Community mobilization




Feature Story
The power of visibility — My story as the first person who came out as a person living with HIV in Fiji
18 April 2023
18 April 2023 18 April 2023Jokapeci Cati is the Program Manager and founder of the Fiji Network for Positive People (FNP+). This is her self-told story of how she became the first person living openly with HIV in Fiji.
I grew up in the harbour town of Suva. I was brought up in the Seventh Day Adventist Church. During youth camps we had two sessions on HIV. To me it was just a session. I had this perception that I am not promiscuous so I can’t become HIV positive.
I got married at 21 and got infected in my marriage. I was diagnosed in 2000 but I suspect I was living with HIV since 1999. My husband was sickly and became bed ridden. I did not blame him. I felt like he got infected before we were married and did not know he was living with HIV. In 2003 he died due to AIDS-related causes. He was 31.
We did not have treatment in Fiji at that time. People living with HIV were just monitored. When I was diagnosed they told me “you have to look after yourself because you can die”. In the initial stages there was depression, denial and stress. But as soon as I got diagnosed one of my dreams was to meet another person living with HIV.
With my family there was no change in the way they treated me. It was support from the word go. I did not see any element of discrimination from my parents and siblings.
Going public
Coming out was not an overnight decision for me. It took me six months to juggle the pros and cons. Somehow my mind was not dwelling on the negative. Because there was no support system in place at the time, I felt the need to speak out.
So I started with the church. I went to the pastor and told him of my diagnosis. Then I had to disclose to my church community. The hardest bit was opening up to your very own people. Once I gained the support of the church I spoke to the Council of Chiefs, Fiji’s traditional leaders forum. Because those platforms gave me a positive reception I then went to the media because I felt I was ready to speak to the nation.
Organising and advocating
In 2003 I was privileged to meet the right people at the Ministry of Health and we coordinated the first meeting of FNP+. By 2004 I got the organisation registered, up and running.
From the start I was advocating for treatment because I could see my first husband dying. The Ministry of Health’s HIV coordinator at the time, Maire Bopp Dupont, connected us to the Asia Pacific Network of People Living with HIV. That is how I got to know that other countries in the region were offering treatment. We went to the Council of Chiefs and Parliamentarians to advocate. The Health Ministry at the time was saying “we are not ready… we need to put the systems and structures in place”. I think because we came out publicly it put some pressure on them. The very next year, in June, treatment was available.
It was exciting. For the first time we felt the advocacy was worth the sacrifice. Our work involved talking to nurses, doctors and civil society organisations that were part of the care team. I started antiretroviral therapy five years ago when we adopted the “treat all” policy. It is so exciting that we are able to take treatment with the assurance that we would live! And it is for free!
Living life fully
I did not let HIV decide my future. Because of being part of the FNP+ management team I found the need to venture into education. I got a degree in psychology and social work from the University of South Pacific.
When I lost my first husband I was in this dilemma about whether to have children. I met my current husband in the HIV organisation. When we decided to have children, it was a public affair in Fiji. I was an HIV positive, pregnant woman. It was a learning curve for me and the entire nation.
The UNAIDS Goodwill Ambassador for the Pacific, Ratu Epeli Nailatikau, was Fiji’s President at the time. He made it his business to come to the hospital during my delivery and my first son’s HIV test. He wanted a copy of my son’s HIV negative test result. This became his advocacy document. He has been spreading the message since then that there is no need to discriminate against women living with HIV who want to have children. It’s time we support them through prevention of mother-to-child transmission (PMTCT) treatment. I am now the mother of three HIV negative children.
The way forward
We are working to get FNP+ funding from the Global Fund to continue our national activities and regional support. I’m glad the focus is now on community-led monitoring and services and that it’s coming from the donor’s mouth.
Other Pacific countries don’t have networks of people living with HIV. Fiji is the only one. People throughout the region are living in isolation. Our second piriority is to organise at the regional level.
Our third challenge is that although everyone who is living with HIV is encouraged to take treatment, we have stockouts. At one point we weren’t getting Dolutegravir so people had to change to a combination of drugs until it became available. Labs are also a challenge, especially the turnaround time for viral load tests. If FNP+ does not continue to apply pressure to address these issues people would suffer silently.
HIV in a small island developing state
For sure people living with HIV from key population communities have had a more difficult time. They were ostracised, they were discriminated against. I did not face that. There was a time, around 2004 and 2005, when people who died due to AIDS had to be burned at night before the sun rose! The stigma and discrimination are not as bad as that now, but they still exist.
