SRH




Update
Sexual health and rights and HIV integration critical to ending AIDS among young people
12 February 2016
12 February 2016 12 February 2016A powerful message about the need to progress on both the response to HIV and the sexual and reproductive rights of young people came out of the seventh Africa Conference on Sexual Health and Rights, which took place in Accra, Ghana, from 8 to 12 February.
The theme of the conference was “Realizing demographic dividend in Africa: the critical importance of adolescents and youth sexual and reproductive health and rights”. It was hosted by the First Lady of Ghana, Lordina Mahama, who is also the President of the Organisation of African First Ladies against HIV/AIDS (OAFLA), and brought together a broad range of stakeholders from government, the diplomatic community, youth groups, organizations of people living with HIV, the private sector, academia and the media.
The conference concluded that it was possible to end AIDS as a public health threat by 2030 only if the sexual and reproductive rights of young people were respected. The need for multisectoral investment in services for young people, including comprehensive sexuality education, was underlined.
Of the total number of adolescents living with HIV globally in 2014, 83% lived in sub-Saharan Africa. AIDS is now the leading cause of death among adolescents in Africa, and adolescents are the only age group in which AIDS-related deaths are not decreasing. In low- and middle-income countries, one in every three girls is married before reaching the age of 18, and one in nine is married before reaching their 15th birthday. Only a quarter of girls and a third of boys are reported to have a full understanding of how HIV is transmitted or how it can be prevented.
During the conference, Ms Mahama championed OAFLA’s launch of the continental All In campaign to end AIDS among adolescents. OAFLA also launched an initiative to end child marriage by 2020.
Quotes
“Enough is enough. Africa should no longer let its young people die from preventable diseases, nor allow young people to be immobilized by cultural practices that no longer have relevance. Achieving the 90–90–90 treatment target for HIV will help ensure no young person is left behind. As president of the Organisation of African First Ladies against HIV/AIDS and as a mother, I will rally the First Ladies around saving our adolescents from the effects of HIV. We will empower our young people to lead the drive—it is time to take the right action and make Africa a better place for the young.”
“The global community is daring to dream of a socially transformed world that is more equal, more peaceful, more sustainable. UNAIDS’ strategy recognizes the critical need to put youth, and particularly adolescent girls, at the heart of all efforts. Ensuring that young people can realize their sexual and reproductive health and rights is central to ending the AIDS epidemic. If we invest in girls and young women, boys and young men, and build coalitions across sectors, we can end AIDS by 2030.”
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025

Feature Story
UNFPA, WHO and UNAIDS: Position statement on condoms and the prevention of HIV, other sexually transmitted infections and unintended pregnancy
07 July 2015
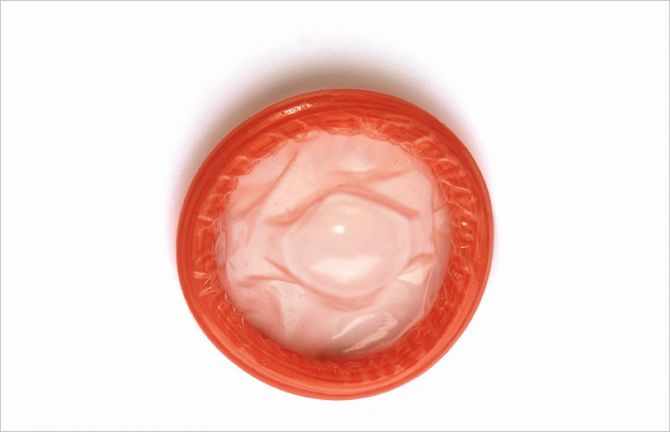
07 July 2015 07 July 2015Condoms are a critical component in a comprehensive and sustainable approach to the prevention of HIV and other sexually transmitted infections (STIs) and are effective for preventing unintended pregnancies. In 2013, an estimated 2.1 million people became newly infected with HIV[i] and an estimated 500 million people acquired chlamydia, gonorrhoea, syphilis or trichomoniasis.[ii] In addition, every year more than 200 million women have unmet needs for contraception,[iii] leading to approximately 80 million unintended pregnancies.[iv] These three public health priorities require a decisive response using all available tools, with condoms playing a central role.
