equal protection under the law and access to income support and to health care. UNAIDS joins this call to action, underscoring the importance of a human rights-based approach to COVID-19 responses, centred on empowerment and community engagement.
Quotes in this article were gathered through NSWP’s COVID-19 Impact Survey, which is collecting responses from sex workers and sex worker organizations in order to monitor what governments are doing for the sex worker community at this time.
Resources
Related




Feature Story
Sex workers adapting to COVID-19
21 April 2020
21 April 2020 21 April 2020Although difficult for everyone, the COVID-19 pandemic has had severe impacts on key populations, many of whom are experiencing economic hardship and anxiety about their health and safety.
Rito Hermawan (also known as Wawan), the Advocacy Coordinator of the Network of Sex Workers of Indonesia (OPSI), explained that the places that sex workers work in Indonesia have been closed down. Since, for their own safety, sex workers are avoiding working on the streets, many have been left without an income, unable to make ends meet.
It’s been about a month since Indonesia enacted a set of preventive measures against COVID-19. With the uncertainty of when life may return to normal, OPSI is supporting the urgent needs of the sex worker community.
Many sex workers are increasingly needing mental health support to combat the stress and anxiety they are currently experiencing. In a rapid survey conducted by the Indonesian Positive Network to review the needs of people living with HIV and key populations, more than 800 out of 1000 people surveyed expressed a need to access mental health and psychosocial support.
In order to address this, OPSI uses social media to provide virtual mental health support. “Through our social media, we are able to reach sex workers and empower them with information, motivation and support. They need to know that they are not alone, even though we may not be physically close,” said Mr Wawan.
A video teaching meditation and breathing techniques was recently launched to help sex workers cope with stress and to improve their general well-being. OPSI is also highlighting innovative work, such as making masks for sex workers during the COVID-19 pandemic. For those who need one-on-one support, OPSI has also established a counselling hotline.
In addition to supporting the sex worker community in Indonesia, OPSI is also exploring ways for outreach efforts to be continued despite the current conditions. The essential work of outreach workers should not come to an abrupt halt because of COVID-19, but it will need to move to a virtual form.
With technical assistance from the United Nations Population Fund Indonesia, OPSI developed a module on virtual outreach. The module outlines how outreach workers can adapt their work online, such as by using WhatsApp. The outreach workers are provided with lists of HIV counselling and testing services that are still open in 88 districts in Indonesia, which they can use to refer sex workers.
Sex workers, like others, are facing incredible hardships during the COVID-19 pandemic, whether it be struggles with their mental health, difficulty in continuing their work and loss of income. The role of networks and organizations of sex workers like OPSI is incredibly important in ensuring that the needs of sex workers are supported at this vital time.
Resources
Region/country


Feature Story
UNAIDS and Reckitt Benckiser join forces to distribute hygiene packs to people living with HIV during the COVID-19 outbreak
17 April 2020
17 April 2020 17 April 2020UNAIDS Regional Support Team for Eastern and Southern Africa (RST ESA) and Reckitt Benckiser (RB) have today joined forces to distribute more than 195 000 “hygiene packs” to people living with HIV in the eastern and southern African (ESA) region. Twenty-five thousand additional packs will be supplied to Nigeria and Egypt.
The packs consist of a three-month supply of Dettol soap and Jik surface cleaner and will be distributed in 19 ESA countries through UNAIDS Country Offices and networks of people living with HIV as part of efforts to reduce exposure to the impact of COVID-19 among people living with HIV.
The ESA region has the biggest burden of HIV globally, with 20.6 million people living with HIV in 2018. While countries in the ESA region are currently relatively unaffected by COVID-19, it is critical to take bold and unprecedented steps to curtail the spread of the virus now, due to fragile health systems and extreme socio-economic inequalities.
“UNAIDS will be working closely with communities and networks of people living with HIV at a country level in the coming weeks to facilitate distribution of the hygiene packs. As we continue to respond to the COVID-19 pandemic in this region, it is important that communities lead and that we put people at the centre,” said Aeneas Chuma, Director of the UNAIDS RST ESA, a.i.
