Asia Pacific

Update
Lessons from Thailand: integrating HIV services into national health schemes
01 February 2016
01 February 2016 01 February 2016In the late 1990s, the Thai Government started offering free antiretroviral medicines to several thousand people. Apiwat Kwangkaew, currently Vice-Chair of the Thai Network for People Living with HIV, was one of the lucky ones.
“Twenty years ago I got really sick because of AIDS. I didn’t think I was going to make it,” said Mr Apiwat. Within a few months of starting treatment, he was healthy again.
“What was really tragic was that antiretroviral medicines existed, but my friends and other people living with HIV were not accessing them,” he said.
Because of that experience, ensuring access to HIV treatment has been his life’s passion. He is now one of Thailand’s better known advocates for people living with HIV.
Since the 1990s, the situation has vastly improved. In 2002, Thailand became one of the first members of the Association of Southeast Asian Nations (ASEAN) to integrate HIV services into its universal health coverage scheme. Between 2010 and 2014, coverage of people living with HIV receiving antiretroviral medicines increased from 42% to 61%.
Suchada Chaivooth, Director of the HIV and Tuberculosis programme at the National Health Security Office, said that Thailand had found many benefits from this integration. “The government can negotiate a good price for antiretroviral medicines because it’s supplying a large number of people living with HIV,” she said.
Panya Shoosiri, a gardener from Amphur Thamai village in Chantaburi Province, central Thailand, is one of the many people accessing free antiretroviral medicines. He has been living with HIV for more than 15 years. His monthly income is about US$ 100. “All HIV services are covered by the national plan. It’s a big relief for me,” said Mr Panya.
In 2014, Thailand reached a new milestone, becoming the first country in ASEAN to offer free HIV treatment to people living with HIV regardless of their CD4 count, the measurement used to indicate how significantly the immune system has been affected by HIV. Previously, people who tested positive could only access antiretroviral medicines after their CD4 count had decreased to 350 cells/mm3.
“I campaigned hard for this development because I am sure it will save many lives,” said Mr Apiwat. “People living with HIV often only came back to the hospital when they were really sick and by then the antiretroviral medicines didn’t work so well and they were more likely to die,” he added.
Since the new guidelines went into effect, Thailand has seen enrolment on its HIV treatment programme increase by more than 30%.
During a visit to Bangkok, UNAIDS Executive Director Michel Sidibé said, “The AIDS response in Thailand and around the globe has a lot to offer the universal health-care movement.”
Mr Sidibé pointed out that the AIDS response has achieved one of the most remarkable expansions in modern history. In 2000, fewer than 1% of people living with HIV in low- and middle-income countries had access to treatment. The annual cost per person was sky high. As of June 2015, the global number reached 15.8 million people or 40% of the total number of people living with HIV around the world.
He emphasized so much has been achieved in such little time because the AIDS movement has prioritized people. From the early days of the epidemic civil society has played a key role in expanding access to HIV services.
In Thailand, the government earmarks funds for health-care facilities to team up with community groups. “Our HIV programme is one where hospitals work in partnership with community groups to provide prevention services, reaching key populations at higher risk of HIV and providing them with HIV testing and care,” said Ms Suchada.
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025






Update
Global health leaders set priorities for achieving universal health coverage
29 January 2016
29 January 2016 29 January 2016Public health leaders and key stakeholders from around the world have come together at the Prince Mahidol Award Conference to discuss how limited health resources can be used in the most cost-effective way to provide high-quality health care.
Her Royal Highness Princess Maha Chakri Sirindhorn opened the conference by saying it came at a key moment since it followed the adoption of the Sustainable Development Goals by countries late last year. The UNAIDS Executive Director Michel Sidibé delivered a keynote address speaking about the need for a paradigm shift, moving from a disease response to a people-centred approach.
The conference, which is taking place in Bangkok, Thailand from 26 to 31 January, is being held under the theme Priority Setting for Universal Health Coverage. It is welcoming more than 900 government officials, representatives of intergovernmental organizations, international development partners and researchers from around 50 countries.
