Men who have sex with men
Documents
UNAIDS data 2024
02 December 2024
Suggested citation. UNAIDS DATA 2024. Geneva: Joint United Nations Programme on HIV/AIDS; 2024. Licence: CC BY-NC-SA 3.0 IGO. Related: The 2024 global AIDS report The Urgency of Now: AIDS at a Crossroads, released 22 July 2024, is available here.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025

Feature Story
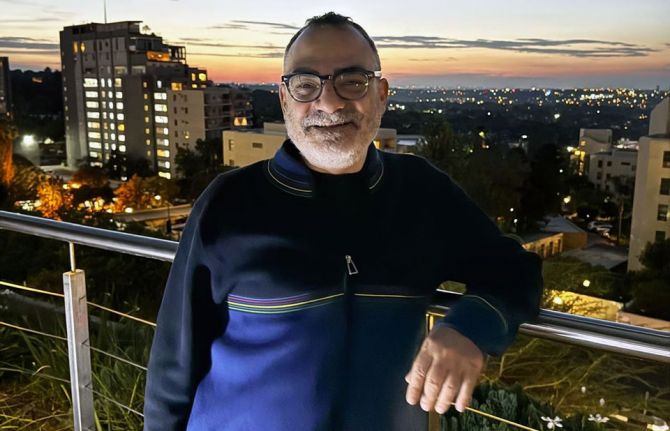
Christoforos Mallouris: From personal struggle to collective strength
29 November 2024
29 November 2024 29 November 2024Christoforos Mallouris' journey from humble beginnings in Cyprus to becoming a prominent global HIV advocate is a powerful story of personal transformation.
In his youth, Mallouris struggled with accepting his sexuality. "I couldn’t admit to myself that I was gay," shares Mallouris. The burden of self-stigma made it difficult for him to value his life: "In a way, I was homophobic towards myself and others."
At 29, while studying in Chicago, he was diagnosed with HIV. The diagnosis marked a pivotal moment in his life. "It changed how I understood myself, really forcing me to learn to value my life and accept who I am."
By the time he was diagnosed, he had already developed AIDS. Fortunately, Mallouris got support from his sister, who came to take care of him during his lowest moments.
Being HIV-positive in the United States as a foreign student presented its own set of challenges. "At the time, being HIV positive in the United States as a foreigner was illegal," Mallouris recalled, "so if the authorities found out, I would be deported." The fear of deportation hung over him as he was doing his PhD in astrophysics, but that fear also catalyzed his first act of activism.
Faced with health insurance that covered only two months of his costly HIV medication, Mallouris approached the Dean of Students at the University of Chicago. He boldly stated, "What are you going to do about it? I’m sure you don’t want this to go to the press." To his surprise, the Dean took immediate action, negotiating better health insurance coverage for all students with chronic illnesses.
As Mallouris’ health improved, he began to question his career path. Although he had completed his PhD in astrophysics, he no longer felt fulfilled enough by that field. He sought something that connected directly to being able to help people.
After securing a postdoctoral position at the Institute of Astrophysics in Paris, Mallouris found himself increasingly drawn to HIV work, so he started volunteering at a local NGO focused on HIV education and prevention for non-French speakers in Paris. It wasn’t long before he realized that this work was where his heart was.
He joined the Global Network of People Living with HIV, managing community empowerment programs in the HIV response. "I changed my career because of my HIV status," he said. "I wanted to do something that truly impacts lives."
Mallouris has had to overcome stigma and discrimination throughout his journey. Dating, for instance, was difficult. "There was a lot of rejection as soon as people found out I was HIV-positive," he shared. But despite the challenges, he found strength in the support of his friends, who have stood by him unconditionally. "I am lucky to have a strong network of support."
Mallouris joined UNAIDS in 2013, first as a Community Mobilization Advisor in Geneva and later as an Equality and Rights Advisor in Johannesburg. He describes UNAIDS as a supportive and inclusive workplace, where he feels valued for his skills and experience.
Mallouris highlights that the work to help secure treatment for people living with HIV is inseparable from the work to secure the recognition of people living with HIV as equal human beings. "Success in the HIV response depends on accepting all people, especially the most marginalized members of society.”
