



Feature Story
Key population-led organizations delivering health services in Bangkok
27 January 2020
27 January 2020 27 January 2020Boy Somjai and Jam Chainukul (not their real names) are a young same-sex couple from Bangkok, Thailand. At the start of their relationship, they decided to take HIV tests for the first time. Looking for information online, their friends suggested the Rainbow Sky Association of Thailand (RSAT), a community-based HIV clinic located off a busy street in Bangkok.
RSAT, with four clinics and 10 drop-in centres in different cities across Thailand, serves as a one-stop service where gay men and other men who have sex with men and transgender people can access HIV prevention services and take part in HIV-related information sessions, with flexible service hours suitable for the lifestyles of many people from key populations.
Danai Linjongrat, the Executive Director of RSAT, said, “Access to HIV services for key populations is among the biggest challenges to the HIV response in the country. It is extremely important that key populations can access HIV prevention and treatment services without fear of discrimination.”
Mr Boy and Mr Jam, who now return to RSAT every three months for regular check-ups, said, “When we first visited the clinic, we were really nervous, as we were looking for a place that respects our confidentiality. Here we found more than an HIV clinic—we found a place we can trust, like a family. The health staff made us feel comfortable to share our story; they did not judge us and they understood our needs with an open mind.”
The success of RSAT is credited in part to its health workers being members of the populations they serve. RSAT has adopted the country’s key population-led health services model, in which people from key populations identify and meet the HIV and other health-related needs of their peers. “We understand the needs of our clients, what they want, where they live and how they feel, because our staff members are people from the communities,” says Mr Linjongrat.
Community health workers provide needs-based and client-centred services, including pre-exposure prophylaxis (PrEP), legal consultations, harm reduction, screening for sexually transmitted infections, counselling and hormone level check-ups for transgender people. Depending on the outcome of a person’s HIV test, they are offered a referral for antiretroviral therapy or an in-depth discussion about taking PrEP, all in a non-judgemental and supportive atmosphere.
RSAT is one of seven community-based organizations in Thailand that provide PrEP services free of charge through lay providers under the Princess PrEP Project. Currently, 1200 people are accessing PrEP through RSAT clinics and drop-in centres. The Thai Red Cross AIDS Research Centre, with the support of the United States President’s Emergency Plan for AIDS Relief through the LINKAGES Thailand project, implements continuous capacity-building to ensure that community health workers can provide HIV services in accordance with national standards.
RSAT uses different ways to generate demand for and promote its programmes and to carry out outreach work. Phubet Panpet, Deputy Director at RSAT, said, “Depending on our target audience, we go to different places, such as saunas, entertainment complexes, schools and universities, to raise awareness about HIV prevention and encourage people to get tested for HIV.”
Kunpawee Isalam, a staff member of the outreach team in Bangkok, is a transgender person who understands the stigma and discrimination faced by the transgender community. “We plan outreach activities that we know transgender people will be interested in, with the aim of increasing their self-confidence. For many, it is so hard to feel they can get support, and they fear discrimination. RSAT provides a safe space and HIV prevention options,” she said.
RSAT uses social networking sites to reach out to young gay men and other men who have sex with men. Staff members register as users and create profiles on dating applications to share HIV-related information. “At the beginning of the conversation, the outreach worker explains about the clinic and engages people in a conversation related to HIV prevention,” said Mongkol Jaidee, a field officer. “I choose the location, see who is connected, and send them personal messages to introduce the services provided by the clinic. I normally receive positive feedback, and it is common for people to come back later with questions and visit us in the following days.”
Mr Linjongrat concluded, “We differ from other services by caring for people by looking into what they need and what we can do to help them. Community-led services are a proven strategy and an essential feature of the HIV response in Thailand.”
RELATED INFORMATION
Region/country


