Feature Story
Pan-African Parliament calls for increased domestic resources for HIV and health in Africa
15 July 2019
15 July 2019 15 July 2019A communiqué adopted at the High-Level Pan African Summit on HIV and Health Financing has called for parliamentarians to ensure the right to health for all and for stronger advocacy to increase domestic resources for HIV and health.
“There is an urgent need for our governments to mobilize domestic resources to ensure sustainable and affordable access to HIV treatment, for all, to ensure that all women have the same chances as I did to raise HIV-free and healthy children,” said Valerie Maba, President of the national network of HIV-positive organizations of the Congo.
Roger Nkodo Dang, the President of the Pan-African Parliament, highlighted the urgency of finding durable sources of financing to respond to HIV and to improve public health services in Africa.
Significant increases in both domestic and international funding have enabled African countries to rapidly expand their HIV programmes in recent years. In 2018, 16.3 million people living with HIV were on antiretroviral therapy in sub-Saharan Africa, representing 70% of the total number of people on antiretroviral therapy globally. At the end of 2017, about US$ 21.3 billion was available for HIV programmes in sub-Saharan Africa, with domestic investments accounting for approximately 56% of total resources.
Countries were also encouraged in the communiqué to further contribute to global solidarity in the upcoming replenishment of the Global Fund to Fight AIDS, Tuberculosis and Malaria. “Today, we are honoured to be among you and we salute the efforts of 11 African member states that have already stepped up and pledged,” said Marijke Wijnroks, Chief of Staff of the Global Fund.
In 2001, the heads of state of the African Union committed, through the Abuja Declaration, to allocate at least 15% of national budgets to health care in order to achieve universal health coverage. However, the share of expenditure allocated to health in national budgets in Africa has in fact decreased, and in 2018 there was a gap of US$ 5 billion for the AIDS response, and only two out of 55 African Union member states complied with the Abuja Declaration targets.
In February 2019, African Union member states reiterated their commitment to increase domestic resources for health on the sidelines of the 32nd Ordinary Session of the Assembly of Heads of State and Government through the Declaration of the Investing in Health Africa Leadership Meeting.
“Ending AIDS by 2030 is a Sustainable Development Goal and an aspiration of Agenda 2063. Controlling the epidemic is a prerequisite for sustainable results. If our governments do not Fast-Track and ensure the financial sustainability of the response, the socioeconomic and human burdens will get worse,” said Clémence Bare, Director of the UNAIDS Liaison Office to the African Union.
Held under the auspices of Denis Sassou Nguesso, the President of the Congo, and convened by UNAIDS, the Pan-African Parliament and the Regional Office for Africa of the World Health Organization, the summit was held in Brazzaville, Congo, on 11 and 12 July.
Related


Feature Story
Indonesia commits to piloting PrEP
15 July 2019
15 July 2019 15 July 2019Indonesia has decided to pilot pre-exposure prophylaxis (PrEP) in four cities with high levels of HIV prevalence. PrEP is a way for people who do not have HIV but who are at substantial risk of getting it to prevent HIV infection by taking a pill every day. It is hoped that the pilot project will pave the way for a wider roll-out across the country.
The commitment to piloting PrEP came during the 1st Indonesian Symposium on PrEP, which was organized by UNAIDS at the end of June. The two-day event brought together around 150 clinicians, public health officials and representatives of key populations, who shared their experiences of PrEP research and implementation strategies across the Asia-Pacific region. The pilot in Indonesia will be conducted in close collaboration with the Ministry of Health.
PrEP is a highly effective prevention choice for people who are at high risk of HIV infection such as sex workers, people who use drugs and gay men and other men who have sex with men. It is having a big impact in reducing new HIV infections in Australia and its availability is increasing in New Zealand, Thailand and Viet Nam. China, India, Malaysia and Philippines have also initiated pilot projects.
Prevention efforts are vital to strengthening the HIV response in Indonesia and PrEP would be a significant addition to the country’s combination prevention approach. Indonesia had 46000 new HIV infections in 2018 and has one of the fastest growing epidemics in the Asia Pacific region. In 2018 there were 640000 people living with HIV in the country and only 17% had access to treatment.
