Feature Story
Osh signs the Paris Declaration
22 August 2019
22 August 2019 22 August 2019Osh, Kyrgyzstan, has become the latest city to sign the Paris Declaration to end the AIDS epidemic in cities, becoming the second city in the country to commit to reaching the 90–90–90 targets by the end of 2020.
“We sign this declaration because we realize that large cities are the engine of HIV,” said Kadyrov Nurbek Suyunbaevich, Deputy Mayor of Osh. “Thanks to effective HIV testing and treatment, we can control the epidemic and people can live a healthy and fulfilling life. The city of Osh is taking steps to end AIDS and we are already allocating funds for HIV prevention.”
“UNAIDS is pleased that Osh has become a Fast-Track city. By signing the Paris Declaration, Osh will also strengthen health systems in the city,” said Meerim Sarybaeva, the UNAIDS Country Manager in Kyrgyzstan.
Osh is one of the oldest cities in central Asia, with a population of almost 300 000 people. It was one of the first places in central Asia to be affected by HIV, owing to the drug trafficking routes that passed through the city. From 2005 to 2007, there was a severe outbreak of nosocomial HIV infections among children in the city. According to government statistics, there are more than 1100 people living with HIV in Osh.
Osh implemented some of the first HIV prevention programs in Kyrgyzstan. The city has expanded its HIV rapid testing programme for people at higher risk of HIV, launched a treatment adherence programme for people living with HIV based on mobile technology and is scaling-up the coverage of opioid substitution therapy.
“This is an important political step, which requires that we mobilize the necessary resources, both human and financial, to ensure effective HIV prevention programmes for all key populations,” said Aybar Sultangaziev, Director of the Partnership Network Association
Since the launch of the Fast-Track cities initiative on 1 December 2014, more than 350 cities and municipalities around the world have signed the Paris Declaration. The declaration offers cities not only tools to end AIDS but also a platform to address social inclusion and public health.
Related information
Region/country
Related




Feature Story
Preparedness, proactiveness and speed are key to tackling humanitarian emergencies
15 August 2019
15 August 2019 15 August 2019When Cyclone Idai hit Mozambique and the eastern part of Zimbabwe in mid-March, it couldn’t have come at a worse time. A month earlier, Zimbabwe had issued an emergency appeal for some 5.3 million people affected by an ongoing economic crisis, and limited rainfall had ruined crops. The sudden pounding rain and wind threw everything into chaos. Three hundred people died, hundreds disappeared and 40 000 lost their homes. Food insecurity plus a lack of basic services, including health care, skyrocketed in the hardest hit province of Manicaland.
For Mumtaz Mia, the UNAIDS Acting Country Director in Zimbabwe at the time, the most pressing issue was to ensure that people living with HIV, including pregnant women enrolled in prevention of mother-to-child transmission of HIV programmes, could access HIV treatment.
“In Zimbabwe, where emergencies are not a new phenomenon, people living with HIV were left stranded when their medicine got washed away,” she said.
For her, preparedness is key. “For the AIDS response, we must anticipate any disruptions to services that emergencies bring.”
Born in Malawi, Ms Mia has dealt with droughts and floods throughout eastern and southern Africa. She also spent some time in Kenya dealing with post-election conflict and worked five years in South Sudan for UNAIDS before her stint in Zimbabwe.
She recounted that the UNAIDS country office met with the government, civil society, donors and other key stakeholders to discuss immediate action. Quickly, they made sure that HIV-specific needs were integrated in the emergency response. That meant coordinating, with UNAIDS Cosponsors, the Ministry of Health and Child Care and the National AIDS Council, to ensure the distribution of antiretroviral therapy and condoms, food support for people living with HIV and safe deliveries for pregnant women. They also set up assessments to address additional health and HIV needs following the disaster.
Almost 150 000 people living with HIV were in the cyclone-affected districts, and about 83% of them were accessing antiretroviral therapy. Most of them experienced a disruption of treatment during the crisis.
“Without a clear plan and instructions on action that needs to be taken in an emergency, precious days and weeks can be wasted trying to figure out what to do,” Ms Mia said.