Feature Story
Empowering young people living with HIV to become agents of change in Thailand
23 January 2020
23 January 2020 23 January 2020There are approximately 24 000 young people aged 15–24 years living with HIV in Thailand. In 2018, young people accounted for nearly half of the 6400 new HIV infections in the country.
Thailand has made great strides in its AIDS response, providing antiretroviral therapy free of charge as part of its universal health coverage scheme. However, adolescents and young people living with HIV often fall out of care or do not receive the support they need to remain on treatment. Self-stigma, stigma and discrimination and transition from paediatric care to adult care are some of the challenges faced by adolescents and young people living with HIV.
To close this gap, three years ago the United Nations Children’s Fund (UNICEF) and other national partners led by the Thai Network of People Living with HIV created the Thai Network of Youth Living with HIV. The main objective was to empower adolescents and young people living with HIV to be agents of the change that they wanted to see in their lives. The network’s capacity was built to provide referral services, life-skills training and peer-to-peer support for adolescents and young people living with HIV.
Kritthanan Ditthabanjong, one of the first active members, is now Head of Corporate Communication at the network. Studying to become a journalist, he also works as a content editor for websites and magazines in Thailand and is a well-recognized young leader. Mr Ditthabanjong represents the network at public events and in the media, voicing the needs of young people living with HIV.
“I have publicly disclosed my HIV-positive status because I want other people to learn from my experiences and to give young people the information they need to lead healthy and dignified lives. I feel confident to speak out because I have support from my friends and community,” he said.
With technical and financial support from UNICEF and other partners, and through a variety of platforms and strategies, the network offers emotional support around receiving an HIV-positive diagnosis, provides HIV information to reduce self-stigma, builds coping skills and creates a supporting network to tackle stigma and discrimination. “Young people living with HIV need emotional support and a community they can trust,” said Mr Ditthabanjong.
Trained young leaders with the network provide counselling for young people living with HIV and link them to health facilities, hospitals and community-led services for HIV treatment and care. The young leaders also accompany young people living with HIV to medical appointments and carry out follow-up home visits to help them adhere to treatment.
The network uses social media to reach out to young people, providing information on HIV and promoting self-acceptance. Initiatives such as the online campaign Growing Up with HIV offer safe spaces that enable young people to ask questions about different topics, including HIV prevention and safe sex, and share opinions and thoughts.
“Growing Up with HIV allows young people to be part of our community and make them feel they are not alone,” continues Mr Ditthabanjong.
Mr Ditthabanjong engages in other campaigns and social media initiatives with UNICEF that address young people in general in Thailand but also allow him to bring in the voices and perspectives of young people living with HIV. He has recently joined Dare to Dream, a public campaign created by UNICEF for Thai young people to voice their opinions on education and what is required to prepare them for the transition to adulthood. “From a shy adolescent who did not wish to speak and constantly glanced at his counsellor for approval a few years ago, Mr Ditthabanjong followed a path with us and he was one of nine motivational speakers at the Dare to Dream youth campaign, a role model for young people in his country,” said a UNICEF staff member.
Mr Ditthabanjong concludes, “One day I had an interview on social media. As soon as I came off, I received a text from a young person who had recently been diagnosed with HIV. “My mum and dad do not accept me, and I want to kill myself,” he said. I phoned him, met him and convinced him to join our network. Now this person is doing well. Our work is impacting people’s lives.”
Related information
Region/country




