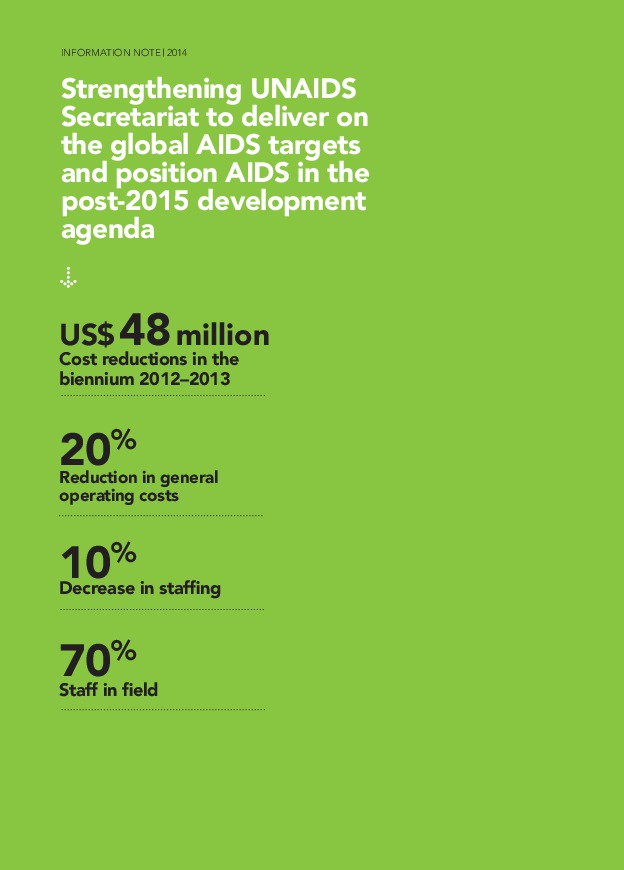
Health systems strengthening








Publications







Publications


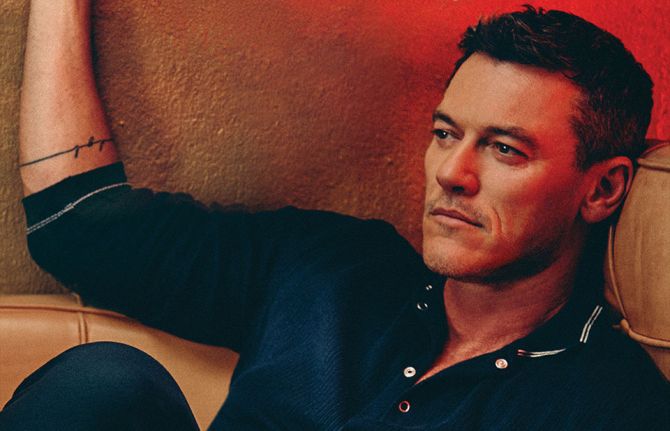
L to R: Chair of the Board of Directors for the African Society for Laboratory Medicine, Trevor Peter; Chief Executive Officer of the African Society for Laboratory Medicine, Tsehaynesh Messele; UNAIDS Executive Director, Michel Sidibé; and Director of UNAIDS Regional Support Team for Eastern and Southern Africa, Sheila Tlou.
Update
UNAIDS and the African Society for Laboratory Medicine formalise partnership to improve laboratories and access to HIV testing
09 December 2013
09 December 2013 09 December 2013UNAIDS and the African Society for Laboratory Medicine (ASLM) signed a Memorandum of Understanding on 8 December to collaboratively improve access to HIV testing and strengthen health systems throughout Africa.
The aim of the collaboration is to improve access to inexpensive, accurate and simple HIV and TB diagnostics to ensure the long-term effectiveness and quality of antiretroviral therapy (ART), which is key to achieve the objectives of the UNAIDS 2015 Treatment Initiative.
The ASLM is committed to supporting efforts to expand access to key diagnostics through its 2020 strategic vision—strengthening laboratory workforce development, improving laboratory accreditation, harmonizing regulatory systems and strengthening national and regional laboratory networks.
Quotes
“We must ensure people living with HIV have access to quality laboratory services in Africa. We continue to fail children because we do not have adequate diagnostics and laboratory capacity. HIV testing needs to be simpler, quicker, more cost-effective and more widely available, so that we can fast-track lifesaving treatments to our communities.”
“Coordinated efforts, based on best practices, are essential for building effective HIV programmes. Effective implementation can produce significant benefits for millions of patients without access to HIV testing and will substantially improve the effectiveness of HIV treatment and prevention services.”
Multimedia
Multimedia
Related
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025
 Status of HIV Programmes in Botswana
Status of HIV Programmes in Botswana

