PNG




Feature Story
PrEP for her: Cambodia, Indonesia, Papua New Guinea and the Philippines prepare to introduce the Dapivirine ring to help prevent HIV
22 November 2024
22 November 2024 22 November 2024The only HIV prevention that Elena Felix knew of was condoms. But condoms were not something that she was able to make use of, and she contracted HIV. Thirty years after her diagnosis, she’s helped conduct research to determine whether women in the Philippines would use a more confidential tool, and one that does not need a man to agree, to lower women’s risk of HIV infection.
“We hear from women that some partners insist on not using condoms. We hear cases too of rape. Women need protection that does not depend on men” the Association of Positive Women Advocates founder explained.
The Dapivirine Vaginal Ring or DVR was given the green light by the World Health Organization for women at high risk of contracting HIV in 2021. Unlike other types of pre-exposure prophylaxis (PrEP), this one is exclusively for women. It is a silicone vaginal ring that is inserted and worn for 28 days before being replaced. It releases an antiretroviral drug locally, reducing the risk of HIV infection through vaginal sex by half.
Since its introduction, the technology was made available in several (11) African countries. And with good reason. Around two-thirds of new HIV infections in Eastern and southern Africa and Western and central Africa are among adolescent girls and women. The combination prevention strategies implemented in these two regions have super-charged progress, driving the global 39% decline in new infections since 2010.
But the Asia Pacific picture is quite different.
“This region has an HIV prevention crisis,” Eamonn Murphy, UNAIDS Regional Director for Asia Pacific and Eastern Europe Central Asia said. “And I am not speaking only of the countries where new infections have doubled, tripled or increased six times since 2010. The average regional decline in new infections is far too slow. At 13% it has virtually flatlined.”
He was speaking to a group of community, government, research and development partners from Cambodia, Indonesia, Papua New Guinea and the Philippines who met from November 11 – 12 in Bangkok. Findings were disseminated from a DVR acceptability and feasibility study conducted by ThinkPlace, and a discussion held on next steps. UNAIDS and the World Health Organization (WHO) are providing technical support for this initiative. The Australia Department of Foreign Affairs and Trade (DFAT) funded the research as part of its ongoing support for prevention work in the region.
Seven percent of new infections in Asia Pacific are among sex workers while 12 percent occur among the intimate partners of key populations. Angeli Achrekar, UNAIDS Deputy Executive Director, called for women in Asia and the Pacific to be provided more HIV prevention options.
“Choice is the way to go!” Ms Achrekar stressed. “Providing options in prevention tools and service delivery increases overall use and results. We must ensure that people have access and that they are supported with the appropriate policies and enabling environment. The ring has great potential to be empowering as an additional choice for women, including in Asia Pacific.”
A person newly acquires HIV in the Asia Pacific region every two minutes. Despite this, the overall momentum on rolling out pre-exposure prophylaxis (PrEP) options has been sluggish. At the end of 2023 there were just 204,000 PrEP users in this region, 98% short of the 8,200,000 target by 2025. The vast majority of those on PrEP were men.
ThinkPlace Regional Director, Elliot Duffy, revealed that overall, the studies found women have high interest in this discreet, woman-controlled prevention method. Sex workers in the four countries sought the DVR given their high vulnerability to sexual violence. And in all countries the sex workers indicated that they would want to access the DVR through community-based health services or their local healthcare facilities. The research also found that healthcare providers in the four countries were enthusiastic about offering this new prevention option.
“The number one barrier is the extent to which women understand how the ring would fit. Many had questions like, “would it be lost in my body? Will I feel pain? Will I be able to have sex?’ Some women worried about a partner thinking they distrusted them,” Mr Duffy explained. “The DVR is not immune to the challenges of other HIV programs and continued effort is needed to increase awareness, generate demand and create services that are accessible.”
Already the research findings have resulted in the introduction and phased implementation of the DVR into 2024 – 2026 Global Fund grant implementation for Cambodia and Indonesia. Cambodia has begun pilot testing. At the meeting the four country teams developed plans to guide their next steps, including on further research, legal and policy reviews, regulatory approvals and community system strengthening.
DFAT Health Adviser, Joshua Metcalf-Wallach, emphasized that as stakeholders switched gears from research to rollout, they should keep communities in the driver’s seat.
“Our Indo-Pacific prevention work has shown that HIV services work best when they are key population- and community-led. As we expand prevention options for women, let us be guided by their needs and demands,” he ended.
Our work
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025