Feature Story
Supporting communities to be involved in the AIDS response in Thailand
20 January 2020
20 January 2020 20 January 2020The UNAIDS Country Office in Thailand, with a small team of three staff members, is located in Bangkok. Orawan Bettenhausen, the Administrative Assistant, has been part of the team for almost 20 years. “Being part of the UNAIDS family has empowered and transformed me into who I am today. I have been very fortunate to have had country directors who have coached me, and great colleagues and peers, both within and outside of UNAIDS, who have assisted, supported and inspired me,” she said.
Ms Bettenhausen recalls meeting a person living with HIV, a representative of the Thai Network of People Living with HIV, in her first weeks with UNAIDS. “I asked him about his life. When he finished talking, I was in tears,” she said. “To my surprise, he told me that neither he nor any other person living with HIV would want me to feel sorry for them. They just wanted to be accepted for who they are. He taught me a huge lesson, and I made a commitment to work for people living with and affected by HIV.”
Throughout the years, she has assisted the Country Director and the team to get communities, civil society organizations and people living with HIV meaningfully involved and engaged in the AIDS response. “As the Administrative Assistant , I do feel that I support our community partners in different ways, such as contributing to the execution of joint projects, facilitating logistic support to make sure communities can attend regional and national events and providing interpretation from Thai to English and vice versa. I feel I am giving community members the opportunity to overcome language barriers, to be present in decision-making spaces to voice their needs and showcase their work outside Thailand,” she explained.
Ms Bettenhausen has witnessed important changes in the AIDS response in Thailand. For example, she remembers UNAIDS implementing projects in collaboration with civil society organizations and facilitating dialogues between policymakers, HIV programme implementers and community representatives at a time when stigma and discrimination against people living with HIV and key populations was a major concern in the country.
Since 2015, Thailand has implemented the 3-by-4 Package for Stigma-Free Health Facilities, with comprehensive programmes to address and remove barriers to accessing health services. In 2019, the country announced the Thailand Partnership for Zero Discrimination, which goes beyond health settings and includes areas such as workplaces and the education system. UNAIDS has been involved since the outset of the initiative by providing technical assistance to formulate the zero discrimination strategy, to develop a monitoring and evaluation plan and to operationalize the strategy in a joint effort with the Thai Government and civil society.
“My contribution to this achievement was to provide continuous support to the Country Director, who played a critical role in linking stakeholders from different sectors and bringing them together, making sure that communities were always involved and enabled to speak up. Now our government counterparts work alongside civil society organizations. All key stakeholders are equal and come together to make decisions and move in the same direction. A true partnership!” said Ms Bettenhausen.
Ms Bettenhausen grew up in northern Thailand. Her passion for the public sector started in early childhood, as she watched her father improve the livelihoods of farmers and their families through his work as an adviser for the German Government and rural development donors. Later, while studying for a master’s degree in management, she realized business was not her calling and made the decision to write her dissertation on the Human Development Center, a nongovernmental organization working in the Klong Toey slum in Bangkok. The two months that she spent working in the slums and collecting data for her dissertation gave her insight into urban poverty, drug use, child abuse and HIV. “After I graduated, I joined the business world for two years, but I felt my vocation was to follow in my father’s footsteps and to work for people. Fate was on my side and I got a position with UNAIDS,” she said.
Ms Bettenhausen’s main challenge at the Country Office is to keep up with the various tasks, as administrative work is often time-consuming. Nevertheless, she believes that everything done with due diligence is contributing to making a difference. Her work is not only critical to ensuring that the UNAIDS Country Office can fulfil its mandate, but also key to achieving the goal of ending AIDS by 2030.
Region/country





