Update
Parental consent laws leave adolescents vulnerable to HIV
14 February 2022
14 February 2022 14 February 2022Sexual activity often starts during adolescence. Many countries have age of consent laws in relation to sexual activity that are inconsistent with minimum age laws for accessing sexual and reproductive health information and services without parental permission. This means that adolescents may legally have sex before they can legally access any information or services relating to safer sex practices or contraception, leaving them at greater risk of HIV, other sexually transmitted infections (STIs) and unwanted pregnancy.
The removal of laws that require parental permission to access services for sexual and reproductive health and HIV prevention, testing and treatment has been shown to improve health-seeking behaviours. That effect is even stronger when schools can provide age-appropriate comprehensive sexuality education to young people so they can protect themselves from HIV, STIs, unwanted pregnancy and gender-based and sexual violence.
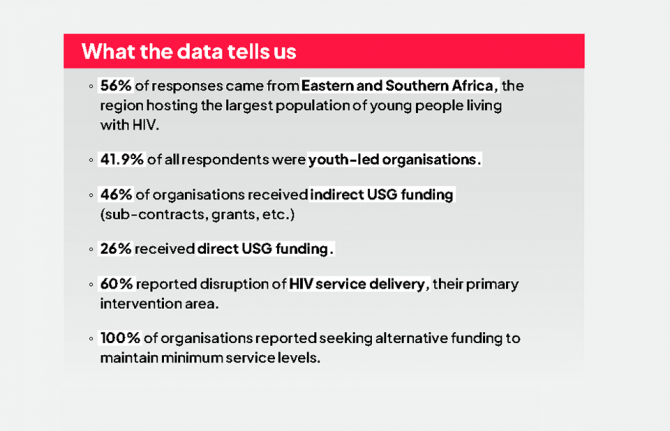
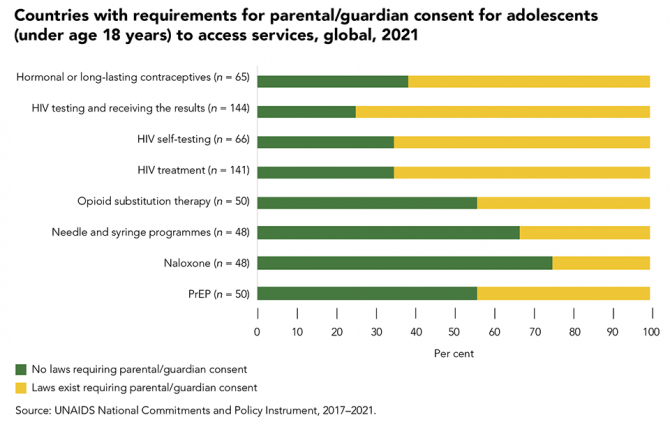
Forty countries reported to UNAIDS in 2021 that they have laws requiring parental/guardian consent for adolescents to access hormonal or long-lasting contraceptives, 108 reported that this consent is required for an HIV test, 43 for HIV self-testing, 92 for HIV treatment and 22 for PrEP. Among these countries, some provide exceptions based on demonstrated maturity: 10 for hormonal or long-lasting contraceptives, 15 for HIV testing, eight for self-testing and nine for HIV treatment. The age cut-off of parental consent laws varied by service. The majority of countries that reported having requirements for parental/guardian consent had an age cut-off of 18 years, with exceptions in a few countries where adolescents as young as 14 years could access a service without parental/guardian consent, which varied by service.
Our work
Related
 “Who will protect our young people?”
“Who will protect our young people?”