She also believes that interagency contingency plans with specific tasks assigned to each agency to be taken in the event of an emergency would help action to be taken more quickly. “Using simple and clear guidance on the actions required by UNAIDS in emergency situations and the impact they can have on HIV are critical to guide country offices and managers,” she said, adding that “It’s important to earmark financial resources so that you can access and use the money right away.”
She practises yoga to help cope in times of stress and praises her supportive husband. “We try to have a semblance of a normal life at home during chaotic times,” she said, although she admits that often it is not easy. Throughout, she focuses on the people that needed her help. “I leave my door open, I listen to their stories and that gives me perspective to forge ahead.” That’s why she reiterated that in time of need, you cannot let people down. “Speed is of the essence.”
The UNAIDS Country Director for the Bolivarian Republic of Venezuela, Regina Lopez de Khalek, agrees. “In a humanitarian emergency, you have to act really quick in order to save lives, which means reinventing your everyday tasks to focus solely on the crisis,” she said.
In her case, she is dealing with the impact on people living or affected with HIV, of a political and economic crisis that affects more than 80% of the population. Inflation in the Bolivarian Republic of Venezuela has exploded, making basic food items beyond reach. Shortages have plagued the country, and medicine is no exception. Since May 2019, the country has recognized that there are some “humanitarian needs”, facilitating the delivery of medicine and rapid HIV and syphilis tests. With the help of international nongovernmental organizations, almost 60 tonnes of life-saving medicine have been delivered to the country. UNAIDS also worked for the country to receive emergency funds from partner organisations.
More recently, UNAIDS, the United Nations Population Fund and the Office of the United Nations High Commissioner for Refugees have jointly focused efforts to help people affected by stigma, discrimination and sexual violence. This included distributing post-exposure preventive kits, an emergency medical response for people exposed to HIV, to health services and introducing HIV tests to maternity units, as well as supporting civil society.
For Ms Lopez de Khalek, working jointly with other United Nations agencies and partners on the ground makes all the difference. “Not only does working hand in hand make sense, but it allows the AIDS response to stay relevant in a humanitarian situation,” she explained.
She recommends following the Inter-Agency Standing Committee HIV Task Force in Humanitarian Settings guidelines, but not to overlook the local and national context. “Know and understand the situation of the country you are in,” she said, “because although emergencies may seem equal, each crisis takes on the particularities of the country in which they occur.” And be proactive. “Act accordingly in advance, so that you are not just reacting,” she said. In her mind, it’s key to set up relationships, collaborate and engage with others and build a comprehensive response so that in the event of an emergency you and the people you are there to help are not left behind.
Simone Salem echoes that sentiment. “The key asset that helped me to respond to emergencies has always been the number of contacts I had across the countries as well as good relations with key people who were able to help,” the UNAIDS Community Mobilization Adviser in the Middle East and North Africa region said.
She added that when you start acting and giving concrete help, people will trust you and seek your support.
Ms Salem describes her work in Iraq, Libya and the Syrian Arab Republic as life-changing. “With each person I help, I realize the importance of my job and how crucial it is to always be alert to people’s needs,” the Egyptian said.
Recently, she helped people migrating or fleeing their homes to access HIV treatment and counselling. With the help of activists and regional networks, she supported the evacuation of lesbian, gay, bisexual and transgender (LGBT) people who had been targets of violence.
In times of crisis, she admires the solidarity that sprouts up at all levels. For example, Tunisians recently offered to give surplus HIV treatment to Libyans. The same occurred at the height of the Syrian conflict, with Lebanese people donating medicine.
Over time, she has become a much better decision-maker. Her secret? “Listen to what is said and also what is not being said, when analysing complex situations,” Ms Salem explained.
In her mind, it’s not a question of gender but of personality, although she said that women and vulnerable people she worked with came to her because they felt that she may be more supportive. The only regret she has is when she cannot help someone. “That’s very hard.”
Using her heart is how she explained she listened to people. When young LGBT people came to her saying that her comforting words had given them hope, she was touched.