Thailand is one of the countries that have succeeded in putting people at the centre of their universal health coverage plan. Thailand champions the scale-up of community-led services. The Bangkok Metropolitan Administration, for example, works closely with civil society and communities.
During his visit to Thailand, Mr Sidibé visited two community-led programmes with Ms. Pusadee Tamthai, the Deputy Governor of Bangkok. One was the Service Workers in Group Foundation, better known as SWING, which supports sex workers by providing screening for sexually-transmitted infections, HIV counselling, testing, treatment, care and support services.
Mr Sidibé also visited the Tangerine clinic, housed at the Thai Red Cross AIDS Research Center, which is the first clinic to offer comprehensive sexual health services to transgender people in Thailand. Mr Praphan Phanuphak, Director of the Research Center, is a pioneer in the AIDS movement and demonstrates how science, integrated into community work, brings health care to even the most marginalized people.
Quotes
“It is time to address the critical linkages between health, injustice, inequality, poverty and conflict. Our collective challenge towards universal health coverage will be how to reach the most vulnerable and marginalized—the hardest to reach.”
“As we set priorities, let us keep people at the centre, particularly the most vulnerable.”
"We believe that equitable services are about equal partnerships with communities and civil society so the Bangkok Metropolitan Administration values and continues to strengthen its collaboration with community organizations in the delivery of HIV and other essential health services."
“Empowering people is essential for good universal health coverage, as only if people have a voice will they ask for the services they really need. SWING and other community networks and civil society organizations are working with the Bangkok Metropolitan Administration to ensure their voice is heard.”
Speeches
Region/country
Related


Feature Story
Japan hosts major conference on financing the response to AIDS, tuberculosis and malaria
17 December 2015
17 December 2015 17 December 2015Japan hosted the Fifth Replenishment Preparatory Meeting of the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) on 16 and 17 December, which laid the groundwork for a pledging conference in mid-2016 at which donors will finalize the Global Fund’s next three-year funding cycle.
The participants included Japan’s Foreign Minister, Fumio Kishida, health ministers from several countries, Margaret Chan, the Director-General of the World Health Organization, Bill Gates, co-chair of the Bill & Melinda Gates Foundation, and Luiz Loures, Deputy Executive Director of UNAIDS.
”We have an unprecedented opportunity in the next five years to break the AIDS epidemic,” said Mr Loures. “If we scale up care, treatment and prevention services and create an environment where people have full access to them we will be on course to end the AIDS epidemic by 2030.”
On the eve of the meeting, Japan also organized a conference on universal health coverage in order to evaluate the financial systems and funding required by countries to promote access to affordable health care and medicine. Universal health coverage is key to ending the epidemics of HIV, tuberculosis and malaria, which are fuelled by poverty, stigma and discrimination.
Japan has been one of the leading investors in the AIDS response, supporting programmes focused on key populations across Asia and investing in projects such as the Kenya HIV Situation Room, which is using cutting-edge technology to provide high-quality data about that country’s epidemic.
While he was in Japan, Mr Loures also visited PLACE Tokyo, which provides community-based services related to HIV and sexual health, including consultation services for people living with HIV.
“The role of communities remains as critical as ever in addressing the realities, needs and challenges of people living with HIV in Japan,” said Mr Loures. “I congratulate PLACE Tokyo for the work they are doing to support people living with HIV, their partners and family members.”
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025




Feature Story
Fiji’s AIDS response provides lessons for broader sustainable development agenda
07 December 2015
07 December 2015 07 December 2015Fiji has a low-level AIDS epidemic, with fewer than 1000 people estimated to be living with HIV in 2014. A combination of engaged leadership, integrated multisectoral action, evidence-informed and rights-based approaches and people-centred partnerships are behind the country’s success in the response to HIV. The Fijian strategy provides important lessons to help ensure greater progress across broader sustainable development issues and goals.
