





Feature Story
HIV testing and support for homeless people in Belarus
11 May 2020
11 May 2020 11 May 2020Homeless people have difficulty accessing health-care services at the best of times, but the COVID-19 pandemic has curtailed access even more. Stigma and discrimination and the conditions they live in make homeless people particularly vulnerable not only to COVID-19 but also tuberculosis, HIV, hepatitis and other diseases.
“Before the COVID-19 pandemic there were about 11 shelters in Minsk where people could get clean clothes, wash themselves, have food and stay for a night. Now only three of them remain open,” said Karina Radchenko, a volunteer from Street Medicine, the country's first volunteer network to treat the homeless. “We know that some of them are living with HIV, but because they don’t have proper identification and residence registration they can’t get free treatment. This is why we need to keep providing support to the homeless, especially now.”
Launched by Street Medicine, UNAIDS, the Positive Movement—a Minsk-based nongovernmental organization that provides HIV services—and the Ministry of Health of Belarus, a new initiative is providing HIV testing and support to the homeless during the COVID-19 pandemic.
Working on the streets, the volunteers distribute condoms, hygiene packs and over-the-counter medicines and provide HIV testing and counselling together with first aid, such as wound treatment and bandage application. The first phase of the initiative will see at least 200 homeless people in Minsk and beyond being tested for HIV and will collect information on their HIV prevention needs and the barriers they face in accessing HIV treatment and other health services.
“Homeless people very often don’t have identification, and this complicates a formal recognition of their HIV status and their access to HIV treatment,” said Vera Ilyenkova, the UNAIDS Country Manager for Belarus. “One of the goals of this initiative is to help people who test positive for HIV to get connected to health facilities so they can get treatment and proper documents from the authorities.”
Our work
Region/country
Related


Feature Story
Dealing with COVID-19 in Cameroon
11 May 2020
11 May 2020 11 May 2020Q&A with UNAIDS Country Director Savina Ammassari
Savina Ammassari has been the UNAIDS Country Director for Cameroon since 2018. Before that, she worked for UNAIDS in India, Myanmar and Cambodia as a Strategic Information Adviser. She has supported initiatives promoting sustainable development, equity and human rights in more than 20 countries.
Because she has lived and worked in so many countries and speaks many languages, she considers herself quick to adapt, but COVID-19 has definitely tested her.
Savina, did you feel like COVID-19 was a tsunami coming your way?
Yes, indeed, I saw the tsunami coming. I’d followed the COVID-19 outbreak in China, the rapidly unfolding epidemic in Italy, my home country, which already has claimed more than 24 000 lives. I was acutely aware that many countries in sub-Saharan Africa, including Cameroon, would be ill-prepared to address the devastating health and economic impacts of COVID-19, where fragile health systems and chronic poverty represent significant challenges for government, community and United Nations system responses to the pandemic.
The realities of the crisis enveloping the world were starkly brought home to me when my brother-in-law, working as a surgeon in Brescia, the epicentre of the Italian epidemic, developed severe COVID-19 symptoms, leading to bilateral pneumonia. Fortunately, he was ventilated and received experimental treatments. His life has been saved. But I know this will not be the case for everyone, especially in countries with weaker health-care systems.
Cameroon is now the COVID-19 epicentre in western and central Africa. The first cases were detected at the airport of the capital, Yaoundé. Additional cases were soon recorded in Douala, the largest city of the country. Despite early measures taken by the Government to isolate initial cases, testing and contact tracing, community transmission has taken hold. Limited access to testing services makes it difficult to know the extent of transmission.
The Cameroon response has faced significant constraints, not least the capacity to scale up testing and expand contact tracing and the provision of intensive care unit/ventilation support for the seriously ill, as well as adequate personal protective equipment for medical staff. The rapid implementation of community education programmes, emphasizing hand hygiene and social distancing, is an ongoing challenge, especially in poor, often overcrowded, urban areas.
How did Cameroon prepare? In Cameroon, there initially was a sense of optimism that, somehow, Africa, unlike other regions, would manage to avoid the catastrophic consequences of the pandemic. There was little awareness that Cameroon was most likely just a matter of a few weeks behind.