Mallouris is proud as he looks back, and hopeful as he looks ahead. He will always speak out for the rights of communities, even when—especially when—it isn’t popular.
HIV may have started as a burden in his life, but over time, it has become his strength, guiding him towards work that makes a profound difference, advancing a world where everyone is safe, has a place, and is welcome.














Press Release
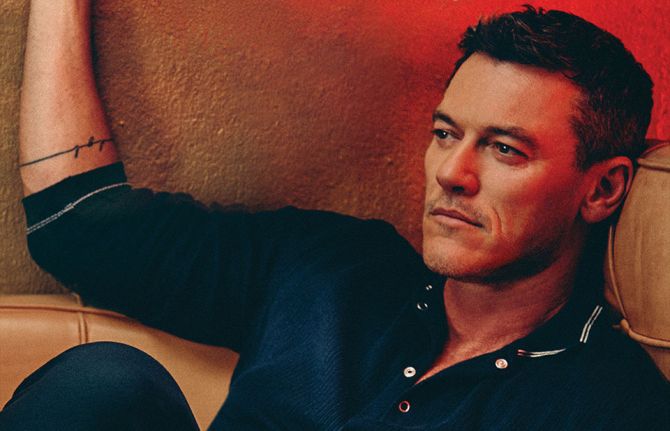
Global celebrities unite behind UNAIDS’ call for world leaders to “take the rights path to end AIDS”
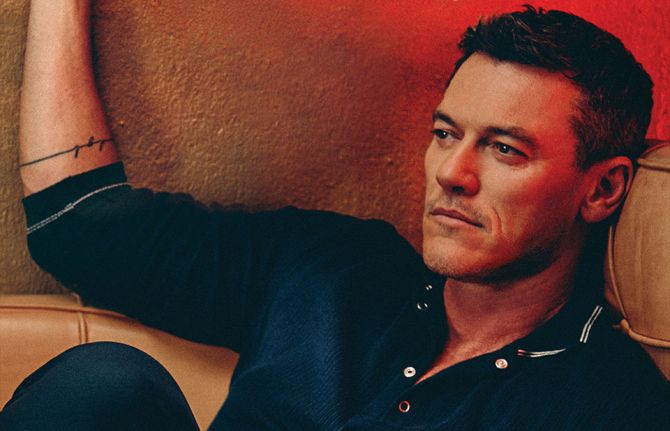
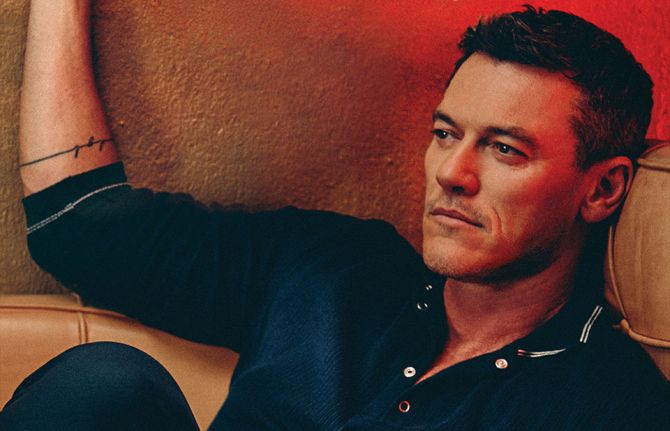
01 December 2024 01 December 2024GENEVA, 1 December 2024 — This World AIDS Day (1 December), sixteen global celebrities, including Hollywood film star Luke Evans and singer-songwriter Sia of the Unstoppable hit song, are uniting behind UNAIDS’ call for world leaders to protect human rights, which they say is vital to ensuring the success of efforts to end AIDS.
The celebrities, including actress and comedian Margaret Cho; comedian and poet Alok Vaid-Menon; fashion designer and television personality Tan France; actor Alan Cumming; actor, broadcaster and comedian Stephen Fry; actress Uzo Aduba; Moroccan artist OUM; South African actress Thuso Mbedu; Chinese actor and singer Huang Xiaoming; professional football player Racheal Kundananji; Pakistani-British actor and comedian Mawaan Rizwan; Filipino model and actress Pia Wurtzbach; Ukrainian singer and TV show host Vera Brezhneva; and popular television presenter Erkin Ryzkullbekov have come together in support of UNAIDS call to “Take the rights path to end AIDS.”