“Fiji’s AIDS response has much to celebrate—and much to share,” said UNAIDS Deputy Executive Director Jan Beagle during her visit to Fiji from 30 November to 3 December. “There has been strong recognition that the most effective results can only be achieved through partnership, across sectors, through strong leadership and with community at the centre. By taking AIDS out of isolation, the impact can go far beyond the AIDS response.”
Partnership across government, communities, the health and education sectors and the United Nations system has led to focused prevention and treatment strategies and action. Responding to evidence of potential risk for key populations, Fiji has implemented a number of key policy and legal reforms, including decriminalizing sex between men and removing HIV-related travel restrictions and laws criminalizing HIV transmission or exposure.
Leaders in the country have consistently championed the HIV agenda, including through sustained activities to raise awareness in schools and among faith communities and the private sector.
In a meeting with Ms Beagle, President Jioji Konrote of Fiji expressed his personal commitment to continuing action on AIDS. Minister of Health and Medical Services Jone Usamate confirmed the country’s commitment to implementing the UNAIDS Fast-Track approach to increase action and front-load investments on HIV over the next five years and to end new HIV infections among children within the next two years.
“We need to continue the solid work in Fiji and use the experience and opportunity to strengthen efforts on climate change, noncommunicable diseases and gender-based violence,” he said, underlining the alignment of Fiji’s new National AIDS Plan with the UNAIDS strategy towards ending the AIDS epidemic by 2030.
Partners in the Fijian AIDS response agree that further scale-up must be continued to ensure sustained progress in the country and across the Pacific region.
“We cannot afford complacency on HIV and we need to keep it on the agenda, because we know that progress here is also having benefits across health, development, gender and rights issues,” said Speaker of the Parliament Jiko Fatafehi Luveni, a prominent advocate for HIV and women’s issues.
The newly elected Secretary of the Fiji Council of Churches, Simione Tugi, underlined the important role of faith-based communities and organizations across multiple religions to reach people in greatest need.
“Established networks, particularly within the faith community, help reach people even in hard to reach areas,” Mr Tugi said. “We will continue to be advocates for HIV through these structures so that we leave no one behind.”
Active involvement of people living with and affected by HIV is heralded by all partners as one of the key enablers for progress in the AIDS response.
Jokapeci Tuberi Cati of FJN+, Fiji’s network of people living with HIV, said, “We have made our voices heard and have been listened to, but we need ongoing focus, commitment and resources allocated to HIV. And we need to keep fighting stigma and discrimination for a more equal Fiji and safer society for all.”
Region/country
Related




Feature Story
How Quezon City in the Philippines is turning around the AIDS epidemic
03 December 2015
03 December 2015 03 December 2015A young man wearing a striped red T-shirt and faded blue jeans enters a popular bar in downtown Quezon City, the Philippines. He starts speaking to the owner and is soon joined by several other young men. It’s 10 p.m. and the group blends in seamlessly with the other bar customers. The young men are not here to relax, though. They are peer educators and health workers employed by Quezon City’s health department.
“You just get used to it,” said Mai. “The night is to us what the day is for others. It’s the job.”
Outside, a street lamp casts an orange glow on a city ambulance that purrs softly, parked and waiting unobtrusively for clients. The group of men has come to conduct HIV counselling and testing with bar patrons and staff, who are mostly gay men or other men who have sex with men. On this steamy night they test around 50 people.
With nearly 3 million residents, Quezon City is the Philippines’ most populous urban centre and has made stopping a burgeoning AIDS epidemic a top priority.
“Quezon City is unrelenting in its effort to pursue and sustain its programme of zero new HIV infections, zero discrimination and zero AIDS-related deaths. We remain committed to providing preventive interventions, treatment, care and counselling to ensure our people receive a better quality of life,” said Mayor Herbert Bautista.