“That was so precious to me and really keeps me going," Ms Salem said. “I push and push so that people are treated fairly and with compassion.”
Related




Feature Story
Preventing HIV and sexual and gender-based violence in peacekeeping and humanitarian operations
15 August 2019
15 August 2019 15 August 2019In Africa alone, there are currently seven peacekeeping operations and a large number of other humanitarian operations. Across the continent, 600 million people live in countries affected by fragility, conflict and violence and seven out of 10 women in conflict settings and in refugee populations are exposed to sexual and gender-based violence. In certain contexts, women who have experienced violence are 50% more likely to be living with HIV.
Uniformed personnel working in peacekeeping operations are routinely exposed to a range of health risks during their work, owing to the type of work they do, the locations they are sent to and the conditions in which they often have to serve. The health and welfare of uniformed personnel is therefore a matter of concern. Of equal importance, however, is the well-being of the people among whom the uniformed personnel work.
In order to protect both deployed personnel and civilians, a new code of conduct on preventing and reporting sexual and gender-based violence, including among peacekeeping operations, was drawn up by the African Union in November 2018.
“We urgently need a more overarching, concerted and harmonized strategy to tackle the issues of sexual and gender-based violence and HIV during conflicts and in humanitarian settings,” said Bineta Diop, the African Union Special Envoy for Women, Peace and Security.
The new code of conduct, outlined in the African Union policy on the prevention of and response to sexual exploitation and abuse during peacekeeping operations, prioritizes the elimination of all forms of gender-based violence and puts peacekeeping operations at the forefront of ensuring justice and the protection of vulnerable populations. The challenge now is to implement the code of conduct.
“The African Union has zero tolerance for sexual and gender-based violence and calls for the immediate implementation of policies by member states that use a survivor-centred approach and offer the full range of support services,” said Admore Kambudzi, Director of the Peace and Security Department of the African Union Commission.
In June, the African Union Commission and the UNAIDS Liaison Office to the African Union, in collaboration with the United Nations Office to the African Union, convened the first of a series of meetings to formulate practical recommendations for a collective way forward in addressing sexual and gender-based violence and HIV in fragile settings.
The participants agreed that it is essential to develop a survivor-centred approach to conflict-related sexual violence based on developing the resilience of survivors and to provide mental health and psychosocial support. Including men and boys in ending sexual and gender-based violence will be key to success.
The participants also called for the health and well-being of the uniformed personnel of peacekeeping operations to be ensured, both before and during active service. A protocol on integrating HIV programmes in African Union peacekeeping operations will be finalized and a team of experts to map the current situation in crisis-affected countries, to identify gaps and areas of strength and to suggest a way forward to end sexual and gender-based violence and exposure to HIV will be assembled.
“I urge partners to take action to eradicate sexual and gender-based violence and HIV in fragile settings within the context of the African Union theme for 2019, the Year of Refugees, Returnees and Internally Displaced Persons,” said Clémence A. Habi Bare, the Director of the UNAIDS Liaison Office to the African Union.
Related




Feature Story
Redefining HIV prevention messages for young people in Latin America
14 August 2019
14 August 2019 14 August 2019A dozen young people from nine different countries in Latin America came together in July at the 10th International AIDS Society Conference on HIV Science in Mexico City, Mexico, to develop new youth-friendly communications strategy related to HIV prevention for young gay men and other young men having sex with men.
Although the 12 had never met face-to-face before, they had held several virtual meetings to pave the way for the conference, organized by the Latin American HIV-Positive Youth Network (J+LAC), with support from the Pan American Health Organization/World Health Organization (PAHO/WHO), UNAIDS and UNICEF.
Every year in Latin America, an estimated 100 000 people become newly infected with HIV—a number that has not changed over the past decade. In 2018, young people between the ages of 15 and 24 years accounted for one fifth of all new HIV infections in the region. Young gay men and other men who have sex with men, sex workers, transgender people and injecting drug users are particularly affected.
“We need to remind the world that we cannot talk about prevention without young people and make the world realize that we are involved and concerned,” said Kenia Donaire, a Honduran who was born with HIV.