The discussions at the symposium helped to disperse some of the common misconceptions regarding PrEP, both among communities and services working to reduce new HIV infections. Civil society activists expressed their strong support for PrEP roll-out.
“PrEP will become a necessity for sex workers,” said Rito Hermawan of the Indonesian Sex Workers Network, “As well as using condoms, they can get additional protection by using PrEP. We must educate people about PrEP to stop any misconceptions.”
Other civil society activists echoed their support.
“The more I learn about the benefits of PrEP, the more I wonder why it is not available here,” said Mr. Riunaldi from Intermedika Prana Foundation, “I am hopeful that more people will understand how important PrEP is for our country.”
Participants in the symposium said that many people were already accessing PrEP online, indicating a growing demand in Indonesia.
“It is incumbent on policy makers, health professionals, researchers and civil society organizations to ensure that those at risk of HIV infection have access to the information and resources needed to make informed decisions regarding their health” said Tina Boonto, UNAIDS Country Director for Indonesia.
Region/country


Feature Story
Charting progress against discrimination
12 July 2019
12 July 2019 12 July 2019Laws discriminate in many ways, but the criminalization of people is one of the most devastating forms of discrimination. Despite calls for reform and the commitments under the 2030 Agenda for Sustainable Development to remove discriminatory laws and reduce inequalities:
- Sixty-nine countries still criminalize same-sex sexual relationships.
- More than 100 countries criminalize drug use or the personal possession of drugs and 98 countries criminalize some form of sex work.
- One in five people in prison are there because of drug-related crimes and 80% of those are there for personal possession or use.
- Nineteen countries deport non-nationals on the grounds of their HIV status.
A high-level political forum is meeting in New York, United States of America, from 9 to 18 July to review the progress made against the commitments of Member States towards achieving the Sustainable Development Goals, including those on inequality and on peace, justice and strong institutions.
“As a judge, I have seen the effect that criminal law can have on communities. It takes people outside systems of protection, declares their actions or identity illegitimate, increases stigma and excludes them from any protections our judicial, social and economic systems may provide,” said Edwin Cameron, Justice of the Constitutional Court of South Africa.
Criminalization affects access to health services, housing, education, social protection and employment. The criminalization of same-sex sexual relationships, sex work or drug use prevents people from accessing health-care services, including HIV prevention, testing and treatment. Data show that gay men and other men who have sex with men are 28 times more at risk of HIV than the general population, people who inject drugs are 22 times more at risk and sex workers and transgender women are 13 times at risk.
“To fully implement the Sustainable Development Goal agenda and make sure that no one is left behind, we need to ensure the laws are protecting people from discrimination and not pushing people into hiding from society,” said Lloyd Russell Moyle, United Kingdom Member of Parliament.
Groups that represent criminalized people are often barred from registering as nongovernmental organizations, and, for example, sex workers often can’t unionize. Propaganda laws may mean that information on, for example, HIV prevention can’t be disseminated.
“Ending AIDS and meeting the health-related Sustainable Development Goals targets will not be possible without addressing discrimination, violence and exclusion. We have an opportunity to harness the lessons from the AIDS movement and place rights and the meaningful participation of the most marginalized at the centre of the response,” said Luisa Cabal, Director for Human Rights and Gender, UNAIDS.
Criminalized groups often experience higher rates of violence than the general population. Victims of violence who are also criminalized often can’t report crimes against them to the police, and lawyers risk violence and other repercussions if they take up their cases.
“Discrimination against and criminalization of people living with HIV still continues to this day. And we are facing in Indonesia persistent stigma against and criminalizing of key populations. We will never end AIDS if we are not making their needs and rights a top priority for access to health care, protection against violence and realization of the right to health,” said Baby Rivona, from the Indonesian Positive Women Network.
Countries that decriminalize drug use and make harm reduction services available have seen reductions in new HIV infections. Evidence shows that decriminalizing sex work could avert between 33% and 46% of new HIV infections among sex workers and clients over 10 years. However, reductions in new HIV infections are not the only outcome—other outcomes include improvements in well-being and trust in law enforcement, reductions in violence and increased access to health-care and support services. Above all, however, decriminalization of people results in them no longer being seen as criminals and stigmatized by society.