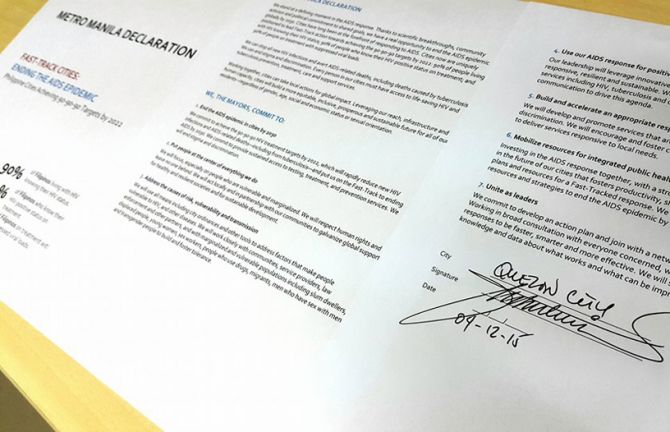
UNAIDS has encouraged cities to accelerate their AIDS response by front-loading investments and reaching critical HIV prevention and treatment targets. In the Philippines, Quezon City is leading the push to implement the UNAIDS Fast-Track Strategy in urban areas.
On 4 December, Quezon City hosted a meeting with representatives from cities in the Metro Manila area on how to end the AIDS epidemic by 2030. Participants adopted the Fast-Track approach.
UNAIDS estimates there were 6400 new HIV infections nationwide and 36 000 people living with HIV in the country in 2014. HIV prevalence among men who have sex with men was 3.3% in 2013, compared to 1.68% in 2011. Among the general population aged 15–49, the estimated HIV prevalence was lower than 0.1% in 2014.
Quezon City: a trailblazer in the country’s HIV response
While a network of facilities catering to the health needs of sex workers has existed since the 1990s in the Philippines, in 2012 Quezon City became the first city in the country to open a clinic providing services for men who have sex with men and transgender people.
Klinika Bernardo, popularly known as the Sundown Clinic, is located along a busy highway. It operates from 3 p.m. until 11 p.m., allowing a maximum number of clients to visit.
“We cater to men who have sex with men from all over the Philippines,” said Leonel John Ruiz, head physician at Klinika Bernardo. “Only 40% of our clients are from Quezon City.”
From the start, demand for services at the Sundown Clinic was high. Almost 250 HIV tests and pre- and post-test counselling services were conducted in its first two months of operation and 18 people tested HIV-positive. By the end of 2014, the clinic had conducted more than 2500 tests, of which a little more than 200 were HIV-positive. The first Sundown Clinic was so successful that the city opened a second one earlier this year.
The Sundown Clinic: a safe space for men who have sex with men and transgender people
While same-sex sexual relations are legal in the Philippines, such relationships are viewed negatively by many people and there is a high degree of stigma and discrimination towards gay men and other men who have sex with men. Fear of being outed and ostracized prevent many men who have sex with men from accessing traditional health services. Studies by city health officials show that two thirds of men who have sex with men in Quezon City have never had an HIV test.
With its row of potted plants and bright green decor, Klinika Bernardo exudes a cheerful atmosphere. It has 10 staff members, with four peer educators, who include men who have sex with men and a transgender woman. Clients can choose the educator who best suits their needs. Instead of documenting and calling clients by their name, the clinic maintains their anonymity by giving each person a number.
Staff are skilled at reassuring jittery clients.
“This is my first HIV test. I do not know what to expect,” said one young man while filling out registration forms. “I tried to read up on HIV so I would have some background information, but it took me awhile to gather the courage to come here. My partner came here with me, too, after hearing about it from our friend. We’re taking the test together.”
The young man found the staff supportive and skilled at easing his fears.
People who test HIV-positive receive counselling on antiretroviral medicines and are accompanied by staff through their initial months of HIV treatment, which is free in the Philippines.