Feature Story
Turning the tide of the HIV epidemic in Thailand
17 January 2020
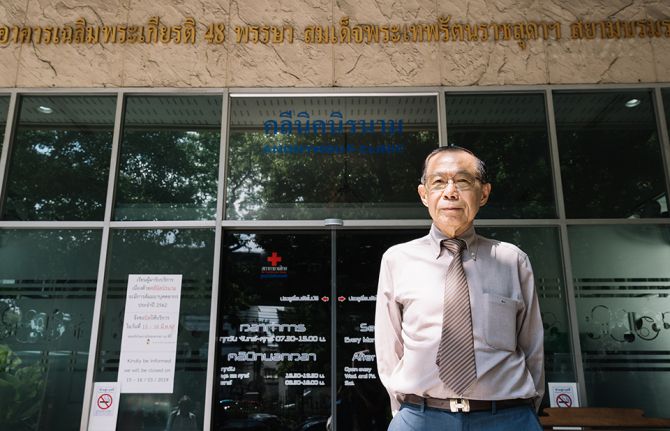
17 January 2020 17 January 2020It is a morning like any other at the Thai Red Cross AIDS Research Centre, a civil society organization operating under the umbrella of the Thai Red Cross Society. In a building in the heart of Bangkok, nurses, doctors, counsellors and peer educators are busy with their daily work, providing HIV services for the 200 people who attend the Thai Red Cross Anonymous Clinic every day for medical check-ups, HIV tests and HIV prevention services, including condoms and pre-exposure prophylaxis (PrEP).
When he was 35 years old, Praphan Phanuphak―the Director of the centre, which he co-founded in 1989―discovered the first case of HIV in Thailand. “It happened by accident. A patient was referred to me to investigate why he had a recurrent fungal skin infection,” he recalled. “In February 1985, this patient was admitted with pneumocystis pneumonia. During that month, another man was referred to the hospital with generalized cryptococcus infection. Both were diagnosed with HIV. Since then, I have devoted my life to treating people living with HIV and developing solutions to expand access to HIV services in the country.”
Mr Praphan remembers that in the early days of HIV the response in Thailand faced several challenges. At the time, Thai law required hospitals to report the names of people diagnosed with HIV to the Ministry of Public Health, which contributed to increasing stigma and discrimination against people living with HIV. In response, the Thai Red Cross established the Thai Red Cross Anonymous Clinic, Asia’s first anonymous clinic, and advocated with the Thai Government to remove the reporting law. The Anonymous Clinic remains the most renowned centre providing voluntary HIV testing in the country.
“Until the beginning of 2000, antiretroviral medicines were not available through public health facilities in Thailand, and many people living with HIV could not afford to buy them,” said Mr Praphan. He said that in 1996 the Thai Red Cross AIDS Research Centre was the first to provide free antiretroviral medicines as part of its clinical trials through the HIV Netherlands–Australia–Thailand Research Collaboration.
“After years of despair, a time of hope finally came. For that, I want to thank Her Royal Highness Princess Soamsawali, who stood by our side by setting up a fund for the prevention of mother-to-child transmission of HIV in 1996, several years before the Thai Government started its successful prevention programme,” said Mr Praphan.
The AIDS response in Thailand has changed dramatically over the years. In 2006, Thailand integrated its HIV services, including antiretroviral therapy, into its universal health coverage scheme. Since 2014 Thailand has provided antiretroviral therapy for all regardless of their CD4 level. Everyone can access treatment for free, and people living with HIV are offered treatment immediately after diagnosis.
However, many people are starting antiretroviral therapy late. “We have the medicines, but many people are not being diagnosed fast enough,” warned Mr Praphan. Despite tremendous progress, the HIV epidemic is not yet over in Thailand. HIV remains concentrated among key populations: almost 50% of new HIV infections in 2018 were among gay men and other men who have sex with men. Low uptake of HIV testing among key populations is related to the acceptability of services and stigma and discrimination, which hinder access to HIV diagnosis, prevention and care.
“From our experience, helping key populations to reach their peers and bring them to HIV drop-in centres, where they can be tested, is the best way to detect and diagnose people living with HIV early enough,” said Mr Praphan, who successfully advocated to amend Thai law to allow certified lay providers from key populations to provide a number of HIV services.
The Thai Red Cross AIDS Research Centre’s approach focuses on undertaking pilot projects to generate evidence to inform national planners and policymakers. That evidence provides a foundation for national acceptance and the roll-out of innovation on a national scale.
Taking the lead in reaching out to key populations, the centre has been offering PrEP to people at substantial risk of HIV since 2014 through projects such as the Princess PrEP Programme. In October 2019, Thailand introduced PrEP under its universal health coverage benefits package as a pilot phase in efforts to scale up PrEP nationwide.
Mr Praphan believes that policymakers and programme implementers should understand that, “We cannot continue to do business as usual. In Asia and the Pacific, several countries are still either sceptical or conservative in terms of promoting the necessary approaches to change the course of the HIV epidemic.” He thinks that the region cannot achieve the 90–90–90 targets by 2020 at the current pace. “We need to think out of the box and look at what other countries are doing that can be taken as a model. This is how we can move faster on our way towards ending AIDS as a public health threat.”
Region/country





Feature Story
UNAIDS Executive Director urges Uganda to do more domestically
09 January 2020
09 January 2020 09 January 2020The new Executive Director of UNAIDS, Winnie Byanyima, has visited the country of her birth, Uganda, on a working visit.
During her meeting with the Minister of the Presidency, Esther Mbayo, she commended the efforts of the President of Uganda, Yoweri Museveni, in the response to HIV. She highlighted the US$ 7 billion funding gap in the global AIDS response, saying more needs to be done domestically. “Today, Uganda has 93% of the AIDS response funded externally,” she said. “Our friends are the ones keeping us alive, but we cannot depend on them forever.”
She added that many African countries, including Uganda, will soon become middle-income economies and therefore will receive less international aid. Throughout the day she reiterated the same message to United Nations staff, stakeholders and partners―find ways to overcome stagnating levels of funding and reduce financial waste, inefficiencies and corruption.
Ms Byanyima also emphasized the need to focus on women and girls in Africa. “More needs to be done to rectify gender inequalities and end gender-based violence,” she said.
In eastern and southern Africa, girls and young women are two times more likely to acquire HIV than their male counterparts. In Uganda, overall HIV prevalence stands at 5.7% and 34% of new infections are among young people aged 15–24 years.
She also noted that Uganda should not waiver in protecting the human rights of everyone, and should drop the current law on same-sex sexual relationships. She said that governments should not discriminate, saying that gay men and other men who have sex with men and sex workers should not be denied access to health care.
During a meeting with civil society, Ms Byanyima encouraged them to speak up, telling them “You are the voice of citizens and you should hold government and others accountable.”
Region/country
Related