20 February 2025
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


At the launch, a Russian-made mobile clinic and diagnostic centre was presented to the Government of the Khatlon Region.

Local citizens in the city of Kurgan-Tube during the public launch of the Technical Assistance Programme in Tajikistan.
Feature Story
Technical Assistance Programme for Countries of Eastern Europe and Central Asia in Combating Infectious Diseases launched in Tajikistan
12 September 2013
12 September 2013 12 September 2013The national launch of the Technical Assistance Programme for Countries of Eastern Europe and Central Asia in Combating Infectious Diseases took place in the Tajikistani city of Kurgan-Tube, in the Khatlon Region on 10 September 2013.
The Technical Assistance Programme, supported by a three-year grant of US$ 16.5 million from the Russian Government, aims to strengthen health systems, ensure better epidemiological surveillance of HIV, and promote the scale up of HIV prevention programmes among key populations at higher risk in Armenia, Kyrgyzstan, Tajikistan, and Uzbekistan.
The Programme is supported by the contribution of the Russian Government as a leading partner for health and development in countries of the Commonwealth of Independent States, and is being implemented by UNAIDS, in partnership with the non-governmental organization 'AIDS Infoshare'.
The launch was attended by representatives of the Russian Presidential Administration, the Russian Ministry of Foreign Affairs, the Ministry of Health of Tajikistan, the Government of the Khatlon Region, the City of Kurgan-Tube, the Ministry of Health of Armenia, as well as representatives from UNAIDS, 'AIDS Infoshare' and civil society organizations from Russia and Tajikistan.
The HIV epidemic in Tajikistan, affects mainly people who use drugs and now the number of new HIV infections is growing among people migrating abroad for work. Knowledge about HIV prevention remains limited among migrant workers and access to HIV services are not widely available upon their return as most live in rural and hard to reach regions of the country.
At the launch, a Russian-made mobile clinic and diagnostic centre was presented to the Government of the Khatlon Region. Equipped with the latest in medical equipment and diagnostic systems, the clinic will provide populations at higher risk of HIV infection in the Khatlon Region with access to integrated HIV testing, counselling and other forms of medical diagnostics and treatment.
Quotes
Through this programme Tajikistan will reach the communities most at risk of HIV infection and will break the trajectory of the epidemic.
The people of Tajikistan are very grateful for the timely, generous support of the Russian Government in this important programme.
This initiative is a new level of cooperation in the positive history of economic and cultural relations between the people of the Russian Federation and the people of the Republic of Tajikistan.
Russia considers this to be a model of donor aid effectiveness that will be promoted during Russia's Presidency of the G8.
Migration should never be a barrier to access quality health services or learn one's HIV status. This mobile clinic will bring the latest HIV information and medical technology to communities in Tajikistan that are most at risk of HIV infection.
Related
 Status of HIV programmes in Tajikistan
Status of HIV programmes in Tajikistan

05 March 2025
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025

Press Release
African leaders embrace shared responsibility and call for innovative solutions to accelerate the response to AIDS, tuberculosis and malaria
27 September 2012 27 September 2012African leaders gather to review progress made in the implementation of the 2001 Abuja Declaration on HIV/AIDS, Tuberculosis and Other Related Infectious Diseases and call for sustainable strategies to advance health towards 2015 and beyond.