Quezon City’s HIV programme becomes a model for other cities
Quezon City operates the Sundown clinics and has significantly increased investments in its HIV programmes in the past few years. And the city's efforts to scale up HIV testing are getting results. The number of gay men and other men who have sex with men being tested almost quadrupled between 2011 and 2014.
“In the three years that we have been operating, the perspective has definitely changed,” says Mr Ruiz. “Before, we would have a hard time inviting people for testing. Now, most of our clients are walk-ins. People are personally and actively seeking information.”
Quezon City won the prestigious Galing Pook Award for outstanding local governance in 2014 for its pioneering HIV clinics. Several other local city governments are starting to adapt the Quezon City model and establish their own clinics.
While the Sundown Clinic staff are proud of their achievements, they are looking forward to closing shop one day.
“I pray before sleeping,” says Adel, the only female peer educator at Klinika Bernardo. “I pray that there would come a day when there will be no one in need of our services. That’s what I am working for.”
Related


Feature Story
UNAIDS appoints former President of Fiji as a Regional Goodwill Ambassador on World AIDS Day 2015
01 December 2015
01 December 2015 01 December 2015Fiji has shown significant leadership and commitment to the response to HIV. On the occasion of World AIDS Day 2015, UNAIDS has appointed the country’s former President, Ratu Epeli Nailatikau, as a Regional Goodwill Ambassador for the Pacific. The announcement was made by Jan Beagle, Deputy Executive Director of UNAIDS, during a World AIDS Day ceremony in Suva attended by representatives of government, civil society and international organizations.
“Fiji has some important lessons to share in a number of areas, including leadership, multisectorality, integration and partnership, that can benefit the region, and beyond, as we strive to reach the goal of ending AIDS by 2030,” said Ms Beagle. “His Excellency Ratu Epeli Nailatikau has been a steadfast advocate and at the forefront of these efforts, championing the HIV response and the meaningful inclusion of key populations.”
Building on his experience and years of commitment, Mr Epeli Nailatikau will help mobilize political support for the UNAIDS Fast-Track approach across the region, to accelerate and front-load investment over the next five years as a critical step towards ending the AIDS epidemic as a public health threat by 2030. In his new role as Regional Goodwill Ambassador he will also work with UNAIDS to help to ensure that the human rights of people living with HIV and key populations at higher risk of HIV are protected and respected, and that young people, women and girls and people living with and affected by HIV are meaningfully engaged in the HIV response.
With the exception of Papua New Guinea, HIV prevalence is low across the Pacific. However, a combination of factors could lead to a rise in the HIV epidemic in the region. These include widespread migration and mobility, high levels of multiple sexual partners, a large caseload of untreated sexually transmitted infections (STIs), low knowledge about HIV and STIs, high levels of transactional sex and significant levels of intimate partner violence. Stigma and discrimination towards key populations at higher risk of HIV is also high.
Former President Ratu Epeli Nailatikau said, “To get where we need to be, I believe it is time to Fast-Track the HIV response. As UNAIDS Regional Goodwill Ambassador I will work tirelessly to end the AIDS epidemic not only in Fiji but throughout the Pacific. You can count on me.”
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025



Feature Story
Republic of Korea’s network of people living with HIV opens its doors in Seoul
10 November 2015
10 November 2015 10 November 2015Munsu has been living with HIV for 20 years and has played an active role in the Republic of Korea’s AIDS movement. However, like thousands of people in his situation, he has not shared his HIV status with his family because he is fearful of their reaction and the social isolation that such a disclosure would most likely bring about.
He is all too aware of the stigma and discrimination faced by HIV-positive people in his country.
Munsu is a founding member of the Korean Network of People Living with HIV/AIDS (KNP+), a Seoul-based organization with some 2000 members, established in 2011 to bring five existing organizations under one umbrella and to provide a concerted and connected voice for the country’s HIV-positive community. On 30 October 2015, after several years of effort, KNP+ opened its first official office and community space.