Feature Story
Youth networks are saving lives
10 July 2019
10 July 2019 10 July 2019A study undertaken by Watipa and commissioned by UNAIDS and the PACT as part of its #uproot agenda found that young people play an essential role in demand creation, linkages to care and uptake of services for HIV and sexual and reproductive health and rights.
The report showcasing the results, titled Young people’s participation in community-based responses to HIV: from passive beneficiaries to active agents of change, showed that young people, particularly role models and leaders who are living with HIV, play a critical part in enabling access to HIV treatment and retention in care. The results showed that the support provided by young people to their peers has a positive effect on antiretroviral therapy adherence, navigating disclosure and living positively with HIV. Details of the types of support show that young people are actively involved in peer psychosocial support, peer-to-peer consultations, policy engagement processes, peer mobilization around specific campaigns and projects, and peer-supported hospital and care access.
Young people, including young key populations and young people living with HIV, also play a key role in primary HIV prevention, early testing and diagnosis. Peer education, outreach and community engagement are all areas where young people are informing and influencing their peers. In some examples, young people working as peer supporters and volunteers provided HIV testing and counselling services, distributed condoms or worked alongside community-based health assistants.
62% of surveyed individuals who were members of a youth organization in the HIV response indicated that they themselves provide HIV services directly to young people. These were services designed to benefit and reach young people as the focus groups. The provided services include information about sexual and reproductive health and rights (51%), peer support (50%), psychosocial support (42%), condom promotion and distribution (41%), antiretroviral therapy adherence support (32%) and HIV counselling and testing (30%). Many of the organizations surveyed offered integrated services, including referrals, prevention, and testing and treatment of other sexually transmitted infections (STIs) (38%), tuberculosis (28%) and/or hepatitis B and C (22%).
As one key informant mentioned, “It’s easy to disseminate the knowledge among ourselves, because if [I] am part of it, then it’s easier to talk to somebody of my age about it.”
The primary data was collected through three methods: 1) an online quantitative survey with 32 questions that was offered in five languages (Arabic, English, French, Russian and Spanish), peer interviews, which were semi-structured qualitative interviews conducted by young people in either English or their local language in six different countries, and key informant interviews, which were semi-structured qualitative interviews conducted in English via Skype by two young consultants leading the research team. The total number of participants was 143, between the ages of 20 and 29.
The role of young people in community-based responses to HIV is vital to achieve and sustain positive health outcomes in the context of HIV. One key informant said that “Young people living with HIV are changing the game in the community. They are peer educators, mentors . . . they support other young people at health facilities to direct them about services to make the process swifter for them while receiving services. Many young people are involved in advocacy where they speak for the voices of [the] young.”
However, the lack of appropriate or proportional remuneration for the role of young people in demand creation and enabling linkages to care seems to be a critical barrier to the sustained, effective and meaningful involvement of young people. Other barriers inhibiting their participation included a lack of funding for institutional support, a lack of capacity or support for the knowledge necessary to participate fully in technical discussions, and a lack of tailored tools and resources to support participation in different processes and mechanisms.
The study also provides thirteen recommendations from the young people who participated in the research, and are aimed at government authorities, United Nations entities, donors, civil society organizations and other stakeholders in the HIV response. These recommendations include the need to involve young people in design, planning and delivery of HIV policies, programmes and services as well as recognize the essential role that young people have in implementing service delivery to their peers.
Related
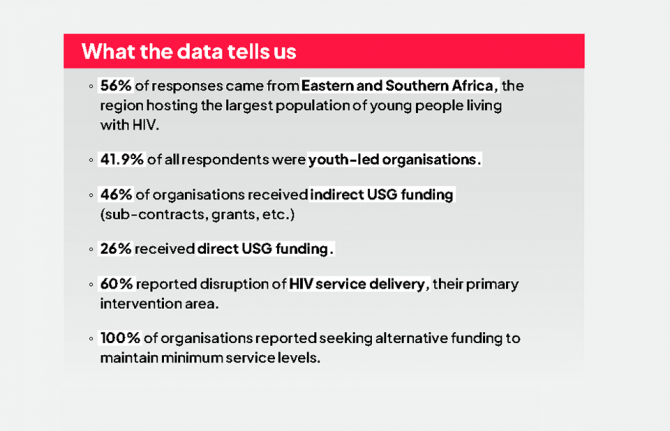
 “Who will protect our young people?”