The initiative to distribute the hygiene packs is part of RB’s “Fight for Access Fund”, which aims to improve access to health, hygiene and nutrition for all.
“We are delighted to partner with UNAIDS, in our collective response to the global COVID-19 pandemic,” said Russell Taylor, RB’s Regional Director Africa, Health. “Our immediate focus is to address the stress faced by our consumers and communities where we operate, to break the chain of infection. The distribution of the hygiene packs to people living with HIV in a region which is heavily affected by the AIDS epidemic is a critical part of our response.”
Although there is currently no clear evidence that people living with HIV are at an increased risk of acquiring COVID-19 or of becoming more ill from it, many people living with HIV are ageing and/or have other health conditions. These include Tuberculosis, heart disease or lung disease, which are known to make people susceptible to more severe COVID-19 disease.
In addition, there are 6.8 million people living with HIV in the ESA region who do not have access to antiretroviral therapy which may compromise their immune systems.
Thus, UNAIDS encourages people living with HIV to take precautions to reduce exposure to COVID-19 and to reach out to their health-care providers to ensure they have adequate stocks of essential medicines. This includes following World Health Organization (WHO) guidelines of washing and/or sanitizing hands, practicing social distancing, and seeking health care if one is ill.
Resources
Region/country





Feature Story
Keeping HIV treatment available in Pakistan during COVID-19
15 April 2020
15 April 2020 15 April 2020Sitting near her broken window, Ashee Malik (not her real name), a transgender woman who lives in Punjab Province, Pakistan, is counting her earnings, realizing that her income has fallen sharply. Her only source of money is dancing, begging and entertaining her clients, but since the lockdown imposed on 20 March to stop COVID-19, she hasn’t been able to leave her home. Her bright clothes are in her wardrobe, as is her makeup kit, laying unused for weeks. “We are concerned about our well-being, as we do not have enough resources to support ourselves and our families,” she said.
Ms Malik’s story is similar to that of most transgender people living in Pakistan, who face stigma, discrimination and social isolation. Access to health services, education and employment is one of the many challenges that transgender people face in the country, despite the passing of the Transgender Persons Protection of Rights Act 2018. And COVID-19 and the associated lockdown are making matters worse. As of 15 April, there were more than 5900 confirmed cases of COVID-19 in Pakistan and 107 deaths.
Owing to the restrictions on the movement of people, there is a real risk of a disruption to critical services for people living with HIV, which disproportionality affects transgender people in Pakistan.
The Khawaja Sira Society (KSS), which works with transgender people, has stepped in to provide support, working with the most marginalized and promoting knowledge about how to prevent HIV and COVID-19.
“The transgender community is even more vulnerable due to the prejudice and stigma and discrimination against them. We need to develop a COVID-19 prevention model by keeping in mind the dynamics and issues of the community in this pandemic,” said Mahnoor Aka Moon Ali, the Director of Programmes for KSS.
During discussions that KSS had with 150 transgender people, of whom approximately 30% are living with HIV, several issues were repeatedly raised, including the lack of income and the small size of Dheras, community homes for transgender people, in which four or five transgender people live together, making social distancing difficult. Since most of the transgender people contacted are illiterate, public health campaigns on how to prevent infection by the coronavirus are not getting through. Fear of the disease is high, which is impacting on mental health. The Government of Pakistan has announced that food aid will be made available, but transgender people face challenges in accessing the scheme, which is dependent on verification based on the national identification card, something that most transgender people in the country simply don’t have.
Social media is increasingly being used during the lockdown and together with UNAIDS Pakistan, KSS is disseminating information on hygiene, preventive measures and social distancing on social media and is engaging with the community on COVID-19. KSS, together with provincial government authorities, is also working to ensure that people living with HIV can get multimonth refills of antiretroviral therapy delivered to their home.
“We as transgender people living with HIV feel we are at risk by visiting government-run antiretroviral therapy centres. We need antiretroviral therapy to be delivered to us,” said Guddi Khan, a transgender woman who is living with HIV.
