Condoms

Press Statement
UNAIDS urges countries to invest in HIV prevention as key to ending AIDS
13 February 2025 13 February 2025Despite proven effectiveness, UNAIDS is alarmed by a decrease in condom use in several countries
Geneva, 13 February 2025– On International Condom Day, UNAIDS and partners are calling for HIV prevention efforts to be stepped up. In 2023, around 3,500 people became newly infected with HIV every day, bringing the total number of people newly infected in 2023 to 1.3 million.
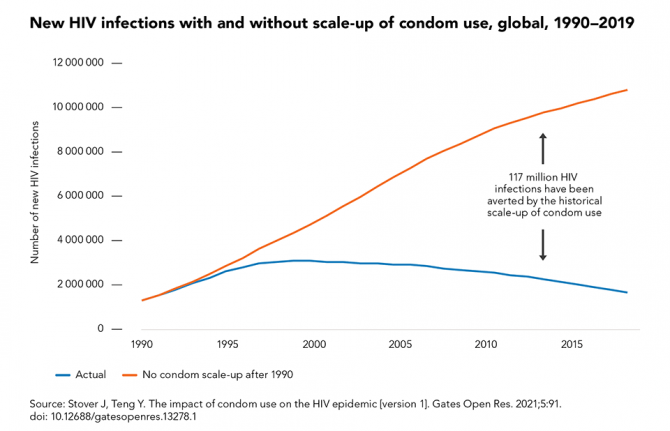
One of the most effective, low-cost HIV prevention tools available today are condoms which are 98% effective when used correctly and consistently. Condom use has averted an estimated 117 million new HIV infections globally from 1990 to 2019 however, new data reveal that there has been a decline of 6-15% in condom use in a number of countries, according to the Demographic and Health Surveys (DHS), a Condom Landscape Analysis, and the World Health Organization (WHO.)
For the past few years, the estimated global public sector and subsidized condom procurement declined by an average of 30% from peak procurement in 2011. This decline occurred despite the population in Africa growing to an estimated 400 million since 2010. As a consequence, fewer free or subsidized condoms are available per capita in Africa now than a decade ago.
"Condoms are a critical part of a comprehensive approach to HIV prevention and public health.. We also want to make sure medical breakthroughs like long-acting HIV medicines are affordable and accessible to all to give people most at risk additional HIV prevention options,” said Angeli Achrekar, UNAIDS Deputy Executive Director for Programmes.
Public and international investment in condom distribution, education, and social marketing has decreased in recent years. As a result, a new generation of young people has not been exposed to condom promotion.
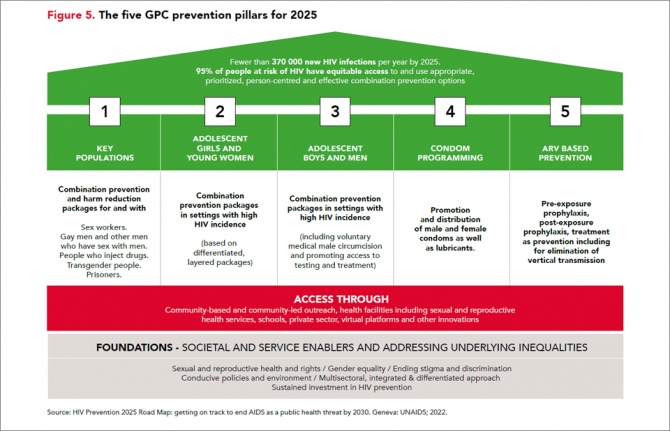
As new drugs and injectable HIV prevention methods gain ground in the next few years, condoms as well as PrEP (pills for people who may be at risk of acquiring HIV), voluntary medical male circumcision and treatment remain essential to achieving global health targets related to HIV and sexual and reproductive health.
Your Health. Your Power. Your Choice. Your Future.