“Who will protect our young people?”

02 June 2025


Feature Story
Pakistan: bringing services closer to communities affected by the HIV outbreak
03 July 2019
03 July 2019 03 July 2019A newly refurbished paediatric centre is to open in Ratodero, Pakistan, to serve families affected by the recent HIV outbreak in the district of Larkana. It is expected that the centre will be operational by mid-July.
Alia (not her real name), the mother of a two-year old girl, lives in the village of Mirpur Bhutto, in Ratodero Taluka in Larkana district. Alia’s world has been turned upside down since her family was caught up in the HIV outbreak in the area.
“My daughter was diagnosed with HIV just a few days ago, but she became so weak so quickly. She couldn’t eat anything we gave to her,” says Alia. After Sameera’s (not her real name) diagnosis, she was referred to Sheikh Zayed Children Hospital in Larkana to start antiretroviral therapy. The hospital is more than 50 kilometres away from the family home.
“I got these dispersible tablets for Sameera and some fever medicine, and since she started her treatment, I have seen some improvements in my daughter’s health. Her fever has gone and before there was diarrhoea from which she also recovered,” explains Sameera’s mother.
Alia’s husband is a farmer and earns less than two dollars a day. “We can hardly support our family of ten members,” she explains.
Poor road conditions and economic constraints make it difficult for Alia and her daughter to travel from their village to the district capital Larkana, currently the nearest health facility where her daughter can receive the treatment she needs.
Since the HIV outbreak was first reported in Larkana at the end of April, UNAIDS, UNICEF, the World Health Organization, the Sindh AIDS Control Programme and other partners have been calling for a new paediatric treatment centre in Ratodero to bring HIV services closer to the affected communities. As a result of these efforts and in the framework of the “Sindh HIV Outbreak Response Plan, May 2019-Apr 2020,” UNICEF is refurbishing the paediatric HIV treatment centre at Taluka Headquarters hospital in Rotadero, ensuring that treatment will be available in the area where Alia and her daughter live. When the new centre opens, HIV treatment services for Sameera will be less than 10 kilometres away.
“I know my Sameera will be fine and that she will get married and have children. This is what the doctor told me. For this to happen she must continue her treatment forever. I will follow the doctor’s instructions because this is what will save my daughter’s life,” says Alia.
By the end of June, 877 people had been newly diagnosed with HIV in the Larkana district. More than 80% of the new cases are among children aged under 15 years old. A total of 721 people had already been registered in care programmes and 482 people (365 of them children under the age of 15) were on treatment.
“UNAIDS is working closely with the government, civil society organizations, the association of people living with HIV, UN agencies and all other partners to ensure that both the immediate response to the HIV outbreak and longer-term programmatic measures will be implemented and sustained,” said Maria Elena Borromeo, UNAIDS Country Director for Pakistan and Afghanistan.
Region/country


Feature Story
No end to AIDS without respecting human rights
28 June 2019
28 June 2019 28 June 2019“Sex workers are 13 times more at risk of becoming HIV positive than the general population globally. But, in Australia, where sex work is decriminalised, we have the same rate of infection as the general population. This is evidence of the importance of the legal environment” says Jules Kim, head of the Scarlet Alliance, the Australian Sex Workers Association.
The Human Rights Council first examined the question of HIV and human rights 29 years ago, in 1990. Since then, it has been steadfast in its assertion that progress in the response to the AIDS epidemic is indissociable from progress on human rights issues. Today, as it discusses new recommendations on human rights and HIV, its work is more important than ever.
A total of 48 countries and territories still maintain travel restrictions on people living with HIV. One in five people living with HIV report having been refused health care because of their HIV status, and in many parts of the world, people who use drugs and sex workers live in fear of arrest for being in possession of clean syringes or condoms.
Adolescent girls and young women are among those worst affected because of a lack of respect for their rights. In 2017, 79% of new infections among 10-19 year-old young people in eastern and southern Africa were among females. Inequalities and institutional barriers increase vulernabilities and decrease access to services. Young people in 45 countries are unable to access sexual and reproductive health services or HIV testing services without parental permission.