Feature Story
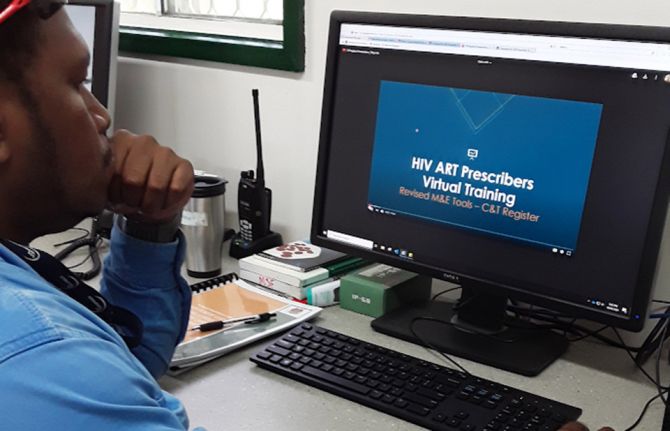
Virtual training for antiretroviral therapy prescribers launched in Papua New Guinea
04 August 2020
04 August 2020 04 August 2020The National Department of Health has launched the first-ever virtual training for prescribers of antiretroviral therapy in Papua New Guinea. Using Google Classroom, 21 video lectures with a total of more than six hours of content, covering HIV treatment, care and service delivery guidelines, as well as monitoring and evaluation tools, are provided to the learners. The content includes video lectures and associated assessment materials, which have to be completed within seven days after enrolment.
Thirty days since the launch, 105 participants have been successfully enrolled, of whom 70% had been unable to participate in any refresher training for the past three years.
Google Classroom requires an Internet-ready gadget—a smartphone, a laptop or a tablet— Internet access and a valid email address to be enrolled. Since some antiretroviral therapy prescribers do not have an email address, some local clinics have set up onsite classrooms where multiple trainees can join the online course from one computer, learning as a group.
The National Department of Health has successfully got support from partners, including UNAIDS, the World Health Organization, USAID, United States Centre for Disease control, World Vision and FHI 360, to cover US$ 15 of Internet access per participant, using cards with a seven-day data plan from a nationwide Internet provider network.
“Crises can also be opportunities and the impending COVID-19 crisis pressed us to find an innovative solution. The virtual antiretroviral therapy prescribers training shifted the goal posts, showing us that we could respond effectively and offer solutions. I am so proud of the partners that supported us in this and now we also have a more cost-effective way of training across the enormous geographic barriers that we find here in Papua New Guinea,” said Peniel Boas, Manager, Sexually Transmitted Infection and HIV Programme, National Department of Health.
The participants provided positive feedback on the training. “I really enjoyed learning a lot of new information. I would recommend that any sexually transmitted infection/HIV refresher training be conducted in this manner in the future, to minimize costs and provide this opportunity to health-care workers who otherwise do not have the possibility to attend,” said a nurse from the Leguava Clinic in West New Britain Province.
“The training provides relevant content which is well presented by the facilitators. I enjoyed the quizzes at the end of each presentation. The bonus being that it doesn’t take the worker away from their worksite, it doesn’t incur travel costs and it allows the participants to learn at their own pace. Also, the fact that the facilitators are still available on the platform is a great opportunity for ongoing mentorship,” said a student from the Innanaka Clinic in Hela Province.
The team behind this initiative comprises members of the National HIV Technical Working Group, including the UNAIDS country office, and lecturers, content providers, online class moderators and others. Google Classroom is free for use and all materials are stored in Google Drive using a Google account.
The virtual trainings will be followed by supervisory visits and onsite mentoring to be conducted by the sub-teams of the National HIV Technical Working Group. Due to this successful experience, this format is now being considered for other trainings in Papua New Guinea.
“The quick and strategic action to offer the antiretroviral therapy prescribers training virtually has saved lives here in Papua New Guinea. Without it, we could not have effectively rolled out the new HIV treatments that are combating HIV drug resistance,” said David Bridger, UNAIDS Country Director for Papua New Guinea.
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025