Since an uninterrupted supply of antiretroviral therapy is essential for people living with HIV, the Pakistan Common Management Unit for AIDS, TB and Malaria, in collaboration with UNAIDS and other partners, has established virtual platforms and helplines in order to ensure that coordination is continued. An emergency stock of antiretroviral therapy has been made available for people living with HIV for the next two months and a buffer stock is being made available through the Global Fund to Fight AIDS, Tuberculosis and Malaria in order to avoid interruptions in the event that imports of medicines are disrupted.
“We are working closely with the Association of People Living with HIV, federal and provincial governments and the UNAIDS family to monitor the situation and quickly help address barriers in accessing life-saving HIV services in these extremely challenging times of the COVID-19 crisis,” said Maria Elena Borromeo, the UNAIDS Country Director for Pakistan and Afghanistan.
Resources
Region/country


Feature Story
Community networks extend arms to connect people to medicine in Viet Nam
17 April 2020
17 April 2020 17 April 2020When the Vietnamese Government introduced social distancing mid-March 2020 to respond to COVID-19, Binh Nam (not his real name), already on distance learning from his college since February, lost his part-time job at a small company. He decided to leave Ho Chi Minh City, which had a cluster of confirmed COVID-19 cases, to settle back in his home town, about 300 kilometres away.
“Going home seemed like the best option for me at the time,” Mr Nam said.
He arrived at his parents’ home just before buses shuttling people back and forth across the provinces stopped. With stricter lockdown measures taking effect in early April, he realized he was in a bind. He would run out of HIV treatment.
“I considered going to a local HIV clinic, but feared my HIV status would be disclosed,” he said. “I also could not buy antiretroviral medicine at private clinics because that would clear out my savings.”
And he definitely did not want to ask his parents, because they didn’t know he was living with HIV.
“I felt desperate,” he said. As a last resort, Mr Nam texted a man who runs a social media channel on HIV information, education and counselling that he follows.
Upon learning of Mr Nam’s situation, Nguyen Anh Phong, a representative of the Viet Nam Network of People Living with HIV (VNP+) in the south of Viet Nam and co-founder of the Lending a Helping Hand Fund, mobilized some funds to get him an antiretroviral therapy refill.
“This was among the first calls for help that made us notice more and more people were stuck in their home province with a limited amount of antiretroviral medicine,” Mr Phong said.
He and his VNP+ peers decided to form a group on one of the most popular social media chatting platforms in Viet Nam to find ways to connect people and help them collect medicine at clinics other than their own. More than 150 community members joined the group across the country.
Community feedback filtered back to the Viet Nam Authority for HIV/AIDS Control (VAAC) at the right time as it was drawing up emergency contingency plans. It was dealing with a hospital closed because of a temporary COVID-19 quarantine in Hanoi, so people couldn’t access HIV services or treatment. And with so many people stranded in the provinces, something had to be done.
VAAC issued new guidelines on HIV care and treatment during the pandemic developed with technical support from the United States President’s Emergency Plan for AIDS Relief, the Global Fund to Fight AIDS, Tuberculosis and Malaria and the United Nations.
“We invited the Viet Nam Network of People Living with HIV to join our technical discussions and to give us feedback because they know the challenges faced by people living with HIV,” said Phan Thi Thu Huong, VAAC Deputy Director in charge of HIV care and treatment.
The guidelines allow for multimonth antiretroviral therapy refills for all people on HIV treatment and for the provision of pre-exposure prophylaxis and tuberculosis medicines.
Provinces have been assigned focal points and hotline numbers for people who experience unusual symptoms.
More importantly, the standard referral requirements were eased in order to allow clients temporary access to alternative HIV clinics for antiretroviral therapy refills. VAAC also proactively resolved procurement challenges in order to avoid stock-outs, so Mr Nam and others could access HIV clinics of their choice for refills.
Viet Nam’s HIV epidemic is concentrated mostly among gay men and other men who have sex with men, transgender women, people who inject drugs and female sex workers and their intimate partners, with a rising HIV prevalence among gay men and other men who have sex with men .
“I believe that by joining hands, we can help all people get their refills so that no one misses their treatment because of COVID-19,” said Mr Phong.