Today, Cameroon is the most affected country in the region and second in sub-Saharan Africa, with a quickly rising rate of infections. The scarcity of test kits obviously hides the real number of infections. Counting individual infections, recoveries and fatalities does not provide the real picture. UNAIDS advocated for a modelling of the epidemic in order to enable quantification of health-care needs and procurement.
As the first COVID-19 cases were detected in Yaoundé, a small number of health-sector officials gathered with the Minister of Health to discuss and plan epidemic containment and impact mitigation measures. I was one of the United Nations officials requested to be part of the group, given UNAIDS’ experience in epidemic management. I underscored the need to build on existing systems and make use of the community-driven efforts of the national AIDS response. I advocated for frontloading investments in communication and community mobilization to prevent COVID-19 infections, using a multisectoral approach.
The multisectoral response fell into place through the direct involvement of the United Nations Resident Coordinator (UNRC) with my support. I facilitated the UNRC’s efforts to connect the Minister of Health with development partners in weekly teleconference calls. Partners were ready to assist but lacked information on the most immediate needs.
UNAIDS has supported the Ministry of Health to model the COVID-19 epidemic to better understand and quantify needs. This has been done through teleconferencing, with the participation of various technical and financial partners. It has helped with the prioritization of needs and the quantification and costing of urgently required supplies and equipment. Partners were ready to support this effort, but required not only a modelled, costed national COVID-19 response plan but also a well-articulated procurement schedule based on the plan. UNAIDS has also successfully advocated for the establishment of a strategic information working group to analyse more in-depth data from surveillance, model the epidemic, and monitor and evaluate the COVID-19 response.
Communicating is indeed key. But how do you deal with things as basic as the lack of running water in many sub-Saharan African countries, making handwashing difficult. How are people coping with this and other measures, such as physical distancing?
This is indeed a major challenge in Cameroon as there is a lack of consistent water supply in many urban and rural communities. The use of hand sanitizers is not an affordable option for most people and locally produced product is not necessarily quality assured and safe for use.
Similarly, physical distancing and self-isolation are remote, often unrealistic options for communities where large numbers of people, as a rule, share common spaces in their home and community environments. The government has put in place a series of strict measures to contain the spread of COVID-19 (closing schools and educational or training institutions, banning gatherings of all kinds, imposing the use of face masks on public transport), although a comprehensive lockdown has not been promulgated to date. There are legitimate concerns on how a full lockdown could affect the majority of people, as more than 80% of the population work in the informal sector and live hand-to-mouth. Yet, from a public health perspective, lockdowns are a must. Balancing concerns is a major challenge.
Savina, you have never shied away from challenges. Would you say this is the biggest challenge you have faced, and why?
Yes, this crisis is unprecedented, unpredictable. I’m concerned at how the COVID-19 pandemic will affect not only our staff and their dependents but also people living with HIV, who need to continue accessing antiretroviral therapy and services, and people who are already stigmatized, vulnerable and socially and economically marginalized.
We have already witnessed a worrisome rise in stigma and discrimination against members of key populations in Cameroon and are making sure that the UNCT and partners keep human rights issues high on the agenda.
Our work is already challenging in normal times as Cameroon is facing enormous development and humanitarian hurdles. Already, Cameroon’s humanitarian crises on three fronts are not getting enough international attention. It’s the least funded humanitarian crisis worldwide. The COVID-19 epidemic multiplies these challenges several times over.
UNAIDS is mobilizing communities and networks in COVID-19 prevention work and making sure that civil society is adequately consulted and involved in the national response to the new virus.
How do you unwind in the evening? How do you recharge your batteries?
I’m afraid I don’t give enough time to relaxing, as I work around the clock, which isn’t good. Perhaps one of the challenges of COVID-19 is to take up new interests outside of work, that can be sustained and enjoyable well into the future.
What are the lessons learned? Will you do things differently from now on?
I’ve learned once again that unity makes force. In unpreceded emergencies like the current one, where no one has the answer or a magic bullet, everyone’s competence and experience is needed. Connecting people, bringing in resources, getting a transparent exchange—all this is paying off. It requires strong leadership and a cohesive team effort.