International Condom Day is a reminder of the importance of protecting one’s own health. This year's theme focuses on the importance of ensuring equitable access to condoms, combating myths and misconceptions, and encouraging open conversations about preventing new HIV infections.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Watch: The truth about condoms
Our work
Documents
2024 global AIDS report — The Urgency of Now: AIDS at a Crossroads
22 July 2024
This UNAIDS 2024 report brings together new data and case studies which demonstrate that the decisions and policy choices taken by world leaders this year will decide the fate of millions of lives and whether the world’s deadliest pandemic is overcome. Related links: Press release | Special web site | Executive summary | Fact sheet | Video playlist | Epidemiology slides | Data on HIV | Annex 2: Methods Regional profiles: Asia and the Pacific | Caribbean | Eastern Europe and Central Asia | Eastern and Southern Africa| Latin America | Middle East and North Africa | Western and Central Africa | Western and Central Europe and North America Thematic briefing notes: People living with HIV | Gay men and other men who have sex with men | Transgender people | Sex workers | People who inject drugs | People in prisons and other closed settings | Adolescent girls and young women | Other translations: German
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025
 UNAIDS urges that all essential HIV services must continue while U.S. pauses its funding for foreign aid
UNAIDS urges that all essential HIV services must continue while U.S. pauses its funding for foreign aid

01 February 2025


Press Release
Reductions in new HIV infections in several Global HIV Prevention Coalition countries, but global progress needs to be accelerated
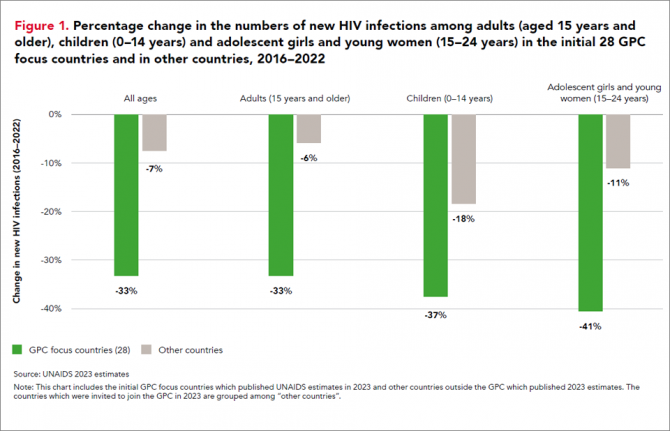
13 March 2024 13 March 202413 March 2024—A new report, HIV Prevention: From Crisis to Opportunity shows that HIV infections continue to decline in countries that are part of the Global HIV Prevention Coalition (GPC) faster than in the rest of the world.
Eleven GPC focus countries have reduced their annual number of new HIV infections by at least 66% since 2010. By comparison, the average reduction in new HIV infections since 2010 globally is 38%. The GPC is a coalition of 38 countries working together to accelerate declines in new HIV infections to achieve the target of having 95% of the people who are at risk of HIV accessing effective combination prevention options.
The GPC countries that have prioritised primary prevention and treatment and that have focused on reaching people most at risk have secured the strongest consistent declines in new HIV infections.
Globally, progress in HIV prevention has been highly uneven and a majority of the world’s countries are not currently on track to achieve the 2025 targets. Indeed, several countries are experiencing prevention crises with low access to services and face record rising new HIV infections.
“The findings of this report offer crucial lessons for action,” said Angeli Achrekar, Deputy Executive Director Programme, UNAIDS. “The report shows that sustained political leadership, investment in effective HIV prevention programmes, and an enabling policy environment are crucial to end AIDS as a public health threat by 2030.”
Declines in new HIV infections have been boosted by the cumulative impact of combination HIV prevention options and increased access to antiretroviral treatment which has also increased viral suppression in people living with HIV. People who are on treatment and are virally supressed cannot transmit HIV.
“It’s remarkable to see what has been achieved in the AIDS response in the past 20 years. But the progress to date has not been equitable and is not yet sustainable, and we must never confuse progress with being sure of success,” said Mitchell Warren, GPC co-chair and Executive Director, AVAC. “Our progress is fragile, and what we’ve achieved today could slip away even more quickly than it was achieved if we let complacency take hold.”
Key populations and adolescent girls and young women are still at high risk of new infections
HIV incidence remains unacceptably high among populations where gaps in HIV prevention investments persist. This includes key populations in all regions globally and adolescent girls and young women in parts of sub-Saharan Africa.
Around 3100 young women and girls aged 15-24 became newly infected with HIV every week in sub-Saharan Africa in 2022 and HIV incidence declined less rapidly than it has among young men. Only 43% of the sub-national areas in which there is elevated HIV incidence among young women are being reached with dedicated prevention programmes for young women.
Although GPC countries have shown solid gains in reducing new HIV infections, challenges remain worldwide in reaching key populations most at risk of new HIV infections including men who have sex with men, sex workers and people who inject drugs. Every week, more than 11 000 new HIV infections occur among key populations and their sexual partners globally.
Only 44% of sex workers, 28% of gay men and other men who have sex with men, and 37% of people who inject drugs accessed two or more HIV prevention services in the previous three months according to median values reported by GPC countries ––against a target of 90%.