L to R: President of Benin, Yayi Boni, United States Secretary of State Hillary Rodham Clinton and UNAIDS Executive Director Michel Sidibé
Credit: UNAIDS/B.Hamilton
NEW YORK/GENEVA, 26 September 2012— African leaders gathered in New York on the sidelines of the 67th Session of the United Nations General Assembly to discuss the African Union (AU) Roadmap. This initiative outlines long-term sustainable strategies to finance and provide access to HIV treatment and prevention services and other health services in Africa as called for in the Millennium Development Goals.
“Ten years after Abuja, millions of lives have been saved and Africa has prospered,” said President of Benin Boni YAYI, in his capacity as Chairperson of the African Union. “These foundations have to be made permanent for this generation and for all our future generations.” President Boni YAYI presented the African Union’s Roadmap for Shared Responsibility and Global Solidarity for AIDS, Tuberculosis and Malaria.
Shared responsibility and global solidarity
President Joyce Banda of Malawi embraced the concept of shared responsibility. “I am fully committed to mobilizing additional domestic resources while ensuring efficient use of external funds,” she said in a statement of support to meeting. President Banda also highlighted her country’s pioneering work to “ensure all HIV positive pregnant women, irrespective of their CD4 count, commence antiretroviral therapy and take HIV treatment for the rest of their lives.”
The transformation of access to health in Africa has come from inspired African leadership coupled with strong international support. Health investments, from funders and domestic resources have expanded manifold in Africa. Weak health systems have been replaced with a greater focus on human resources and ingenuity to provide health care in remote areas.
United States Secretary of State Hillary Rodham Clinton addressed the gathering and recognized the renewed commitment by the African Union to the AIDS response. “If every nation devastated by HIV follows the example of many of the leaders in this room and steps up to shared responsibility, we won’t just keep up our momentum—we will accelerate our progress and move even faster toward the day when we can announce the birth of an AIDS- free generation,” she said.
Towards the 2015 goals and the post 2015 agenda
With three years to go to meet the Millennium Development Goals, as well as the global AIDS targets agreed to in the 2011 United Nations Political Declaration on AIDS, participants echoed the need for strong political leadership and enhanced country ownership.
As a first step, African leaders agreed to accelerate the implementation of the Roadmap on Shared Responsibility and Global Solidarity for AIDS, Tuberculosis and Malaria adopted by the African Union in July 2012.
“Africa has not only shown that it cares but that it has increased its capacity to provide health care for its people. Millions of lives have been saved as investments into healthcare have increased—both domestic and international,” said Michel Sidibé, Executive Director of the Joint United Nations Programme on HIV/AIDS (UNAIDS) who moderated the high-panel debate. “For every African to realize their right to health, a new paradigm of sustainable health services has to be put in place. For this we must secure the investments needed, secure good laws, secure the science, secure shared responsibility and global solidarity as well as secure access to lifesaving health services.”