Male and female condoms are the only devices that both reduce the transmission of HIV and other sexually transmitted infections (STIs) and prevent unintended pregnancy.
Laboratory studies show that condoms provide an impermeable barrier to particles the size of sperm and STI pathogens, including HIV.[v] [vi] Condoms, when used consistently and correctly, are highly effective in preventing the sexual transmission of HIV. Research among serodiscordant couples (where one partner is living with HIV and the other is not) shows that consistent condom use significantly reduces the risk of HIV transmission both from men to women and women to men[vii] [viii] [ix] Consistent and correct use of condoms also reduces the risk of acquiring other STIs and associated conditions, including genital warts and cervical cancer.[x] With a failure rate of about 2% when used consistently and correctly, condoms are very effective at preventing unintended pregnancy.[xi] [xii]
Condoms have played a decisive role in HIV, STI and pregnancy prevention efforts in many countries.
Condoms have helped to reduce HIV transmission and curtailed the broader spread of HIV in settings where the epidemic is concentrated in specific populations.[xiii] Distribution of condoms has been shown to reduce rates of HIV and other STIs in sex workers[xiv] [xv] [xvi] and men who have sex with men.[xvii] In India[xviii] [xix] and Thailand[xx] increased condom distribution to sex workers and their clients in combination with other prevention interventions were associated with reductions of transmission of both HIV and other STIs. Zimbabwe[xxi] and South Africa are two high-prevalence countries where increased condom use was found to contribute to reductions in HIV incidence.[xxii]
A recent global modelling analysis estimated that condoms have averted around 50 million new HIV infections since the onset of the HIV epidemic.[xxiii] For 2015, 27 billion condoms expected to be available globally through the private and public sector will provide up to an estimated 225 million couple years protection from unintended pregnancies.[xxiv] [xxv]
Condoms remain a key component of high-impact HIV prevention programmes.
Recent years have seen major scientific advances in other areas of HIV prevention. Biomedical interventions including antiretroviral therapy (ART) for people living with HIV can substantially reduce HIV transmission. While the success of ART may alter the perception of risk associated with HIV, studies have shown that people living with HIV who are enrolled in treatment programmes and have access to condoms report higher condom use compared to those not enrolled.[xxvi]
Condom use by people on HIV treatment and among serodiscordant couples is strongly recommended. [xxvii] Only when sustained viral suppression is confirmed and very closely monitored, and when the risk of other STIs and unintended pregnancy is low, it may be safe not to use condoms.[xxviii] [xxix] [xxx]
Oral pre-exposure prophylaxis (PrEP)—where antiretroviral drugs are used by HIV-negative people to reduce their risk of acquiring HIV—is also effective in preventing HIV acquisition, but is not yet widely available and is currently only recommended as an additional tool for people at higher risk, such as people in sero-discordant relationships, men who have sex with men and female sex workers, in particular in circumstances in which consistent condom use is difficult to achieve.[xxxi] Voluntary medical male circumcision (VMMC) can reduce the risk of HIV acquisition by 60% among men, but because protection is only partial, should be supplemented with condom use. [xxxii]
Hence, condom use remains complementary to all other HIV prevention methods, including ART and PrEP, in particular when other STIs and unintended pregnancy are of concern. The roll-out of large-scale HIV testing and treatment, VMMC and STI control programmes, and efforts to increase access to affordable contraception all offer opportunities for integrating condom promotion and distribution.
Quality-assured condoms must be readily available universally, either free or at low cost.
