Male circumcision




Feature Story
Voluntary medical male circumcision shown to be highly cost-effective, highlighting the need to intensify scale up and sustainability
27 September 2023
27 September 2023 27 September 2023UNAIDS’ Global AIDS Update The Path that Ends AIDS underscores 2 main challenges faced by voluntary medical male circumcision (VMMC) programmes: diminished funding and low coverage among men in their twenties and older. Since VMMC was recommended by WHO and UNAIDS in 2007 as key to HIV prevention in high-prevalence settings, about 35 million men have accessed services across the 15 VMMC priority countries. While this shows good progress, the Global AIDS update highlights that VMMC coverage remains far from reaching the 90% global coverage target for impact in many subnational areas of priority countries. Additionally, funding has declined by almost half since 2020 from approximately US dollars 285 million to US dollars 147 million for the 15 countries funded by the United States President’s Emergency Plan for AIDS Relief (PEPFAR). But questions have arisen about VMMC’s cost-effectiveness under growing coverage of other biomedical interventions, such as antiretroviral treatment.
“We need strong political leadership to scale up implementation of VMMC programmes; tackle the inequalities holding back progress; and ensure sufficient and sustainable funding” said Angeli Achrekar, UNAIDS Deputy Executive Director of Programmes. “Countries that are putting people and communities first in their policies and programmes are already leading the world on the journey to ending AIDS by 2030.”
Voluntary medical male circumcision is a simple, safe procedure that has proven to reduce the risk of HIV transmission by up to 60% in heterosexual men. But is it cost effective? For how long must policy makers continue to promote VMMC among adolescent boys and adult men across VMMC priority countries? This is what a group of researchers investigated.
Now published in The Lancet Global Health and using 5 existing mathematical HIV models, the researchers aimed to assess whether providing VMMC for the next 5 years would continue to be a cost-effective use of HIV programme resources in sub-Saharan Africa. The models applied assumptions based on HIV epidemiology in VMMC priority countries focusing on Malawi, South Africa, and Zimbabwe. The impact and cost-effectiveness were projected over 50 years to capture clients’ lifetime HIV exposure and infection.
Findings reveal that a continuation of VMMC was cost-effective even in regions with low HIV incidence; VMMC was cost-effective in 62% of settings with HIV incidence of less than 1 per 100 person-years in men aged 15–49 years, increasing to 95% with HIV incidence greater than 10 per 100 person-years They underscored VMMC’s importance in continuing to avert HIV infections and related healthcare costs over time.
While details of the results varied by country and model (see Box1), overall VMMC was shown to be highly cost-effective and even cost saving in nearly all countries and scenarios.
| Box 1 Varying results across countries
|
The authors concluded that despite the scale-up of antiretroviral therapy and low HIV incidence in some settings, the continuation of VMMC for at least the next 5 years is cost-effective in almost all settings considered in this study.
“Clearly, intensified efforts and commitments are needed to scale up VMMC while at the same time sustaining these services to reach men and boys,'' said Dr Meg Doherty, Director of WHO’s Global HIV, Hepatitis and STI Programmes. “The new Global AIDS report shows a widening gap for men that is important to recognize and address efficiently and effectively for their own health and to reduce new infections.’’
These analyses support a call to action on intensified efforts to reach men and boys in general and for continued funding for VMMC programmes. The discussion on VMMC sustainability is crucial. UNAIDS and WHO are urging countries to intensify their efforts in scaling up VMMC to global coverage targets (90%), at the same time address programme sustainability.
In the 2025 HIV Prevention Roadmap, VMMC remains a core component of combination HIV prevention under the pillar of men and boys. It is not only cost-effective, but also, cost-saving in many settings. Accordingly, continued progress towards male circumcision coverage targets in all the VMMC priority countries must be accelerated
Our work