United Nations Special Envoy for Global Education Gordon Brown speaking at the event.
A key to this agreement is advancing a new model of mutual accountability that can help unite African governments and their development partners in a series of practical actions and which will bring Africa closer to ending the AIDS epidemic. Data released this year by UNAIDS shows that scientific advances and improved programme practices have helped to reduce the number of new HIV infections and AIDS-related deaths. Life-saving HIV treatment is now reaching more than 8 million people around the world—more than 6 million of which are in Africa, the region most affected by the epidemic.
“This is the time for Africa to intensify its efforts and create a new international compact against AIDS,” said President Macky Sall of Senegal.
During the dialogue it was agreed that the capacity of AIDS Watch Africa be strengthened. It was also suggested that AIDS Watch Africa, the African body mandated to ensure accountability for action, create a new model of accountability in consultation with Africa’s development partners.
Sustainable and innovative health financing
The leaders, which also included the Presidents of Comoros, Equatorial Guinea and Namibia, the Deputy Prime Minister of Kenya and development partners including France, Sweden, Brazil, the African Union Commission, European Commission and World Bank, also discussed ways to ensure that health financing is adequate and sustained. In recent years many countries in Africa have adopted innovative ways of generating resources for health, beyond traditional means. For example, Rwanda and Uganda now place levies on mobile phone usage with proceeds supporting HIV programmes. Zimbabwe’s AIDS levy now provides about US$ 30 million as the country’s economy expands. Social health insurance is also being explored by many countries.
At the same time domestic investments for health have increased, but the majority of countries have not yet met the Abuja target of allocating 15% of government budget to health. Leaders at the meeting agreed that this goal should be maintained and all efforts be taken to achieve this target. However they also agreed that international investments, which have remained stable in recent years, must be sustained and increased. They also called for new and diversified sources of international investments—especially from countries with emerging economies.
Sustainable access to medicines
A majority of the pharmaceutical needs of Africa are met through imports. The need to boost local capacity to manufacture essential quality-assured medicines as well as developing regional markets for them, including through common regulatory frameworks was highlighted at the event.
“Africa must be a source of knowledge and science, not just needs and wants,” said President Moncef Marzouki of Tunisia. “We will make all efforts to ensure that Africa meets more of its pharmaceutical needs through increased local production.”
Getting to zero
“If every girl and every boy goes to school and is taught about HIV prevention we can reach the global goal of Zero new HIV infections, zero discrimination and zero AIDS-related deaths,” said Gordon Brown, the United Nations Special Envoy for Global Education. “To the UNAIDS vision of Zero if we add zero illiteracy, we can end AIDS faster.”
There are nearly 23.5 million people living with HIV in Africa. New HIV infections in the region have declined by 22% since 2001. By the end of 2011, an estimated 56% of people eligible for HIV treatment in sub-Saharan Africa were accessing it—with treatment coverage increasing by 22% across the region between 2010 and 2011.
Publications
Publications
- World leaders embrace the African Union Roadmap on AIDS, TB and malaria: Establishing Shared Responsibility and Global Solidarity as a vision for global health in the Post-2015 development agenda
- The Roadmap: Shared responsibility and global solidarity for AIDS, TB and malaria in Africa
- Africa in the lead
- AIDS Watch Africa: African High Level Advocacy & Accountability Platform to Combat HIV/AIDS, TB and Malaria
Related Information
Multimedia
Multimedia
Speeches
Press centre
Download the printable version (PDF)