Our work
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025



Feature Story
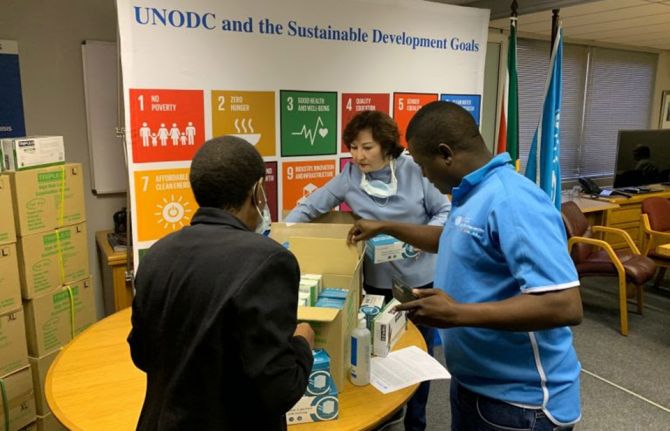
United Nations agencies coordinate their COVID-19 response in South Africa
12 May 2020
12 May 2020 12 May 2020United Nations entities in South Africa, including UNAIDS, are working closely together to support government and community responses to the COVID-19 pandemic. The United Nations in South Africa has jointly engaged with civil society, the private sector and key affected communities, including people living with HIV and tuberculosis, to rapidly respond to the impact of a national lockdown that commenced on 26 March.
Using the World Health Organization eight-pillar approach, the United Nations in South Africa has developed a multisectoral plan centred on the immediate health and other needs of people, including access to medicines, HIV prevention and testing services, food security, education, social protection and community resilience.
On 30 April, the United Nations in South Africa launched an emergency flash appeal for US$ 136 million to support close to 10 million people in need. The appeal will help fund the civil society response and ensure that the needs of key populations and vulnerable communities are met in the response to COVID-19, including continued health support to people living with HIV, migrants and refugees, women and children affected by violence and communities facing shortages of food and other essentials.
UNAIDS has worked with partners to coordinate the United Nations in South Africa plan, providing support to strategic information, community engagement and communication. Funds already available to the United Nations Joint Team on HIV/AIDS are being reprogrammed to ensure that civil society, people living with HIV, key populations and vulnerable communities continue to be supported in the AIDS response while also addressing new challenges from COVID-19.
United Nations staff, including UNAIDS staff based in provinces with a high HIV burden, are working in the national and provincial COVID-19 command centres and supporting community health workers actively engaged in screening, contact tracing and voluntary testing. South Africa has massively scaled up screening for COVID-19.
Supporting community innovation
The United Nations has actively engaged with civil society organizations through sector networks, some of which have been established to coordinate responses to the pandemic, such as the C19 People’s Coalition and the COVID-19 Front, and long-standing networks, including the South African National AIDS Council (SANAC) Civil Society Forum and the National Economic Development Council Community Constituency. Their plans include a strong emphasis on advocacy, communication and social mobilization around issues such as medical care, shortages of food and fresh water, crowded housing conditions, homelessness and loss of income. The United Nations Country Team is providing technical support to civil society and resource mobilization through its emergency flash appeal.
UNAIDS has also supported organizations representing people living with HIV to survey and document the needs and challenges of people living with HIV in accessing essential health and social services, antiretroviral therapy and safety and hygiene services committed by the government. The survey results will inform a dialogue led by people living with HIV to find joint solutions.
Working with the government and other partners
Under the leadership of the United Nations Resident Coordinator in South Africa, Nardos Bekele-Thomas, the United Nations in South Africa is fully supporting the all-government, all-society COVID-19 response led by the National Command Council, chaired by the President, with a cutting-edge Ministerial Advisory Council that provides the science and evidence for decision-making.
The United Nations has jointly consulted the government, including the Department of Health and the Department of Social Development, to explore response needs, including support to the National Solidary Fund set up by the President for resource mobilization. The United Nations also briefed the diplomatic corps, the business sector, private foundations and philanthropies on how the United Nations is responding to support the government, civil society and communities. Consultations were also held with the World Bank, which is currently developing a post COVID-19 strategy and possible support to the national response.