02 June 2025

Update
Experience of childhood violence is high
07 February 2022
07 February 2022 07 February 2022Experiences of violence too often occur early in life. Violence in childhood has been linked to increased risks of: HIV and other sexually transmitted infections; mental health problems; delayed cognitive development; poor school performance and dropout; early pregnancy; reproductive health problems; communicable and noncommunicable diseases; and injury.
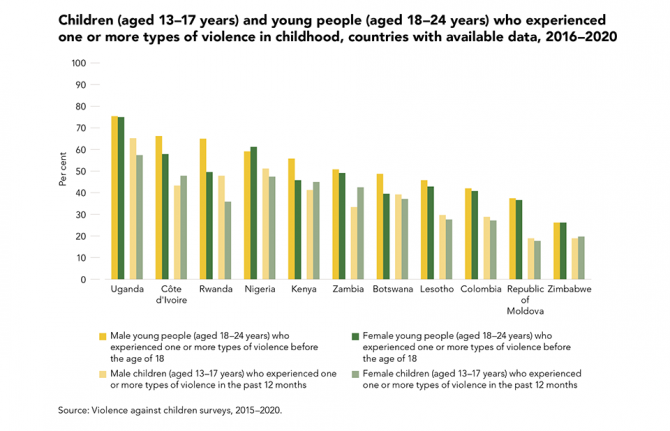
Among the 11 countries with available data between 2016 and 2020, violence (physical, sexual and/or emotional) experienced within the past 12 months by children (aged 13 to 17 years) ranged from 19.2% in the Republic of Moldova and Zimbabwe to 65.4% in Uganda among males, and from 17.7% in the Republic of Moldova to 57.5% in Uganda among females.
The percentage of young people (aged 18 to 24 years) who experienced one or more types of violence during childhood (before the age of 18) is high across all 11 countries with available data between 2016 and 2020, ranging from 26.3% in Zimbabwe to 75.6% in Uganda among males, and from 26.5% in Zimbabwe to 75.3% in Uganda among females.
Related
 “Who will protect our young people?”
“Who will protect our young people?”

02 June 2025


Update
One hundred and fifty thousand preventable new HIV infections among children in 2020
31 January 2022
31 January 2022 31 January 2022Most of the 150 000 new HIV infections among children in 2020 could have been prevented. A strong start would be to better engage women and girls at significant risk of acquiring HIV infection in integrated antenatal care and HIV services, including HIV prevention and testing, delivered at the local level, and to ensure that those who are HIV-positive receive treatment before pregnancy. Nearly 65 000 child infections occurred in 2020 because women already living with HIV were not diagnosed during pregnancy and did not start treatment.
More than 35 000 additional child infections occurred because women acquired HIV during pregnancy or breastfeeding, which led to a spike in their viral load and a high risk of vertical transmission. Women at substantial risk of HIV infection require tailored combination HIV prevention, including pre-exposure prophylaxis, more comprehensive counselling, repeat HIV testing and the provision of self-testing kits for partners.
More than 38 000 additional child infections occurred when mothers who started antiretroviral therapy did not continue treatment during pregnancy and breastfeeding, and nearly 14 000 occurred among women who were on treatment but not virally suppressed. Improving the quality of treatment and care—including the use of optimized treatment regimens and peer-assisted retention efforts (such as mentor mothers)—can help close these gaps.
Our work


Update
Missing men living with HIV
24 January 2022
24 January 2022 24 January 2022Globally, the testing and treatment targets for 2020 were almost reached among adult women (15 years and older) living with HIV. Men living with HIV, however, are consistently faring worse than women across the HIV testing and treatment continuum. Compared to women living with HIV, there are 740 000 more men living with HIV who do not know their HIV status, 1.3 million more men who are not on treatment and 920 000 more men who are not virally suppressed.
While gender norms that prize male strength and stoicism may partly explain why many men delay seeking care, other factors are also at play. Primary health-care services in eastern and southern Africa place a great deal of focus on women of reproductive age, and reproductive, maternal and child health services offer ideal entry points for HIV services; similar entry points for men are not commonplace. Interventions to reach and include men more successfully in HIV testing and treatment services are increasing—including through workplace-based interventions and greater use of self-testing approaches, and by providing services at outpatient departments—but a more finely-tuned understanding of why men's use of HIV services continues to lag can help shape additional ways to close this gap.
Our work
Related