Feature Story
The Dominican Republic to confront its HIV treatment gap
23 August 2012
23 August 2012 23 August 2012
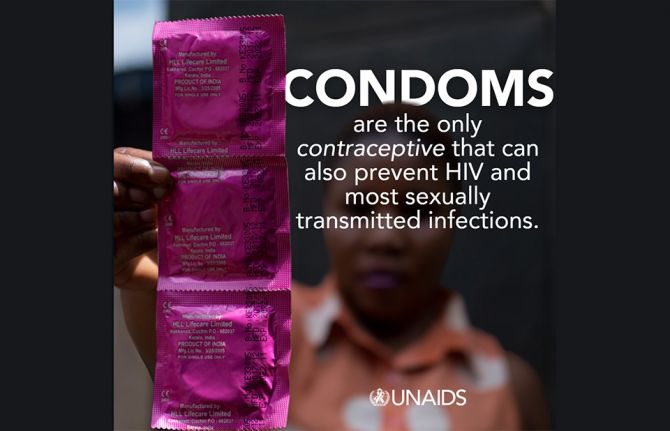
Image from an initiative by people living with HIV in the Dominican Republic launched to draw attention to the fact that the availability of generic drugs has significantly reduced treatment prices in the global market.
The Dominican Republic is one step closer to ensuring that all people living with HIV access treatment. The country’s National Social Security Council has established a commission to look into the technical, financial and operational implications of including antiretroviral therapy (ART) in the Basic Health Plan.
The establishment of the commission comes after a financial feasibility study about covering people living with HIV under the country’s family health insurance. The study was done in 2011 by the United Nations Development Programme (UNDP), United Nations Children’s Fund (UNICEF), Pan American Health Organisation (PAHO) and the Joint United Nations Programme on HIV/AIDS (UNAIDS).
The newly-established commission—whose membership includes several national health system offices in addition to regional and global partners such as PAHO and UNAIDS—is set to complete its work during the last quarter of 2012.
It is a step towards ensuring that treatment is maintained, and lives of Dominicans living with HIV are saved.
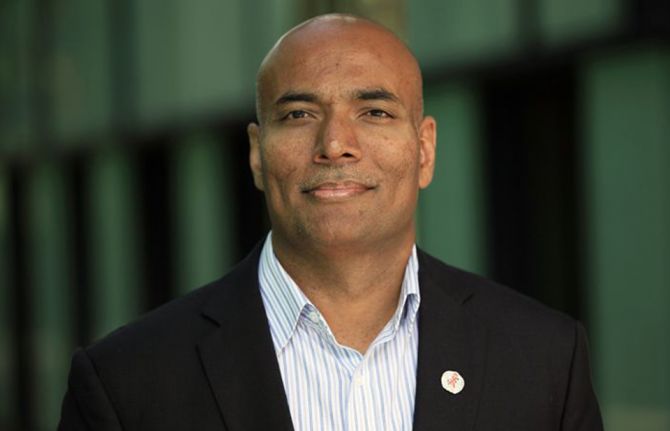
UNAIDS Caribbean Director, Ernest Massiah
According to UNAIDS Country Coordinator, Ana Maria Navarro, the development comes at a critical time and is a direct consequence of a feasibility study elaborated by United Nations agencies in the Dominican Republic. “This resolution brings us nearer to securing the sustainability of the AIDS response,” said Dr Navarro.
The Dominican Republic is classified as a middle-income country even though there are marked inequalities in income distribution. At present access to HIV treatment is completely financed by international donor agencies. While more than 20 000 people are currently receiving HIV treatment, more than 2 500 individuals known to be living with AIDS do not have access to life-saving drugs.
This is despite a guarantee of universal access to treatment for people living with HIV made in the country’s 2007 – 2015 National Strategic Plan on HIV and AIDS. The treatment gap also contradicts the principles of universality and equity that informed the 2001 reform of the Social Security System. Moreover, a new HIV law introduced last year provides for the comprehensive healthcare of people living with HIV.
But a 2002 regulation for the operationalization of the Basic Health Plan excludes coverage of antiretroviral drugs on the basis of their high cost. A primary objective of the feasibility study was to provide evidence that HIV treatment is not as expensive as local authorities believed.
“This is one giant step for the Dominican Republic,” said UNAIDS Caribbean Director, Ernest Massiah. “It is a step towards ensuring that treatment is maintained, and lives of Dominicans living with HIV are saved. People living with HIV can continue to work, support their families and participate in the simple joys of life to which we are all entitled. This is about respect, dignity and life.”
In April 2012, people living with HIV in the Dominican Republic launched an initiative to draw attention to the fact that the availability of generic drugs has significantly reduced treatment prices in the global market. The Dominican Network of People Living with HIV (REDOVIH+), Alianza Solidaria de Lucha contra el SIDA (ASOLSIDA), Fundación Grupo Paloma and Grupo Clara jointly launched a petition which called for the 2012 presidential candidates to address the financial sustainability issues related to their treatment ahead of elections at the end of May.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Comprehensive Update on HIV Programmes in the Dominican Republic
Comprehensive Update on HIV Programmes in the Dominican Republic