Update
Male circumcisions disrupted by COVID-19, fall short of the 2020 target
29 November 2021
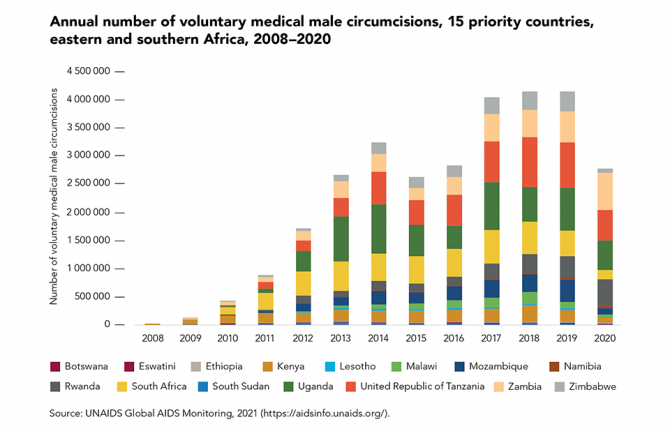
29 November 2021 29 November 2021In areas with high HIV prevalence and low rates of male circumcision, voluntary medical male circumcision (VMMC) can greatly contribute to HIV prevention. Despite this, there was a steep drop in the number of VMMCs performed in the 15 priority countries in 2020, due mainly to service disruptions caused by the COVID-19 pandemic: approximately 2.8 million procedures were performed in 2020, compared with 4.1 million in 2019.
Several countries suspended their programmes when the pandemic took hold, including South Africa. Despite this, programmes in some countries proved resilient enough to recover quickly and expand during the rest of 2020—notably in Rwanda and Zambia, where programme coverage grew by about 15%. In these countries, adjustments for the safe continuation of VMMC services during COVID-19 included changes in promotion and demand generation, client transportation, service delivery at a health facility or in the community and post-procedure follow-up appointments.
A total of about 18 million VMMCs were performed in 2016–2020, far shy of the 2020 target of 25 million. As well as COVID-19, an additional setback in 2015 and 2016 was the detection of tetanus cases in Uganda, which led to activities being scaled back in that country.
Our work
Related
 The impact of the US funding freeze and cuts on Namibia’s civil society: A struggle for survival
The impact of the US funding freeze and cuts on Namibia’s civil society: A struggle for survival
10 March 2025
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025
 Status of HIV Programmes in Botswana
Status of HIV Programmes in Botswana

20 February 2025
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025


Feature Story
We are off track to meet the 2020 targets on the number of voluntary medical male circumcisions
01 February 2021
01 February 2021 01 February 2021Voluntary medical male circumcision provides lifelong partial protection against female-to- male HIV transmission, reducing heterosexual male vulnerability to HIV infection by approximately 60%.
Voluntary medical male circumcision can also act as an entry point for providing adolescents 15 years and older and adult men in settings with generalized epidemics with broader health packages to improve their health outcomes. When combined with high levels of treatment coverage and viral suppression, evidence shows that the impact of voluntary medical male circumcision is particularly significant.
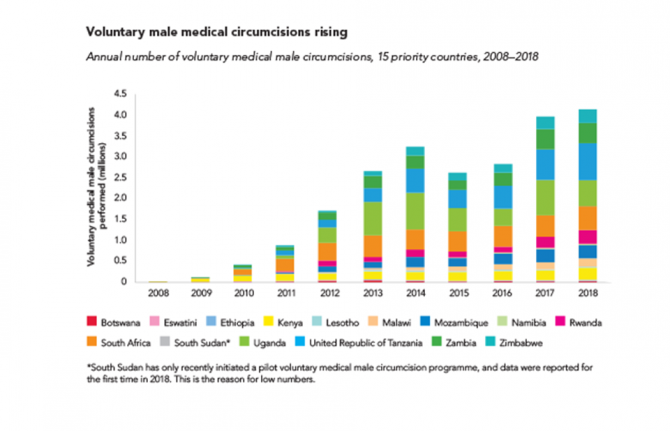
However, annual circumcisions in the 15 priority countries have remained relatively stable since 2017, falling short of the annual amounts needed to reach the 2020 target of 25 million additional circumcisions since the beginning of 2016.
Our work
Documents
Voluntary medical male circumcision — Remarkable progress in the scale-up of voluntary medical male circumcision as an HIV prevention intervention in 15 eastern and southern African countries
21 February 2020
Global data have highlighted the challenges in reaching desirable health outcomes for men in the HIV response. However, the voluntary medical male circumcision programme is a good example of an intervention that has consistently managed to reach men with good-quality HIV services for more than a decade.