Working hand in hand and getting results is what communities do best, according to Marie-Odile Emond, the UNAIDS Country Director for Viet Nam. “These networks are pillars of peer support and resilience and now more than ever they’re like an extended arm of the public health sector,” she said.
Resources
Region/country





Feature Story
Building peace through sustainable initiatives
16 April 2020
16 April 2020 16 April 2020“Peace is not merely the absence of war—it is when people have access to resources that enable them to meet their basic needs so they can live their life with dignity. If people have no nutritious food, if children do not go to school, if there is a conflict, then they are not at peace. COVID-19 came to remind us about it,” said Karambu Ringera, the founder and President of the International Peace Initiatives in Kenya.
Ms Ringera says that peace is holistic—even though her organization focuses on women living with HIV and AIDS-related orphans, she believes that it is also working for peace.
Her work started back in the early 2000s, when Ms Ringera was a student in the United States of America. When she returned to her home town in Kenya, Meru, for the summer holidays, she met a group of women, some of whom had recently lost their husbands. Most of the women didn’t know the cause of death of their husbands, but since AIDS-related deaths in Kenya were at their peak then, Ms Ringera suspected the reason. She encouraged the women to find out their own HIV status so as to not follow in their husbands’ footsteps.
Moved by the plight of many of the women she met, many of whom couldn’t afford to send their children to school or access HIV treatment, when back in the United States Ms Ringera arranged a cultural event, at which Kenyan food was served and people could learn about African culture. She collected US$ 400—enough to send seven children to school.
“I love the proverb about not just giving a person a fish, but teaching them how to fish,” she said. She wanted to help more children at home in Kenya, but, said Ms Ringera, “I wanted to go beyond just being someone who came to study poor women, create a solution for them and ask them to implement it.” For her, it was important for the women to understand that they could help themselves.
The women decided that they would make jewellery, which could be sold at her cultural fundraising events. At the same time, women started developing more skills, such as weaving and catering, so they could start their own businesses and support themselves.
Nearly two decades later, Ms Ringera runs a nongovernment organization that provides sustainable initiatives for orphans, women living with HIV, survivors of violence and communities with the tools and resources they need to move on from violence, poverty and crisis to stability and self-reliance.
In the beginning, many of the women who work at the International Peace Initiatives couldn’t afford a US$ 3 school uniform for their children. Today, Ms Ringera is proud that many have put their children through university. “People even in vulnerable circumstances can transform their lives. We have women and children, young people, to show that this is possible. We need to create interventions that inspire people to save themselves,” she said.
In the time of COVID-19, though, Ms Ringera is worried.
“We will need a good strategy to survive as a family,” she said. “Since 2009, when our children’s home was opened, this is the first time that we closed its doors to visitors. We did this immediately after hearing the news about the new coronavirus.”
The children’s home is home to 76 children, who need to be fed three times a day. Ms Ringera thinks that sustainability is key—Ms Ringera and her team are planting crops, keeping chickens and trying to collect a store of food for at least three months. “I feel that more and more, people need to create their own sustainable systems where they are, so that during challenges like this, at least they can have their own food locally,” she said.
Resources
Region/country
Related

Feature Story
When will men stop thinking that women’s bodies are their property?
09 April 2020
09 April 2020 09 April 2020Restrictions in movement, social isolation and increased socioeconomic pressures around the world have led to an increase in violence against women and girls since the start of the COVID-19 pandemic. As the United Nations Secretary-General António Guterres said, “Peace is not just the absence of war. Many women under lockdown for COVID-19 face violence where they should be safest: in their homes.”
Before the COVID-19 outbreak, at least one in three women and girls experienced physical and/or sexual violence, one of the most widespread human rights violations in the world. In areas with a high prevalence of HIV, intimate partner violence has been found to increase the risk of women acquiring HIV by 50%. Ending violence against women and girls must be a priority everywhere.