19 February 2025

Feature Story
Strengthening health systems: delivering on the broader health and development agenda
07 December 2011
07 December 2011 07 December 2011
UNAIDS Deputy Director, Programme Dr Paul De Lay and Ethiopian Minister of Health, H.E. Tedros Adhanom Ghebreyesus.
Credit: UNAIDS/J. Ose
“Health and Social Affairs: Making Health Systems Work to Effective HIV Response,” was the title of a ministerial panel held on the third day of the International Conference on AIDS and STIs in Africa (ICASA). The panel highlighted how the AIDS response has had additional benefits for the broader health and development agenda.
UNAIDS Deputy Director, Programme Dr Paul De Lay participated in the panel together with the Ethiopian Minister of Health, H.E. Tedros Adhanom Ghebreyesus, Director of the CDC Center for Global Health, Dr Kevin De Cock and the Executive Director of SAfAIDS Lois Chingandu.
Responding to the critics who say that the AIDS response has created vertical programmes at the expense of the broader health system, Dr De Cock asserted that, “there is evidence that the scale up of AIDS services has had a positive impact on health systems strengthening in the [African] continent.”
For example, the push for HIV treatment has focused attention to the lack of human resources, poor infrastructure, insufficient supplies and other related issues.
“It is time to take stock of the many vertical health initiatives that have produced measurable results but also created parallel structures, high net transaction costs, and fragmentation,” said Dr De Lay. “We strongly advocate for integrated approaches that maximize efficiencies and achieve positive health beyond HIV, in the broader health system,” he added.
It is up to us to work hard in our own capacity to reach the three zeros. The dependence syndrome can be broken down and communities should have the capacity to respond for themselves
Auxiria Mwanza from Zambia Red Ribbon Award winner 2010
The Ethiopian Minster of Health H.E. Ghebreyesus in his address stressed the importance of integration of services within health systems. “Strong health systems mean better results for HIV but also better results in other health related issues such as maternal health or immunization programmes.
For health systems to deliver results, Dr De Lay added, there is a need to address the legal, policy and regulatory environment as well as the social and cultural context which may act as barriers for people to access services.
Social change in the AIDS response has often been driven by civil society, and many lessons can be learned from this experience. There is still a need to put in place critical enablers for health systems, such strong advocacy to meet funding commitments, respect for human rights, and political commitment.
“Effective systems depend on effective governments and are based on the respect for human rights,” said civil society representative Ms Chingandu. “Health systems cannot be effective without a robust and accountable civil society,” she added.
Since the dawn of the AIDS epidemic, activist have not only generated investments in AIDS but have instilled more vigorous sense of accountability and urgency among in global and national leaders in delivering on the commitment of health for all.
The panel concluded that the AIDS response has had a far-reaching and unquestionable impact on health care globally: building infrastructure and systems, improving the quality of services, reaching socially marginalized and vulnerable groups, and engaging consumers.
External links
External links
Related
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025
 Status of HIV Programmes in Botswana
Status of HIV Programmes in Botswana