An epidemic of fear
According to the Korea Centers for Disease Control and Prevention, there are more than 10 000 people living with HIV in the country. The Republic of Korea’s epidemic is heavily concentrated among gay men in urban settings, with men representing 92% of all HIV infections since data collection began in 1985.
Despite the country’s low HIV prevalence, fear of HIV is a problem. A national survey conducted in 2005 indicated that only half of respondents would care for a family member if he or she were HIV-positive. Reports also indicate that HIV phobia is present in health-care facilities.
At the KNP+ community centre event, Minji Kim, a young doctor and a volunteer with KNP+, shared the ignorance towards HIV she encountered in medical school. “One of our classes focused on AIDS and I was shocked at my classmates’ reactions,” said Minji. “They were making fun and mocking people living with HIV. I knew I had to do something to change this.”
Munsu thinks one of the reasons HIV is so feared in Korean society is that it is linked to homosexuality, transgender sexuality and other issues that are negatively viewed. This “double dose” of exclusion, he said, forces many people living with HIV to be isolated, especially from their family.
As the attachment to loved ones is particularly strong in Korean society, rejection by family members can mean that many people living with HIV are abandoned and segregated from social events. This situation extends to the provision of health care, he noted. “Many people living with HIV cannot be admitted to hospital because they have no family member to be responsible for them, to be their caregiver. This is essential in Korea if you want medical services,” said Munsu.
Overcoming stigma as a priority
As stigma in daily life is one of the top concerns most cited by members of KNP+, the organization and its partners are prioritizing efforts to respond. With its permanent office in place, KNP+ is preparing to compile Korea’s first People Living with HIV Stigma Index.
The Stigma Index initiative is a collaboration between the Global Network of People Living with HIV, the International Community of Women Living with HIV/AIDS and UNAIDS. The initiative aims to document HIV-related stigma and discrimination and provide a mechanism to compare experiences in different settings and across time. Findings will be used to advocate for change and progress to redress the situation. The Stigma Index is also important in that it empowers people living with HIV in the process, involving them directly in the design, deployment and analysis phases. This participatory approach is led by organizations of people living with HIV with support of international and domestic partners.
The Stigma Index will be carried out in 2016. A research team to oversee its development and deployment is expected to be operational in January 2016.
KNP+ is optimistic that the results of the Stigma Index will influence policies, particularly around human rights, improve psychosocial support programmes for people living with HIV and boost service uptake by making it easier for people to come forward. The organization also hopes to use the data collected to shape a national zero stigma campaign it plans to launch in 2017. Most importantly for the organization, the Stigma Index should kick start a long overdue dialogue on removing the deep-rooted fear of HIV in Korean society.
Steve Kraus, Director of the UNAIDS Regional Support Team for Asia and the Pacific, applauded the organization for taking the Stigma Index forward, stating that it is a key tool in bringing about change for people living with and affected by HIV.
“Our experience in all of the countries in our region that move forward in compiling the Stigma Index show that some remarkable things happen—a greater dialogue and understanding is established and a space for political mobilization is created,” said Mr Kraus. “It is in turn used for advocacy on budgets, on policies, on programmes and especially for reaching out to the community to make sure that no one is left behind and everybody feels included in the national response.”
Region/country
Related


Update
India and Africa strengthen partnership on accessible and affordable medicines
30 October 2015
30 October 2015 30 October 2015During a high-level event on 30 October on the sidelines of the Third India-Africa Forum Summit 2015 in New Delhi, India, leaders from India, the African Union, several African nations and major Indian pharmaceutical companies pledged to address existing and emerging challenges to health commodity security in Africa.
The Indian pharmaceutical industry produces low-cost generic medicines that have been instrumental in scaling up access to HIV treatment in developing countries. The low price of generic first-line regimens is one of the factors that have contributed to the milestone achievement of providing access to life-saving antiretroviral therapy to more than 15 million people around the world.