At a meeting held on the sidelines of the 41st session of the Human Rights Council, co-convened by Brazil, Colombia, Mozambique, Portugal and Thailand, UNAIDS Deputy Executive Director, Shannon Hader, called on countries to dismantle barriers that prevent people accessing essential services. “It has been four years since the world committed to ending the AIDS epidemic by 2030 and three years since the United Nations General Assembly adopted the High-Level Political Declaration on Ending AIDS, which included a commitment to remove human rights barriers by 2020. We have less than two years to deliver on that promise”.
The event marks the presentation of a report and recommendations on HIV and human rights being presented by Michelle Bachelet to the Human Rights Council on July 1. The report, resulting from consultations with civil society, experts, governments and UN mandate holders in February, includes best practise examples, including on the training of health workers on ending stigma and discrimination, on decriminalizing drug use and same-sex sexual activity, model laws on HIV, the training of judges and lawyers, civil society advocacy, and international funding opportunities specifically for human rights programming.
“We cannot address the human rights dimensions of HIV without civil society, who plays a critical role” stated Rui Macieira, Ambassador of Portugal to the United Nations in Geneva.
“The 2030 Agenda for Sustainable Development is an important agenda for people, planet, prosperity, peace and partnership. In order not to leave anyone behind. States should increase their efforts to reach the most marginalized,” said Peggy Hicks, director of the Thematic Engagement, Special Procedures and Right to Development Division of the Office of the High Commissioner for Human Rights.
Member states will examine the recommendations that highlight how reforming criminal laws is critical to advancing progress towards the elimination of HIV, including laws criminalizing gender expression or adult consensual sex, including sex work and same sex relations, as well as drug use. The recommendations include a call for strengthening cooperation at regional, sub-regional and global levels to support and invest in programmes and services that promote the right to health and rights of people living with HIV. This is important in the context of shrinking donor funding for HIV and health programmes, including in newly transitioned middle-income countries.
“I live with HIV, I come from a very small community, a slum area of a Kenyan city. If the recommendations of this report are implemented in a facility that I walk to everyday – a health facility, a police station, then it will work and provide us with the services we need and deserve as a basic human right.” concludes Lucy Wanjiku, a young woman living with HIV.


Feature Story
“The staff at the clinic are very friendly. I am an old client so they all know me very well”
02 July 2019
02 July 2019 02 July 2019This story was first published by UNFPA
Windhoek, NAMIBIA - Sometimes it is best to go where everyone does not know your name, but where you feel welcome just the same. It is that way for many sex workers and men who have sex with men (MSM) in Namibia, who bear the brunt of criticism, repulsion and stigmatism in almost all aspects of their daily lives.
As a result, these men and women shy away from accessing essential health services, such as HIV testing/treatment, prophylaxis (PrEP), condoms, lubricants and contraceptives.
According to the first ever integrated bio-behavioral surveillance study (IBBSS) 2014, among MSM in Namibia, HIV prevalence among MSM was estimated to be 10.2 per cent in Keetmanshoop, 7.1 per cent in Oshakati, 10.1 per cent in Swakopmund/Walvis Bay, and 20.9 per cent in Windhoek the capital city.
The estimated HIV prevalence estimated among MSM in Oshakati and Swakopmund/Walvis Bay approximated that of the general population of adult males in the surrounding Oshana and Erongo regions, as measured by the Namibia Demographic and Health Survey, 2013.
HIV prevalence among MSM in Keetmanshoop was slightly lower than that of the general population of adult males in Karas Region, while HIV prevalence among MSM in Windhoek was nearly twice as high as HIV prevalence among adult males of the general population in Khomas Region.
Non-judgemental care
In 2018, the Namibia Planned Parenthood Association (NAPPA) with support from United Nations Population Fund (UNFPA) Namibia convened several advocacy meetings with key partners aimed at establishing a drop in centre at the Out Right Namibia offices.
Out Right Namibia is a Namibian organisation working with the lesbian, gay, bisexual, transgender and intersex (LGBTI) community aimed at advancing the rights, interests and expectations of the LGBTI community in Namibia.