Feature Story
Treating HIV-positive children with speed and skill
26 December 2019
26 December 2019 26 December 2019How innovations in rapid testing and child-friendly medicines are saving lives in Uganda.
By Karin Schermbrucker and Adrian Brune — Originally published by UNICEF
Last year, nearly 450 infants acquired HIV every day – most of them during childbirth. These children are at extremely high risk of dying in the first two years of life. But so many of them are never diagnosed or treated.
Inadequate HIV testing and treatment for children is a widespread challenge. Although the 2019 global treatment rate for HIV-positive mothers stands at 82 per cent, the diagnosis and treatment of children with HIV is just 54 per cent in most regions.
This gap in coverage is often because diagnostic processes tend to be more complicated and cumbersome for children. Infants require a special type of testing for HIV (virological), which is not readily available in most low- and middle-income countries.
And although there are age-appropriate antiretroviral medicines for children, they can be hard to find in many areas largely due to a lack of investment in testing them.
This delayed diagnosis and treatment doesn’t have to happen. UNICEF and Uganda’s Ministry of Health recently enacted HIV treatment reforms for children to great success. With the help of partners and innovative diagnostic tools, 553 facilities across the country were able to provide antiretroviral therapy for children – up from 501 in 2017.

Dr. Denis Nansera, a paediatrician, examines Kansiime Ruth, 25, and her daughters aged 1 and 4 years, at the Mbarara Regional Referral Hospital in Mbarara District, Western Region, Uganda on 20 August 2019. "A good number of mothers used to fall out of antenatal care. But with (medical advancements), we see a huge reduction in the time taken to diagnose a child, and time taken to get child on medication,” Dr. Nansera says. Photo: UNICEF/UNI211885/Schermbrucker

Kansiime's one-year-old daughter is weighed and measured at the Mbarara Regional Referral Hospital on 20 August 2019. UNICEF, in partnership with the Ministry of Health of Uganda and the Clinton Health Access Initiative has implemented Point of Care Early Infant Diagnostic (POC EID) testing. This rapid testing process uses devices that are easy to transport, operate and maintain, allowing more health centres to diagnose infants. With early diagnosis, infants can immediately start anti-retroviral therapy. Photo: UNICEF/UNI211886/Schermbrucker

Enoch Turyatemba, a laboratory technician at Mbarara Regional Referral Hospital, takes a blood sample from a baby for early infant diagnosis testing, which screens for HIV and determines results on the same day. "Before the Point of Care [POC] machines, we collected dry blood samples and had to send them away. The turn-around time was sometimes months,” Enoch says. “With a POC machine, HIV-positive children can start treatment the next day. “We are saving lives,” Enoch adds. Photo: UNICEF/UNI211916/Schermbrucker

Enoch Turyatemba tests a sample of blood with the POC machine. In addition to the rapid testing, the Ministry of Health has approved the use of oral pellets of pediatric HIV medicine, which can be mixed with food and/or breast milk to disguise the bitter taste of the medication. The pellets also do not require refrigeration – a huge advancement. Photo: UNICEF/UNI211884/Schermbrucker

Kenyonyozi Joseline holds her baby inside the POC clinic at the Mbarara Hospital. Adolescent girls are more vulnerable to HIV infection because their reproductive systems are not fully developed. Gender inequality and patriarchal norms in Uganda also make it difficult for girls and young women to negotiate safe sex, predisposing them to early pregnancies and HIV. Photo: UNICEF/UNI211905/Schermbrucker

Kenyonyozi carries her baby on her back outside the the POC clinic. Paediatric HIV services lag considerably behind those for adults and pregnant women. While 82 per cent of mothers living with HIV receive treatment, only 54 per cent of children living with HIV are accessing life-saving drugs. Just 59 per cent of babies born to mothers living with HIV are tested for HIV within the first two months of life. Photo: UNICEF/UNI211891/Schermbrucker

Kansiime and her daughters arrive at the Mbarara Hospital. The three family members all live with HIV and go to the clinic regularly to collect their medication. "When I go to hospital, I am surrounded by other women who have come for treatment. We are there for the same reason,” Kansiime says. “This has helped me overcome stigma and given me strength." Photo: UNICEF/UNI211907/Schermbrucker

