Update
Race affecting HIV service provision in the United States of America
15 November 2021
15 November 2021 15 November 2021HIV service disparities by race have been documented in several parts of the developed world.
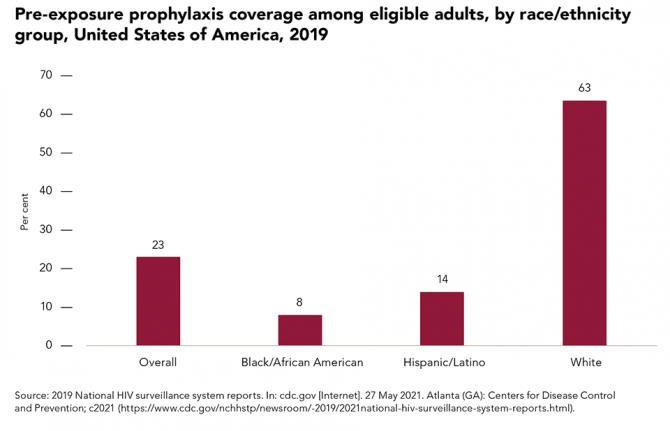
In the United States of America, black people account for a disproportionately large percentage of new HIV infections in the country: 41% in 2019, although they represent only about 13% of the national population. This is in part due to lower coverage of HIV prevention services. Just 8% of black Americans and 14% of Hispanics/Latinos who were eligible for pre-exposure prophylaxis were prescribed it, compared to 63% of whites.
Studies also report significant racial disparities in HIV treatment outcomes, with delayed initiation of treatment and care, lower adherence to antiretroviral therapy, increased stigma and discrimination, mistrust of or lack of access to health-care providers and inadequate access to health insurance among the contributing factors. Many of these gaps are among black and Latino gay men and other men who have sex with men, who must contend with both racial inequalities and homophobia.

Update
Retention in care a growing concern
08 November 2021
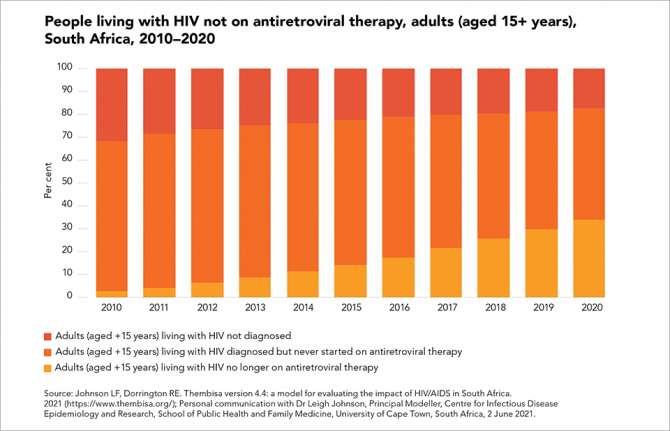
08 November 2021 08 November 2021Data from South Africa highlight the challenge faced by many treatment programmes when it comes to successfully retaining people in HIV care.
The HIV treatment programme in South Africa reaches more people living with HIV than any other in the world, with more than 5 million adults (aged 15 years and older) receiving antiretroviral therapy in 2020. Among the 2.5 million adults living with HIV in South Africa who are not on treatment, a steadily increasing percentage are people who had started treatment but are no longer receiving it.
Efforts to support people on treatment to maintain treatment and achieve durable viral suppression are critical to improving health outcomes, maximizing the preventive benefits of treatment and preventing the emergence of drug-resistant strains of HIV. The World Health Organization recently updated its HIV treatment guidelines with a new recommendation to trace people who have disengaged from care and provide support for re-engagement.