Update
Voluntary medical male circumcision―4.1 million performed in 2018
21 October 2019
21 October 2019 21 October 2019Voluntary medical male circumcision (VMMC)―the removal of all or part of the foreskin of the penis by a trained health-care professional―reduces heterosexual male vulnerability to HIV infection by approximately 60%. Its effects last a lifetime. VMMC is also an entry point for providing men and boys with broader health packages to improve their health, and indirectly benefits women and girls.
VMMC can have a major impact on HIV epidemics in high-prevalence settings. VMMC services incorporate a package of prevention interventions, including safer sex education, education on and provision of condoms, HIV testing and the management of sexually transmitted infections.
About 11 million VMMCs have been performed in 15 priority countries in eastern and southern Africa since the beginning of 2016. In 2018 alone, about 4.1 million voluntary circumcisions were performed among males of all ages, a slight increase from the 4 million carried out in 2017.
There has been progress towards the target of 25 million additional circumcisions for HIV prevention from 2016 to 2020. However, at the end of 2018, when 15 million circumcisions should have been performed, the world was off-target by 4 million circumcisions.
Related

Update
Voluntary medical male circumcision accelerating in Malawi
29 May 2019
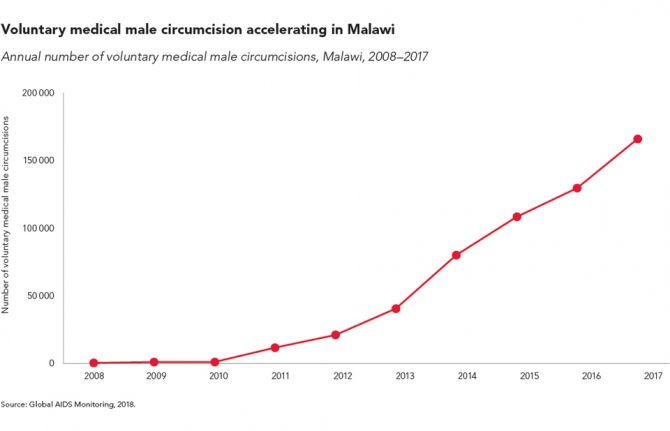
29 May 2019 29 May 2019Voluntary medical male circumcision (VMMC) remains the only one-time intervention for reducing the risk of HIV infection. The procedure provides lifelong partial protection against female-to-male HIV transmission and should be used as part of wider sexual and reproductive health service provision for boys and men.
Scaling up VMMC in combination with condom promotion, pre-exposure prophylaxis, HIV testing and prompt initiation of antiretroviral therapy can have a major impact on HIV epidemics in high-prevalence settings. In Malawi, more than 165 000 circumcisions were conducted in 2017, more than double the number conducted in 2014 and up from just 589 in 2008.
In 2016, the United Nations General Assembly set a target of voluntarily circumcising an additional 25 million men in high-incidence countries by 2020, or 5 million men per year.
Related information
Region/country
Related