Both the drop in centre and NAPPA Okuryangava clinic had flexible working hours to allow key population to access sexual and reproductive health (SRH) and HIV services at their convenient times, it also involved opening the clinic on Saturdays to allow key population to access services without fear of stigma and discrimination.
All service providers and staff at the drop in centre and clinic were trained and sensitised on the importance of quality, non-judgemental service provision to key population. The staff at Outright Namibia were also mobilised to build awareness and information about the services being provided at the drop in centre and clinic.
Pleasant experience
“I have had a very pleasant experience visiting NAPPA. As a sex worker, it is important that I feel comfortable and go to clinics where I’m free of judgement. NAPPA has opened their doors for me and I feel at home. There are no complications here as the services are free and I prefer this clinic over local hospitals,” said sex worker, Martha Keto (not her real name).
Keto, 30, has been a sex worker for almost 12 years and has been receiving PrEP treatment at the clinic since October 2017. ”I come regularly for my tests and for PrEP treatment which keeps me protected from contracting HIV. The testing I receive here not only keeps me updated on my HIV or STI status, but it keeps up with my overall health. I am informed about a lot of health information including my liver and the nurses are even able to tell if my alcohol consumption is too high,” she said.
“The staff at the clinic are very friendly. I am an old client so they all know me very well. I would recommend NAPPA services to my colleagues who are also workers. Their doors are always open for us, even during weekends we are able to come in if needed. There is a large number of sex workers in Namibia and I hope the services provided by NAPPA could be exposed so that more sex workers will be informed of the free services that are offered here,” she said.
Keto’s sentiments are shared by Cinton Nati and Gideon Markus, (not their real names) who are both homosexual males receiving services at the NAPPA clinic.
“If it had not been for the friendly staff at the NAPPA clinic and their constant support and encouragement, I would have not visited the clinic as recommended by the nurse,” said Nati. He said this made it easy for him to develop a personal relationship with the clinic’s staff because they were very encouraging and as a result, he was able to see major improvements not only in his health but also his confidence.
Prior to visiting NAPPA, Nati experienced emotional and mental difficulties associated with being newly diagnosed with HIV. As a result, he would often miss his appointments as he found it difficult to accept the reality of being newly diagnosed with HIV.
“Since the very first time my partner and I went to the NAPPA clinics, both at Out Right Namibia and at Okuryangava, we have been treated very well and the staff have gone out of their way to make us feel safe. I have had counselling sessions to make sure that I am doing alright and also checkups to make sure the medication is not having any side effects on my body and that I remain healthy. The staff at the clinics have also regularly checked that we understand how to look after ourselves and that we practice sound sexual health guidelines,” said Markus.
“Each time we visited the clinic at Okuryangava, Sister Fungai Bhera (Senior Registered Nurse) would first make time to chat to us about how we have been. This might sound like a small thing to others, but to me, it means the world as I know she cares about us and that I am taken care of and in safe hands,” said Van Den Berg.
He alluded: “LGBTI community in Namibia has never had proper support from our country’s leaders and as a result, there is still a lot of LGBTI people that get discriminated against and live in fear of their communities as we do not enjoy the same legal rights. Hence we live very secretive lives, sometimes even double lives. I think it is these secret lives that make it easy for LGBTI people in Namibia to land in situations where they are highly vulnerable to getting infected with HIV and other sexually transmitted infections.”
More KPs accessing services
In 2018, a total of 523 KPs were reached with sexual and reproductive health services at the two sites. This included 233 sex workers, 188 men who have sex with men 70 truck drivers and 32 women who have sex with women. A total of ten outreach events were held targeting KPs at various hotspots in Windhoek.
The comprehensive service package provided at the two sites included: HIV testing and counselling, those who tested positive were immediately enrolled for treatment; PrEP services, those who tested negative were also counselled and informed about PrEP services and those who agreed were enrolled on PrEP; family planning services including condoms; sexually transmitted infections (STIs) screening and treatment; and information education related to SRH, HIV and gender-based violence.
Region/country
Related


Feature Story
New modelling research shows partial progress in South Africa’s response to HIV
28 June 2019
28 June 2019 28 June 2019South Africa is making strong progress in scaling up HIV testing and increasing viral suppression in patients receiving antiretroviral therapy (ART), but is not yet reaching its targets for treatment coverage and HIV prevention, according to an updated Thembisa model released at the 9th South Africa AIDS Conference in June.