I think in the Pacific it is really hard to come out with your HIV status because of our small size. We have these connected communities and if someone comes out it is easy to trace who else could be HIV positive. We have this communal upbringing so people don’t want any negative repercussions for their families.
When other people living with HIV meet me, they are happy. They want to come out and speak, but they don’t know how. Now there is funding for this community engagement in more Pacific countries. We just need to give them support and a bit of time.
Fiji recently received technical support for the seventh cycle of Global Fund applications and the Indo Pacific HIV Prevention Program supported by the Australian Department of Foreign Affairs and Trade (DFAT). UNAIDS Pacific supports peer network meetings to encourage sharing among PLHIV. UNAIDS also recently collaborated with Rainbow Pride Fiji Foundation, the Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM) and the National Association of People with HIV Australia (NAPWHA) to develop a PLHIV booklet in the local languages. This booklet provides information on living with HIV and helps empower PLHIV to take control of their health and wellbeing. This project is supported by the New Zealand Ministry of Foreign Affairs and Trade and DFAT.
Region/country
Related


Press Release
New UNAIDS Collaborating Center at Georgetown leverages strengths in HIV/AIDS law, policy and politics
12 April 2023 12 April 2023WASHINGTON DC, 12 April 2023 — The Joint United Nations Programme on HIV/AIDS (UNAIDS) today designated the Global Health Policy and Politics Initiative at Georgetown as a United Nations Collaborating Center to support and advance policy and laws impacting HIV/AIDS with the overarching goal of addressing the inequalities driving the pandemic.
Bridging the Georgetown School of Health and the O’Neill Institute for National & Global Health Law, the Global Health Policy and Politics Initiative leverages scholarship and technical strengths of policy and law experts embedded across Georgetown University. Matthew Kavanagh, PhD, director of the Global Health Policy and Politics Initiative at the O’Neill Institute, and assistant professor of global health in the School of Health, will spearhead the Collaborating Center.
“Legal and political forces continue to shape not only AIDS but all of the pandemics of our time. With Prof. Kavanagh’s leadership, this new Collaborating Center relationship will help build on the work he did at UNAIDS over the last year and a half and deepen our joint efforts to build the law and policy environment needed to end AIDS,” said UNAIDS Executive Director Winnie Byanyima, during a visit to Georgetown on April 12.
From September 2021 to January 2023, Kavanagh served as UNAIDS’ Interim Deputy Executive Director and special advisor to Byanyima in creating a new policy, advocacy, and knowledge branch at UNAIDS. Kavanagh stood up the structures to achieve the ambitious new Global AIDS Strategy focused on closing the inequalities underlying the continuing AIDS pandemic.
“As a Collaborating Center we look forward to working alongside United Nations colleagues from across the Joint Programme to explore more deeply the political determinants of health and help inform the development of laws and policies that can help end the HIV/AIDS pandemic and build resilience for future pandemics,” said Kavanagh. “Alongside my global health colleagues at the O’Neill Institute, School of Health, and through Georgetown’s Global Health Institute, we will be able to amplify our collective work to further advance the effective use of law and policy in response to global public health challenges, including HIV.”
Work of the Global Health Policy & Politics Initiative includes the HIV Policy Lab, a collaborative effort between Georgetown University, UNAIDS, and the Global Network of People Living with HIV, to document, track, and ultimately improve HIV-related policy environments around the world as well as work on community-led monitoring and social science research on the political determinants of health. It was founded at the O’Neill Institute, one of the world’s premier health law and policy institutes that believes that the law is a fundamental tool for solving critical health problems around the world.
“We are thrilled to partner with UNAIDS to launch this innovative Collaborating Center,” said Lawrence O. Gostin, JD, faculty director of the O’Neill Institute, which is also a designated WHO Collaborating Center. “For the past 15 years, the O’Neill Institute’s mission has been to fight for health and justice by advancing laws and policies to tackle critical health challenges worldwide. AIDS changed the world and showed the power of social mobilization. Under the extraordinary leadership of Matt Kavanagh and working with the School of Health, the Center will make a major impact on global public health and justice. I'm proud we are working in deep partnership with UNAIDS.”
“This collaboration reflects our commitment to health equity and presents new interdisciplinary opportunities for students and faculty to advance knowledge and inform policy at the nexus of inequality, law, policy, and HIV,” said Christopher J. King, PhD, dean of the School of Health, a home for scholars and students to work collaboratively across disciplines to address human health and wellbeing from various perspectives. “We are also fortunate to work alongside dedicated faculty members in Georgetown’s Global Health Institute who bring to bear significant scholarship and technical strengths in many aspects of work to eliminate HIV/AIDS.”