Feature Story
Getting HIV services to marginalized groups in Papua New Guinea
11 March 2020
11 March 2020 11 March 2020There are around 45 000 people living with HIV in Papua New Guinea, with marginalized groups, such as sex workers and other women who exchange sex for money, goods and protection, gay men and other men who have sex with men and transgender women, most affected. However, less than half of the people who belong to those vulnerable groups have ever taken a test to know their HIV status.
In November 2018, UNAIDS, the Global Fund to Fight AIDS, Tuberculosis and Malaria and other partners implemented a new outreach programme in the capital, Port Moresby, to try to reduce the impact of HIV among those groups of people by mapping the HIV epidemic and expanding HIV treatment and prevention services. Under the project, several outreach teams were created to promote and increase the uptake of testing and prevention services and to link people to HIV prevention and care services, if necessary.
By April 2019, the outreach teams had contacted 5000 people and tested 3000 of them for HIV, offering advice and support so that each person understood their test result.
“I like that we go to new places where people have never been offered an HIV test,” said a member of one of the outreach teams. “My motivation is meeting the young girls and taking care of them—making sure they take their medication.”
The outreach workers sometimes face harassment while conducting their work and change out of their official uniforms and into their own clothes so that people feel more comfortable talking to them. But the outreach workers find the work deeply rewarding.
“I have lost friends to AIDS, so that keeps me doing this work,” said another of the outreach workers. “It makes me work extra hard not to see someone else lost to this disease.”
The outreach teams are led by members of marginalized groups, an essential part of establishing community trust and engagement. In addition, leaders offer coaching, support and advice to field workers on a daily basis in order to ensure that their activities are as effective as possible.
The outreach programme is saving lives. Another of the outreach workers recalled his work with a transgender person, who he persuaded to try medication after testing positive for HIV.
“He told me that because he is transgender, he will only talk to a friend and that when he saw me, he knew I was a friend. Later, he brought in his companion to take a test.”
“This is a model of what can be achieved when we put our trust in community-led HIV services and programmes,” said Winnie Byanyima, UNAIDS Executive Director, in discussion with the outreach workers during her visit to Papua New Guinea with the United Nations Deputy Secretary-General, Amina Mohammed. “These outreach workers are heroes and they are saving lives.”
The outreach programme is also cost-effective and is projected to save hundreds of thousands of dollars over the next two years.
Region/country
Related




Feature Story
HIV data check in Papua New Guinea’s National Capital District
06 March 2020
06 March 2020 06 March 2020For six weeks, two teams covered 12 HIV clinics on a data checking mission in Papua New Guinea. UNAIDS joined the country’s strategic information technical working group in the National Capital District, which includes Port Moresby, to inspect the clinics’ records to see if they match the records of the National Department of Health.
“The data quality assessment is part of the country’s HIV monitoring and evaluation plan to ensure the quality of data and reporting of the AIDS response,” explained Zimmbodilion Mosende, UNAIDS Papua New Guinea Strategic Information Adviser.
Led by USAID, the two teams of 12 branched out into smaller teams to look at the number of people registered as enrolled on antiretroviral therapy, the number of people newly starting treatment, the percentage of people returning for refills and the number of people who did not return to the clinics. In addition, the groups checked information on, for example, the age and sex of each person.
The volunteers from civil society groups, international nongovernmental organizations, development partners and key government offices went through the records of nearly 5000 people.
Papua New Guinea has the highest HIV incidence and prevalence in the Pacific region. The country of 8.4 million people represents 95% of the reported HIV cases in the region. There are approximately 45 000 people living with HIV in the country, of whom 65% are on antiretroviral therapy.
The groups tried to find out if there are discrepancies in the data and the reasons behind them. Albert Arija, Monitoring and Evaluation Specialist of USAID, described the reasons for discrepancies, which range from there being an inadequate number of staff, hence not enough time to fill out all entries, to incorrect data entry or at times misinterpretation of information. For fear of stigma and discrimination, some clients don’t want to give personal information.
One key missing data point was also birthdates. “Many people in Papua New Guinea cannot recall their exact date of birth,” said Mr Arija.
The technical working group is advocating for the use of electronic forms and real-time reporting. “Since the current antiretroviral therapy forms are still paper-based, there are several potential data quality risks, including human errors, from the data entry and processing,” Mr Mosende said.
Overall, most of the clinics had good quality data and processing, according to the teams’ assessment. They hope to simplify the overall process to scale up the data check for the whole country.
Related information
Region/country
Related