Of the 36.9 million people living with HIV in 2014, around 25.8 million live in sub-Saharan Africa. By mid-2015, 11.4 million people living with HIV in sub-Saharan Africa had access to treatment. The achievement builds momentum for ending the AIDS epidemic as a public health threat by 2030.
However, despite the progress made so far, the price of second- and third-line medicines and diagnostics continues to be a barrier to HIV treatment access. One of the actions that will improve the situation is ensuring that pharmaceutical innovations are available, affordable and accessible to all.
As part of the Pharmaceutical Manufacturing Plan for Africa, African Union member states are taking steps to develop the local pharmaceutical sector on the African continent to enable Africa to manufacture a sustainable supply of high quality and affordable essential medicines. The development of the pharmaceutical industry will contribute to better public health outcomes and economic growth across the continent. An African and international consortium of partners that includes UNAIDS is supporting the local production of medicines.
Kenya, South Africa, Uganda and Zimbabwe are already producing World Health Organization pre-qualified antiretroviral medicines, with other countries planning to start production.
Quotes
“I call on India and my African peers to support the extension of the least developed country waiver and sustained TRIPS flexibilities to ensure access to affordable ARVs and other medicines. I urge India to continue to produce antiretroviral medication at the quantities required for the rapid scale up of treatment until such a time that the African pharmaceutical industry in fully developed.”
“India is committed to ensuring that the TRIPS flexibilities will be fully harnessed to provide sustained and uninterrupted access to life-saving medicines. TRIPS flexibilities have proved to be a lifeline for the poor and we have a duty to ensure that this line does not snap.”
“A strengthened partnership between India and Africa will create an irresistible force for investment in science, medicine and technology, bringing better health outcomes to millions of people as we work towards ending the AIDS epidemic and achieving universal access to healthcare as part of the Sustainable Development Goals."
External links
Region/country
Related


Feature Story
Thailand leads the way in the Asia–Pacific region to ensure that all children are born HIV-free
22 September 2015
22 September 2015 22 September 2015“When I was 30 years-old, I was surprised to learn that I was pregnant,” said Prem Paika, who lives in Chiang Mai, Thailand. “My partner, who I had been with for the past eight years, thought he was infertile, so we did not use any birth control.”
Ms Paika was also concerned because she and her partner had been diagnosed with HIV five years earlier. She had been taking antiretroviral medicine for the past few years and went to consult with the doctor overseeing her HIV treatment at a public hospital.
“I was very worried my baby would have HIV, but my doctor reassured me that the antiretroviral medicine would protect my baby,” said Ms Paika.
Untreated, women living with HIV have a 15–45% chance of transmitting the virus to their children during pregnancy, labour, delivery or breastfeeding. However, that risk drops to under 5% if antiretroviral medicines are given to both mother and child through the stages when infection can occur.
Thailand has made the elimination of new HIV infections among children a priority and has consistently adapted its prevention of mother-to-child transmission programme in accordance with the latest research findings. The country is currently following the World Health Organization’s guidelines to provide lifelong antiretroviral medicine to all pregnant women living with HIV. The Ministry of Public Health has implemented measures in its hospitals to ensure that mothers living with HIV receive key services.
“We have developed a system in hospitals where the mother’s confidentiality is guaranteed. Health sector staff have been trained to communicate well with their patients,” said Danai Teewanda, Director from the Bureau of Health Promotion at the Ministry of Public Health in Thailand.
Ms Paika found her regular doctor supportive and she was happy because the hospital provided psychological counselling for her through her pregnancy and until her child was one year old. She could also access her HIV treatment and receive her antenatal check-ups in the same hospital and so did not have to travel from one part of town to another, visiting different specialists.
However, despite efforts by Thailand’s health authorities to create a supportive environment, stigma remains a problem among staff working in other health areas. Ms Paika found that the hospital’s gynaecologist treated her badly and was often misinformed.
“From my first antenatal examination, the gynaecologist encouraged me to have an abortion. He wouldn’t let me see the sonogram as he said in any case there was no point. He told me my baby only had a 2% chance of being born free of HIV.”