To ensure safety, efficacy and effective use, condoms must be manufactured according to the international standards, specifications and quality assurance procedures established by WHO, UNFPA and the International Organization for Standardization[xxxiii] [xxxiv] and made available either free or at affordable cost. Condom use in resource-limited settings is more likely when people can access them at no cost or at subsidized prices.[xxxv] [xxxvi]
Most countries with high HIV rates continue to heavily depend on donor support for condoms. In 2013, only about 10 condoms were made available to every man aged 15-64, and on average only one female condom per eight women in sub- Saharan Africa. HIV prevention programmes need to ensure that a sufficient number and variety of quality assured condoms are accessible to people who need them, when they need them. Adequate supplies of water based-lubricants also need to be provided to minimize condom usage failure, especially for anal sex, vaginal dryness and in the context of sex work.[xxxvii]
Despite generally increasing trends in condom use over the past two decades, substantial variations and gaps remain. Reported condom use at last sex with non-regular partners ranges from 80% use by men in Namibia and Cambodia to less than 40% usage by men and women in other countries, including some highly affected by HIV. Similarly, among young people aged 15 to 24 years, condom use at last sex varies from more than 80% in some Latin American and European countries to less than 30% in some West African countries.[xxxviii] This degree of variation highlights the need for countries to set ambitious national and subnational targets and that in many settings there are important opportunities for strengthening demand and supply of condoms.
Programmes promoting condoms must address stigma and gender-based and socio-cultural factors that hinder effective access and use of condoms.
Effective condom promotion should be tailored for people at increased risk of HIV and other STIs and/or unintended pregnancy, including young people, sex workers and their clients, injecting drug users and men who have sex with men. Many young women and girls, especially those in long-term relationships and sex workers, do not have the power and agency to negotiate the use of condoms, as men are often resistant to using condoms. Within relationships, the use of condoms may be taken to signal a lack of trust or intimacy.
However, few programmes adequately address the barriers that hinder access and use of condoms by young people,[xxxix] key populations[xl] and men and women in relationships. In some contexts, sex workers are forced to have unprotected sex by their clients.[xli] [xlii] and carrying condoms is criminalized and used as evidence by police to harass or to prove involvement in sex work[xliii] [xliv] These practices undermine HIV prevention efforts and governments should take actions to end these human rights violations.[xlv] Condom programmes should ensure that condoms and lubricants are widely available and that young people and key populations have the knowledge, skills and empowerment to use them correctly and consistently.[xlvi] Condoms should also be made available in prisons and closed settings,[xlvii] [xlviii] and in humanitarian crises situations.[xlix]
Adequate investment in and further scale up of condom promotion is required to sustain responses to HIV, other STIs, and unintended pregnancy.
Despite the low cost of condoms, international funding for condom procurement in sub-Saharan Africa has stagnated in recent years.[l] Collective actions at all levels are needed to support the efforts of countries that depend on external assistance for condom procurement, promotion, and distribution and to increase domestic funding and private sector investment in condom distribution and promotion.[li]
Although condoms are part of most national HIV, STI and reproductive health programmes, condoms have not been consistently distributed nor promoted proactively enough.[lii] National condom distribution and sales can be strengthened by applying a total market approach that combines public sector distribution, social marketing and private sector sales.[liii] [liv] Administrative barriers that prevent programmes and organizations from providing sufficient quantities of condoms for distribution need to be removed. In high-HIV prevalence locations condom promotion and distribution should become systematically integrated in community outreach and service delivery, and in broader health service provision.
[i] UNAIDS. 2014. World AIDS Day Report 2014.
[ii] WHO, Dept. of Reproductive Health and Research. Global incidence and prevalence of selected curable sexually transmitted infections.
[iii] UNFPA/Guttmacher Institute. 2012. Adding It Up: Costs and Benefits of Contraceptive Services.
[iv] Sedgh G et al. Intended and Unintended Pregnancies Worldwide in 2012 and Recent Trends. Studies in Family Planning, 2014, Vol 45. 3, 301–314, 2014.
[v] Carey RF et al. Effectiveness of latex condoms as a barrier to human immunodeficiency virus-sized particles under conditions of simulated use. Sex Transm Dis 1992;19:230-4.
[vi] WHO/UNAIDS. 2001. Information note on Effectiveness of Condoms in Preventing Sexually Transmitted Infections including HIV.
[vii] Holmes K et al. Effectiveness of condoms in preventing sexually transmitted infections. Bulletin of the World Health Organization, 2004, 82 (6).