Update
Papua New Guinea launches its first report on key populations
21 May 2018
21 May 2018 21 May 2018Papua New Guinea has published the results of its first comprehensive survey on key populations in the country. The report is the conclusion of a study that collected estimates of the sizes of key population and biobehavioural data, which will be used to inform prevention and treatment services and policies for HIV and other sexually transmitted infections.
“Only when we ensure that Papua New Guinea’s HIV programming reaches the right people in the right way and place, and at the right time, will the increasing HIV infection rates amongst key populations be slowed,” said David Bridger, the UNAIDS Country Director for Papua New Guinea, at the report’s launch.
The study, Kauntim mi Tu (count us), was carried out in the three largest urban areas of the country—Port Moresby, Lae and Mount Hagen. It revealed that female sex workers, gay men and other men who have sex with men and transgender people often do not seek health care, get tested for HIV or other sexually transmitted infections or use condoms.
Members of key populations in the country face real and perceived stigma, discrimination and violence from police, clients and others in their communities on a daily basis, according to the report. High rates of stigma, discrimination and violence are deterring them from seeking or accessing health-care services.
A member of Friends Frangipani, an organization of sex workers, said, “Many of us live very difficult lives. We don’t all have access to clean water, healthy food or a safe space. We are struggling. Yet we are told to look after ourselves, protect ourselves from HIV and, if HIV-positive, stay healthy. That is very hard for many of us. People need to understand our lives better, and Kauntim mi Tu has done that.”
While adult female HIV prevalence is estimated at 1.1% nationally, the study found that prevalence was nearly 20% among female sex workers in Mount Hagen and almost 15% in the capital, Port Moresby. More than half of gay men and other men who have sex with men and transgender people were found to have never been tested for HIV. Three out of four men in the second largest city, Lae, reported having experienced violence related to their sexuality or sexual identity.
The study included biological testing, with participants offered point-of-care tests and, if needed, same-day treatment for syphilis, chlamydia and gonorrhoea. The research team included members of key populations.
The study’s principle investigator, Angela Kelly-Hanku, noted that much work remains to be done. “This work must be done in the context of safe, respectful and enabling environments that support adequate public health responses and invest in new and dynamic ways to increase HIV testing and ensure that treatment is continuously available, that viral load testing is standard HIV care and that prevention is paramount to everything. We cannot be complacent,” she said.
The report is available at http://www.aidsdatahub.org/sites/default/files/publication/PNG_Kauntim_mi_tu_Multi-Site_Summary_Report_from_the_Key_Population_IBBS_2018.pdf.
Key populations in the country
Region/country
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025