The results of the annual updated Thembisa model (version 4.2) was released by researchers at the Centre for Infectious Diseases Epidemiology and Research, University of Cape Town. Work on the Tembisa HIV estimates is funded by UNAIDS through a grant from the United States Centres for Disease Control (CDC), and used data from multiple sources including recent surveys by the Human Sciences Research Council and the Medical Research Council of South Africa.
South Africa is committed to reaching the UNAIDS 90–90–90 Fast-Track targets by 2020. The aim of this strategy is to ensure that 90% of people living with HIV are tested and know their status, that 90% of people living with HIV are receiving treatment, and 90% of people on treatment have a suppressed viral load. The latest Thembisa estimates indicate that South Africa reached 90–68–88 by mid-2018. This means that total viral load suppression among all people living with HIV was 55%, which is 18 percentage points below the target of 73%.
The Thembisa model also estimates that men had a lower uptake of HIV testing and treatment compared to women. As a result, in 2018, 47% of HIV-positive men were virally suppressed compared to 58% of HIV-positive women. This was also reflected in annual AIDS-related deaths which halved from 2010 to 2018, but with men increasingly over-represented.
Women accounted for 62% of new HIV infections in adults from 2017 to 2018. The lead developer of the Thembisa model, Leigh Johnson, said two factors were hampering progress on reducing HIV incidence: low ART coverage and the need to improve linkage and retention in care, and evidence of reduced condom use. He noted that adolescent girls and young women (15–24 years) account for 31% of all sexually-acquired HIV and require special attention.
The Thembisa results highlighted concern about slow progress in reducing HIV incidence. The model estimates that in the last year there were more than 240 000 new HIV infections in South Africa, which was a reduction of less than 40% from 2010. The UNAIDS target is to reduce annual new infections by 75% between 2010 and 2020. To achieve this, South Africa would need to reduce new infections to fewer than 100 000 by mid-2020, which poses a significant challenge.
The Thembisa results show that that KwaZulu-Natal, the province with the most severe HIV epidemic, succeeded in reducing its annual new HIV infections by 49% from 2010 to 2018. Thembisa also estimates that annual new infections among children declined 55% from 29 000 in 2010 to 13 000 in 2018.
More detailed results and model details are available on the Thembisa website: https://thembisa.org/downloads
Region/country


Feature Story
Positive movement: safety, trust and services for people who inject drugs
28 June 2019
28 June 2019 28 June 2019Most people in the capital city of Belarus become infected with HIV from injecting drugs. As a result, a nongovernmental organization in Minsk and the government have responded with HIV mobile testing clinics, drop-in centres and peer counselling to establish trust with people who often shy away from official health services.
Last year, more than 10 000 people visited the three mobile clinics positioned around the city of Minsk offering HIV testing, care and support services. Of 4000 people tested who inject drugs, more than 500 tested positive for HIV.
Word-of-mouth lets people know the mobile clinics are parked up. Positive Movement, the Minsk-based nongovernmental organization that operates the clinics, also lists their locations on its website. In the van-sized clinics you can get an HIV test, talk to a doctor or simply drink tea and chat with peer counsellors.
Positive Movement staff members have first-hand knowledge of issues affecting their clients. Of the 200 employees working there, more than three quarters have been affected by drug use and/or HIV.
“At first, employees were clients, now they are board members,” says Irina Statkevich, the head of Positive Movement’s board. “We believe that harm reduction works and that we can defeat HIV infection,” she says. "If we decide that this service is needed by our customers, we will do everything to get it!”
Above, Positive Movement’s office
Eight years ago, when she started working at the organization, she explains that it was impossible to utter the words needle and syringe exchange programme. “We had to do things incognito.”
Now they have drop-in centres open all day that not only provide clean needles and syringes but also food, HIV testing and a place to wash as well as legal and medical counselling. Peer-to-peer consultant Julia Stoke likens the centres to safe-havens.
Above, Julia Stoke, peer consultant in Drop-in centre
“This is an island of security,” she says. “A person who uses drugs has a need for safety first, then trust, and then a range of services."