Ms Paika turned to her HIV treatment doctor for comfort and her partner complained to the hospital’s director. After this, she found that the gynaecologist treated her better. Finally, the big day arrived: she gave birth to a baby girl.
“They provided her with an antiretroviral prophylaxis and she was tested at one month and then every six months. She was HIV-negative each time. I am so happy she is free of HIV,” said Ms Paika.
Through its efforts, Thailand has achieved remarkable progress in eliminating new HIV infections among children. In 2014, country programme data showed that almost 95% of HIV-positive pregnant women received antiretroviral medicines to reduce the risk of HIV transmission and almost 98% of their babies were born free of HIV.
The country is hoping to further reduce new HIV infections among children. “We have a few weak spots, such as early detection. We are encouraging women to seek antenatal care within the first 12 weeks of their pregnancy,” said Mr Danai.
Since 2013, Thailand has provided free antenatal services to pregnant women at all health centre facilities, promoted HIV counselling and testing for couples and provided antiretroviral medicines to infants as soon as possible after birth. The country hopes by 2016 to have virtually eliminated new HIV infections among children.
Senior government health authorities from Thailand were among representatives from 20 countries who attended the 10th Asia–Pacific United Nations Elimination of Parent-to-Child Transmission of HIV and Syphilis Task Force meeting in Beijing, China, from 15 to 17 September. The meeting examined regional successes, but also roadblocks to stopping new HIV infections among children.
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025





Feature Story
Photography exhibition aims to reduce HIV stigma and discrimination in Pakistan
07 September 2015
07 September 2015 07 September 2015A photography exhibition portraying the inspirational stories of people living with HIV opened in Islamabad, Pakistan, on 7 September.
A Photo Story on People Living with HIV in Pakistan is a collection of 25 portraits of men and women living with HIV who have taken the decision to share their stories of HIV-related stigma with the public. It is the first exhibition in Pakistan to shine the spotlight on the resilience of people living with HIV. Each photo is accompanied by a short interview in which people express their challenges and concerns, but also their determination to bring about change and eliminate stigma and discrimination.
Nazir Masih, the Chief Executive Officer of the New Lights AIDS Control Society, a non-profit organization dedicated to providing treatment, care and support for people living with HIV, is one of the people portrayed in the exhibition. He said, “HIV is a problem of human beings and it is not an issue of any particular religion or nation. That is why hurdles and threats cannot deter me from the path of helping those in need and will not stop me, come what may, because this is what I have been made for.”
In Pakistan, it has often been difficult to disseminate key HIV information, owing to cultural and social barriers. The aim of this exhibition is to give a human face to the epidemic, with photographs that will have a lasting impact and can be shared on multiple platforms.
“We salute the courage and willingness of the men and women showcased in this exhibition to disclose their status in the hopes of transforming society,” said Steve Kraus, Director of the UNAIDS Regional Support Team for Asia and the Pacific, who inaugurated the exhibition. “Let us embrace our brothers and sisters living with HIV. Only when we reach zero discrimination can we end the AIDS epidemic in Pakistan.”
Stigma and discrimination towards people living with HIV remains a widespread challenge in Pakistan. The country’s People Living with HIV Stigma Index, conducted in 2010, revealed high levels of stigma and exclusion from families and religious activities and discrimination in employment. One third of respondents reported being denied access to health care in the previous 12 months.
Abdul Baseer Khan Achakzai, National Programme Manager, National AIDS Control Programme, said “The Government of Pakistan is committed to scaling up targeted interventions to prevent the rise in HIV prevalence among key and vulnerable populations and to fostering an organized national response to halt new HIV infections, improve the health and quality of life of people with and affected by HIV and initiate community-based HIV testing to bridge the gap between registered and estimated HIV cases.”
The exhibition was produced in collaboration with the National AIDS Control Programme of Pakistan, the United Nations Information Centre and UNAIDS.