UNAIDS, PAHO/WHO and UNICEF are strong advocates for the involvement of young people not only as beneficiaries of services but also as partners and leaders in the design, development, implementation and monitoring and evaluation of policies and programmes.
“Too often, young people are not at the decision-making tables creating the programmes they need to protect themselves from HIV. You have the potential to set an example on how young people can lead, advocate, create demand and deliver tailored services to end an epidemic that is the second leading cause of death among adolescents. We need new ways to communicate, generate demand and link young people at higher risk of HIV to services,” said Shannon Hader, UNAIDS Deputy Executive Director, Programme.
Young people living with HIV in Latin America have been working together to design an HIV prevention communications strategy for young gay men and other young men having sex with men in the region. In advance of travelling to the conference, they worked together to map existing communications campaigns and initiatives on combination prevention of HIV and other sexually transmitted infections and discussed how to translate complex scientific content into effective key messages for their peers.
“Young men who have sex with men and other vulnerable youth need access to HIV prevention information in a way that makes sense to them,” said Maeve de Mello, regional advisor on HIV prevention at PAHO. “We are very pleased to support this talented group of young people. Their personal experience and voices will better prepare us to address this public health concern in a way that adults alone cannot.”
At the conference they shared their ideas with leading health and communications experts and discussed digital strategies to reach young people with compelling messages on HIV prevention and ending stigma and discrimination.
“Learning about the latest advances and successful experiences in the response to HIV, while being able to learn what goes on from the other side of the screen from digital experts such as YouTube was a really enriching experience,” said Horacio Barreda, one of J+LAC coordinators. “We need a strategy that focuses on the needs and affinities of young gay people, who live their lives in the virtual and off-line worlds.”
“This is a successful start of an important journey through which we believe we will reach Latin American youth in all its diversity.”
The group now plans to bring their strategy and advice to key stakeholders in the response to HIV, including to ministries of health, United Nations agencies, and other partners.
Related


Feature Story
Fear of the unknown
12 August 2019
12 August 2019 12 August 2019When her husband came home with a positive HIV test, Jokapeci Tuberi Cati decided that she wanted to get tested too.
“Fear of the unknown, of the stigma associated with HIV and of rejection were all going through my mind before the test,” she said.
Once she got tested in Lami, Fiji, she sighed and said to herself, “done and dusted.”
But she had a nagging thought that her test would be positive and she started thinking about a coping mechanism. She kept playing over and over the same scenario, with one question: how will she live from this point onward?
“In fact, little happened in reality,” Ms Cati said. She recounted that an experienced doctor treated her with the utmost care when he informed her of her HIV-positive status.
She returned home and decided that she and her husband would bear the diagnosis together as a couple. No one needed to know anything.
With time, Ms Cati learned to cope with her new status and vowed to accept her new life. She now wanted to help people to understand the issue so that they would not go through the same experience.
But first she had to let people know.
“The moment I decided to disclose my HIV status to my family and friends, there was a different magnitude of support,” she said. Thinking back to 20 years ago, she still cannot forget how people reacted with such warmth.
That emboldened her to become much more proactive and share her story with a greater number of throughout the country. She is now a programme manager at the Fiji Network for People Living with HIV. Despite losing her husband, Ms Cati is thankful she found out about her status, because with medication she did not transmit HIV to her children.
“Better to know than not know—the benefits are huge,” she said.
Region/country




Feature Story
The right to disclose your own status
02 August 2019
02 August 2019 02 August 2019At 17, preparing for her baccalaureate, Francine Nganhale was carefree. She followed her classmates out of curiosity to the local hospital in Yaoundé, Cameroon, since they had heard about an HIV awareness campaign with free testing.
“This was my first time getting an HIV test and I had no expectations,” she said.
When the results came back, her test was inconclusive. She retook the test and at the fourth try, her result was positive. “The explanations given to me throughout the process piqued my interest and I became much more motivated to find out more,” she said.
Ms Nganhale felt scared and she admits being clueless about what to do next. A doctor walked her through the process and gave her a lot of information about HIV. It suddenly dawned on her that her three-year old son, who was often sick, had never been tested for HIV. He tested positive and both started treatment.