The agreement establishing the Collaborating Center, signed earlier today, provides a framework for inter-institutional dialogue and cooperation. In the coming months, the institutions will work to stand up a set of inequality-focused activities, develop formal, regular bilateral consultative meetings, and collaborate on sharing data and political analysis in the years ahead.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Contact
Karen Teber, Georgetown
km463@georgetown.edu
Sophie Barton-Knotts, UNAIDS
bartonknotts@unaids.org




Feature Story
LGBTQ+ shelter in Lviv provides lifeline to displaced Ukrainians
27 February 2023
27 February 2023 27 February 2023Oleg Kucherenko (not his real name) traveled from the eastern part of Ukraine to Lviv, in the western part of the country when his city, Kherson, was occupied by Russian forces. He, like many other representatives of the LGBTQ+ community was desperately looking for a safe place to stay.
His friend recommended the Facebook group of the Alliance Global - the largest LGBTQ+ organisation in Ukraine, who helped him find a spot in a shelter.
Once there, he got food, a place to sleep, and was able to contact friends and colleagues courtesy of electric generators and internet service. Up to ten people can stay in this particular shelter. The shelter administrator, Vadim Pryzenko, sees this as a lifeline.
“Our clients can get not only a place to live but also food and social and psychological support,” he said. “For those who are not living here, we provide humanitarian aid, food, hygienic products, and also individual financial support,” Mr Pryzenko said.
Since the war began a year ago, more than 7.9 million Ukrainians have fled abroad and another 6.5 million moved within the country.
Due to growing demand to find accommodation for internally displaced people that Alliance Global experienced, several organizations, including the Fondation de France, International Office of Migration (IOM) and UNAIDS’ Emergency Ukraine Fund, helped them set up the shelter. The shelter also provides health care and HIV services.
Mr Kucherenko got tested for HIV, hepatitis, and other diseases. His HIV test came back positive. He quickly met with a social worker, Andriy Kharatin, who accompanied him to the Lviv AIDS center where he got confirmation of his diagnosis, and additional tests.
"Several days later, with our help connecting him with to the health care system, Oleg started anti-retroviral therapy,” Mr Kharatin said.
Ukraine has the second - after the Russian Federation- biggest HIV epidemic in Eastern Europe and Central Asia (240 000 people are living with HIV according to 2022 estimates).
The country was making good progress in the AIDS response before the war – increasing the number of people living with HIV on antiretroviral treatment to nearly 60%.
However due to their destruction or occupation, more than 30 medical institutions providing HIV services have had to stop their operations, and logistics and supply chains have been broken. Despite this, Ukraine continues to help people living with HIV. Civil society has played a crucial role in adapting their response, engaging and reaching people in need.
“As a doctor, I am very pleased with the cooperation with Alliance Global,” said Dr. Olena Pavlishina from the Lviv Clinical Hospital. “Thanks to this cooperation we have the opportunity to be in touch with both internally displaced people and people who do not trust doctors much.”
In the past, she explains, a lot of the work was handled by health professionals.
“This part of the work that was previously done by health workers is now being done by social workers and civil society organisations,” she said.
And Mr Pryzenko doesn’t imagine that changing in the near future. He fears that if the war drags on, more people will come to the shelter and need services.
Meanwhile, Mr Kucherenko lives and works in Lutsk, not far from Lviv. He picks up his HIV medicine supply for three months and will get his next batch by mail when needed. He also stays in touch with his social worker for psychological support online.
Region/country




Press Statement
One year on: We must sustain the HIV response in Ukraine
23 February 2023 23 February 2023One year on, the war in Ukraine continues to inflict massive suffering and destruction. Since the start of the war on 24 February 2022, more than 13.5 million people have been internally displaced or forced to flee to neighboring countries as refugees, including people living with HIV and key populations.
Ukraine, the country with the second-largest AIDS epidemic in the Eastern Europe and Central Asia region, has been hit hard by the war.
The country was making strong progress in the AIDS response by: 1) increasing the number of people living with HIV on life-saving medicine (more than 150 000 people are on treatment out of 240 000 living with HIV); 2) working hand in hand with community-based organisations and 3) reaching full state financing of innovative HIV prevention services among key populations.
The shock of the war pushed all stakeholders to protect those precious gains.
The government of Ukraine and civil society partners have received enough anti-retroviral therapy (ARV), tuberculosis medicine, and opioid substitution therapy (OST) to provide uninterrupted treatment for everyone with the support of the Global Fund to Fight AIDS, Tuberculosis and Malaria, the United States President’s Emergency Plan for AIDS Relief (PEPFAR), UNAIDS, and other partners.