“The choice is clear if we want to end AIDS as a public health threat. World leaders must take the rights path to protect people’s right to health and life. When human rights are respected and guaranteed, their lives are greatly improved because they can freely seek healthcare, including HIV prevention and treatment.” said Stephen Fry, broadcaster and comedian.
“In far too many countries, people are still criminalized for being who they are or for who they love. When LGBTQ+ people are criminalized, they are driven underground and out of reach of health services, including services to prevent and treat HIV.” said Alok Vaid-Menon, American comedian and poet.
The report highlights gaps in the realization of human rights and shows how violations of human rights are obstructing the end of the AIDS pandemic.
63 countries still criminalize LGBTQ+ people.
Discrimination against girls and women, from denial of education to denial of protection from gender-based violence, is also undermining progress in the global HIV response. In 2023, women and girls accounted for 62% of new HIV infections in sub-Saharan Africa.
“We all win the fight against AIDS when human rights and the right to health are secured for everyone everywhere. We can end AIDS as a public health threat by promoting rights, respect and dignity for all." said, Margaret Cho, actress and comedian.
“When girls cannot get access to education and information, when young women cannot access HIV prevention and testing, they are put at much greater risk of acquiring HIV,” said Winnie Byanyima, Executive Director of UNAIDS.
In 2023 alone, 1.3 million people around the world were newly infected with HIV—three times higher than the global target set for 2025 of no more than 370 000 new infections.
“To protect everyone’s health, we need to protect everyone’s rights,”
UNAIDS World AIDS Day report, “Take the rights path to end AIDS”, shows that the world can end AIDS—if the human rights of people living with or affected by HIV are respected, protected and fulfilled, to ensure equitable, accessible and high-quality HIV services.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
World AIDS Day report 2024
Documents
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
The world’s decades-long response to HIV is at an inflection point. Despite successes, the world is currently not on track to end AIDS as a public health threat by 2030. Press release | Download full report | Download short version
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025




Feature Story
New Asia Pacific healthcare provider toolkit serves people having chemsex
13 November 2024
13 November 2024 13 November 2024Life became chaotic for Poon early. (Not his real name.)
As a gay teenager he was bullied at school by students and teachers. He moved in with his grandparents when his parents separated, but eventually left northern Thailand for Bangkok. There he survived through sex work.
Then Poon learned he was living with HIV. The weight of HIV prejudice merged with the stigma he already carried as a young gay man and sex worker. Some friends he made at a camp disclosed his HIV status online after an argument. He was diagnosed with major depressive disorder.
A partner introduced him to drug-use during sex. He went on to use multiple substances including methamphetamines and cocaine.
“Sex, drugs and alcohol are my escape,” he said.
This was one of the stories shared at the 6th Asia Pacific Chemsex Symposium (APCS). Held in Bangkok on November 6 and 7, the event brought together over 300 stakeholders from 27 countries. They shared their research and responses to a practice that remains largely hidden and not yet well understood. The event specifically explored pleasure as opposed to risk as an entry point for providing services.
Chemsex—also called High Fun in several Asian countries—refers to the use of stimulant drugs during sexual activity. It lowers inhibitions and may increase risk-taking. There are several public health implications including higher rates of HIV and sexually transmitted infections (STIs), lower adherence to treatment, overdose and the fallout linked with intoxication.
In Asia Pacific four of every five new HIV infections are among people from key population communities including men who have sex with men or MSM, people who use drugs, people in prisons or other closed settings, sex workers and transgender people. Young people make up a quarter of all new HIV infections and in some countries around half of new infections are among youth ages 15 to 24.
Several countries in the region are facing an HIV prevention crisis with new infections among MSM either increasing or decreasing far too slowly. In 2023, 43% of new infections in Asia-Pacific were among MSM. At the same time, there is evidence that the practice of chemsex in this community ranges from 3% to 31% depending on the country. But although chemsex is most visible in the MSM community, it is practiced by people from all populations.