Update
Braving the Kokoda trail to raise HIV awareness in Papua New Guinea
03 July 2017
03 July 2017 03 July 2017The Kokoda trail winds through the Owen Stanley Range in Papua New Guinea and is billed as one of the world’s most challenging treks. Nearly 100 km long, the track goes through rugged mountainous terrain and hikers are buffeted by hot and humid days followed by intensely cold nights. Carol Habin is a member of the national organization of people living with HIV in Papua New Guinea, called Igat Hope Inc., and she decided to raise HIV awareness by hiking the trail in June. She joined a group of around 20 people from Australia, which also included HIV-positive people.
“As a woman who works in HIV advocacy programmes, I have come to realize that women are vastly underrepresented in my country,” said Ms Habin. “Violence against women in Papua New Guinea is extremely high. I wanted to walk the trek to not only raise awareness about HIV stigma and discrimination, but also to empower women living with HIV and to make sure their voices are heard.”
The initiative Ms Habin joined was led by the HIV Foundation of Queensland under the Kokoda+Stronger Than You Think project. UNAIDS supported the mobilization of resources for Ms Habin’s participation in the trek. The team was led by Ji Wallace, who is an Australian living with HIV and an Olympic athlete.
“With a lot of work, we can change the attitude of the community,” said Mr Wallace. “It may not happen overnight, but we have the power within us to change.”
The trekkers took eight days to complete the hike. They conducted HIV awareness sessions with people living in villages along the track.
“I was surprised to find out how little the villagers knew about HIV,” said Ms Habin. “This initiative was very helpful in getting them to understand people living with HIV. I think also thanks to media coverage we have helped transform the way the public views HIV-positive people. I’ve shown everyone that as a woman living with HIV I can do anything, even hike one of the world’s toughest trails.”
Papua New Guinea has the largest HIV epidemic in the Pacific Islands. In 2015, there were 40 000 people living with HIV in the country and 2700 new HIV infections. The country is one of the few in the Asia and the Pacific region in which women are at higher risk of HIV than men, with 56% of new HIV infections occurring among women.
“I particularly want young women to understand they can say no to sex and stand up for their rights,” said Ms Habin.
The hikers completed the hike in late June and returned to Port Moresby for a celebration. UNAIDS Papua New Guinea Country Director David Bridger congratulated the team.
“Papua New Guinea has made immense progress in its HIV response,” said Mr Bridger. “But until the fear that generates misconceptions and breeds stigma is overcome, the AIDS epidemic will continue to claim lives. The Kokoda+Stronger Than You Think initiative is an innovative way to help break down misconceptions and celebrate the strength of people living with HIV. I congratulate your efforts.”
Ms Habin plans to build on the initiative and work with the Government of Papua New Guinea to encourage more people to take HIV tests and adapt HIV prevention to the needs of young women.
Region/country
Related


A satellite event on 21 July at the 20th International AIDS Conference in Melbourne, Australia, explored how public–private partnerships are leveraged in the response to HIV in Papua New Guinea.

“Ending AIDS by 2030 will require keeping HIV high on the post-2015 development agenda, and the active engagement of all stakeholders, including the private sector.” —Jan Beagle, UNAIDS Deputy Executive Director
Update
Public–private partnerships making a real difference in Papua New Guinea
21 July 2014
21 July 2014 21 July 2014A satellite event on 21 July at the 20th International AIDS Conference in Melbourne, Australia, explored how public–private partnerships are leveraged in the response to HIV in Papua New Guinea. The event highlighted in particular the role of the private sector in building innovative partnerships that form the foundation for successful public health interventions.
Papua New Guinea remains the most HIV affected country in the Pacific region, with a prevalence of 0.7%. It is a very challenging environment in which to operate, especially to implement and scale‐up HIV interventions in rural and remote regions. In many of these difficult to reach regions the private sector, and in particular the resource industry, has a strong operational and logistical capacity that can be leveraged to strengthen health systems.
One significant public–private partnership in Papua New Guinea is between Oil Search (the largest oil and gas exploration and development company incorporated in Papua New Guinea), the National Department of Health and the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund), which brings together corporate business systems, technical country expertise and multilateral funding.
Speaking at the meeting, UNAIDS Deputy Executive Director Jan Beagle commended such initiatives and stressed the vital importance of building multisectoral alliances to broaden and deepen the AIDS response, especially as the post-2015 development agenda is being defined. She also emphasized the importance of collective leadership from governments, civil society, international organizations and the private sector. Her sentiments were echoed by other high-level speakers, including Michael Malabag, Minister of Health of Papua New Guinea, Brett Mason, Parliamentary Secretary to the Minister for Foreign Affairs of Australia, Oil Search Managing Director Peter Botten and Mark Dybul, the Executive Director of the Global Fund. END
Quotes
"In Papua New Guinea, we have very good positive results from our public–private partnerships. The government has appreciated, in particular, the role of Oil Search as well as our partnerships with UNAIDS, the Government of Australia, the Global Fund and others."
"The partnership between the Oil Search Health Foundation and the Papua New Guinea Department of Health intends to leverage our respective strengths. The Department of Health brings a lot of knowledge and expertise. The Foundation brings logistics, community presence and further health and systems expertise with a delivery ethos more typical of the private sector."
"Ending AIDS by 2030 will require keeping HIV high on the post-2015 development agenda, and the active engagement of all stakeholders, including the private sector."
Photo galleries
Resources
Region/country
Related