Vyacheslav Samarin agrees. As a social worker at one of the drop-in centres, he explains that people who use drugs often face difficult situations like a loss of housing, a lack of documents, poor health and sometimes nothing to eat and nowhere to sleep. “In many cases,” Mr. Samarin says, “One problem often leads to another.”
Above, Vyacheslav Samarin, a social worker at a drop-in centre in Minsk
“Many are in denial about their health,” he continues. Many clients fear stigma and have different priorities. He says it’s key to support people and not let them feel defeated and abandoned.
“At the very beginning, people do not want to believe their diagnosis, so we are careful to talk to them about starting treatment,” says the red-haired social worker.
Over the years he has noticed changes. "Today there are more treatment methods and the staff listen much more to people living with HIV.” He says that relationships between patients and doctors are much improved.
Also, the government of Belarus has been much more supportive of the work.
Tatiana Migal from the ministry of health confirms this. “By working on HIV prevention among people who use drugs and supporting people living with HIV for nine years, Positive Movement has not only gained considerable experience in this field but has also contributed significantly to reducing HIV infection among people who inject drugs.”
Ms Migal stresses the importance of peer counselling, social support centres and syringe exchange programmes as well as methadone substitution therapy.
“According to estimates by the World Health Organization and UNAIDS harm reduction programmes will help overcome the HIV epidemic in Belarus,” she says.
Related


Feature Story
Pushing for harm reduction success in Burundi
25 June 2019
25 June 2019 25 June 2019This story was first published by WHO
Getting life-saving harm reduction services to people who use drugs in Burundi was the aim of a recent learning trip to Kenya supported by the World Health Organization (WHO). This saw a team of Burundian physicians and health advocates travel to Mombasa County, Kenya, to learn about good practice from one of the pioneers of harm reduction on the African continent.
Led by Burundian non-profit, Jeunesse au Clair Medical (JCM), the team will push for a comprehensive package of harm reduction interventions in Burundi. Like many other countries in Africa, injecting drug use is not often acknowledged, and a public health response therefore not implemented.
Drug use is widely criminalised and stigmatised and its complexities misunderstood. WHO defines harm reduction as an evidence-based public health response that includes the provision of needle and syringe programmes (NSP), opioid substitution therapy (OST) and access to testing and treatment of HIV, tuberculosis (TB) and viral hepatitis B and C.
Keen to gain insight into the Kenyan experience and inform the development of a programme in Burundi, the Burundian team of doctors, a counsellor and a national coordinator of a network of people who used drugs, visited the Reach Out Center Trust in Mombasa. They observed the delivery of OST programmes and learnt about advocacy with local influencers – in an excellent example of south-to-south learning.
Kenya’s response to minimising the adverse effects of drug use, although not without its own challenges, has succeeded largely through grassroots advocacy and on-boarding key influencers – making it easier for harm reduction to be accepted. This multi-level approach includes collaboration between government and civil society, involving both law enforcement and networks of people who use drugs.
At a visit to the Mombasa Inspectorate in charge of drug-related offences, the team learnt first-hand from the Chief Inspector the importance of police engagement, highlighting the negative impact drug use can have on young lives and the need for strategies that work. Today, some 100 police officers in Mombasa are trained on harm reduction with their work focusing on supporting, not punishing.
In addition to police buy-in, identifying other key influencers such as spiritual and village leaders, other government officials, and people who use drugs themselves, can ensure that harm reduction programmes are effective and sustainable.
Advocacy wasn’t the only thing on the agenda, the team from Burundi also saw in practice how the Kenyan clinics functioned, how methadone is dispensed, they spoke with peer educators and outreach officers, and were trained on data collection for programme monitoring. An important learning if they want to show evidence to get government and donors on their side.
While Kenya is several years ahead in its harm reduction journey, with local input, their learnings can be adapted to other contexts.
“The burden caused by drugs requires interventions at grassroots and education must be provided by trained people to avoid misinformation,” said Dr Egide Haragirimana, clinical officer at JCM.
JCM are putting into action their learnings and will next be involving networks of people who use drugs to better understand what their needs are, to inform future harm reduction initiatives.