Civil society has been the engine of the national HIV response along with the Ukrainian Public Health Centre before the war and throughout the year. They have delivered services, medicines, and humanitarian aid to those in need without fail despite bombings, attacks, lack of electricity and reduced access to the east and south of the country.
This effort needs our ongoing support and funding. We cannot let Ukraine’s HIV response fall back.
UN agencies and partners on the ground have been working closely with local authorities to reach and help people in need. More recently they have delivered humanitarian assistance to hard hit territories in the country that have only now become accessible.
“Delivering essential aid and assistance relies on collaboration,” said Winnie Byanyima, UNAIDS Executive Director. “A coalition of government, civil society and international organisations has been and continues to be a cornerstone of the effective HIV response in Ukraine during the war. UNAIDS stands in solidarity with all the people and our partners working so hard on the frontlines.”
A UNAIDS Emergency Fund has enabled partners across the country to sustain HIV care and support services, as well as providing direct humanitarian assistance and targeted support to the most vulnerable. This has meant, for example, creating dozens of shelters for internally displaced persons, including people who use drugs, LGBTIQ+ people, and other key populations linking HIV service providers with available humanitarian assistance programmes. The Fund has received support from the Red Cross Monaco, the United States of America and Germany.
With further funding from Germany, civil society organizations in Moldova, Poland, and other neighboring countries united their efforts to improve access to services for Ukrainian refugees living with HIV.
UNAIDS has issued an urgent call to the international community for additional funding for civil society organisations to keep providing essential HIV support services in Ukraine and in countries receiving refugees in need of HIV services.
UNAIDS will continue to support HIV prevention, testing, treatment, care and support for people across Ukraine affected by the war and people displaced by the conflict.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Key humanitarian messages
War in Ukraine and the HIV response
Region/country




Feature Story
Thailand partners develop community-led HIV care curriculum
23 February 2023
23 February 2023 23 February 2023For 20 years Kochaphan Wangtan has been a community health worker, serving other people living with HIV (PLHIV) in Thailand.
“I’ve seen many friends living with HIV come to care very late with opportunistic infections,” she said.
“I focus on helping to bring them in and provide support to start antiretroviral treatment right away and I also conduct home visits, counselling and psychosocial screening so I can link them to services they need,” Ms Wangtan explained.
Ms Wangtan is from the Jai-Prasan-Jai Comprehensive Continuum of Care Center (CCC) from the Phan District Hospital in Chiang Rai province. She is one of almost one thousand PLHIV health workers who are embedded in more than 230 Thai hospitals and serve almost 60,000 PLHIV annually.
For the first time, the country has rolled out a national community health worker certification for these volunteers. The initiative is called “A Comprehensive Continuum of HIV/AIDS Care and Support for and by People living with HIV.” The curriculum was developed by the Ratchasuda College of the Mahidol University through close collaboration with the Thai Network of People Living with HIV/AIDS (TNP+) as well as support from the Health Ministry’s Division of AIDS and STIs and the National Health Security Office. USAID-PEPFAR via the III Unify Collaboration Programme and UNAIDS provided technical and financial support.
“PLHIV volunteers have provided the first community engagement in the HIV response since the start of the epidemic in Thailand,” said UNAIDS Country Director, Patchara Benjarattanaporn. “Peer-led support boosts treatment initiation and retention and is central to the HIV response,” she said. This initiative ensures that PLHIV-led health services are standardized, recognized and valued.
Two modules are delivered over 90 hours. The first module focuses on theoretical training, including on holistic follow-up care, treatment adherence counselling and developing a comprehensive service plan. The second module is practical. Along with its HIV focus, the curriculum also integrates tuberculosis, sexually transmitted infections, Hepatitis C and non-communicable diseases. Earlier in the month the first cohort of 46 PLHIV health workers received their certification.
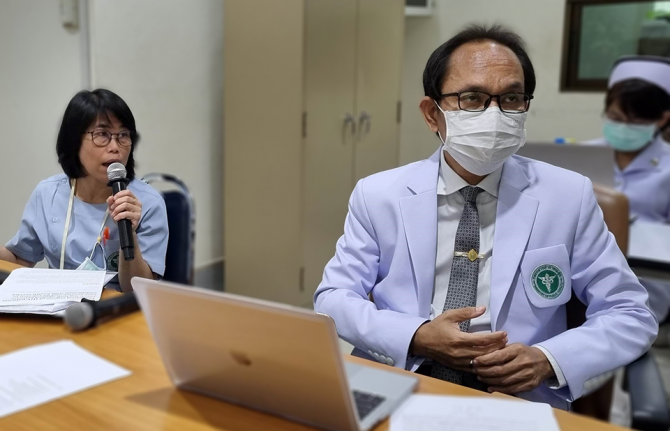
Dr. Wachara Riewpaiboon, a rehabilitation physician and former Ratchasuda College Dean, developed the curriculum.