[viii] Weller S et al. Condom effectiveness in reducing heterosexual HIV transmission. Cochrane Database Syst Rev. 2002;(1):CD003255.
[ix] Smith DK et al. Condom effectiveness for HIV prevention by consistency of use among men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2015 Mar 1;68(3):337-44.
[x] Also see: http://www.cdc.gov/condomeffectiveness/brief.html
[xi] Trussell J. Contraceptive efficacy, in: Hatcher RA et al., eds., Contraceptive Technology: Twentieth Revised Edition, New York: Ardent Media, 2011, pp. 779–863.
[xii] Kost K et al. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception, 2008; 77:10-21.
[xiii] Hanenberg RS et al. Impact of Thailand's HIV-control programme as indicated by the decline of sexually transmitted diseases. Lancet, 1994, 23;344(8917): 243-5.
[xiv] Ghys PD et al. Increase in condom use and decline in HIV and sexually transmitted diseases among female sex workers in Abidjan, Cote d’Ivoire, 1991–1998. AIDS, 2002, 16(2):251–258.
[xv] Levine WC et al. Decline in sexually transmitted disease prevalence in female Bolivian sex workers: impact of an HIV prevention project. AIDS, 1998, 12(14):1899–1906.
[xvi] Fontanet AL et al. Protection against sexually transmitted diseases by granting sex workers in Thailand the choice of using the male or female condom: results from a randomized controlled trial. AIDS, 1998, 12(14):1851–1859.
[xvii] Smith D et al. Condom efficacy by consistency of use among MSM: US. 20th Conference on Retroviruses and Opportunistic Infections, Atlanta, abstract 32, 2013.
[xviii] Boily M-C et al. Positive impact of a large-scale HIV prevention programme among female sex workers and clients in South India. AIDS, 2013, 27:1449–1460.
[xix] Rachakulla HK et al. Condom use and prevalence of syphilis and HIV among female sex workers in Andhra Pradesh, India - following a large-scale HIV prevention intervention. BMC Public Health, 2011; 11 (Suppl 6): S1.
[xx] UNAIDS. 2000. Evaluation of the 100% Condom Programme in Thailand, UNAIDS Case Study.
[xxi] Halperin DT et al. A surprising prevention success: Why did the HIV epidemic decline in Zimbabwe? PLoS Med. 2011. 8;8(2).
[xxii] Johnson LF et al. 2012. The effect of changes in condom usage and antiretroviral treatment coverage on human immunodeficiency virus incidence in South Africa: a model-based analysis, Journal of the Royal Society Interface. 2012, 7;9(72):1544-54.
[xxiii] Stover J. 2014. Presentation. UNAIDS Global Condom Meeting, Geneva, November 2014.
[xxiv] In line with standard assumptions, 120 condoms are required for 1 couple year of protection. Projected condom sales for 2015 cited based on: Global Industry Analysts. 2014. Global Condoms Market. May 2014.
[xxv] Stover J et al. Empirically based conversion factors for calculating couple-years of protection. Eval Rev. 2000 Feb; 24(1):3-46.
[xxvi] Kennedy C et al. Is use of antiretroviral treatment (ART) associated with decreased condom use? A meta-analysis of studies from low- and middle-income countries (LMICs). July 2014 h International AIDS Conference. Melbourne, WEAC0104 - Oral Abstract Session.
[xxvii] Liu H et al. Effectiveness of ART and condom use for prevention of sexual HIV transmission in sero-discordant couples: a systematic review and meta-analysis. PLoS One. 2014 4;9(11):e111175.
[xxviii] Swiss AIDS Federation Advice Manual: Doing without condoms during potent ART. Swiss AIDS Federation, 2008.
[xxix] Fakoya A et al. British HIV Association, BASHH and FSRH guidelines for the management of the sexual and reproductive health of people living with HIV infection. HIV Medicine, 2008, 9: 681-720, 2008.
[xxx] Marks G et al. Time above 1500 copies: a viral load measure for assessing transmission risk of HIV-positive patients in care. AIDS 2015, 29:947–954.