HIV prevention is being obstructed by shortfalls in prevention financing, and by punitive laws. Social stigma, violence, discrimination and social exclusion are barriers to key populations’ access to health-care services and information, exacerbating their risk of acquiring HIV. Law reform is a crucial enabler of prevention programmes. Protecting the human rights of everyone is vital for protecting the health of everyone.
Investments in both condom and voluntary medical male circumcision programmes, which are both effective in preventing HIV, have fallen in some of the countries with the largest HIV epidemics. In addition, breakthrough HIV prevention options such as pre-exposure prophylaxis (PrEP), medicine to prevent HIV, are still only available to a small fraction of the people who need them.
There are unprecedented opportunities for HIV prevention in 2024. There is a growing array of prevention options including existing tools and new long-acting prevention technologies, as well as country examples of how to implement prevention at scale and increase choices available to communities.
HIV Prevention programmes need to be at scale, efficient and equitable. The actions that are needed for success and sustainability are known, have been shown to work, and have been agreed: collaborate, follow science, tackle inequalities, protect everyone’s rights, let communities lead, and invest in what is needed. Sliding back on resourcing or inclusion would hurt everyone. Solidarity will benefit everyone. Communities, countries and international partners can prevent new infections – together.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Our work
Documents
HIV prevention: from crisis to opportunity — Key findings from the 2023 Global HIV Prevention Coalition scorecards
13 March 2024
The Global HIV Prevention Coalition focus countries are progressing unevenly towards the goal of reducing HIV infections to levels that would no longer constitute a public health threat. The biggest declines are occurring in eastern and southern Africa and, to a lesser degree, in western and central Africa. Expansion of access to effective ART, combined with an ongoing focus on primary prevention, are driving those achievements.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025




Feature Story
Love and condoms: broadcast on the importance of condoms in eastern Europe and central Asia
05 January 2022
05 January 2022 05 January 2022On the eve of World AIDS Day, the Russian language social media network OK.RU hosted a live broadcast, Telling the Truth, as part of an education project that has been run by UNAIDS and the United Nations Educational, Scientific and Cultural Organization since 2015. The show was organized in collaboration with a popular magazine, Domashniy Ochag, and was devoted to the use of condoms and the link to the HIV epidemic in eastern Europe and central Asia.
During the broadcast, which was watched by more than 1 million people, experts and celebrities discussed the most common myths, misconceptions, difficulties and fears connected to condom use.
Before the broadcast, an online survey of 1050 people aged 18 to 60 years was conducted on what Russian Internet users think about protection against sexually transmitted infections and what they consider to be safer sex. The study found that 87% of respondents had had sex without a condom, with older respondents reporting higher rates of sex without a condom.
“HIV has already reached the general population in this region. Almost 70% of all new HIV infections have been linked to heterosexual sex in recent years. At-risk people include single women aged more than 35 years and men and women who no longer worry about contraception and therefore do not use a condom,” said Natalya Ladnaya, Senior Researcher at the Central Research Institute of Epidemiology, Rospotrebnadzor.
Among the reasons for unprotected sex, the respondents most often named “awkwardness of discussing it with a partner”, which was reported by 41% of the respondents. In addition, “trust in a partner” (35%), “discomfort during intercourse” (20%), “fear of spoiling romance” (31%) and “fear of being misunderstood by a partner” (19%) were listed among the reasons for not using a condom.
Appearing on the broadcast was Masha Godlevskaya, who has been living with HIV for 22 years. She works as a peer consultant for the EVA Association, which provides HIV services. She explained that many women who go to the EVA Association for a consultation are embarrassed to carry condoms because of the stereotype that having a condom available means that they are available and ready for sex.
“Both women and men are victims of this story,” said Ms Godlevskaya. “If a man insists on having sex without a condom, the woman should be ready to say: “I don’t want to. I don’t want to offend you, but no sex without a condom.””
“We help women believe in themselves, work with a psychologist, fight back against their abusers, build new relationships where they can discuss everything frankly. I want our women to be able to defend their bodies, their rights, and be able to take their lives into their own hands,” she added.
Vera Brezhneva, UNAIDS Goodwill Ambassador for Eastern Europe and Central Asia, noted that many women vulnerable to HIV were born in the time of the Soviet Union, when there was no promotion of safer sex. “I didn’t know about HIV at all. Most of us at that time were afraid of pregnancy only. We believed in love as if love protects you from everything. We were not told that a condom is not protection against men or women but protection against infections.”