The United Nations has asked that governments dedicate funding in national COVID-19 response plans for domestic violence shelters, increased support for call-in lines, including text services, so reports of abuse can take place discreetly, online legal support and psychosocial services for women and girls. As UNAIDS knows well, these services are usually run by civil society organizations and community-led networks, which now need financial support more than ever. Finally, shelters should be designated as essential services and kept open, in the same way that pharmacies and food shops are.
When hundreds of millions of women and girls continue to be subjected to abuse and violence, it comes at a huge cost to themselves and to their families, communities, societies and economic development.
“We need to break this vicious cycle of violence, abuse and inequality,” said Winnie Byanyima, UNAIDS Executive Director, in a recent opinion piece. She added that there can be no impunity and survivors must be heard and justice must be done.
Video
Our work
Related

Feature Story
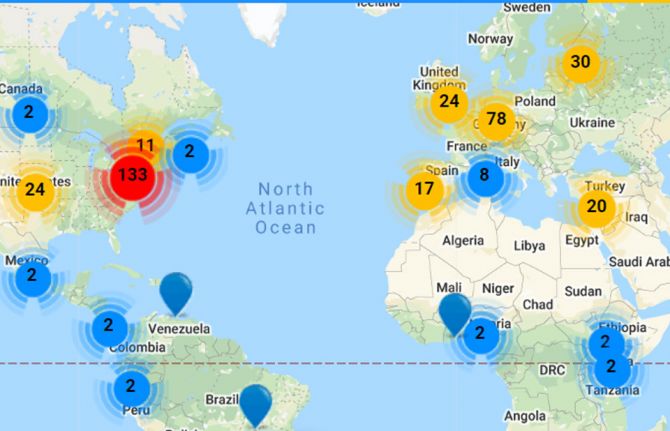
New innovations map to strengthen the response to COVID-19
08 April 2020
08 April 2020 08 April 2020A Coronavirus Innovation Map has been launched by StartupBlink together with the Health Innovation Exchange—a UNAIDS initiative to leverage the potential of innovations to improve the health of all—and the Moscow Agency of Innovations.
The map is a directory of hundreds of innovations and solutions globally that could support and strengthen the response to COVID-19, helping people to adapt to life during the COVID-19 pandemic and to connect innovators so they can collaborate on solutions.
The map provides information on five categories: prevention, diagnosis, treatment, information and life and business adaptation. As part of the prevention category, for example, the directory highlights the Track Virus app, which shows where the virus has spread in Israel, and a test kit to detect COVID-19 developed by E25Bio that will be able to deliver results in half an hour.
The directory also shows ways in which people can get medicines without leaving their home—telehealth and home medicine delivery solutions will be just as relevant for COVID-19 as for the AIDS response.
The information category shows how people can get timely and accurate information about the crisis and innovations, while the life and business adaptation category shows how people can adapt by doing things virtually—in only a short amount of time, schools and universities have switched to e-learning and home offices have replaced onsite offices.
The map is designed to provide information to government officials, venture capitalists, entrepreneurs and others to support the response to COVID-19 and address the pandemic and its impact.
“We are facing a challenge like never before and we need to work together to bring the best of ideas to beat the virus. The Coronavirus Innovation Map aims to provide a platform for innovators, every one of us, to collaborate and engage with the response,” said UNAIDS Director of the Office of Innovation, Pradeep Kakkattil.
“You can share ideas on the platform or reach out to innovators through the platform. We have seen a number of existing tools and innovations already being repurposed for COVID-19 with great success and believe that the platform will help bring new solutions faster into the hands of those at the forefront of the response,” added Eli David, CEO of StartupBlink
Over 500 innovations have already been received on the platform and the Health Innovation Exchange will produce a report on shortlisted innovations to be shared with country partners for the COVID-19 response.
Our work


Feature Story
A tribute to Maeve Kennedy Townsend McKean
09 April 2020
09 April 2020 09 April 2020In the 15 years since I went public with my diagnosis of HIV, it remains daunting to stand in front of a new audience and share my story. Though I expect them, I have never quite gotten used to the disbelief and shock I see in people’s eyes, the jaws gone slack, the overwhelming empathy. Because we have come such a long way in the journey against HIV, my story now is a happy one, meant to inspire people to know more, do more, support more so we can reach all those who still need access to prevention, testing, treatment. I do what I do because I hope others will feel more comfortable getting tested and treated for HIV if they see someone who has been healed, who is still embraced by their family, friends, colleagues and community.