Update
PEPFAR announces continued progress against HIV
06 December 2017
06 December 2017 06 December 2017New results from the United States President’s Emergency Plan for AIDS Relief (PEPFAR) announced on World AIDS Day 2017 show strong advances in scaling up HIV prevention and treatment.
UNAIDS recently reported that nearly 21 million people living with HIV are accessing antiretroviral therapy—more than half of the 36.7 million people living with HIV are now on life-saving treatment. PEPFAR’s latest data show that PEPFAR supported more than 13.3 million of those men, women and children.
PEPFAR’s new data also indicate that there have been significant declines in new HIV infections among adolescent girls and young women. In the 63 districts of 10 African countries implementing PEPFAR’s pioneering DREAMS (Determined, Resilient, Empowered, AIDS-free, Mentored and Safe) public–private partnership, the majority (65%) of the highest HIV burden communities or districts achieved a greater than 25% decline in new HIV infections among adolescent girls and young women. Importantly, new HIV infections declined in nearly all DREAMS programme districts.
By the end of September 2017, PEPFAR had provided voluntary medical male circumcision to more than 15.2 million men and boys. This result was reached through the largest single-year increase (3.4 million) in new voluntary medical male circumcisions since the beginning of PEPFAR.
PEPFAR has supported more than 6.4 million orphans and other vulnerable children and their caregivers affected by HIV and has prevented HIV infection among 2.2 million babies born to women living with HIV.
The new data add to PEPFAR’s impact results released in the past year, which show that five African countries are approaching control of their HIV epidemics. They also highlight critical advances being made under the PEPFAR Strategy for Accelerating HIV/AIDS Epidemic Control (2017–2020), which was launched by United States Secretary of State Rex Tillerson at the 2017 United Nations General Assembly.
Quotes
“We are at an unprecedented moment in the global AIDS response. Our latest results clearly show the remarkable impact of the United States President’s Emergency Plan for AIDS Relief’s accelerated HIV prevention and treatment efforts.”
Partner


Feature Story
Using market research for long-term sustainability of VMMC in Zimbabwe and Zambia
19 October 2016
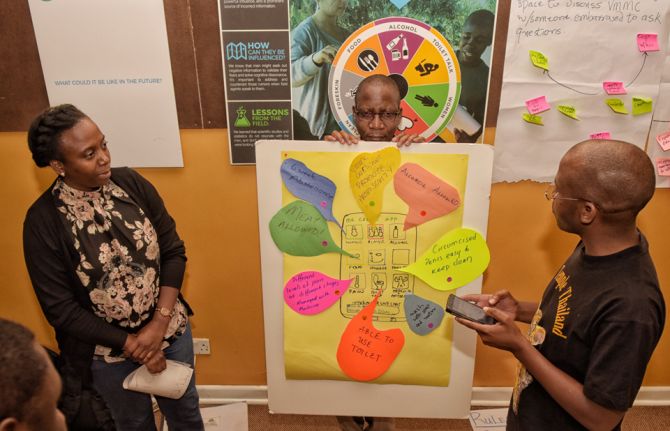
19 October 2016 19 October 2016Voluntary medical male circumcision (VMMC) provides at least a 60% protective effect against HIV infection for men, but, while service delivery for VMMC has improved, uptake has stalled. In response, the Bill & Melinda Gates Foundation funded Ipsos Healthcare, a market research company, to investigate how to better understand behavioural and psychographic characteristics of men and boys and the barriers and facilitators within their journey from awareness of the VMMC to uptake.
Much is known about why men undergo VMMC, but those reasons and how men’s beliefs influence decisions to opt for it have not been systematically mapped.
The stages a man goes through when deciding to have VMMC in Zambia and Zimbabwe were documented in order to understand the path to the decision, what affected their decision, the roles of key influencers and how boys and men tend to take different paths to VMMC, depending on their age. Ipsos discovered that, on average, it took men two years and three months to move from awareness of VMMC to having the procedure.
Ipsos surveyed 2000 men between the ages of 15 and 30 in the two countries. The findings showed that men fall into six groups with respect to their attitudes towards VMMC and wanted answers regarding five themes: sex appeal; procedure; pain; social support; and the benefits.
With support from the Bill & Melinda Gates Foundation to translate this research to practice, PSI Zimbabwe and the Society for Family Health, Zambia, used the results of the research to fine-tune and tailor messages to different groups of men. The research also improved the confidence of community workers in delivering previously uncomfortable messages, especially on pain and sex.
PSI Zimbabwe and the Society for Family Health, Zambia, prioritized the different groups by group size, ease of conversion, ability to advocate with peers and risk behaviour. After analysis of the research, they created “personas” of each group and identified areas where programmes and specific messaging could have the most impact.
Community workers mobilizing demand for VMMC report that they are able to quickly identify potential clients from the prioritized groups and target age groups. They are seeing fewer men but achieving a higher conversion rate as a result of the shift from group discussions to one-on-one discussions based on the research.
PSI Zimbabwe and the Society for Family Health, Zambia are now piloting messages and final concepts before scaling up programmes for the long-term sustainability of VMMC implementation.
Hands up for #HIVprevention — World AIDS Day campaign
Region/country
Related