20 February 2025

Feature Story
Can MDG 6 be achieved with the Health Workforce we have?
09 June 2011
09 June 2011 09 June 2011
Credit: AMREF
If international aims such as achieving health-related Millennium Development Goals (MDGs) and universal access to HIV services are to be realized, the serious global shortage of health workers must be urgently addressed. This shortage has been severely exacerbated by the AIDS epidemic reducing staff numbers and significantly increasing the workload of those remaining.
At a side event during the High Level Meeting on AIDS in New York this week, the need to recognise human resources as a crucial element in the global AIDS response was explored in depth. Without sufficient human resources, countries' efforts to scale up comprehensive AIDS services will not be sustained, making it impossible to reach the MDGs.
The meeting, Can MDG 6 be achieved with the Health Workforce we have?, was jointly organized by the Global Health Workforce Alliance (GHWA), along with the Government of Brazil, the Commonwealth Secretariat, UNAIDS and the African Medical and Research Foundation (AMREF).
A lively panel discussion, including heads of state, senior representatives from donor and international organisations, civil society and the private sector, examined the interconnectivity of HIV and human resources and also shared best practices.
Joining discussants Mphu Ramatlapeng, both Global Fund Vice-chair and Lesotho’s Health Minister and Secretary Jarbas Barbosa, Brazil’s Secretary of Health Surveillance, were keynote speakers Dileita Mohamed Dileita, Prime Minister of Djibouti and Maxensia Nakibuuka, a Ugandan community health worker living with HIV. The session was moderated by Pulitzer prize-winning journalist Laurie Garrett, who is also Senior Global Health Fellow at the Council on Foreign Relations research centre.
Mr Dileita Mohamed Dileita highlighted the effects of an insufficient number of health workers, their uneven distribution, and limitations in their competencies in his own country, Djibouti. Dr Barbosa agreed that uneven distribution of staff is a major problem in Brazil.
Speaking as a community health worker Maxensia Nakibuuka from Uganda emphasized the difficulties she and her colleagues faced, “We are left to do it alone. Without system strengthening, without budgets; with nothing…We need to be recognized.”
According to Mphu Ramatlapeng, the Global Fund is helping countries meet their needs, with round 11 of Fund proposals including support for health workforce strengthening. She also stressed the crucial need for all stakeholders to work together.
The role of the private sector in offering support was examined. Michael Bzdak, Johnson & Johnson ‘s Director of Contributions and Community relations, spoke of their corporate social responsibility and building health care capacity, primarily in terms of leadership, management techniques and skills training.
Dr Sigrun Mogedal, former-Ambassador, HIV/AIDS and Global Health Initiatives, Norway, and former Chair of the GHWA board, commented on the need to “do things differently.” She referred to the recently released Alliance taskforce report Will we achieve universal access to HIV/AIDS services with the health workforce we have? A snapshot from five countries and stressed actions required by governments and other decision makers. These include: estimating numbers and types of health workers needed to reach international targets; strengthening health workforce management systems; implementing costed plans for increasing and improving the health workforce; and scaling up successful approaches.
Another important aspect raised was the need to focus considerable attention not only on workforce training but on staff retention strategies, looking at motivation and job satisfaction. This point was made by Dr John Palen, Senior HRH advisor of the US President’s Emergency Plan for AIDS Relief (PEPFAR).
The answer to the central question posed was a sobering one: if the impact of AIDS on health workers is not seriously addressed, the human resources crisis will worsen and MDG 6 will become almost impossible to attain. Although progress is being made, there are still many gaps and challenges to overcome.
A report of the meeting will be made available shortly.
Related

Feature Story
It’s possible: Making the most of linking sexual and reproductive health and HIV responses
09 June 2011
09 June 2011 09 June 2011
Dr Babatunde Osotimehin.
Credit: UNFPA
Linking sexual and reproductive health and HIV is of critical importance. Worldwide more than 80% of HIV infections are sexually transmitted. In addition, sexual and reproductive ill health and HIV are fueled by similar causes such as poverty, limited access to services, lack of correct information, gender inequality and social marginalization.
On 8 June, during a side event at this week’s General Assembly High Level Meeting on AIDS in New York, the question of how exactly such linkages can be strengthened was explored. The event was sponsored by UNAIDS, the UN Educational, Scientific and Cultural Organization (UNESCO), the UN Population Fund (UNFPA), the World Health Organization (WHO), and the International Planned Parenthood Federation (IPPF).
The highly interactive session looked at the issue through the prism of five key thematic areas: cost-effectiveness and cost savings of linkages; prevention of mother to child transmission though a sexual and reproductive health platform; comprehensive sexuality education for young people; ending gender-based violence; and human rights of people living with HIV.
Making ‘people-sense’
In his opening remarks, Dr Babatunde Osotimehin, UNFPA Executive Director, explained how the integration of sexual and reproductive health and HIV services makes ‘people-sense’. These services include testing for HIV and other sexually transmitted infections, prevention of mother-to-child transmission, support for fertility decisions, and access to condoms, contraception and correct information. He went on to emphasize wider policy and human rights implications.
“Linking sexual and reproductive health and HIV goes beyond integrating health services,” he said. “It demands from us that we fortify the human rights platform–ending stigma, violence and discrimination.”
Human rights and the right to health were said to be at the core of greater integration of services. A broader human rights agenda can also be promoted that goes beyond service delivery and tackles legal reforms, such as those relating to the right to information and freedom from violence, abuse and coercion.
Sharing ideas and experience
The participants shared ideas and experiences of how those working in the fields of HIV and sexual and reproductive health have combined their efforts to make interventions more effective in creative and innovative ways, including strategies to strengthen treatment as a prevention option.
It was stressed that mother- and child-centred care can improve both sexual and reproductive health and HIV outcomes. For many women, pregnancy is the first point of access in the health system and they can benefit from a range of interventions, including HIV prevention and treatment integrated into routine maternal health care; family planning; and preventing and managing sexually transmitted infections and gender-based violence.
The discussion also showed that when comprehensive sexuality education is effectively implemented on a national scale, there is potential for cost saving from averting HIV infections, other STIs and unintended pregnancies.
Participants examined how men can benefit from greater integration. For instance, in countries where voluntary male circumcision is being implemented for HIV prevention, the number of men accessing other sexual and reproductive services, such as prevention of mother-to-child transmission and treatment of STIs, has increased.
The meeting closed with agreement that linking sexual and reproductive health and the HIV response, especially in a climate of austerity, is a gateway to strengthening both the human rights agenda and health systems.
External links
Related