The hard part for her was telling her mother. She postponed telling her, but she felt more and more isolated. And she recalls hearing negative comments from her extended family about people living with HIV. “I had decided to challenge myself and live a long and healthy life and no one would deter me,” she said. When her mother finally found out, she told others about her daughter’s HIV status. Regardless, Ms Nganhale forged ahead. She holds no grudges, saying that her mother cared for her and her son financially for years.
As a social worker, Ms Nganhale works mainly with people living with HIV, raising awareness and distributing HIV treatment.
Her husband is also a social worker overseeing 106 Cameroonian HIV associations. He can relate to his wife’s experience. Charles Noussi used to be a professional football player in the Maldives. During a routine team medical check-up, all his teammates underwent a battery of tests. The next day, when he showed up for practice, he bumped into the manager, who forbade him to train with the others.
“I had no clue what was going on,” he said. “Meanwhile I slowly realized that most people were hiding something from me.” He wanted to get to the bottom of it and asked to see the medical team responsible for the check-up. That’s when finally someone told him his HIV-positive status.
“I suddenly realized that I was the last to know,” Mr Noussi said. The news only got worse. He had 48 hours to pack up and leave the country. “Do you know how hard it is to abandon a career I loved and lose my good salary all because of my HIV status?” he asked. “It broke my heart and more.”
A sponsor helped him flee to Thailand, where he accessed health services. “So many people were supporting me and reassuring me,” Mr Noussi said. Quickly, he joined an HIV advocacy group. “After a year, I told myself that perhaps I should use my knowledge and return to my home country,” he said. Again, mentalities differed in Cameroon. He faced discrimination and despite being healthy and open about his HIV status, many of his acquaintances and friends abandoned him.
“Thank goodness my mother helped me a lot, not only on a nutritional level, but also socially and psychologically,” he said.
Two decades later, he believes HIV-related stigma has decreased in Cameroon. HIV treatment is free, unlike many years ago, when he paid for everything himself. No doubt about it, he said, knowing your status is crucial.
His wife agrees. “No need to tell someone not to worry—it's normal to worry,” she said. “What's key is reassuring someone that they are in control of their life.”
Related story: A tribute to Charles Domingo Noubissi
Region/country


Feature Story
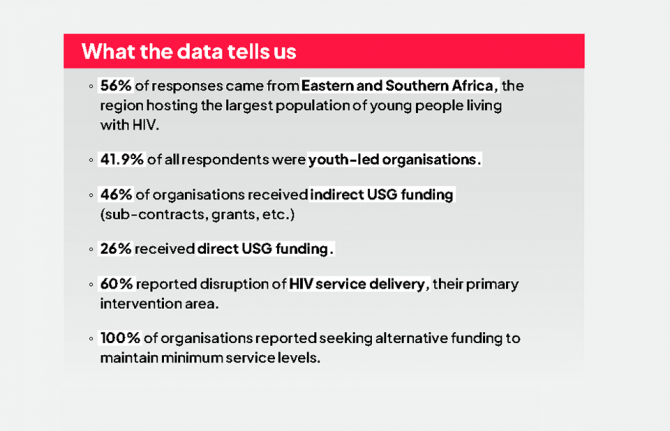
Mapping HIV laws and policies
31 July 2019
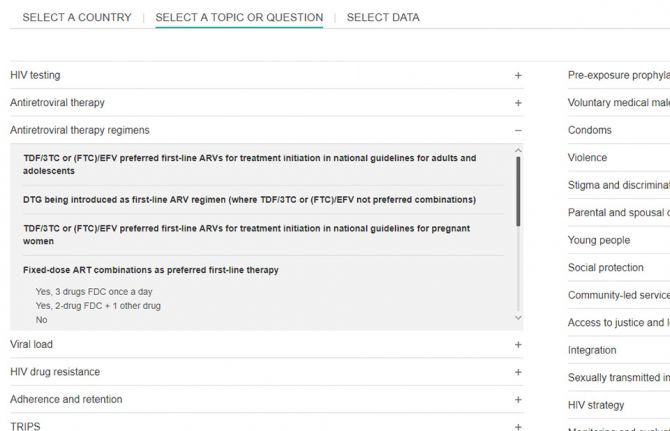
31 July 2019 31 July 2019A new website that enables people to identify national laws and policies related to the AIDS response has been launched by UNAIDS.