[xxxi] WHO. 2015. Technical update on Pre-exposure Prophylaxis (PrEP), February 2015. WHO/HIV/2015.4.
[xxxii] WHO. 2007. New Data on Male Circumcision and HIV Prevention: Policy and Programme Implications. WHO/UNAIDS Technical Consultation on Male Circumcision and HIV Prevention: Research Implications for Policy and Programming Montreux, 6 – 8 March 2007 Conclusions and Recommendations.
[xxxiii] WHO, UNFPA and Family Health International. 2013. Male Latex Condom: Specification, Prequalification and Guidelines for Procurement, 2010 revised April 2013.
[xxxiv] International Organisation for Standardisation. 2014. ISO 4074:2014 Natural rubber latex male condoms -- Requirements and test methods. http://www.iso.org/iso/catalogue_detail.htm?csnumber=59718.
[xxxv] Charania MR et al. Efficacy of Structural-Level Condom Distribution Interventions: A Meta-Analysis of U.S. and International Studies, 1998–2007. AIDS Behav, 2011, 15:1283–1297.
[xxxvi] Sweat MD et al. Effects of condom social marketing on condom use in developing countries: a systematic review and meta-analysis, 1990–2010. Bulletin of the World Health Organization 2012, 90:613- 622A. doi: 10.2471/BLT.11.094268.
[xxxvii] Use and procurement of additional lubricants for male and female condoms: WHO/UNFPA/FHI360 Advisory note. 2012.
[xxxviii]Source: Data from a database of Demographic and Health Surveys (DHS) available at statcompiler.com (verified January 2015).
[xxxix] Dusabe J, et al. “There are bugs in condoms”: Tanzanian close-to-community providers’ ability to offer effective adolescent reproductive health services. J Fam Plann Reprod Health Care 2015;41:e2.
[xl] Key populations are defined groups who, due to specific higher-risk behaviours, are at increased risk of HIV irrespective of the epidemic type or local context. Also, they often have legal and social issues related to their behaviours that increase their vulnerability to HIV. These guidelines focus on five key populations: 1) men who have sex with men, 2) people who inject drugs, 3) people in prisons and other closed settings, 4) sex workers and 5) transgender people. In consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations. World Health Organization 2014.
[xli] Global Commission on HIV and the Law. Risks, Rights & Health. 2012
[xlii] UNAIDS. 2014. The Gap report.
[xliii] Open Society Foundations. 2012. Criminalizing condoms. How policing practices put sex workers and HIV services at risk in Kenya, Namibia, Russia, South Africa, the United States and Zimbabwe. http://www.opensocietyfoundations.org/reports/criminalizing-condoms.
[xliv] Bhattacharjya, M et al. The Right(s) Evidence – Sex Work, Violence and HIV in Asia: A Multi-Country Qualitative Study. Bangkok: UNFPA, UNDP and APNSW (CASAM). 2015.
[xlv] WHO; UNFPA; UNAIDS; NSWP; World Bank. 2013. Implementing comprehensive HIV/STI programmes with sex workers: practical approaches from collaborative intervention. 2013.
[xlvi] Vijayakumar G et al. A review of female-condom effectiveness: Patterns of use and impact on protected sex acts and STI incidence. International Journal of STD and AIDS, 2006, 17(10):652-659.
[xlvii] UNODC/WHO/UNAIDS. 2006. HIV/AIDS Prevention, Care, Treatment and Support in Prison Settings A Framework for an Effective National Response.
[xlviii] UNODC/ILO/UNDP/WHO/UNAIDS. 2012. Policy brief. HIV prevention, treatment and care in prisons and other closed settings: A comprehensive package of interventions.
[xlix] Inter-Agency Standing Committee (IASC). 2003. Guidelines for HIV/AIDS interventions in emergency settings. Task Force on HIV/AIDS in Emergency Settings.
[l] UNFPA. 2015. Contraceptives and condoms for family planning and STI/HIV prevention. External procurement support report 2013.