And yet, while I have done it many times, and it’s a story with a positive bent, each time I share it publicly my heart pounds and my mouth runs dry. Early in my days of disclosure, a friend suggested I look for a smiling face in the crowd, someone who looked strong and positive, so I could absorb their energy and stay calm and upbeat even as I was full of fear.
Recently, the Atlantic invited me to a talk for World AIDS Day in Washington, DC, and I was particularly nervous. Having been at UNAIDS for nearly six years at the time, I was out of practice having my personal journey with HIV be the focus of my work. I knew a lot of people in the audience, professionally, but not personally. As I took the stage, I found myself shaking. I sat down, straightened the creases in my pants and scanned the room hoping for an encouraging looking face.
And then I saw Maeve. She smiled that radiant, confident smile that could say so many different things, as needed, in any moment. She seemed to understand that this was different, that it was personal, and that I was afraid. She nodded. And just like that, I was fine. I took a deep breath and told a room full of strangers and professional colleagues about what it’s like to live with HIV, to face the fear of death, the stigma, the treatment, the guilt that you have survived and others have not.
These last days, mourning her loss, I remembered a conversation I had with Maeve about the idea of survivor guilt. She pointed out that those of us who work daily to protect and extend the lives of others shouldn’t feel guilty, but rather, responsible—it was an idea that came from the AIDS community. I loved that idea. Survivor guilt became survivor responsibility to me because of Maeve.
Maeve’s amazing contributions to social justice, to global health, to policies that made people’s lives safer, longer, happier and healthier are multitudinous. A public health and human rights lawyer, Maeve’s deep commitment to immigrants, refugees, women and children, including issues of violence, and rights for lesbian, gay, bisexual, transgender and intersex people, was rarely matched. She inspired so many of us and served as a role model in myriad ways. Many words have been said about her contributions by many who knew her longer or better than I did. But perhaps because I knew her less well, and yet felt that she was there deeply, personally, profoundly for me when she could sense I needed it, several times, I can uniquely appreciate some of Maeve’s finest qualities. She had an almost extrasensory perception of what was needed, especially in delicate moments. She shared her strength, her courage, and in doing so, made difficult things seem possible, doable.
From Capitol Hill in the United States of America, where she worked for Senator Dianne Feinstein, to the Peace Corps in Mozambique, where she was a volunteer, to the United States Department of Health and Human Services and the United States President’s Emergency Plan for AIDS Relief, where she served in various roles for President Barack Obama, Maeve’s ability to advance social justice was remarkable. Her lifelong commitment to public service was infused with her effervescent spirit, her indefatigable energy and that famous smile, capable of lighting up a whole room and lifting your heart.
It is difficult to describe the loss one feels when someone like Maeve leaves us. The world hardly makes sense. Why would someone so talented, so helpful, so selfless, so beautiful in every sense be taken so early? It raises all kinds of existential questions. And creates a new type of survivor guilt in those of us who were not taken instead. But remembering that conversation I had with Maeve and, in her honour, instead of being sad, I will recommit myself to the work with an even deeper sense of responsibility to carry on, to continue to try to extend the kinds of elemental forces for good she so often instigated.
A granddaughter of the late Senator Robert F. Kennedy and grandniece of former President John F. Kennedy, Maeve embodied the best qualities of a global humanitarian. The effects of her efforts will be felt for generations to come. It will take many of us working together to fill the gaps left by Maeve. But she lives on through and in us. I know I, for one, whenever I think something is too hard, or too daunting, will conjure her smile, see her nod and simply get on with it, as I know she would do.
Maeve worked with many UNAIDS colleagues over the last decade and was a strong ally of the organization. UNAIDS deeply mourns her loss and the whole of its global staff extend our heartfelt condolences to her family.
Regan Hofmann, Director, a.i., United States Liaison Office, UNAIDS
Region/country
Related
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025