Update
Pre-exposure prophylaxis use expands, but not fast enough
17 January 2022
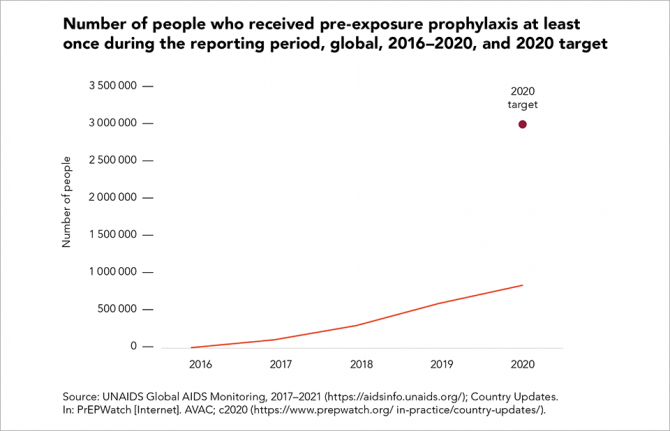
17 January 2022 17 January 2022It has been more than a decade since the first evidence of the efficacy of daily oral pre-exposure prophylaxis (PrEP) was published. PrEP is now a valuable additional option for people who are at higher risk of acquiring HIV, and its global uptake has continued to increase, despite the COVID-19 pandemic: country data show that approximately 845 000 people in at least 54 countries received PrEP in 2020—a 43% increase since 2019, and a 182% increase since 2018.
Much of the PrEP scale-up is still highly concentrated in a fairly small number of countries, notably the United States of America, and in eastern and southern Africa, where Kenya and South Africa accounted for 158 630 (19%) of people who received PrEP at least once during 2020 in the region.
There continue to be substantial gaps in the availability of PrEP, however: the total number of people using this prevention option in 2020 was just 28% of the target of 3 million in low- and middle-income countries, which represents only 8% of the new global 2025 target.
Our work

Update
COVID-19 hit treatment take-up, but 28.2 million people living with HIV now on treatment
06 December 2021
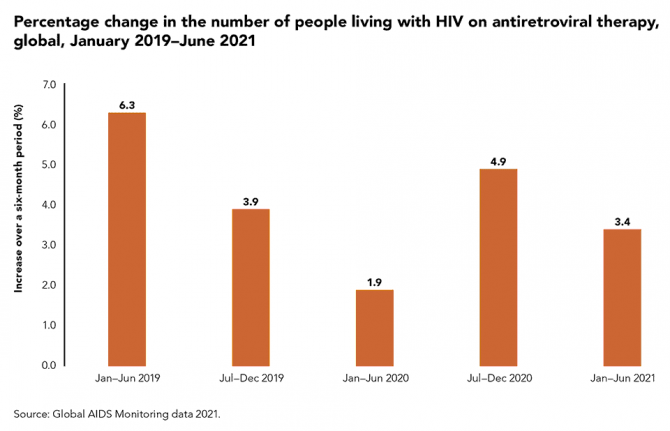
06 December 2021 06 December 2021There have been substantial setbacks in the HIV response during the COVID-19 pandemic, particularly when many countries were in their first lockdowns and HIV programmes were scrambling to adapt, but there have also been many inspiring examples of adaptation and resilience.
The number of people living with HIV receiving antiretroviral therapy increased by just 1.9% between January and June 2020, from 25.5 million people to 26.0 million people. This was followed by an accelerated 4.9% increase from July 2020 to December 2020, reaching 27.3 million people, and then a 3.4% increase during the first six months of 2021. At the end of June 2021, there were 28.2 million people living with HIV on treatment globally.
Our work
Related