The UNAIDS Country Director for South Africa, Mbulawa Mugabe, emphasized the importance of using lessons from the AIDS epidemic to put people at the centre of the COVID-19 response and encourage communities to identify issues and develop solutions. “We need to make sure that we act with purpose and speed,” he said. “Communities have mobilized themselves and are determined that people who need services have access to them. We remain concerned that COVID-19 may impact differently on the 5 million people in South Africa who are living with HIV and on treatment and the 2.5 million people who are not currently receiving antiretroviral therapy. It is important to protect the progress in the AIDS response to date and continue achieving the HIV prevention and treatment targets for 2020.”
The Joint Team on HIV/AIDS in South Africa is working with the Department of Health, primary recipients of the Global Fund to Fight AIDS, Tuberculosis and Malaria and the United States President’s Emergency Plan for AIDS Relief in an effort to safeguard access to HIV services and promote multimonth dispensing of antiretroviral therapy.
UNAIDS is working with the United Nations Office on Drugs and Crime, the Department of Social Development, SANAC and other partners to address disruptions for homeless people, including those who use drugs, so they can access essential services, including antiretroviral therapy, replacement needles and syringes and methadone, even after they were relocated to emergency shelters. The Office of the United Nations High Commissioner for Human Right is monitoring the impact of the lockdown regulations and enforcement procedures on marginalized people and key populations and is advocating to end stigma and prevent punitive measures. The social protection cluster in the United Nations team is working with government and civil society to address humanitarian challenges.
The World Health Organization and UNAIDS are working with the Department of Health and SANAC to develop communication materials directed at communities, including podcasts to be made available through WhatsApp and community radio stations.
Our work
Region/country


Feature Story
Combatting COVID-19 discrimination in Jamaica
08 May 2020
08 May 2020 08 May 2020Some Jamaicans have responded to the COVID-19 outbreak in extreme ways. Family members of one of the first confirmed cases received death threats, and nurses have reported being barred from public transport. Some people have given the health authorities wrong addresses to avoid the stigma that a home visit would attract.
UNAIDS Jamaica and civil society organizations serving people living with HIV have joined the national discourse to share a key lesson learned from HIV: that stigma and discrimination are barriers to an effective response.
Two-thirds of Jamaicans would not purchase vegetables from someone they knew to be living with HIV, according to the 2017 Knowledge Attitude and Behaviour Study. The effect of such widespread prejudice is seen in the island’s treatment outcomes. According to government estimates, while an estimated 84% of people living with HIV were aware of their status in 2018, less than half (47%) were on treatment
For Jumoke Patrick, Executive Director of the Jamaica Network of Seropositives, there are clear parallels between people’s reactions to the novel coronavirus and HIV.
“People living with HIV feel they need to stay away from people and from accessing services. They feel they need to reduce and limit their lives because of how people treat them. We have some of the same treatment meted out to people positive with, or suspected of having, coronavirus. When there’s fear we respond in a defensive way,” Mr Patrick explained in a webinar hosted by UNAIDS Jamaica.
Community organizations have reported that some COVID-19 stigma has even been directed to people living with HIV. UNAIDS Jamaica has been working to raise awareness among policymakers and through the news media about the importance of building trust with affected people while combatting stigma and discrimination among the wider population.
“Just as with HIV, success in combatting COVID-19 absolutely depends on people’s willingness to get tested and access care. Verbal abuse, violence and intimidation will only chase people away from services,” said Manoela Manova, UNAIDS Country Director for Jamaica.
The Jamaica Ministry of Health has launched an antidiscrimination campaign that includes stories of harassed COVID-19 patients in virtual press conferences.
“None of us are immune to the virus,” Christopher Tufton, the Jamaican Minister of Health, said at a recent press conference. “None of us must claim or think that we will exclusively escape and it is somebody else’s fault. We must treat each other in a way that almost assumes that tomorrow we are going to need the support from those who are so infected and impacted today. We really need to cut the hate and work together as a country and as communities, to overcome.”
Our work
Region/country


Feature Story
United Nations in South Africa launches US$ 136 million COVID-19 flash appeal
07 May 2020
07 May 2020 07 May 2020The United Nations agencies in South Africa have launched a joint flash appeal to support 9.9 million people to cope with the COVID-19 response.