Feature Story
Yale convenes together senior health practitioners to build leadership and strategic problem-solving to improve health systems
05 June 2011
05 June 2011 05 June 2011
Credit: Carl Kaufman / Yale
The Global Health Leadership Institute (GHLI) of Yale University held its 2011 GHLI Conference from 5-10 June 2011 under the theme of “moving health systems forward”. The Conference convened senior health practitioners from around the world to facilitate collaborative solutions in strengthening health systems.
Speaking on 5 June, UNAIDS Executive Director Michel Sidibé gave an inaugural address to the conference to commemorate 30 years since the start of the AIDS response and shared UNAIDS’ perspective on future directions.
“We are so pleased to have Michel Sidibe join us to open our conference this year and help further bring attention to the role strategic planning and leadership play in helping solve global health issues,” said Elizabeth Bradley, Ph.D., faculty director, Yale Global Health Leadership Institute. “The conference is about gathering health officials from around the world to share experiences, develop leadership and identify creative ways to solve problems that affect the everyday lives of people in these countries,” she added.
Mr Sidibé stressed the transformative role that the AIDS response has played in community mobilization and strengthening health systems. “The AIDS response has led to enormous progress towards scaling up access to treatment and reaching out to people at risk of HIV infection, with a strong human rights focus. This has been, and continues to be, a catalyst for change in the health systems of many affected countries.”
The AIDS response has led to enormous progress towards scaling up access to treatment and reaching out to people at risk of HIV infection, with a strong human rights focus. This has been and continues to be a catalyst for change in the health systems of many affected countries
Michel Sidibé, UNAIDS Executive Director
This year’s week-long event brought together senior health practitioners from Ghana, Liberia, Rwanda, and South Africa to focus on health system issues including mental health, maternal mortality, human resource management and management capacity building. These countries have achieved improvements in health despite limited resources and have gathered to discuss and apply strategic problem solving to national health priorities.
In his speech, Mr Sidibé also recognized the leadership of these four countries and praised their high level representation at the General Assembly High Level Meeting on AIDS.
Each country delegation, comprised of senior leadership from Ministries of Health, non-governmental organizations and academic institutions, brought a health system challenge to address at the conference with the support of Yale faculty and experts. Delegates participated in interactive lectures, cross-country roundtable discussions, keynotes and facilitated work sessions. Delegates met with prominent leaders in global health and received training in strategic problem-solving and leadership.
Global Health Leadership Institute
The Yale Global Health Leadership Institute (GHLI) develops global health leadership through innovative education and research programmes that strengthen the capacity of countries and communities to ensure health equity and quality of care for all.