Update
Harm reduction services reduce new HIV infections
01 November 2021
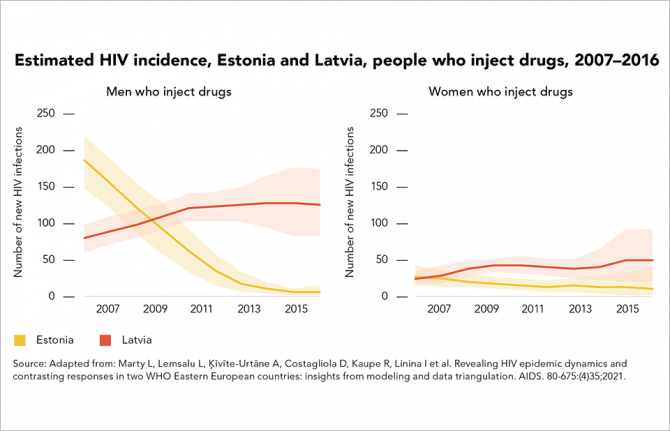
01 November 2021 01 November 2021The neighbouring Baltic states of Estonia and Latvia offer starkly contrasting examples of how different public health approaches affect HIV epidemics among people who inject drugs. In the early 2000s, the two countries had among the highest rates of HIV diagnosis in Europe. As was the case for many European countries at that time, the sharing of non-sterile injecting equipment among drug users was fuelling their HIV epidemics.
The two epidemics began to diverge in the mid-2000s. According to the HERMETIC study, new HIV infections in Estonia declined by 61% countrywide and by 97% among men who inject drugs between 2007 and 2016.
Latvia’s HIV epidemic followed a different trajectory. The HERMETIC study highlights that, between 2007 and 2016, new HIV infections increased by 72% overall. By 2016, overall HIV incidence in Latvia was almost double that in Estonia (35 cases per 100 000 people versus 19 cases per 100 000).
Both epidemics centred largely on the sharing of injecting equipment by people who inject drugs, and probably on unprotected sex between people who inject drugs and their sexual partners. The HERMETIC study concludes that the main difference between the two epidemics lay in the availability of harm reduction services.
Needle–syringe programmes had been operating in Latvia since 1997, but on a very limited scale. As late as 2016, Latvia was distributing about 93 needle–syringes per drug user per year; neighbouring Estonia was distributing 230 per user per year. Both countries expanded access to opioid substitution therapy, which is proven to reduce drug injecting and HIV transmission, and improved HIV testing and antiretroviral therapy services for people who inject drugs. Although access to opioid substitution therapy remained limited in both countries, it was higher in Estonia than in Latvia.
The HERMETIC study’s results indicate that by 2016, about half the people who inject drugs in Estonia were taking HIV tests in a 12-month period—and three quarters of those who tested HIV-positive were on antiretroviral therapy. In Latvia, meanwhile, about 10% of people who inject drugs took an HIV test in any given year between 2007 and 2016, and only 27% of those living with HIV were on antiretroviral therapy. Slow adoption of international HIV treatment guidelines contributed to the low treatment coverage in Latvia.
Related




Update
Regional HIV summit aims to reinforce HIV response in Western and Central Africa
01 November 2021
01 November 2021 01 November 2021Delegations from 26 countries including 16 government ministers and representatives from civil society from the West and Central African region have formally opened the regional HIV summit, co-organized by UNAIDS and the Civil Society Institute of HIV and Health in West and Central Africa.
Following the welcome speeches, participants ranging from the heads of National AIDS councils to donors, the Global Fund and UNAIDS as well as their co-sponsors, began addressing the lagging HIV response in the region and how to overcome such setbacks.
The Western and Central Africa region represents only 8% of the world’s population but is home to more than 12% of all people living with HIV globally. In addition, 1 in 3 new HIV infections among children occur in this region with only 35% of children on treatment (vs 77% of adults.)
For Daouda Diouf, Executive Director of the Civil Society Institute of HIV and Health in West and Central Africa based in Dakar, a reset button must be activated to get HIV back on the agenda and further empower civil society.
“Our main expectation from the summit is to have civil society officially recognized as a key contributor in the countries within the official health systems and unofficial ones that the community health workers and civil society so aptly support,” he said.
Mr Diouf wants civil society to be on a more equal footing in the region and stressed that when community health workers, peer educators and civil society are involved, countries tend to have better health outcomes.
UNAIDS Fast Track Director a.i. Fodé Simaga agrees. Citing the fact that more than 65% of the new HIV infections in the region are among key populations and their partners, he believes civil society plays a crucial role with a specific added value.
“Considering the statistics, we rely on civil society and their networks to find people at risk of HIV, and reach out to them,” he said. He added that what is needed now is to reinforce their capacities.
“We can no longer consider civil society low-cost, ad-hoc health providers, they are an integral part of the healthcare systems that now need to be fully funded and supported,” Mr Simaga said.
Aside from advocating for civil society, a main session will focus on governments increasing domestic funding in the HIV response and another will be on the Education Plus initiative that stresses the importance of keeping girls and young women in secondary school. Additional break-out sessions will focus on HIV policies such as where and how to best distribute anti-retroviral pills, multi-month dispensing of medicine, prevention and combating stigma and discrimination.
The President of Senegal, Macky Sall, will close the three-day summit with a call to action from governments and civil society to close the gaps in the region’s HIV response.