“The health system is not only for health professionals… It belongs to everyone,” she said. “Getting an HIV diagnosis does not help clients understand what they are facing. When people living with HIV tell their story, it is very different knowledge they are imparting. The knowledge that helps people make decisions for themselves usually comes from peers, not doctors.”
For her, care goes beyond medicine.
“It is not only biology that we are dealing with, but also psychology and our interaction with our social environment—how people look at people living with HIV and how they perceive themselves,” Dr Riewpaiboon continued. “It is very important to help people see the positive side of their experience.”
According to Nurse Chulaporn SingPae, an HIV Coordinator at the Phan District Hospital, PLHIV volunteers help with counselling, adherence, missed appointment follow-up, home visits, treatment deliveries, overcoming stigma including self-stigma and promoting understanding of U=U, undetectable equals untransmittable. (An undetectable viral load means the virus is not transmittable aka untransmittable.) The training ensures that these contributions are recognized by the health system as meeting quality standards.
Now that the course has been developed and tested, the curriculum has been recognized by the National Health Security Office (NHSO). Thai civil society organizations, who provide HIV and STI services with certified community health workers have been accredited and are eligible to register as health service units in the Universal Health Coverage scheme. Having supported the development and pilot of the curriculum, UNAIDS is now supporting a study to cost these services. The office is also working to promote sufficient and sustainable financing for community-led health services for PLHIV and key populations.
“This training is going to become the guarantee that a peer educator provides a high quality of service, in a holistic way, which encompasses not just the physical but also the mental, emotional and social aspects,” said Apiwat Kwangkeaw, Chairperson of the Thai Network of People living with HIV/AIDS. “As this becomes institutionalized, we are sending a message to the health system as a whole to let the community of peer educators be an equal partner,” he said. Mr Kwangkeaw hopes this will translate into sustainable domestic financing for community-led health services and better quality of life for PLHIV.
Region/country
Related
Related
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025
 Zambian football star Racheal Kundananji named UNAIDS Goodwill Ambassador for Education Plus in Zambia
Zambian football star Racheal Kundananji named UNAIDS Goodwill Ambassador for Education Plus in Zambia

23 January 2025
 Global leaders commit to accelerating global efforts to end AIDS as a public health threat by 2030
Global leaders commit to accelerating global efforts to end AIDS as a public health threat by 2030
13 December 2024
 To end AIDS, communities mobilize to engage men and boys
To end AIDS, communities mobilize to engage men and boys

04 December 2024
 Global celebrities unite behind UNAIDS’ call for world leaders to “take the rights path to end AIDS”
Global celebrities unite behind UNAIDS’ call for world leaders to “take the rights path to end AIDS”
01 December 2024
 Empowering youth to lead Togo’s HIV response
Empowering youth to lead Togo’s HIV response

31 October 2024




Feature Story
Thailand’s Mplus: HIV services delivered in style
13 December 2022
13 December 2022 13 December 2022“This isn’t your mother’s clinic!” said one amazed visitor.
From banners to brochures, all promotional materials are slick and cheerful. Smiling faces and toned torsos are everywhere. A purple colour scheme covers the whole building. Even files and staff face masks are colour coordinated. A pair of Facebook Live hosts have the good looks and energy of K-pop stars. And the organization’s slogan is decidedly upbeat: “where community fulfills your happiness”.
Over almost two decades, Thailand’s Mplus Foundation has refined a unique approach to providing comprehensive HV services to key population clients including men who have sex with men and transgender women.
Their method goes far beyond a cool brand identity. Mplus has leveraged domestic and international partnerships to create a key population-led health service with impressive results. They dispense more than half of the PrEP in Thailand’s Chiang Mai province.
This year they tested 95% of the almost 8000 people they reached with face-to-face services. Of those who tested positive, 91% were placed on treatment while the other 9% are in follow-up case management. And 100% of their clients who received viral load testing were found to be virally suppressed.
“Community organizations can best reach key populations to receive services. We find that people who do not want to get tested at the hospital are comfortable with peers who they know understand their life,” explained Pongpeera Patpeerapong, Director of the Mplus Foundation.
Since its formation in 2003 Mplus has evolved to deliver a full range of services. They now have health centres in four provinces, while their mobile testing units serve clients in another five districts. They support a local hospital in each province, linking people to care and helping them with adherence. Mplus provides rapid testing, CD4 and viral load monitoring, and is also authorized to dispense medication. A small fleet of motorcycles even makes PrEP deliveries to clients in remote areas.