Kansiime gives her one-year-old daughter her paediatric HIV medicine at home in western Uganda. Her daughter now takes the oral pellets instead of the bitter syrup she used to use, which has helped her viral load. "It is much easier to give her the pellets mixed into food so she doesn’t struggle with the taste,” Kansiime says. “My advice to other mothers: Give your children the medication they need so they can live longer and educate others." Photo: UNICEF/UNI211882/Schermbrucker

Kansiime's four-year-old daughter peeks her head outside the door to her house. She was born with HIV and needs to take medication on a daily basis. But she has survived past the critical period for young children and infants, making her survival into adolescence and beyond more likely. “I love singing – my favorite song is a song called Sconto,” she says. Photo: UNICEF/UNI211903/Schermbrucker

Kabiite Ajara, 32, helps her baby take her paediatric HIV medication in their home in Isongo, Uganda. They are both living with HIV. "I give my baby medication once a day,” she says. “Initially medicine used to make her weak and vomit. But currently she is ok with the drug – I crush the tablet and put it into water, which she takes easily." Photo: UNICEF/UNI211928/Schermbrucker

Kabiite plays with her daughter outside their home. Kabiite is HIV-positive, but regular medication keeps her strength – and spirits – high. "I love playing with my children – taking them to play in the banana plantation, cooking together,” Kabiite says. “[My daughter] loves playing football a lot! And she is good!” Photo: UNICEF/UNI211933/Schermbrucker
This World AIDS Day, UNICEF is calling on all governments and partners to urgently close the testing and treatment gap for children and adolescents living with HIV-AIDS; to establish supportive, stigma-free communities that provide opportunities for testing and care; and to enact improved policies and rights for people living with this survivable epidemic.
UNICEF resources
Region/country
Related





Feature Story
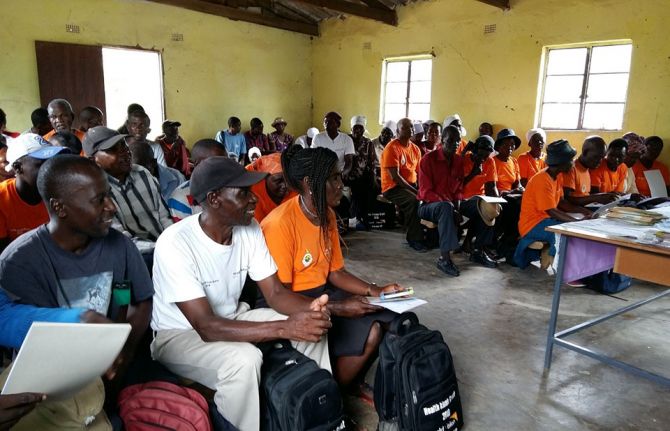
Health kiosks expanding HIV services in Zimbabwe
18 December 2019
18 December 2019 18 December 2019If you drive through Zimbabwe on a typical Saturday or Sunday, you will see many places of religious worship. Some are static structures, while others are mobile. Some services are held under trees or in open spaces.
Many people in Zimbabwe follow a religious faith. The Apostolic community is a major religious sect that discouraged its members from seeking medical care, including HIV services, preferring to use prayer for healing―this led to many people becoming ill and dying from preventable diseases. However, with the implementation of so-called health kiosks, the community is now encouraging its members to access medical care.
David Adashe (not his real name), an Apostolic leader in Gokwe North, explained that health kiosks staffed by church volunteers trained by the Zimbabwe health ministry helped his congregation to access much needed information on HIV prevention. He described it as like, “Going from a thick cloud of darkness into a plane of light of splendour.”
Ms Adashe said that his congregation’s views about seeking medical assistance from health facilities have changed. They now seek out medical care, receive counselling from trained volunteers and are referred to a health facility for additional services, if needed. “I was naive and reluctant to take health issues seriously, but since the emergence of the health kiosk programme, I am now more empowered. I’m now encouraging my family to access health services from the clinic,” he said.
Since March 2018, World Vision Zimbabwe, in collaboration with the Ministry of Health and Child Care, has been empowering faith leaders like Mr Adashe and church volunteers through training and creating safe spaces to bring health information and services to their congregations.
A health kiosk volunteer in Gwanda said, “As a volunteer, I observed that previously it was difficult for some individuals to travel to the local clinic on their own to seek medical advice, but since the programme started it is easy now, since they can access the information on their doorstep through the health kiosks.”
Many faith worship centres participating in the health kiosk programme have seen a threefold increase in the uptake of HIV and health information. Half of the people requesting information on HIV take an HIV test and receive their results. People who test positive for HIV are referred for antiretroviral therapy and supported to stay in care through the help of the trained church volunteers.
Faith leaders and church volunteers are essential in controlling the HIV epidemic. They provide care for their members, create safe space for information-sharing and are trusted by their members. Regular contact with the congregations enables the volunteers to bridge the gap in services for those who need them the most. The health kiosks also serve as effective and sustainable platforms to bring together both faith and non-faith communities to address the health needs of their members and to provide safe spaces to engage on other health matters.
“The findings from the health kiosk programme are promising for addressing the HIV epidemic. This is a key example of community-led responses by, for and within faith communities providing safe spaces and support for their members. These kinds of responses are essential for ending new HIV infections and AIDS-related deaths and critical for reaching universal health coverage,” said Laurel Sprague, Chief of the UNAIDS Community Mobilization, Community Support, Social Justice and Inclusion Department.
Region/country
Related