Update
Letter from Prince Harry to Dr Tedros Adhanom Ghebreyesus and Ms Winnie Byanyima on World AIDS Day
01 December 2021
01 December 2021 01 December 2021By Prince Harry, The Duke of Sussex Founding Patron, Sentebale
On this World AIDS Day we recognise the 40 years that have shaped life for many. We honour those whose lives have been cut short and reaffirm our commitment to a scientific community that has worked tirelessly against this disease. My mother would be deeply grateful for everything you stand for and have accomplished. We all share that gratitude, so thank you.
It is striking to now see the world’s leading AIDS activists are also leading the call for COVID-19 vaccine equity. Vaccinating the world is a test of our moral character and we are experiencing a spectacular failure when it comes to global vaccine equity. Similar to the AIDS crisis, we’ve yet again revealed over the past year, that the value of life depends on whether you were born and/or live in a rich nation, or a developing country.
We’ve known for some time (thanks to medical experts) that if we are unable to meet agreed targets to vaccinate 40% of every country’s population by the end of the year, and 70% by next September, potentially more dangerous COVID-19 variants are likely to arise. Yet, here we are.
While it’s too early to know the full extent of the risk that the Omicron variant poses, which we only know about thanks to the experts in Southern Africa identifying it, there is no doubt that its emergence is of deep concern. Now more than ever, the voiceless majority of the world needs to be heard, and the onus is on our leaders to end this pandemic. Anything less is self-defeating.
That means breaking pharma monopolies that prevent vaccines from getting to communities around the world in need; that means Governments honoring their promises and delivering the doses that they committed; that means pursuing international pandemic agreements with strict timelines and holding each other accountable to them; that means treating all human lives as equal lives.
It’s time to draw from the lessons we learned throughout the HIV/AIDS pandemic, where millions died unnecessarily due to deep inequities in access to treatment. Are we really comfortable repeating the failures of the past? Everything I’ve learnt, from the youth of Sentebale, tells me not. They see how repeating these mistakes is destructive and self- defeating, it is a betrayal of the next generation.
Let’s spend today celebrating and building on the work of champions who turned what was once a death sentence into a manageable condition. Let’s spend tomorrow continuing our efforts to save lives and make a difference.

Update
Key population participation in HIV decision-making varies
13 December 2021
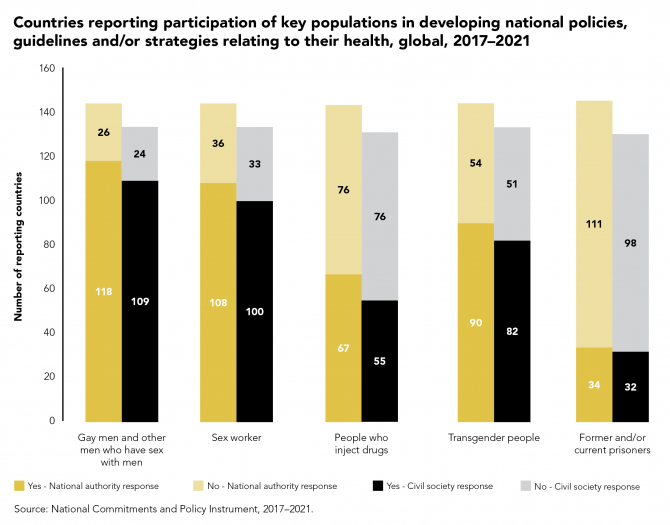
13 December 2021 13 December 2021Today, the active participation of community-led organizations in the governance, planning and implementation of national HIV responses is the rule in many countries.
Members of key populations sit on national AIDS councils and the Global Fund to Fight AIDS, Tuberculosis and Malaria Country Coordinating Mechanisms. Sex workers, transgender people and gay men and other men who have sex with men are engaged in the development of national policies, guidelines and strategies related to their health in the majority of countries that have reported to UNAIDS in recent years. The engagement of other key populations—people who inject drugs and people currently or formerly in prison—is less common.
Our work