Feature Story
Protecting men and boys’ health in Swaziland
21 October 2016
21 October 2016 21 October 2016The Centre for HIV/AIDS Prevention Services (CHAPS) leads a consortium that supports the Swaziland Ministry of Health to implement the national strategic voluntary medical male circumcision plan, which is part of the country’s efforts to keep men and boys free from HIV.
The centre’s work demonstrates how voluntary medical male circumcision programmes can be an important entry point to expanded health programming for men and boys, helping to ensure they are reached with a broad spectrum of vital health messages.
Swaziland has been particularly affected by the AIDS epidemic. In 2015, more than a quarter of 15-49-year-olds were living with HIV. As part of efforts to reduce new HIV infections, Swaziland has developed a plan that it hopes will help to keep young men and boys free from HIV.
Swaziland estimates that its Male Circumcision Strategic and Operational Plan for HIV Prevention 2014–2018 will avert 31 000 new HIV infections by 2028, which will result in cost savings of approximately US$ 370 million by 2035.
Studies have shown medical male circumcision to be around 60% effective in preventing female-to-male sexual transmission of HIV. Swaziland is taking a new and innovative approach to engaging men and boys in HIV prevention efforts and encouraging them to take up the offer of voluntary medical male circumcision to help protect them from becoming infected with HIV.
Lihawu three-day camps
In April 2016, CHAPS and Kwakha Indvodza, a male mentoring project in Swaziland, piloted a new initiative to encourage young men and adolescent boys to become respectful and responsible adults. The initiative, Lihawu (“shield”), is a three-day camp where 25 to 30 adolescent boys and young men aged 15–29 years are guided, mentored and encouraged to hold open and honest discussions about sexuality, sex and sexual health, relationships, gender equality and respect.
The camps are rooted in a Bantu rite of passage tradition and promote the Swazi cultural heritage of ubuntu. They use the traditional Swazi lisango, men’s meeting spaces, where they take part in challenges, games and goal-setting, as well as talking openly about the values of traditional and modern practices.
The camps also provide the opportunity for the men and boys to talk about HIV and participants are offered voluntary HIV counselling and testing. Voluntary medical male circumcision is also offered to participants should they wish to undergo the procedure to help protect them against HIV infection.
To date, more than 350 adolescent boys and young men have participated in Lihawu camps, with many taking up the opportunity to have an HIV test. People testing positive for HIV are directly linked to treatment and care programmes as part of the camp’s services. The Lihawu camps have also seen an uptake in voluntary medical male circumcision, with almost half of all participants opting for the procedure.
Saving lives through soccer
CHAPS also run a successful soccer programme to disseminate information about HIV prevention in the hope of increasing uptake of voluntary medical male circumcision in Swaziland. Through support from the United States President’s Emergency Plan for AIDS Relief, uptake among 15–29-year-olds increased from 2770 in 2015 to 4490 in 2016.
The centre has also appointed a local hero, international soccer player Dennis Yuki Masina, as an ambassador for voluntary medical male circumcision.
Empowering health advisers
CHAPS has also conceptualized and rolled out a unique training programme for health outreach workers. The programme uses best practices and tools from a number of sectors to empower outreach workers as a trusted source of health-care information in the community, particularly on HIV prevention, treatment, care and support and tuberculosis. The health advisers are equipped with a number of approaches to engage people, especially older men, and link them to essential health services, including voluntary medical male circumcision for HIV prevention.