Ms Godlevskaya shared her story of becoming infected with HIV. “I was 16 years old. He was my first love, and, as it seemed to me then, the last one. It was a serious relationship, there was trust and we knew nothing about the need to use a condom.”
Marina Travkova, a family psychologist and sex therapist, noted that adolescents are vulnerable to HIV and other sexually transmitted infections. “They need help. There is nowhere to get reliable information. I am in favour of compulsory sex education in high school and for condoms to be available in school toilets. I always remind my sons before they go out: wallet, phone, brain, condom,” she said.
For a significant part of the population, especially young people, the cost of condoms is too high, noted Ms Ladnaya. “We are discussing these issues with partners, and we hope that there will be government programmes to support the production of condoms. There are nongovernmental organizations that provide condoms for free, but I believe that they should be available at every step,” she said.
Discussing the perception that sex with a condom is worse than sex without one, the reason that people often do not use condoms, the panellists noted that comfort might be related to the quality and size of a condom, as well as insufficient knowledge of how to use a condom and lubricant correctly.
Grisha Tumanov, a journalist and blogger and author of the Man, Where Are You Going? podcast, commented on a viewer’s question: “Is a condom needed if it’s love, which presupposes mutual trust.” He noted that, “We don't have a culture of speaking on sensitive topics, what you expect from relationships, including sexual relationships. And love does not absolve one of responsibility. This does not happen in adulthood. You are responsible for each other.”
Our work
Region/country
Related
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025

Update
Condoms are a critical part of combination prevention
22 November 2021
22 November 2021 22 November 2021When used correctly and consistently, male and female condoms and lubricant offer very high protection against HIV, sexually transmitted infections and unintended pregnancy. Condom use has had an enormous impact on the global AIDS pandemic: model simulations show that increased condom use since 1990 has averted an estimated 117 million new HIV infections, close to half (47%) of them in sub-Saharan Africa and more than one third (37%) in Asia and the Pacific.
If condom use rates are increased to reach 95% coverage of higher-risk sex acts by 2025 and all other prevention interventions remain at 2019 coverage levels, about one third of the required reductions in new HIV infections will be achieved. Consistent condom use, although possible, has proved difficult to achieve among all populations. Women in many countries, for example, need greater agency and support to negotiate consistent condom use. Where available, some people also choose other HIV prevention methods. Condoms alone, therefore, are not sufficient to control HIV epidemics. Full achievement of the 2025 prevention target of reducing annual new HIV infections to under 370 000 requires increased investment in combination HIV prevention to ensure access to and use of condoms as well as the full range of other prevention choices for 95% of people at risk of HIV infection.
Our work


Update
Condom use declining
23 November 2020
23 November 2020 23 November 2020The defunding of condom social marketing programmes and decline in sales of socially marketed condoms in sub-Saharan Africa is emblematic of a decreased focus on condom demand generation, reduced emphasis on condoms in family planning services and weak stewardship of condom programmes since 2010, leaving the world far off the 90% target for condom use.
A new generation of sexually active young people has not been exposed to the intense condom promotion that was in place a decade ago. Condom use at last higher risk sex reported by young women (aged 15 to 24 years) declined in five countries in western and central Africa and three countries in eastern and southern Africa. Condom use at higher risk sex among men (aged 15 to 49 years) also declined in five out of nine countries (compared to the previous survey). The use of condoms across all of western and central Africa and eastern and southern Africa remains far too low.
Our work
Documents
Condoms and lubricants in the time of COVID-19 — Sustaining supplies and people-centred approaches to meet the need in low- and middle-income countries — A short brief on actions, April 2020
06 May 2020
The aim of this brief is to ensure that the COVID-19 pandemic does not disrupt the supply of and demand generation for condoms. Sexual relations may be transformed in the new context of the pandemic, but they have not stopped. While access to male and female condoms has been critical in the global response to reduce HIV, sexually transmitted infections (STIs) and unintended pregnancies over the past three decades, these gains can be lost if condoms are not included in the essential commodities that are freely available to populations during the lockdown of countries. This brief for country condom programme managers and experts provides a summary of relevant actions to sustain supplies of male condoms, female condoms and lubricants, and to adjust approaches for condom promotion during the time of COVID-19.
Related
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025





Feature Story
Turning the tide of the HIV epidemic in Thailand
17 January 2020
17 January 2020 17 January 2020It is a morning like any other at the Thai Red Cross AIDS Research Centre, a civil society organization operating under the umbrella of the Thai Red Cross Society. In a building in the heart of Bangkok, nurses, doctors, counsellors and peer educators are busy with their daily work, providing HIV services for the 200 people who attend the Thai Red Cross Anonymous Clinic every day for medical check-ups, HIV tests and HIV prevention services, including condoms and pre-exposure prophylaxis (PrEP).