The United Nations Country Team in South Africa, under the leadership of the Resident Coordinator, was joined for the launch of the appeal on 30 April by government ministers and others.
The Emergency Appeal on the Impact of COVID-19 in South Africa calls for US$ 136 million to support government efforts to reach vulnerable and marginalized communities to address the impact of COVID-19. It aims to raise funds for health, including HIV/tuberculosis, food security and nutrition, gender-based violence protection and response, education, water and sanitation, coordination and governance.
The United Nations Resident Coordinator, Nardos Bekele-Thomas, said, “Helping South Africa especially at this time makes development sense and it also makes business sense. We focus on the most vulnerable groups. They have potential to be producers and, with disposable income, they will become consumers, investors and productive assets for the economy,” she said.
The Minister of Health, Zwele Mkhize, welcomed the United Nations plan, which will complement national efforts and focus on the needs of vulnerable communities, including people living with HIV and tuberculosis, migrants and refugees, vulnerable women and children, key populations and millions affected by poverty, unemployment and the impact of national restrictions on trade and movement since 26 March. “We have various issues of inequality, unemployment, poverty and densely populated areas and chronic overcrowding in our metros, which are the most affected by COVID-19. We have already started to see local transmissions in these areas, which has given us cause for concern,” he said.
Mr Mkhize said the appeal would also help to ensure that the AIDS response continues unabated, including scaling up testing and treatment for people living with HIV. “We had already started a programme to achieve our 90–90–90 goals in 14 of the 52 districts and we cannot allow this pandemic to disrupt all these efforts and the successes and achievements we have already scored,” he said. “We appreciate the focus on people living with HIV, given the burden of disease.”
The Minister of Health told the launch that it was important to work with communities, civil society and other stakeholders already in place. The COVID-19 response would strengthen South Africa’s resolve to achieve universal health coverage, he said.
Our work
Region/country




Feature Story
Mitigating the impact of the COVID-19 pandemic among people living with HIV in India
06 May 2020
06 May 2020 06 May 2020For the more than 3000 people, including 330 children and adolescents, living with HIV and on antiretroviral therapy in Goa, India, the COVID-19 outbreak is a time of worry—they are worried about COVID-19 and they are worried about being able to stay on their HIV treatment during the lockdown in India.
In order to respond to one of those worries, the team at the Human Touch Foundation, a community-based organization that provides care and support to children and adolescents living with HIV, has, since the start of the lockdown, organized a force of volunteers to deliver antiretroviral therapy to people’s doorsteps.
Health officials at the HIV clinics provide a list of people who need deliveries of antiretroviral therapy, after making sure that the beneficiaries consent. Alternatively, several beneficiaries connect with the Human Touch Foundation directly for a supply of medicine.
“Most people living with HIV are still hiding their HIV status and do not wish that we come directly to their homes for the delivery. With poor mobile connectivity, in many cases we have no option rather than make more than two trips, instead of asking their location with the villagers,” said Peter Borges, the founder and Chief Executive Officer of the Human Touch Foundation.
Along with antiretroviral therapy, the Human Touch Foundation also provides essential groceries—rice, lentils, grams, oil and milk—for children and adolescents living with HIV and their families. “Many children and adolescents are with anxiety and depression, mostly concerning their survival, due to loss of income of their families and scarcity of essential supplies,” said Mr Borges. Bars of soaps are also provided with the packages, distributed in collaboration with UNAIDS, Reckitt Benckiser, the Just Imagine Trust and the Rotary Club of Panaji Riviera.
The Human Touch Foundation is also offering online psychosocial support to children and adolescents living with HIV. “We have streamlined our communication through telecounselling and support. We have a staff team giving coordinating and rendering support to the field team through assessment of the family,” Mr Borges added.
Similar efforts are being undertaken in Bangalore to support people living with HIV. Champion in Me, a community-based organization that provides care, support and skills to adolescents and young people living with HIV, has built a support system to reach out to communities during the lockdown. A force of young volunteers has partnered with the Karnataka Network of Positive People to distribute medicines to 140 people and food provisions to 1200 people. “I praise the courage of our volunteers and supporters that came out to help people living with HIV, in a time of crisis. This is when our organizations and leaders have to stand tall and join efforts to make sure nobody is left behind,” said Elvis Joseph, the Director of Champion in Me.