Update
Condoms are a critical part of combination prevention
22 November 2021
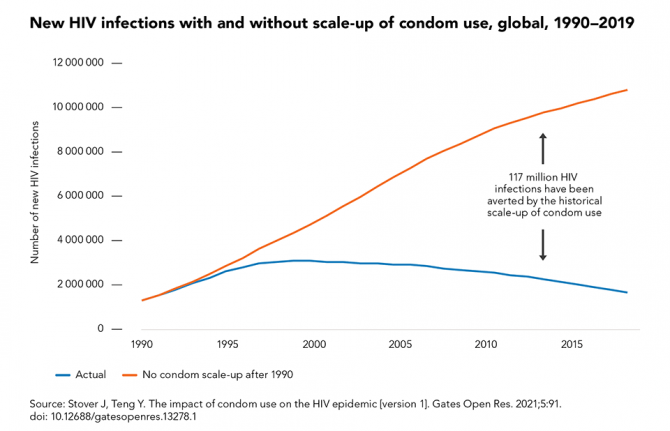
22 November 2021 22 November 2021When used correctly and consistently, male and female condoms and lubricant offer very high protection against HIV, sexually transmitted infections and unintended pregnancy. Condom use has had an enormous impact on the global AIDS pandemic: model simulations show that increased condom use since 1990 has averted an estimated 117 million new HIV infections, close to half (47%) of them in sub-Saharan Africa and more than one third (37%) in Asia and the Pacific.
If condom use rates are increased to reach 95% coverage of higher-risk sex acts by 2025 and all other prevention interventions remain at 2019 coverage levels, about one third of the required reductions in new HIV infections will be achieved. Consistent condom use, although possible, has proved difficult to achieve among all populations. Women in many countries, for example, need greater agency and support to negotiate consistent condom use. Where available, some people also choose other HIV prevention methods. Condoms alone, therefore, are not sufficient to control HIV epidemics. Full achievement of the 2025 prevention target of reducing annual new HIV infections to under 370 000 requires increased investment in combination HIV prevention to ensure access to and use of condoms as well as the full range of other prevention choices for 95% of people at risk of HIV infection.
Our work

Update
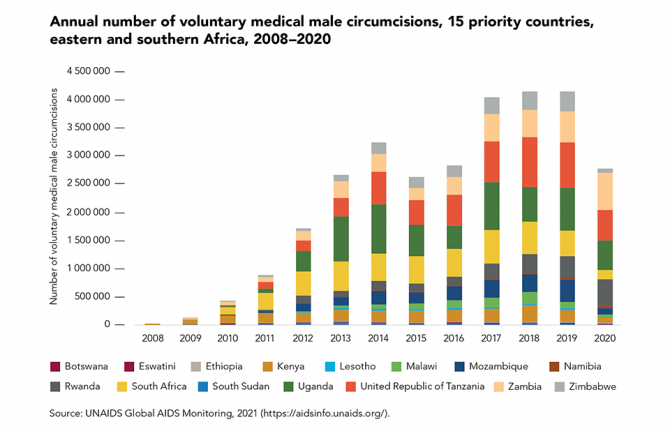
Male circumcisions disrupted by COVID-19, fall short of the 2020 target
29 November 2021
29 November 2021 29 November 2021In areas with high HIV prevalence and low rates of male circumcision, voluntary medical male circumcision (VMMC) can greatly contribute to HIV prevention. Despite this, there was a steep drop in the number of VMMCs performed in the 15 priority countries in 2020, due mainly to service disruptions caused by the COVID-19 pandemic: approximately 2.8 million procedures were performed in 2020, compared with 4.1 million in 2019.
Several countries suspended their programmes when the pandemic took hold, including South Africa. Despite this, programmes in some countries proved resilient enough to recover quickly and expand during the rest of 2020—notably in Rwanda and Zambia, where programme coverage grew by about 15%. In these countries, adjustments for the safe continuation of VMMC services during COVID-19 included changes in promotion and demand generation, client transportation, service delivery at a health facility or in the community and post-procedure follow-up appointments.
A total of about 18 million VMMCs were performed in 2016–2020, far shy of the 2020 target of 25 million. As well as COVID-19, an additional setback in 2015 and 2016 was the detection of tetanus cases in Uganda, which led to activities being scaled back in that country.