Update
Financial shortfalls hold back the HIV response in western and central Africa
25 October 2021
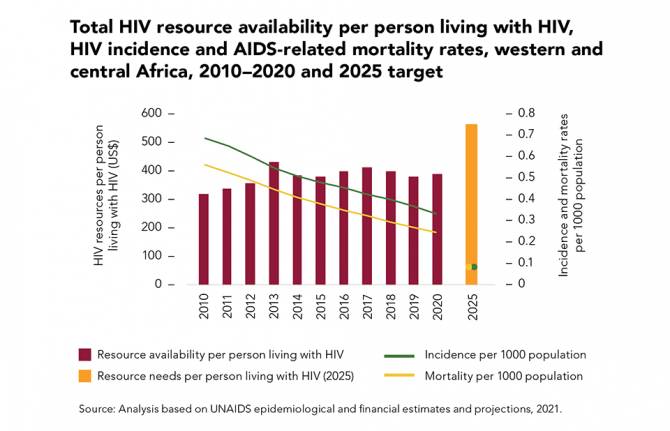
25 October 2021 25 October 2021Underinvestment in the HIV responses of low- and middle-income countries was a major reason why the global targets for 2020 were missed. Financial resource availability during the past five years was consistently below the resources needed, and in 2020 it was 29% less than the US$ 26 billion target for that year (in constant 2016 US dollars).
In western and central Africa, large resource shortfalls and continued reliance on out-of-pocket expenditures (such as user fees for health services) are associated with more modest declines in the incidence of HIV infection and the rate of AIDS-related mortality compared to eastern and southern Africa, where a combination of domestic and international investments has fuelled the rapid expansion of HIV prevention, testing and treatment in areas with a high burden of HIV, resulting in strong and steady reductions in the rate of HIV infections and AIDS-related mortality.
Our work


Update
Upper-middle-income countries pay more for HIV medicines, but price reductions can be achieved
18 October 2021
18 October 2021 18 October 2021The cost of antiretroviral medicines has a major effect on resource needs for HIV responses. Currently, the average prices for first- and second-line antiretroviral therapy are broadly similar in low- and lower-middle-income countries, but are substantially higher in upper-middle-income countries.
For example, countries in eastern Europe and central Asia and in Latin America tend to pay considerably higher prices for antiretroviral medicines compared with countries in other regions. Further price reductions for antiretroviral medicines and other key HIV commodities can be achieved through the strategic use of flexibilities under the Agreement on Trade-Related Aspects of Intellectual Property Rights (TRIPS) and by rearranging procurement and supply management systems to take advantage of economies of scale. If these and other cost savings are made, a 17% increase in resources for HIV testing and treatment can result in a 35% increase in the number of people receiving treatment by 2025—enough to reach the 95–95–95 testing and treatment targets.
Our work
Related

Update
People living with HIV at higher risk of COVID-19 illness but have lower access to COVID-19 vaccines
11 October 2021
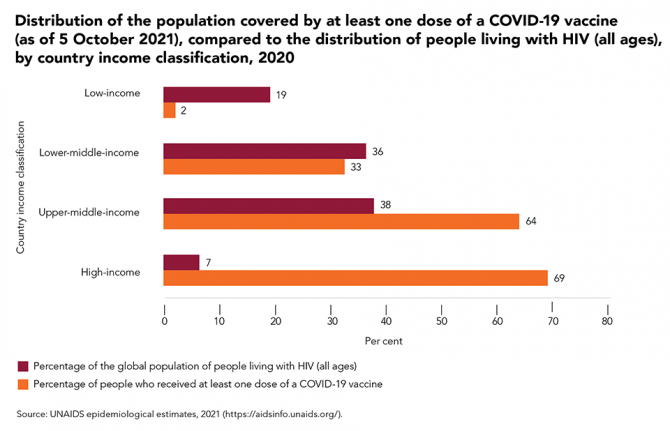
11 October 2021 11 October 2021An increasing body of evidence indicates that people living with HIV who acquire SARS-CoV-2 infection are at heightened risk of requiring hospitalization and having poor clinical outcomes.
Data from the United States of America show that people living with HIV who acquired SARS-CoV-2 infection were much more likely to require hospitalization and suffer severe illness than people who were HIV-negative, while studies from England and South Africa have found that the risk of dying from COVID-19 among people with HIV was double that of the general population. Advanced HIV disease and/or the presence of chronic comorbidities—which tend to be common in people living with HIV—appear to be strongly associated with poor COVID-19 outcomes in people living with HIV.
However, access to COVID-19 vaccines around the world remains exceedingly unequal and unjust. At the beginning of October 2021, there were still low levels of access to vaccines in the low-income and lower-middle-income countries that are home to more than half (55%) of people living with HIV globally.
Our work