At the national level, the National Coalition of People Living with HIV in India (NCPI+) is coordinating efforts with the National AIDS Control Organisation (NACO) and other partners, including UNAIDS, to ensure adherence to treatment and a continuum of care for people living with HIV.
“Since the lockdown started, the National Coalition of People Living with HIV in India established a good communication platform through WhatsApp and emails connecting the National AIDS Control Organisation and networks of people living with HIV to closely monitor challenges, find joint solutions and help coordination,” said Daxa Patel, the President of NCPI+ and the Secretary of the Gujarat State Network of People Living with HIV. As a result, NCPI+ has helped more than 45 000 people living with HIV in India to get home deliveries of antiretroviral therapy.
“HIV-affected communities have played an important role delivering antiretroviral therapy to people who were not able to collect it themselves. The Human Touch Foundation, Champion in Me and the National Coalition of People Living with HIV in India are just some examples of what can be done at the national, state or city level by communities themselves. Many local solutions have been put in place in a joint effort between the government, UNAIDS and community-based organizations to get medicines, food or soap delivered to those in need,” said Bilali Camara, the UNAIDS Country Director in India.
Our work
Region/country


Feature Story
Paying tribute to care workers during an online Labour Day event
01 May 2020
01 May 2020 01 May 2020On 1 May 2020, the UNAIDS Executive Director Winnie Byanyima joined Oxfam Denmark to pay tribute to care workers during an online Labour Day event. Below are the transcripts of her video message.
Hello everyone!
It’s an honour to join you to celebrate 1 May—the international day of workers. In the time of COVID-19, it is our frontline workers in hospitals, community health centres, care facilities, supermarkets, taxis and delivery vans who are risking their lives for us.
Here in Geneva we clap for health workers and carers every evening at 9 p.m. to show our gratitude.
But this is not enough. We must value and fairly reward the work they do.
Women make up 70% of frontline health and care workers. Twenty-four million out of the 28.5 million nurses in the world are women, and they earn on average 28% less than their male counterparts. They are low paid and receive poor benefits. In developing countries, community health workers, mostly women, play a critical role in disease prevention, promoting healthy behaviours and linking community members to formal health centres. Community health workers are often women volunteers, getting no compensation from public health systems. What a gender injustice!
And guess what? The coronavirus is aggravating this injustice. It has been heartbreaking to watch TV images of nurses and doctors who died because they did not have personal protective equipment. We must protect our health workers and ask our governments to prioritize their safety.
Then there is unpaid care work, done mostly by poor women and girls in their households—raising children, feeding families, caring for the sick and the elderly and so on—work estimated to cost about US$ 11.5 trillion globally. The burden of unpaid care work denies women and girls education and economic opportunities, it undermines their well-being and other roles in society and, again, the coronavirus is making this worse. An African woman, who already walked on average 6 km a day to fetch water, now needs to fetch even more because of the virus.
So, as we fight this deadly virus, I say, let us tackle the old gender inequalities that are feeding on and aggravating it. Let us demand fair and equal pay for health and care workers, let us demand that they have the personal protective equipment they need. They are our heroes.
Let’s end exploitation of women by calling for the recognition, redistribution and reward of unpaid care work.
Workers of the world, let’s give value to what truly matters in life, and celebrate and justly reward all care workers.
Thank you!
Watch video message
Resources
Related




Feature Story
“The concern did not just come from the community, but also the health workers”
01 May 2020
01 May 2020 01 May 2020After the 2018 earthquake struck Lombok, in West Nusa Tenggara, Indonesia, the destruction it caused closed most health facilities. Among those affected were people living with HIV, who could no longer access their HIV treatment. Then, Yayasan InSET, a civil society organization in the province, stepped in, teaming up with health facilities in the area and taking on the role of delivering antiretroviral therapy to people in need. Today, the COVID-19 pandemic is threatening to do what the earthquake did to access to HIV treatment, and Yayasan InSET is ready to step in again.