When he was 35 years old, Praphan Phanuphak―the Director of the centre, which he co-founded in 1989―discovered the first case of HIV in Thailand. “It happened by accident. A patient was referred to me to investigate why he had a recurrent fungal skin infection,” he recalled. “In February 1985, this patient was admitted with pneumocystis pneumonia. During that month, another man was referred to the hospital with generalized cryptococcus infection. Both were diagnosed with HIV. Since then, I have devoted my life to treating people living with HIV and developing solutions to expand access to HIV services in the country.”
Mr Praphan remembers that in the early days of HIV the response in Thailand faced several challenges. At the time, Thai law required hospitals to report the names of people diagnosed with HIV to the Ministry of Public Health, which contributed to increasing stigma and discrimination against people living with HIV. In response, the Thai Red Cross established the Thai Red Cross Anonymous Clinic, Asia’s first anonymous clinic, and advocated with the Thai Government to remove the reporting law. The Anonymous Clinic remains the most renowned centre providing voluntary HIV testing in the country.
“Until the beginning of 2000, antiretroviral medicines were not available through public health facilities in Thailand, and many people living with HIV could not afford to buy them,” said Mr Praphan. He said that in 1996 the Thai Red Cross AIDS Research Centre was the first to provide free antiretroviral medicines as part of its clinical trials through the HIV Netherlands–Australia–Thailand Research Collaboration.
“After years of despair, a time of hope finally came. For that, I want to thank Her Royal Highness Princess Soamsawali, who stood by our side by setting up a fund for the prevention of mother-to-child transmission of HIV in 1996, several years before the Thai Government started its successful prevention programme,” said Mr Praphan.
The AIDS response in Thailand has changed dramatically over the years. In 2006, Thailand integrated its HIV services, including antiretroviral therapy, into its universal health coverage scheme. Since 2014 Thailand has provided antiretroviral therapy for all regardless of their CD4 level. Everyone can access treatment for free, and people living with HIV are offered treatment immediately after diagnosis.
However, many people are starting antiretroviral therapy late. “We have the medicines, but many people are not being diagnosed fast enough,” warned Mr Praphan. Despite tremendous progress, the HIV epidemic is not yet over in Thailand. HIV remains concentrated among key populations: almost 50% of new HIV infections in 2018 were among gay men and other men who have sex with men. Low uptake of HIV testing among key populations is related to the acceptability of services and stigma and discrimination, which hinder access to HIV diagnosis, prevention and care.
“From our experience, helping key populations to reach their peers and bring them to HIV drop-in centres, where they can be tested, is the best way to detect and diagnose people living with HIV early enough,” said Mr Praphan, who successfully advocated to amend Thai law to allow certified lay providers from key populations to provide a number of HIV services.
The Thai Red Cross AIDS Research Centre’s approach focuses on undertaking pilot projects to generate evidence to inform national planners and policymakers. That evidence provides a foundation for national acceptance and the roll-out of innovation on a national scale.
Taking the lead in reaching out to key populations, the centre has been offering PrEP to people at substantial risk of HIV since 2014 through projects such as the Princess PrEP Programme. In October 2019, Thailand introduced PrEP under its universal health coverage benefits package as a pilot phase in efforts to scale up PrEP nationwide.
Mr Praphan believes that policymakers and programme implementers should understand that, “We cannot continue to do business as usual. In Asia and the Pacific, several countries are still either sceptical or conservative in terms of promoting the necessary approaches to change the course of the HIV epidemic.” He thinks that the region cannot achieve the 90–90–90 targets by 2020 at the current pace. “We need to think out of the box and look at what other countries are doing that can be taken as a model. This is how we can move faster on our way towards ending AIDS as a public health threat.”
Region/country
Related


Feature Story
Not enough condoms
29 April 2019
29 April 2019 29 April 2019Condoms, if easily available and used consistently and correctly, are one of the most effective and inexpensive methods available to reduce the sexual transmission of HIV and other sexually transmitted infections and to prevent unintended pregnancy. Despite this, condoms are still not sufficiently available to those who need them in many countries with a high burden of HIV.
The estimated condom need in 47 countries in sub-Saharan Africa in 2015 was 6 billion male condoms; however, only an estimated 2.7 billion condoms were distributed.