“We are talking about sex and drugs—two topics that people call taboo,” said Brigitte Quenum, UNAIDS Regional Team Lead for Sciences, Systems and Services at the opening ceremony. “But as HIV has taught us, to reach people, we must confront the realities of their lives.”
Toolkit now available for Asia Pacific health workers
On day 2 of the symposium UNAIDS and UNODC launched the first-ever toolkit on chemsex for Asia Pacific clinical service providers. The toolkit was developed by the Australian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM). It is geared toward health workers in Asia and the Pacific working with men who have sex with men and transgender women.
"The increasing use of stimulant drugs in the region, including for ‘Chemsex’, poses significant health risks, including drug use disorders and various psychosocial challenges," said Masood Karimipour, Regional Representative of UNODC’s Office for Southeast Asia and the Pacific. "This UNAIDS-UNODC toolkit provides essential guidance for healthcare providers to address these challenges through evidence-based interventions. It emphasizes the importance of holistic, non-judgmental care that prioritizes the physical, psychological and social wellbeing of individuals, while ensuring access to harm reduction services and the prevention and treatment of drug use disorders within a comprehensive continuum of care."
The resource was created to support comprehensive clinical services in the region’s restrictive legal environments. Twenty-eight countries in Asia Pacific criminalise drug possession for personal use while 17 criminalise same-sex relations. Penalties for drug-related offences in the region are among the world’s harshest.
The toolkit was developed through consultation with clinicians, community representatives and government agencies. It covers chemsex basics as well as approaches to harm reduction, sexual health, and mental health services. It also covers different service delivery models including face-to-face, online and by communities. The toolkit offers guides and tools on topics such as initiating non-judgmental conversations and risk assessment.
“Stronger HIV prevention strategies tailored to chemsex are needed, along with expanded, inclusive services for sexual, physical and mental health,” said Suniya Taimour, UNAIDS’ Community-led Responses Advisor for Pakistan and Afghanistan.
Thia approach recognises that comprehensive health services can be lifesavers by using one point of contact to address multiple issues including physical, sexual and mental health as well as social issues. Poon is a living example. He has benefitted from a service package that has combined his HIV treatment with harm reduction interventions and psychiatric care. Today he is a 22-year-old university student with clear life goals who feels more empowered about his HIV status.
Our work
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025






Feature Story
Can this innovation change the way people think about HIV?
16 October 2024
16 October 2024 16 October 2024In 2020, a gay Thai man living with HIV sparked controversy with a Facebook post. He was on antiretroviral therapy and had gotten lab tests to check the level of virus in his blood. Since his viral load was undetectable, he wrote, he was going to stop using condoms.
The public responded with a mix of contempt and disbelief. How could he? So selfish! So reckless! The resulting debate spilled from social media onto national radio and TV.
“There was a huge backlash,” remembered Dr Nittaya Phanuphak, the Executive Director of the Institute of HIV Research and Innovation (IHRI). She was telling the story from IHRI’s sunlit offices to teams from Botswana, Ghana, Ivory Coast, Jamaica, Mozambique, South Africa and Zambia. They’d come to Bangkok as part of a learning exchange coordinated by the Global Partnership for Action to Eliminate all Forms of HIV-related Stigma and Discrimination.
Dr Nittaya said that she and her father, Professor Praphan Phanuphak, thought it was their duty to contribute to the public discourse. While the man’s approach might have been unconventional, the science behind his statement was sound.
They would know. Professor Praphan diagnosed Thailand’s first HIV case in 1985 and dedicated his life to HIV research, service delivery and advocacy. He co-founded the Thai Red Cross AIDS Research Centre which in 2014 conducted cutting-edge research as part of the Opposites Attract Study. Done in Australia, Brazil and Thailand, that study tracked couples in which one person was HIV-negative and the other was living with HIV but had achieved an undetectable viral load through successful HIV treatment. It confirmed that after two years of unprotected sex, there were no cases of HIV transmission between more than 300 couples.
“It’s a scientific fact,” Dr Nittaya said. “For me, I felt like we really needed to do something. We cannot just wait 50 years for this knowledge to gradually seep into Thai society.”