Many people living with HIV in West Nusa Tenggara and in the rest of the country are acutely concerned about the possibility of disruption to HIV services and not being able to access antiretroviral therapy, owing to overburdened health facilities or the possibility of lockdowns. A recent rapid survey of 1000 people living with HIV conducted by the Positive Indonesia Network found that more than 41% were extremely anxious about COVID-19, with more than 36% worrying about their ability to obtain their HIV treatment.
“In West Nusa Tenggara, there are more than 500 people living with HIV on treatment who are worried about being unable to go to a clinic to access antiretroviral therapy,” said Himawan Afrian, the head of Yayasan InSET.
Yayasan InSET’s experience of working with hospitals and health centres after the earthquake has left it ready to help out in the COVID-19 outbreak. “Some health facilities actually contacted us a couple of weeks ago to ask for our help. The concern did not just come from the community, but also the health workers. Initially they asked us to raise awareness about COVID-19 prevention to our communities. Now we are working out the arrangements for us to take over the delivery of antiretroviral therapy should the situation worsen,” said Mr Afrian.
Having a close collaboration with the health services has been a big help for Yayasan InSET ensuring that people living with HIV are not left behind during the COVID-19 pandemic. Its direct advocacy has ensured that people living with HIV in the province receive a two-month supply of antiretroviral therapy. The organization has also successfully lobbied the authorities to move the HIV clinic away from the hospital, so people can swiftly pick up their medicines without entering the overcrowded clinics in the hospital, and has successfully advocated to the authorities in Mataram for the provision of food packages for sex workers and people living with HIV for six months.
During emergencies, whether pandemics or earthquakes, collaboration and local solutions are key to ensuring that there is as little disruption as possible to services for people living with HIV.
Resources
Region/country


Feature Story
“I’ve saved lives on the frontline of the COVID-19 pandemic in China”
28 April 2020
28 April 2020 28 April 2020The winter of 2019/2020 in Wuhan, China, will remain with Xiao Yang for the rest of his life. During 60 days working in a makeshift hospital as an emergency nurse, he saw life and death, happiness and sorrow, tears and laughter.
Mr Xiao volunteered to go to Wuhan from his home town, Beijing, to save lives. “Saving life is the responsibility of every medical worker,” he said. This commitment is deeply rooted in his family—17 years ago, his father worked as a doctor on the frontline of the SARS epidemic.
Mr Xiao didn’t tell his boyfriend he was going to Wuhan until the last minute. “He didn’t want me to go, but he respected my decision,” he said.
On the night of their arrival in Wuhan, the volunteers were divided into two groups—intensive care and mild cases.
Mr Xiao was assigned to intensive care. For his protection, he was required to wear five gloves and two masks. However, most of the gloves were too small for him—wearing them for more than 20 minutes hurt. He also found it difficult to breathe. “It felt like someone was covering my mouth all the time,” he said.
Even worse for Mr Xiao is that he is asthmatic. If an asthma attack struck, he wouldn't have time to reach his medicine because of all the protective equipment he was wearing.
“All of us medical workers recorded final words for our families on our phones,” he said.
His boyfriend, Lin Feng, is a policeman. He too has become a lot busier because of the COVID-19 pandemic. When COVID-19 first broke out in Beijing, he was on duty for long hours, inspecting the freeways, streets and residential areas.
When the couple were far apart, instant messaging was the only way to communicate. Covered in snow after finishing his night shift, he received a text message from Mr Xiao reminding him to put on thicker clothes. His reply: “You take care of your patients. I’ll take care of you.”
Six days after his arrival in Wuhan, Mr Xiao realized that death could be near.
As he made his way around the ward, he saw a patient suffering from a drastic drop of blood oxygen level and shortness of breath. He rushed to intubate him—the quickest and most effective way to keep him alive. But he acted too forcefully, his protective suit tearing at his back—a colleague taped up the hole so he could continue to work.
After the patient was stabilized, Mr Xiao could hardly breathe and he felt sharp pains in his hands, ears and face—he had worn masks, gloves and his protective suit for too long. When the pain subsided, fear came over him. That leak could easily have seen him become infected with the new coronavirus. The leak also reminded him of the risks he was facing every day. “I can only pray I will be fine,” he said. “I was prepared for the worst when I decided to come here.”