Update
Slow progress on AIDS-related deaths among adolescents
04 October 2021
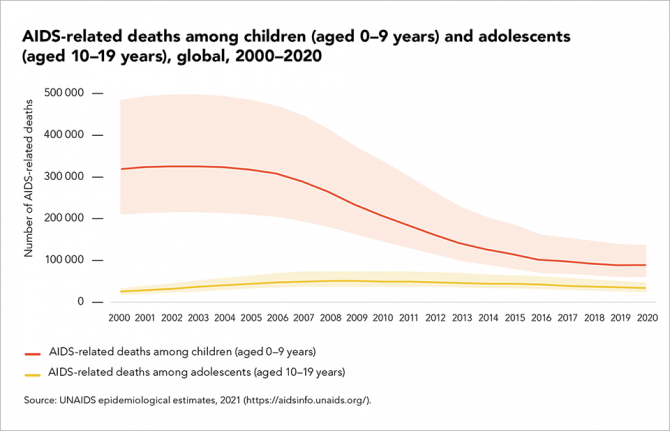
04 October 2021 04 October 2021Current inequalities in HIV testing and treatment for children living with HIV and trends in historical coverage of services to prevent vertical (mother-to-child) transmission of HIV are driving year-on-year trends in AIDS-related mortality.
Reductions in AIDS-related deaths among children and adolescents are steepest among children aged 0 to 9 years (a 60% decline since 2010), reflecting both improvement in efforts to prevent new vertical infections and efforts to diagnose and treat children in the months following childbirth and during breastfeeding.
However, among adolescents (aged 10–19 years), progress is slower, with AIDS-related deaths declining just 37% over the same period.
The single biggest paediatric treatment challenge is to rapidly find children living with HIV who were missed at birth or during breastfeeding and link them to care. Scale-up of rights-based index, family and household testing and self-testing, and integrating HIV screening with other child health services, can help close this gap.
Our work
Related


Update
Children being left behind
27 September 2021
27 September 2021 27 September 2021New HIV infections among children declined by more than half (54%) from 2010 to 2020, due mainly to the increased provision of antiretroviral therapy to pregnant and breastfeeding women living with HIV. However, that momentum has slowed considerably, leaving particularly large gaps in western and central Africa, which is home to more than half of pregnant women living with HIV who are not on treatment.
Gaps in the testing of infants and children exposed to HIV have left more than two fifths of children living with HIV undiagnosed. The number of children on treatment globally has declined since 2019, leaving almost 800 000 children (aged 0 to 14 years) living with HIV not on antiretroviral therapy in 2020. Just 40% of children living with HIV had suppressed viral loads, compared to 67% of adults. Nearly two thirds of children not on treatment are aged 5 to 14 years—children who cannot be found through HIV testing during postnatal care visits. A priority for the next five years is to expand rights-based index, family and household testing and to optimize paediatric treatment in order to diagnose these children, link them to treatment and retain them in life-long care.
Our work
Related

Update
Inequalities at the heart of uneven progress in the AIDS response
20 September 2021
20 September 2021 20 September 2021Progress against HIV has been uneven. The gains made through people-centred approaches within the highest performing HIV programmes have been tempered by insufficient action in other countries.
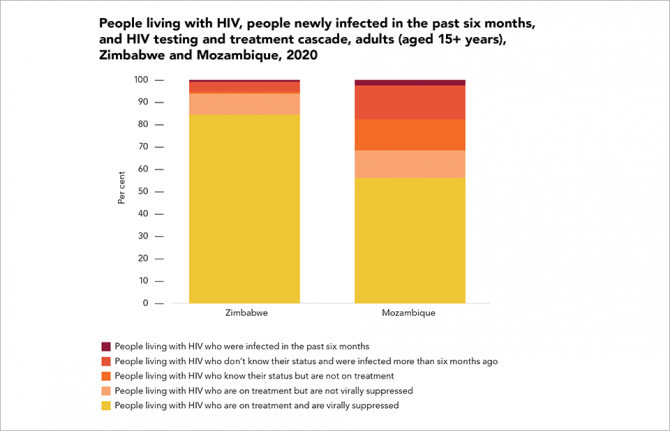
Zimbabwe has been an HIV testing and treatment leader. The southern African country’s AIDS Levy has mobilized a significant amount of domestic funding, communities are strongly engaged in service delivery and international financial and technical support has been strong and consistent. Eighty-two per cent of adults living with HIV in the country have suppressed viral loads. Neighbouring Mozambique, by contrast, has lagged behind the regional average, leaving nearly half (44%) of adults living with HIV in the country with unsuppressed viral loads. Conflict, climate change, high levels of poverty and poor health infrastructure are among the country’s many challenges.