Covering areas as diverse as a country’s ability to diagnose HIV among young babies, the existence of laws that discriminate against transgender people and whether people are prosecuted for carrying condoms, the Laws and Policies Analytics website aims to give a full overview of a country’s laws and policies related to the HIV response. It also allows to view policy data jointly with other data on the HIV epidemic and response.
“We must better understand legal and policy environments to drive effective responses to the HIV epidemic. This new tool will provide access to data on national laws and policies and allow for joint analysis with data on the epidemic and response, so that we can drive more deeply-informed decision-making,” said Shannon Hader, UNAIDS Deputy Executive Director, Programme.
Under the 2016 United Nations Political Declaration on HIV and AIDS, countries committed to accelerate efforts to significantly increase the availability of high-quality data on HIV. The information used on the new website was reported since 2017 and most recently in 2019 through the National Commitments and Policy Instrument (NCPI), a part of the Global AIDS Monitoring mechanism through which countries report their progress against the commitments they made in the 2016 Political Declaration.
Data were provided by national authorities, civil society organizations and other nongovernmental partners engaged in the AIDS response. Data on HIV-related laws and policies compiled from other external official documents complement the nationally supplied data. UNAIDS carries out a thorough validation of all policy data included to ensure their accuracy. Data will be updated annually.
The website hosts data from over 140 countries. Users can search by country or region through an interactive map or can select a specific topic.
Through making policy data widely available, UNAIDS seeks to promote transparency and an increased use of policy data in analyses of the HIV epidemic and the response to HIV in countries worldwide.
The Laws and Policies Analytics website can be accessed at lawsandpolicies.unaids.org.
Laws and Policies Analytics website


Feature Story
I’m just a normal teenager living with HIV
29 July 2019
29 July 2019 29 July 2019Aziwe is 19 years old and lives with her mother, Phatiswa, in an informal settlement called Umlazi, near Durban, South Africa. Both women are living with HIV and both are full of energy, love, hope and optimism for the future.
Aziwe didn’t find out she was HIV positive until she was about 14 years old. She had already been on treatment for five years but her mother had decided not to tell her that she was HIV positive, even while making sure that her daughter stayed healthy by taking her medication every day.
When the doctor asked her if she wanted to know why she had to take medicines so regularly, Aziwe did not hesitate. As she had grown older, so had her curiosity. When the doctor told her that she was living with HIV she broke down. Her mother too.
Now, five years later, Aziwe is a happy, confident teenager who is highly articulate as she tells the family story to the UNAIDS Executive Director a.i. Gunilla Carlsson ahead of the launch of UNAIDS global report on the state of the AIDS epidemic.
Phatiswa lived in the Eastern Cape in 1999 but, like many women, left to find work as a domestic worker in Durban. She’s good at her job and has been working for the same family for 19 years.
The children stayed behind in the Eastern Cape at first. But Aziwe was a sickly child and came to live with her mother a few years later. In 2009, she became very ill and was rushed to hospital where she would remain for 2 weeks. It was there that she was tested for HIV and found to be positive. Phatiswa also tested positive for the virus.
Today, the women take their treatment and encourage others at community support groups to keep taking their medicines so that they stay well. Aziwe also challenges the stigma and discrimination that still surround HIV and has spoken about living with HIV at a church group. She says there is still too much ignorance about the virus and it sometimes upsets her. But she and Phatiswa support each other.
“I have days where I just want to cry but she speaks to me as a mother. I have good family and friends who are always there for me.”
Aziwe explains that she values life so much more because she has lost loved ones to AIDS.
“I want to live because there are so many things that I want to achieve in life—for my mother and for myself.”
Like many young people, she wants to travel and later to work as a talk-show host on television. In the future, she wants to have a family of her own.