The “knowledge” to which she refers is the concept of undetectable = untransmittable, or U=U for short. Last year the World Health Organization further endorsed the principle, stressing that when a person’s viral load is undetectable there is zero chance of sexual transmission.
“Before, HIV treatment just meant longevity,” said Pan (not his real name), a person living with HIV. “But with U=U, now it is love without fear.”
Within three to six months a person who takes their HIV treatment as prescribed and receives viral load monitoring can confirm that they have achieved an undetectable viral load. This removes the self-stigma associated with having an “infectious” disease. For Thai HIV response stakeholders, this concept can also transform the public’s attitudes about people living with HIV, making it easier for them to live full, happy lives.
“If social perceptions can be brought in line with the reality of HIV treatment, we can remove the stigma around getting an HIV test or diagnosis,” said Eamonn Murphy, Regional Director of UNAIDS Asia Pacific and Eastern Europe Central Asia. “The more supportive the society, the more people we successfully treat and the fewer new infections.”
But for the U=U strategy to be fully utilized, work must be done to dispel myths and bolster confidence in science.
According to UNAIDS Country Director for Thailand, Dr Patchara Benjarattanaporn, a key step in the national process was bringing decision-makers together with relevant stakeholders, including voices from communities.
“They considered both global and local evidence,” she explained. “Now there is consensus about the science. U=U also conveys the message ‘you=you’, affirming that all individuals are equal and that people are more than their HIV status. It emphasizes the importance of ensuring people are fully informed about their options and respecting their right to make choices about their sexual health depending on their realities.”
At the opening ceremony of the eight-country learning exchange, Dr Niti Haetanurak, Department of Disease Control Deputy Director, noted that the U=U concept is a key element of Thailand’s “all of society” strategy to address the prejudice and rights violations people living with HIV face. Thailand has a National Costed Action Plan to Eliminate all forms of HIV-related Stigma and Discrimination. The Ministry of Public Health and Sub-National Committee on AIDS Rights Promotion and Protection under National AIDS Committee coordinate the effort. Community organizations play a leading role.
During the exchange the country teams visited the Service Workers in Group (SWING) Foundation which serves sex workers and IHRI’s Tangerine Clinic which primarily serves transgender people. Both have come up with innovative approaches to ensure groups that usually find it challenging to receive healthcare at state-run facilities can get HIV and sexually transmitted infection (STI) testing and treatment in a friendly environment.
A key strategy is training members of those very communities to provide certain services themselves. They can even start clients on treatment for HIV and some other conditions the same day they are diagnosed. This approach makes it less likely for people to disappear into the shadows after diagnosis, with a high chance of infecting others and eventually becoming ill.
“This community-led health model can be applied to any health condition or population. But this does not really address stigma and discrimination. It just bypasses it by opening up alternative service delivery outlets for people who want to avoid negative experiences elsewhere,” Dr. Nittaya said. “We need to address the heart of the stigma as well. That is why we are working on using U=U as a tool to explore how we can shift attitudes.”
The Bangkok Metropolitan Administration (BMA) is integrating this concept into its work in healthcare settings and the workplace. A masterplan is in the works. One branch of the strategy will tackle employers requiring HIV testing in the pre-employment phase or targeting employees they find out are living with HIV. Another aspect of the approach is the integration U=U into all levels of HIV service delivery and ongoing healthcare worker sensitization. All staff in clinics and hospitals are trained, not just nurses and doctors.
The work doesn’t stop there, though. Describing the Bangkok society as “open”, Dr Tavida Kamolvej, Deputy Governor of Bangkok, said that the whole of society was ready for deeper conversations about inclusion and HIV. But how could these approaches be applied in other countries and cities that are not quite as tolerant or accepting, she was asked.
“If you are confronted with beliefs that might not allow open conversations about HIV, sexuality and sex, you can strategically make it about health literacy, dignity and care for all people. I think this is soft enough to make people aware about health and wellbeing,” Dr Tavida advised.