Feature Story
Communities are making the difference in the HIV response
18 December 2019
18 December 2019 18 December 2019For young women and girls, for marginalised, vulnerable groups of people such as gay men and other men who have sex with men, transgender people, sex workers, people who use drugs, prisoners and migrants, the pathway to health is not always as clear-cut as it should be.
Stigma and discrimination, repressive laws, ignorance and even hate, can all prevent vulnerable people from accessing life-saving prevention, treatment and care.
Communities are fighting for HIV services
This is where communities often step in. Communities of people living with HIV, of marginalised and vulnerable groups, of women and of young people, lead and sustain the delivery of peer-to-peer HIV services. They also defend human rights and advocate for access to essential services. They fight every day to keep people at the centre of decision-making and implementation and help to make sure that no one is left behind.
Women and girls are the backbone of care support in their families and communities, providing unpaid and often undervalued work in caring for children, the sick, the elderly and the disabled. They often underpin fragile social support systems. The involvement and leadership of women is vital in the response to HIV and we must support them to leverage their potential.
Community-based services often support fragile public health systems by filling critical gaps; they are led by, or connect, women and other marginalised populations; they provide services that complement clinic-based care and they extend the reach of healthcare to groups that would otherwise fall through the gaps.
Reduced funding is a barrier to HIV
At a time when reduced funding is putting the sustainability of HIV services in jeopardy, community activism remains critical. Indeed, a greater mobilisation of communities is urgently required and barriers that prevent them delivering services and seeking funds must be dismantled. Communities must have the space and power to voice their demands and write their own solutions.
In 2016, world leaders signed the United Nations Political Declaration on Ending AIDS, which recognised the essential role that communities play in advocacy, participation in the coordination of AIDS responses and service delivery. Moreover, they recognised that community responses to HIV must be scaled up and committed to at least 30% of services being community-led by 2030.
Most countries are nowhere near reaching that commitment and where investment in communities is most lacking, there is often weaker progress against HIV and other health challenges.
Communities stand ready to play their part in building healthier and more resilient societies, but they need our support. On World AIDS Day, let’s celebrate communities, recognise the essential role they play in the response to HIV, and commit to meeting the promises made to them.