UNAIDS Deputy Executive Director Jan Beagle with Honourable Julie Soso, Governor of Eastern Highlands province and MP Member of Parliamentary Working Group on Population and Sustainable Development.

UNAIDS Deputy Executive Director Jan Beagle; with Professor Sharon Lewin, local co-chair of AIDS 2014; and Peter Botten, Managing Director of Oil Search Limited

UNAIDS Deputy Executive Director Jan Beagle with Honourable Julie Soso, Governor of Eastern Highlands province and MP Member of Parliamentary Working Group on Population and Sustainable Development.

UNAIDS Deputy Executive Director Jan Beagle; with Professor Sharon Lewin, local co-chair of AIDS 2014; and Peter Botten, Managing Director of Oil Search Limited
Update
Papua New Guinea: the centrality of a multisectoral approach to the AIDS response
06 June 2014
06 June 2014 06 June 2014Papua New Guinea has the highest prevalence of HIV in Oceania (0.5% in 2012) and is experiencing an epidemic concentrated in key population groups and in certain geographical locations. During an official visit to the country, UNAIDS Deputy Executive Director Jan Beagle met with a variety of stakeholders—including representatives of the government, parliamentarians, development partners, civil society, the private sector and faith-based organizations—which were opportunities to highlight that one of the strengths of the AIDS movement globally has been its ability to build coalitions of stakeholders across disciplines and sectors. “AIDS is much more than a health issue, it is a development, human rights and gender issue. To get to zero in Papua New Guinea we need the power of a coalition of all sectors to ensure that no one is left behind,” said Ms Beagle during a meeting with members of the parliamentary working groups on HIV and population and sustainable development.
In Hela Province, Ms Beagle saw first hand the work of the Oil Search Health Foundation. The Foundation, in partnership with the government, civil society and communities, is providing HIV-related services and using HIV as an entry point for broader health and development outcomes—an example of a public–private partnership delivering quality services in a cost-effective way in a challenging environment.
Women are vastly underrepresented at all levels of the government (only three women sit in the national parliament), which limits their power to influence public policy at all levels. Violence against women is extremely high, and is experienced by an estimated two thirds of women. UN Women, as part of its Safe Cities Global Initiative, is promoting a safer working environment for women in two pilot marketplaces in the National Capital District of Papua New Guinea—where 80% of market vendors are women—enabling women to keep their earnings safe and to be safer physically. In the markets, infrastructure is being upgraded, market stalls renovated and potable running water made available. New innovative cashless methods for the collection of fees are being implemented to prevent extortion and theft, market vendor associations established and a referral system for survivors of family and sexual violence in the markets piloted. With support from UNAIDS, health mobile clinics will be established in these pilot markets to provide basic health services, including HIV-related services.
Related


