A new report by UNAIDS demonstrates the critical role communities play, and how underfunding and harmful barriers are holding back their lifesaving work and obstructing the end of AIDS.
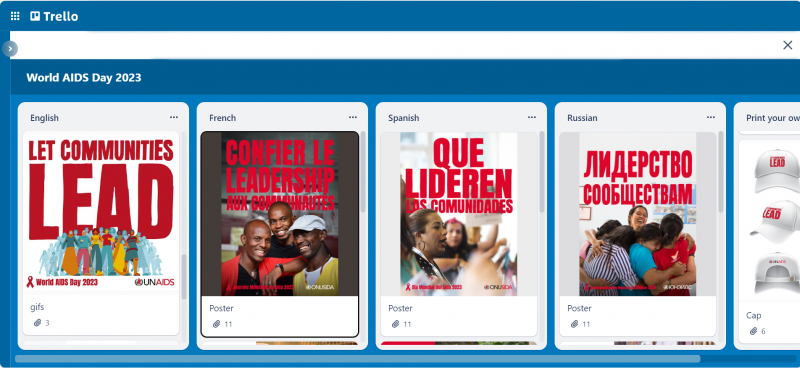
LONDON/GENEVA, 28 November 2023—As World AIDS Day (1 December) approaches, UNAIDS is urging governments across the world to unleash the power of grassroots communities across the world to lead the fight to end AIDS. A new report launched today by UNAIDS, Let Communities Lead, shows that AIDS can be ended as a public health threat by 2030, but only if communities on the frontlines get the full support they need from governments and donors.
“Communities across the world have shown that they are ready, willing and able to lead the way. But they need the barriers obstructing their work to be pulled down, and they need to be properly resourced,” said Winnie Byanyima, Executive Director of UNAIDS. “Too often, communities are treated by decision-makers as problems to be managed, instead of being recognised and supported as leaders. Communities are not in the way, they light the way to the end of AIDS.”
The report, launched in London during a World AIDS Day event organized by the civil society organization STOPAIDS, shows how communities have been the driving force for progress.
Community advocacy from the streets to the courtrooms to parliaments has secured groundbreaking changes in policy. Communities’ campaigning helped open up access to generic HIV medicines, leading to sharp, sustained reductions in the cost of treatment from US$ 25 000 per person per year in 1995 to less than US$ 70 in many countries most affected by HIV today.
Let Communities Lead shows that investing in community-led HIV programmes delivers transformational benefits. It sets out how programmes delivered by community-based organizations in Nigeria were associated with a 64% increase in access to HIV treatment, a doubling of the likelihood of HIV prevention service utilization, and a four-fold increase in consistent condom use among people at risk of HIV. It also notes how, among sex workers reached by a package of peer-based services in the United Republic of Tanzania, the HIV incidence rate was reduced to below half (5% vs 10.4%).
“We are the vehicle for change that can end systematic injustices that continue to fuel HIV transmission. We have seen groundbreaking developments with U=U, improved access to medicines, and have made great strides in decriminalisation," said Robbie Lawlor, Co-Founder of Access to Medicines Ireland. “Yet, we are expected to move mountains without being financially supported. We are supposed to fight for a more equitable world and are tasked with dismantling stigma yet are side-lined in crucial discussions. We are at a tipping point. Communities can no longer be relegated to the periphery. The time for leadership is now.”
The report highlights how communities are at the forefront of innovation. In Windhoek, Namibia, a self-funded project by the youth Empowerment Group is using e-bikes to deliver HIV medicines, food and adherence support to young people who often cannot attend clinics due to their schooling hours. In China, community organizations developed smartphone apps that link people to self-testing which contributed to a more than four-fold increase in HIV tests across the country from 2009 to 2020.
The report reveals how communities are also holding service providers to account. In South Africa five community networks of people living with HIV inspected 400 sites across 29 districts and conducted more than 33 000 interviews with people living with HIV. In the Free State province, these findings led provincial health officials to implement new appointment protocols to reduce clinic wait times and three- and six-month dispensing of antiretroviral medicines.
“I am extremely concerned about the exclusion from health services of key populations like the LGBT+ community,” said Andrew Mitchell, Minister of State for Development and Africa. “The UK champions the rights of such communities, and we will continue to protect them, working closely with our partners in civil society. I thank UNAIDS for keeping us focused on the inequities driving the pandemic and I look forward to working with our partners to champion the voice of people living with HIV and end AIDS as a public health threat by 2030.”
Despite the clear evidence of community-led impact, community-led responses are unrecognized, under-resourced and in some places even under attack. Crackdowns on civil society and on the human rights of marginalized communities are obstructing communities from providing HIV prevention and treatment services. Underfunding of community-led initiatives is leaving them struggling to continue operating and holding them back from expansion. If these obstacles are removed, community-led organizations can add even greater impetus to end AIDS.
In the 2021 Political Declaration on ending AIDS, United Nations member states recognized the critical role communities play in HIV service delivery, particularly to people most at risk of HIV. However, whereas in 2012, when over 31% of HIV funding was channelled through civil society organizations, ten years later, in 2021, only 20% of funding for HIV was available—an unprecedented backsliding in commitments which has cost and is continuing to cost lives.
“At this time, community-led action is the most important countermeasure in the AIDS response,” said Solange Baptiste, Executive Director of the International Treatment Preparedness Coalition. “Yet, shockingly, it isn’t a cornerstone of global plans, agendas, strategies, or financing mechanisms for improving pandemic preparedness and health for all. It is time to change that.”
Every minute, a life is lost to AIDS. Every week, 4000 girls and young women become infected with HIV, and out of the 39 million people living with HIV, 9.2 million do not have access to lifesaving treatment. There is a Path that Ends AIDS and AIDS can be ended by 2030, but only if communities lead.
UNAIDS is calling for: Communities’ leadership roles to be made core in all HIV plans and programmes; Communities’ leadership roles to be fully and reliably funded; And for barriers to communities’ leadership roles to be removed.
The report features nine guest essays from community leaders, in which they share their experience on the achievements they have secured, the barriers they face, and what the world needs to end AIDS as a public health threat.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.