Click here to learn more about the recent eight-country learning exchange to eliminate all forms of HIV-related stigma and discrimination.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025


Press Statement
UNAIDS statement on anti-LGBTQ+ legislation in Georgia
01 October 2024 01 October 2024GENEVA, 1 October 2024—UNAIDS expresses deep concern over the recently adopted anti-LGBTQ+ legislation in Georgia, which poses serious risks to public health and human rights.
UNAIDS supports the UN Office for the High Commissioner of Human Rights' statement that these laws will “impose discriminatory restrictions on education, public discussion, and gatherings related to sexual orientation and gender identity.”
These discriminatory laws violate fundamental rights to autonomy, dignity, and equality, exacerbating stigma and hindering LGBTQ+ people's access to essential health services. This undermines Georgia’s efforts to end AIDS and combat other infectious diseases.
UNAIDS reiterates that laws discriminating against LGBTQ+ individuals have no place in modern society. They lead to harassment, discrimination, violence and social exclusion, jeopardizing efforts to end the HIV epidemic. We call on Georgian authorities to repeal these harmful laws, as they will further isolate marginalized communities and worsen public health outcomes.
Stigma kills, but solidarity saves lives. Upholding the rights of LGBTQ+ people is crucial to advancing public health, social cohesion, and equality for all.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Documents
HIV and gay men and other men who have sex with men — Thematic briefing note — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
Gay men and other men who have sex with men are one of the populations that are disproportionally affected by HIV. In 2022, the relative risk of acquiring HIV was 23 times higher for gay men and other men who have sex with men than in the wider population globally. Trans men who have sex with men may also be at increased risk, although there are few data. Annual numbers of new HIV infections among gay men and other men who have sex with men increased by 11% between 2010 and 2022. Outside of sub-Saharan Africa, the proportion of new HIV infections among this key population has increased, but it has decreased among the remaining population. Despite the disproportionate burden, coverage of HIV services among gay men and other men who have sex with men in many settings continues to be below the 2025 target, with only 40% of them reporting in median accessing at least two HIV prevention options in the past three months in 2023. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
UNAIDS data 2024
02 December 2024
 Global celebrities unite behind UNAIDS’ call for world leaders to “take the rights path to end AIDS”