UNAIDS Deputy Executive Director Jan Beagle with former Minister for Community Development, and renowned AIDS activist, Dame Carol Kidu.
UNAIDS Deputy Executive Director Jan Beagle visited the Pari community during her official visit to Papua New Guinea.
Update
Papua New Guinea: communities at the centre of the AIDS response
29 May 2014
29 May 2014 29 May 2014The communities most affected by HIV have always been at the forefront of the response to the epidemic, mobilizing and inspiring others to act. In her official visit to Papua New Guinea, taking place during the last week of May, UNAIDS Deputy Executive Director Jan Beagle witnessed how community leadership is making a difference for people living with HIV in the country.
Community systems in the country are based on the traditional wantok welfare and care system, whch is grounded on the belief that if one of your wantoks (close friends) is sick, you need to care for him or her. This system has allowed communities to be more responsive in delivering HIV services to those most in need in an effective, rights-based and culturally appropriate manner.
During a visit to the Pari community with former Minister for Community Development, and renowned AIDS activist, Dame Carol Kidu, Ms Beagle highlighted the importance of community leadership in demonstrating acceptance of people living with HIV, raising awareness about HIV prevention and tackling stigma and discrimination.
Quotes
"We need to maximize the participation of people living with HIV; their involvement gives personal power and immediacy to AIDS efforts, improves the technical elements and relevance of programmes, enables buy-in by the broader people living with HIV constituency and the community in general and inspires others into action."
"Zero discrimination is the hardest zero to reach. We need role models, chiefs, councillors, women; we need everyone to have the courage to reject stigma, discrimination and violence, to create a supportive community environment for people living with HIV, and for open discussions at the family and community level on HIV and sexual education issues."
"Women are caregivers in our communities so they need to understand the needs of people living with HIV. Knowledge about HIV needs to go to every household in our villages. We know people are dying from AIDS but we do not talk about it."
Related

Feature Story
Papua New Guinea releases new HIV prevalence estimates
26 August 2010
26 August 2010 26 August 2010
UNAIDS Executive Director Michel Sidibé (second from left) met with His Excellency the Governor General of PNG, Grand Chief, Sir Paulius Matane (middle) during his official visit to Papua New Guinea. 25-26 August 2010. Credit: Noreen Chambers
Approximately 0.92% of the adult population in Papua New Guinea was living with HIV in 2009, according to new estimates from the National Department of Health and the National AIDS Council Secretariat.
This latest round of estimates of HIV prevalence—carried out by a panel of national and international experts—is based on extensive data from antenatal clinics in Papua New Guinea’s Highlands, Southern, Momase, and New Guinea Islands regions.
In recent years, there has been a substantial increase in the number of health facilities in Papua New Guinea conducting HIV tests among pregnant women—from 17 in 2005 to 178 in 2009. New data collected at these facilities have provided a clearer picture of the country’s HIV prevalence than ever before.
“These new estimates have greatly enhanced our understanding of the scale and scope of Papua New Guinea’s AIDS epidemic,” said UNAIDS Executive Director Michel Sidibé, in an official visit to Papua New Guinea. “They provide an opportunity to redouble our efforts to achieve universal access to HIV prevention, treatment, care and support.”
An estimated 34 100 people in Papua New Guinea were living with HIV in 2009. HIV prevalence was found to be the highest in the country’s Highlands and Southern regions, at 1.02% and 1.17%, with lower but increasing prevalence in Momase and New Guinea Islands, at 0.63% and 0.61%. Approximately 3200 people in Papua New Guinea were newly infected with HIV in 2009 and, that same year, some 1300 people died of AIDS.
Papua New Guinea had previously projected a higher national HIV prevalence for the year 2009, based on data from a relatively small number of rural and urban sites. The downward revision in estimates reflects—to a large extent—improvements in national disease surveillance systems. The new findings also indicate that the spread of Papua New Guinea’s HIV epidemic may be levelling off.
“The risk factors that contribute to HIV infection in Papua New Guinea have not changed,” said Mr Sidibé. “We cannot afford to be complacent or reduce investments in the country’s AIDS response.”
Right Hand content
Feature Stories:
Christian faith leaders launch alliance to respond to AIDS in PNG(7 May 2010)
Papua New Guinea launch of the Commission on AIDS in the Pacific (11 March 2010)
Multimedia:
UNAIDS Executive Director talks to Radio Australia about Papua New Guinea’s HIV response