“I’m just a normal teenager living with HIV,” she explains.
Region/country






Feature Story
Botswana puts young people at the centre of its AIDS response
25 July 2019
25 July 2019 25 July 2019While Botswana has made great progress in reducing the number of new HIV infections—down around 36% in total since 2010—young people remain highly vulnerable to the virus. Adolescent girls and young women are particularly at risk of HIV infection as well as other sexually transmitted infections and unintended pregnancy.
In 2018, almost one in four new HIV infections in Botswana occurred among young women and adolescent girls aged 15-24 years old. Less than half of young women and adolescent girls say they have comprehensive knowledge about HIV.
To see what more can be done to address the issues making young people more vulnerable to HIV, the First Lady of Botswana, Neo Masisi, held a retreat in July to look at the challenges confronting them.
Young women participating in the retreat shared some of their experiences with the First Lady and officials from the Ministry of Health.
“I come from a strained family structure where poverty is rife. I never felt loved at home and looked for love outside. I got a boyfriend and eventually I too became a teenage mother,” said Belinda.
The discussions at the retreat will feed into a framework for the development of a national flagship programme for young people.
“Today’s young people are dealing with multiple challenges and they have to take on so much—at school, within changing family dynamics, societal expectations. They question their norms, values and their own worth,” said Ms Masisi. “We need to treat them as leaders so that they can feel valued.”
The Minister of Health, Alfred Madigele, said further consultations would be held with young people to produce the framework.
Earlier this year, the UNAIDS Executive Director a.i., Gunilla Carlsson, appointed Ms Masisi as UNAIDS Special Ambassador for the empowerment and engagement of young people in Botswana.
Region/country
Related


Feature Story
Empowering women living with HIV in Djibouti to live dignified lives
25 July 2019
25 July 2019 25 July 2019Zarah Ali (not her real name) remembers how things changed for the better. “In 2014, I received a loan of 40 000 Djiboutian francs (US$ 250) that I used to develop and improve my garment business. I was also trained in business entrepreneurship, including marketing and customer satisfaction. I import clothes from Dubai and Somaliland and earn a decent income that helps me support my 25-year-old son, my 16-year-old daughter in secondary school and my three-year-old adopted son. I am able to pay for my rent, electricity and water and have decent meals.”
Ms Ali’s loan came from an income-generation programme established by the World Food Programme in collaboration with the United Nations Development Programme, UNAIDS and the national network of people living with HIV in Djibouti (RNDP+). The programme supports the long-term empowerment of, and provides regular incomes to, women living with HIV in Djibouti City. It helps them to achieve financial security and have access to food and improves their access to health-care services. Income-generating activities such as those supported by the programme have a powerful potential to help people living with HIV adhere to antiretroviral therapy and optimize health outcomes.
The loans, ranging from US$ 141 to US$ 438 per person, are for starting or building retail businesses. The beneficiaries, who are selected from among two networks of people living with HIV affiliated to RNDP+ (ARREY and Oui à la Vie – Yes to Life), also receive training on how to run their business. Government support in the form of favourable policies and legislation has been vital to the success of the programme.
Dekah Mohammed (not her real name) now lives a fulfilling life after receiving help from the income-generation programme. Ms Mohammed, who lost her husband to AIDS, lives with six children. After she lost her job in the hospitality sector owing to her deteriorating health and to stigma and discrimination, she started her own clothing business and received a loan of 50 000 Djiboutian francs (US$ 313) to expand her business. The loan was repaid within 10 months. Her business has since expanded into furniture and electronics and she has recruited an employee. “I am no longer a desperate woman. I make enough to take care of my family and dependants,” she said.
The programme has improved the quality of life of many Djiboutian women, allowing them to regain dignity and ensure their financial security. It empowers women and girls to protect themselves from HIV, make decisions about their health, live free from violence and be financially independent.
Building on the belief that empowering women living with HIV and their households to be financially independent strengthens adherence to treatment and leads to more fulfilling and dignified lives, the programme contributes to the World Food Programme’s broader strategic contribution towards ending AIDS as a public health threat by 2030.