Global celebrities unite behind UNAIDS’ call for world leaders to “take the rights path to end AIDS”
01 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
 Can this innovation change the way people think about HIV?
Can this innovation change the way people think about HIV?

16 October 2024
 UNAIDS statement on anti-LGBTQ+ legislation in Georgia
UNAIDS statement on anti-LGBTQ+ legislation in Georgia

01 October 2024
Slide deck - 2024 global AIDS update
22 July 2024
Documents
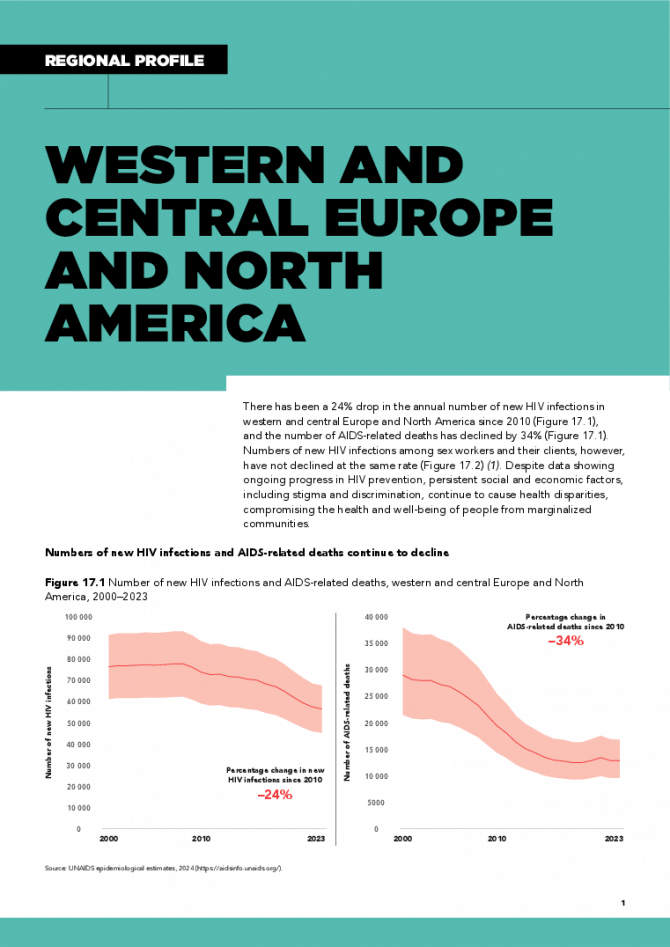
Western and Central Europe and North America regional profile — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
There has been a 24% drop in the annual number of new HIV infections in western and central Europe and North America since 2010, and the number of AIDS-related deaths has declined by 34%. Numbers of new HIV infections among sex workers and their clients, however, have not declined at the same rate. Despite data showing ongoing progress in HIV prevention, persistent social and economic factors, including stigma and discrimination, continue to cause health disparities, compromising the health and well-being of people from marginalized communities. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 UNAIDS urges that all essential HIV services must continue while U.S. pauses its funding for foreign aid
UNAIDS urges that all essential HIV services must continue while U.S. pauses its funding for foreign aid

01 February 2025
Documents
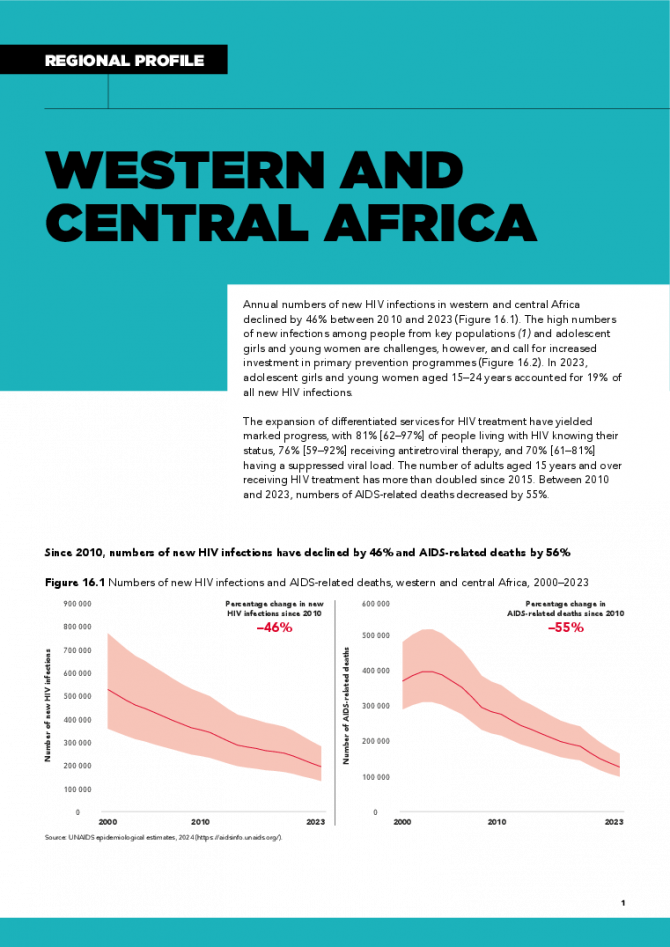
Western and Central Africa regional profile — 2024 global AIDS update The Urgency of Now: AIDS at a Crossroads
22 July 2024
Annual numbers of new HIV infections in western and central Africa declined by 46% between 2010 and 2023. The high numbers of new infections among people from key populations and adolescent girls and young women are challenges, however, and call for increased investment in primary prevention programmes. In 2023, adolescent girls and young women aged 15–24 years accounted for 19% of all new HIV infections. The expansion of differentiated services for HIV treatment have yielded marked progress, with 81% [62–97%] of people living with HIV knowing their status, 76% [59–92%] receiving antiretroviral therapy, and 70% [61–81%] having a suppressed viral load. The number of adults aged 15 years and over receiving HIV treatment has more than doubled since 2015. Between 2010 and 2023, numbers of AIDS-related deaths decreased by 55%. Related links: New UNAIDS report shows AIDS pandemic can be ended by 2030, but only if leaders boost resources and protect human rights now | Full report
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment
Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment

21 January 2025