Both their online and offline engagements are anchored by a peer-led strategy. Their social media presence is commanding—everything from Twitter to Tik Tok. There are closed Facebook groups and special applications for clients to connect with community. Offline, they go beyond information booths to host parties and sport meet-ups. These aren’t just bonding exercises. Clients book appointments online and face-to-face interactions usually result in receiving an HIV test.
Mplus also provides technical assistance to other countries. It has supported an organization in Laos with online interventions and helped community groups in Cambodia develop campaigns to promote PrEP.
They played a key role in advocating nationally for the accreditation of community health workers. All Mplus staff are certified by the Department of Disease Control following a rigorous programme of study, evaluation and practice.
The programme continues to progress. Mplus is strengthening their mental and emotional health support offering, and is working towards becoming certified to provide HIV and sexually transmitted infection (STI) treatment.
While in the past the programme was more heavily funded by the U.S. President's Emergency Plan for AIDS Relief through the United States Agency for International Development, today half of their investments come from branches of the National Health Security Office.
“Domestic funding is very important to develop our systems,” Mr. Patpeerapong said. “Community-based organizations have to be able to access domestic funding to cover more issues, including stigma and discrimination.”
Empowering key population-led health services has been crucial in improving Thailand’s HIV programme results. One of five people living with HIV in Thailand were identified and referred by a key population-led health service under the domestic health financing scheme. Four out of five people on PrEP in the country are served by community-led organizations. These services play a critical role in Thailand’s strategy of Reach, Recruit, Test, Treat, Prevent, Retain.
“Thailand is well-positioned to be a leader in addressing the need for a sustainable community-led response as a critical part of the health infrastructure,” said UNAIDS Country Director for Thailand, Patchara Benjarattanaporn. “By creating an enabling system for health outreach we can address the challenge of late diagnosis and better reach key population communities with services.”
Thailand has integrated HIV services into its Universal Health Coverage scheme and increased investments in key population- and community-led health services. UNAIDS Programme Coordinating Board (PCB) members visited Mplus and other community-led health services ahead of the 51st PCB meeting in Chiang Mai, Thailand.
Region/country
Related


Press Statement
UNAIDS welcomes the appointment of Erika Castellanos as Executive Director of GATE
13 December 2022 13 December 2022GENEVA, 13 December 2022—UNAIDS warmly welcomes the appointment of Erika Castellanos as the new Executive Director of GATE (Global Action for Trans Equality). GATE works to ensure justice and equality for trans, gender diverse and intersex communities through strategic partnerships with diverse global entities, including UNAIDS and other United Nations bodies and mechanisms.
Born in Belize, Erica started her activism focusing on the rights of people living with HIV and sex workers. She brings to her work her lived experience as a transgender woman living with HIV and as a member of different communities of key populations.
“Erika Castellanos is an internationally recognized and highly respected HIV and human rights activist. UNAIDS appreciates our partnership with Erika as a civil society delegate to our Programme Coordinating Board" said Winnie Byanyima, UNAIDS Executive Director. “GATE’s work as a trans-led organization has been critical to foster the engagement of trans, gender diverse and intersex communities in the AIDS response. We look forward to continuing our work with Erika and GATE in addressing the inequalities affecting these communities”.
Erika Castellanos joined GATE in April 2017 as Director of Programs. In February 2022, she took the role of Interim Executive Director during which time she has continued to solidify GATE’s position as a global leader in trans, gender diverse and intersex advocacy.
Erika has served various positions at national, regional and global levels including as Executive Director of the Collaborative Network for Persons Living with HIV (C-NET+) – Belize, Vice-Chair of the Board of the Global Network of People Living with HIV (GNP+), board member of the HIV Justice Network and co-chair of the ViiV Positive Action program for men who have sex with men and transgender people. In 2018, Erika was the first openly transgender advocate to be appointed to the Board of the Global Fund, as part of the communities delegation.