Feature Story
Remembering the leadership of Charlot Jeudy
03 December 2019
03 December 2019 03 December 2019Charlot Jeudy, the President of Haiti’s lesbian, gay, bisexual and transgender (LGBT) community organization Kouraj, was found dead at his home in November. Investigations into the circumstances of his death are ongoing. UNAIDS remembers Mr Jeudy as a fearless campaigner for human rights.
In the aftermath of the devastating earthquake in 2010, the people of Haiti worked to overcome the loss of homes, businesses, public services and more than 100 000 lives. But amid the shared trauma and determination, a harmful narrative emerged.
Some people began to blame the masisi—a derogatory Haitian Creole term for gay men. They thought that the disaster was a divine punishment for the sins of the LGBT community. Members of sexual and gender minorities found themselves subject to intensified exclusion and abuse. Human rights organizations documented cases of LGBT people being denied access to emergency housing, food, health care and work. There were also reports of physical assaults and homophobic rape.
Rather than accept the situation, Charlot Jeudy decided to act. He created Kouraj, which means courage in Haitian Creole. In the struggle for equal rights, Kouraj emphasized the importance of community empowerment and aimed to inspire pride and confidence among LGBT people.
“We wish to put forward an alternative discourse on homosexuality in Haiti because for too long only homophobes have discussed our reality and proposed their own interpretation,” Mr Jeudy said in 2011.
Over the next eight years, Kouraj evolved to offer community training, legal and psychosocial services and sexual health education. It became one of Haiti’s leading advocates for ending discrimination against LGBT people and has played a key role in resisting the introduction of discriminatory laws.
The organization was aptly named. Its members have contended with verbal abuse and death threats. Three years ago, it had to cancel a festival to celebrate the Afro-Caribbean LGBT community after numerous threats of violence. According to friends, Mr Jeudy resisted their pleas to leave the country at the time. In response to a spike in reports of anti-LGBT street violence last year, he worked with the United Nations on a project to promote tolerance and equal rights.
John Waters, Programme Manager of the Caribbean Vulnerable Communities Coalition, paid tribute to Mr Jeudy’s leadership.
"I have watched Charlot Jeudy grow from a young, impatient and impassioned activist into a thoughtful, strategic leader, capable of using human rights not as a sword, but as a shield,” said Mr Waters. “He won over the hearts and minds of others to create allies. Mr Jeudy has left a huge gap in human rights work in the Caribbean. He raised the bar for those who must now follow in his footsteps.”
Mr Jeudy was also an active civil society representative on the body that oversees the management of Haiti’s response to HIV, tuberculosis and malaria.
“Under Charlot Jeudy’s leadership, Kouraj was a model partner,” said Fritz Moise, Executive Director of the Foundation for Reproductive Health and Family Education. “His death is a big loss for the response to HIV in Haiti.”
UNAIDS has added its voice to the expressions of grief and also paid tribute to the leadership of Mr Jeudy.
“Charlot Jeudy exemplified the power of communities to be the voice for the voiceless and to make meaningful change in people’s lives,” said UNAIDS Country Director for Haiti, Mame Awa Faye. “This World AIDS Day we celebrated the power of communities to make a difference. Mr Jeudy did just that.”
Region/country


Feature Story
Commemorating World AIDS Day in Belgium
05 December 2019
05 December 2019 05 December 2019Gunilla Carlsson, the UNAIDS Deputy Executive Director, Management and Governance, commemorated World AIDS Day in Brussels, Belgium, celebrating the power of communities with civil society and Barbara Trachte, the Secretary of State of the Brussels-Capital Region.
Ms Carlsson presented some of the key messages from Power to the people, UNAIDS’ new report, which shows that when people have the power to choose, to know, to thrive, to demand and to work together, lives are saved, injustices are prevented and dignity is restored.
“The AIDS response shows that when communities are empowered and have agency, change happens. Now more than ever we need a fully funded community-led response,” said Ms Carlsson.
She thanked the Regional Government of Brussels and the Federal Government of Belgium for its support for people living with HIV and the organizations working on HIV and related sexual and reproductive health and rights. For many years, Belgium has invested energy and resources to meet the needs of the most vulnerable and communities affected by HIV around the world, with a strong focus on human rights, gender equality, key populations, strengthening health systems and sexual and reproductive health and rights.
"Today, on 1 December, it is important to reinforce that undetectable = untransmittable in order to change society’s view of people living with HIV,” said Thierry Martin, Director of Plateforme Prévention Sida.
During her visit to Belgium, Ms Carlsson also met with the Minister-President of Flanders, Jan Jambon, and signed a new two-year partnership agreement with UNAIDS. Flanders has been a valued and prominent partner since the founding of UNAIDS and has invested energy and resources to meet the needs of communities affected by HIV, with a focus on vulnerable populations and girls in southern Africa.
Mr Jambon expressed confidence in renewing the long-term partnership agreement with UNAIDS. “Since its inception, UNAIDS has been working towards a multisectoral, rights-based and people-centred approach that addresses the determinants of health and well-being for the AIDS response, especially the most vulnerable populations, including the LGBTQI+ communities, and this is now more relevant than ever,” he said.
Mr Jambon also welcomed the reforms within UNAIDS to reinforce a positive workplace culture. “I am confident that with the new policies in place and the new leadership, this will enable staff to deliver at their best and maximize their collective results,” he said.
Ms Carlsson also attended a panel discussion with members of the parliament and representatives of civil society and the United Nations, where she provided an update on the status of the HIV epidemic and response, highlighting key actions for support by the European Parliament and European Union. She emphasized the important role that parliamentarians play in the global response to HIV.

