There are many people from the lesbian, gay, bisexual, transgender and intersex community, like Mr Xiao and Mr Lin, who worked hard to contain the virus and save lives during the pandemic. In the Wuhan Lesbian, Gay, Bisexual and Transgender Center, 26 volunteers worked around the clock to deliver medicine to people living with HIV. UNAIDS was proud to support their efforts by connecting the centre with local health authorities to facilitate the delivery of medicine, helping with the delivery of medicine for Chinese people living with HIV overseas and supporting the establishment of a hotline providing counselling services for people living with HIV. As a result, the centre was able to deliver medicine to more than 2600 people, and the hotline reached about 5500 people.
“It was planned that I would stay for one week, but then it was extended to three weeks and then longer,” Mr Xiao said, choking back his tears.
He finally left in early April, when the COVID-19 pandemic subsided in the city. He said he will remember everything, but he doesn’t want to relive it. Nobody should.
Now safely back with his boyfriend in Beijing, he remembered the captain’s words on his flight to Wuhan, “The flight is from Beijing to Beijing, with a stopover in Wuhan. When you have won the battle, we will take you back home.”
Resources
Region/country




Feature Story
Helping people living with HIV with food supplies in Kyrgyzstan
27 April 2020
27 April 2020 27 April 2020Like most other countries, COVID-19 has not bypassed Kyrgyzstan—cases have been seen in the capital, Bishkek, and in almost all other major cities and provinces in the country.
In order to respond to the pandemic, a state of emergency was introduced on 25 March in Bishkek, Osh, Jalal-Abad and three districts, which restricts people to their home from 20:00 to 07:00 and allows people to leave their residence during the day only for a few specified reasons.
Like everyone else, people living with HIV in the country—UNAIDS estimates that there are 8500 people living with HIV in Kyrgyzstan—have faced a variety of challenges, including loss of earnings and difficulties in feeding their families.
In the small town of Karabalta, in the north of Kyrgyzstan, the HIV community organizations Believe in Yourself and the Country Network of Women Living with HIV work to promote the rights of people living with HIV. In the time of COVID-19, however, their services are even more in need.
Umid Shukurov, the Director of Believe in Yourself, explained that since the lockdown in Kyrgyzstan was announced, people living with HIV have got in contact with the organization in greater numbers. Access to food is a major concern for many. “Many people call us in despair, women cry and ask for help. Of course, we help in every way possible, but our resources are limited. When we, together with the Country Network of Women Living with HIV, compiled a list, we realized that 12 women living in our small town are in a distressed situation. Some of them have recently become mothers or are raising their children alone. Yesterday, we distributed food packages and some women could not believe that someone had reached them and brought them some food. The asked me, “Is it real that someone has heard us?”’’
Baktygul Shukurova, the Director of the Country Network of Women Living with HIV, knew that the network would face various problems after it was set up, but never thought that the problems would be of this magnitude. “Our task is to keep people on antiretroviral therapy. I have been through difficult situations in life myself and I know how difficult it can be when you simply have nothing to feed your children with. Only a person who has been through all this can understand the needs of communities. When you and your children have nothing to eat, you don’t care about the medication.”
Access to antiretroviral therapy is being ensured in the country by the provision of mulitimonth dispensing of medicines. During the COVID-19 pandemic, the national AIDS centre in Kyrgyzstan will be providing three-month supplies of antiretroviral therapy to all people living with HIV who are on treatment.
The UNAIDS Country Office in Kyrgyzstan, with the support of a Russian technical assistance programme, is organizing the delivery of food packages, which will supplement other social assistance available for people living with HIV, to 130 families of people living with HIV who have been the most affected by their loss of earnings. Apart from the food, the packages also contain colouring books, marker pens and watercolour sets for the children of people living with HIV, to help them get through the lockdown.
“We hope that this small help will go some way to enabling people living with HIV to remain on treatment,” said Meerim Sarybaeva, the UNAIDS Country Manager for Kyrgyzstan.
Our work
Region/country
Related
 Women, HIV, and war: a triple burden
Women, HIV, and war: a triple burden

12 September 2025
 Displacement and HIV: doubly vulnerable in Ukraine
Displacement and HIV: doubly vulnerable in Ukraine

11 August 2025
