Erika will begin her new role as GATE’s Executive Director on 1 January 2023.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Our work




Press Release
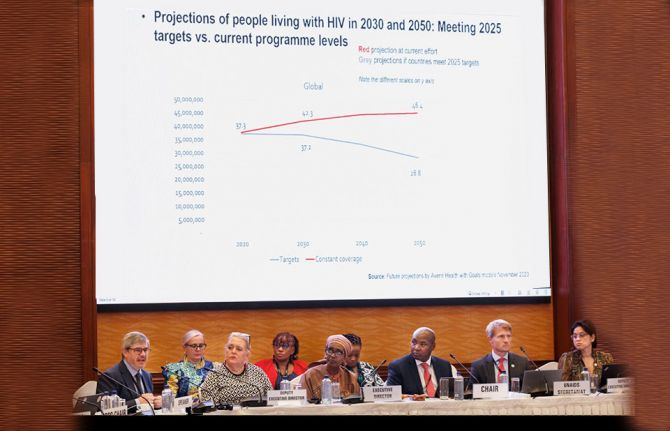
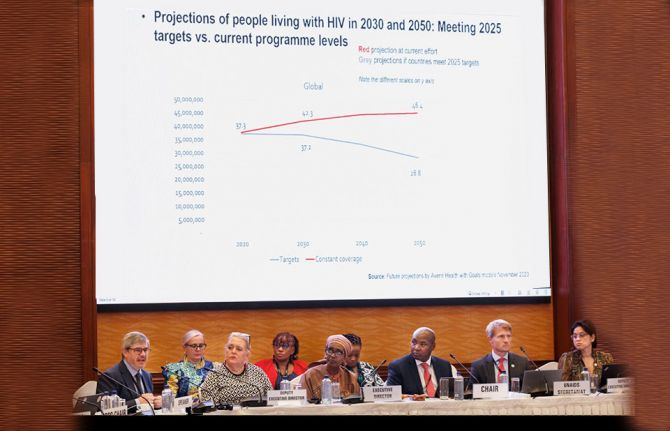
Pandemics can only be defeated if communities are supported to lead, say governments, NGOs and UN
15 December 2022 15 December 2022CHIANG MAI, THAILAND, 15 December 2022—Community-led responses are a critical part of the AIDS pandemic response, and must be prioritised in resourcing. The approach, set out by governments, civil society organisations and United Nations agencies at an international meeting on AIDS in Chiang Mai, Thailand, will also be key for tackling other pandemics and for preparing for the pandemics to come, delegates said. The meeting saw the first international definition of a community-led response to a pandemic, published after a two-year consultative process that brought together 11 governments, representing each region of the world, and 11 civil society representatives. This UNAIDS multi-stakeholder task team on community-led responses was co-convened by the World Health Organization and United Nations Development Programme, and presented outcomes to the 51st Programme Coordinating Board meeting of the UN Joint Programme on HIV and AIDS.
Using the new definitions and recommendations, German Federal Health Minister Prof. Karl Lauterbach and the UNAIDS Executive Director Winnie Byanyima published an article in The Lancet today calling for inclusion of comprehensive “community pandemic infrastructure” in pandemic prevention, preparedness and response in new planning, international agreements, and financing. In it, the leaders show that strong community infrastructure, working synergistically with government, is a necessary but neglected element of effective pandemic prevention, preparedness, and response. Using evidence from AIDS, mpox, COVID-19, and Ebola, the authors describe how community-led organisations bring trust, communications channels, and reach to marginalised groups that complement government roles and improve equity.
The new international definitions and recommendations can help planners and funders for AIDS and other pandemics identify the elements of an effective community response. Community-led organizations, defined as "groups and networks, whether formally or informally organized ... for which the majority of governance, leadership, staff, spokespeople, membership and volunteers, reflect and represent the experiences, perspectives, and voices of their constituencies and who have transparent mechanisms of accountability to their constituencies,” form a backbone of that response. Crucially, it is noted that "not all community-based organizations are community-led.”
"While what is most often understood as infrastructure – like labs and hospitals – are important, also essential to effective pandemic response is the community infrastructure which includes people to do outreach, trusted voices who can speak to excluded communities, independent accountability mechanisms, and participation in decision-making,” explained Dr Matthew Kavanagh, UNAIDS Deputy Executive a.i for Policy, Advocacy and Knowledge. “This task team of governments, civil society, and international organizations has given important new tools to support the building and monitoring of community-led capacity. We will only be able to end AIDS and stop other pandemics by ensuring that this community infrastructure is intentionally enabled, strengthened, monitored, and resourced.”
The United Nations Joint Programme on HIV/ AIDS (UNAIDS) Board meeting in Chiang Mai included dialogue between member states and non-state participants on how to develop laws and policies to facilitate community-led response. The recommendations of the multistakeholder task team include developing better systems for financing community-led organisations, which often face legal, capacity, and eligibility barriers to national and international financing mechanisms; monitoring community-led capacity; and integrating data generated by community groups into response management.
To end the AIDS pandemic, board members pointed out, community responses to HIV must be integrated into all levels of countries’ AIDS strategies including planning, budgeting, implementation, monitoring and evaluation.
The principles developed apply not only to AIDS. "Stopping COVID-19, mpox, and Ebola, and preparing for the next pandemic, all require that partnership of government and community together. The newly agreed framework for defining and measuring community-led responses make us better equipped to address the inequalities that are holding back progress in ending AIDS,” said Dr Kavanagh.
In Thailand, as delegates saw for themselves first hand, key-population-led health services have reached people at increased risk of HIV, achieving among the most equitable HIV responses in the region. In South Africa, community leaders with Ritshidze, which represents people living with HIV, visit clinics and communities to assess COVID-19, HIV, and tuberculosis services and hold administrators accountable for addressing issues such as long waiting times or confidentiality gaps that keep some people away from health services. Amid war, Ukraine’s 100% Life, a network of people living with HIV, has used peer networks to communicate with displaced people, delivering medicines, food, and emergency assistance.
"International pandemic agreements and funding should include specific goals for community-led capacity," said Dr Kavanagh. "To be effective, pandemic responses need to move beyond one-way communications to bring communities into decision making at all levels. Community leadership is not mere nice-to-have. It is essential for ending pandemics."
The Lancet article marking the occasion by the German Health Minister and the UNAIDS Executive Director is here.
The report presented at the UNAIDS Programme Coordinating Board meeting is here.
Resources on Community Led Pandemic Response are here.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Our work
Communities make the difference



Feature Story
The power of bringing together government and community HIV services
15 December 2022
15 December 2022 15 December 2022The Sanpatong Hospital in North Thailand has reinvented and refined its HIV programme for more than three decades. It began attending to people living with HIV in 1989, and in 1996 started offering antiretroviral treatment.
“We have patients who have been with us for 30 years,” says Dr Tawit Kaewprasert, Deputy Director of Provincial Public Health Office and Director of Sanpatong Hospital.
In the last five years the hospital has not had a single case of mother-to-child HIV transmission. An impressive 96% of people on treatment who received viral load tests there this year were virally suppressed, with 98% of those patients being undetectable. Management speaks about the 92% retention rate for clients who were on treatment in 2022 in terms of how those results can be improved.
“We have not achieved that target just yet,” Dr Manusin Kongka says, referring to the proportion of people who stayed on antiretroviral therapy. “But we can reach the target and even achieve beyond 95%.”
The team even aims to achieve 100% viral suppression among people who have been on treatment for at least five years. The current 96% result isn’t considered to be good enough.
This ambitious goal-setting flows from the National HIV Policy and Thailand’s commitment to end AIDS by 2030 through a well-articulated strategy to reach, recruit, test, treat and retain people in care, while also working to prevent new infections.
Of course the strategy relies heavily on Sanpatong and institutions like it. This 130-bed facility boasts a central lab that serves surrounding hospitals in Chiang Mai, Lamphun and Mae Hong Son with HIV diagnosis, CD4, viral load monitoring and some opportunistic infections testing.
Their approach includes the adoption of HIV response best practices including PrEP, index testing and same-day treatment initiation.
“Patients can start treatment before they even get their CD4 result,” Dr Kongka explained.
All staff have received anti-stigma training as well as orientation around the U=U, undetectable = untransmittable, initiative. The facility uses a differentiated approach for antiretroviral treatment delivery. Depending on their health status, some clients can collect multiple month dispensing at district health promoting hospitals while others can receive their medicine by mail.
But a major key to Sanpatong’s success is the linkages it has made with groups of community-led organizations to drive case detection, linkage to care, psychosocial support and the monitoring of services. The Hospital works with Mplus, CAREMAT and FHI360 on prevention, testing and retention in care. Organizations of people living with HIV run support groups. The Community Led Monitoring team even helps primary care nurses to contact patients who have been lost to follow up and conduct home visits. The people living with HIV network collaborated with key community-based organizations in Chiang Mai to conduct community-led monitoring to improve the quality of HIV services at the Sanpatong hospital.
“Our collaboration with community organizations increases awareness about HIV, improves quality of care and access to care, decreases the waiting in community clinics and increases continuity of care for HIV patients,” said Ms Sineenuch Suwansre, HIV Coordinator.
This close collaboration with communities is enhanced by the Thailand Government’s move to integrate HIV services into the Universal Health Coverage scheme. Now certified organizations and lay HIV service providers can access domestic financial support within the national health infrastructure.
“Universal Health Coverage is a mechanism for the sustainable financing of HIV prevention as well as sustainable financial support to key population- and community-led health services. The Thai government’s move to fund Community-led Health Services as an element of the mainstream public health system is a win for people living with HIV, for HIV prevention and for sustainability,” said UNAIDS Thailand Country Director, Patchara Benjarattanaporn.