[li] Foss AM et al. A systematic review of published evidence on intervention impact on condom use in sub-Saharan Africa and Asia. Sex Transm Infect 2007, 83:510–516.
[lii] Fossgard IS et al. Condom availability in high risk places and condom use: a study at district level in Kenya, Tanzania and Zambia. BMC Public Health 2012, 12:1030.
[liii] UNFPA-PSI. 2013. Total Market Approach Case Studies Botswana, Lesotho, Mali, South Africa, Swaziland, Uganda. http://www.unfpa.org/publications/unfpa-psi-total-market-approach-case-studies
[liv] Barnes, J et al. 2015. Using Total Market Approaches in Condom Programs. Bethesda, MD: Strengthening Health Outcomes through the Private Sector Project, Abt Associates.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025


Update
Forced and coerced sterilization: a global violation of human rights
19 March 2015
19 March 2015 19 March 2015UNAIDS and partners called for the elimination of forced and coerced sterilization of women and transgender people at the Commission on the Status of Women (CSW) in New York, United Sates of America.
During a side event hosted on 19 March by UNAIDS, the International Community of Women Living with HIV, Global Action for Trans Equality, the Center on Law and Social Transformation and the Action Program for Equality and Social Inclusion, participants discussed strategies and recommendations to fast-track the end of the practice in the context of the post-2015 development agenda. The dialogue brought together civil society activists, CSW delegates, ministers of gender and United Nations representatives.
The practice of forced and coerced sterilization continues to occur in many parts of the world. The participants discussed how it is a form of institutional violence and a human rights violation, which has been shrouded in silence and protected by societal acceptance.
The practice, however, has been garnering international attention in recent years, with increasing commitment to its elimination affirmed in several statements and resolutions. For example, in November 2014 the Namibian Supreme Court ruled in favour of three women living with HIV who had been subjected to coercive sterilization in public hospitals without their informed consent.
It was also highlighted that the 2014 United Nations interagency statement on eliminating forced, coercive and otherwise involuntary sterilization, to which UNAIDS is a signatory, is also contributing to the global efforts to eliminate this practice by providing guiding principles for prevention and recommendations for legal policy and service delivery.
Quotes
“Eliminating forced and coerced sterilization, which is a fundamental human rights violation, speaks to the heart of UNAIDS’ values, principles and work. It is one of too many sexual and reproductive rights violations.”

Press Statement
Botswana High Court rules in favour of registration of LGBTI civil society organization
18 November 2014 18 November 2014GENEVA, 18 November 2014—UNAIDS welcomes the recent ruling by the High Court of Botswana upholding the right of an organization that supports lesbian, gay, bisexual, transgender and intersex (LGBTI) people to register in the country.
In its groundbreaking judgement, the court held that the refusal by the government in 2012 to register the organization known as LEGABIBO (Lesbians, Gays and Bisexuals of Botswana) violates the rights to freedom of expression, assembly and association protected by the country’s constitution. The ruling represents the first time a high jurisdiction in Africa has upheld the freedom of assembly and association for LGBTI people.
“Through the courage of civil society organizations and the boldness of its judiciary, Botswana is sending an important message of inclusiveness and freedom,” said Michel Sidibé, UNAIDS Executive Director.
A valuable lesson learned in over 30 years of the HIV response is that civil society, particularly organizations of people living with and vulnerable to HIV, is essential to advancing health, dignity and development.
While Botswana has sharply increased access to antiretroviral therapy in the past decade, HIV prevalence in the country is still one of the highest in the world, at 21.9%. In response, Botswana is implementing a national strategic framework that includes the protection of human rights for all as a guiding principle.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Press centre
Download the printable version (PDF)
Region/country
Documents
Services for gay men and other men who have sex with men
14 November 2014
Gay men and other men who have sex with men have been profoundly affected by HIV, and have a 13 times higher HIV prevalence than the rest of the population. New HIV infections among men who have sex with men are driving or substantially contributing to national epidemics in all regions, accounting for 10% or more of new infections in Côte d’Ivoire, Ghana and Nigeria; 33% in the Dominican Republic; and 56% in Peru.
Related
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
 To end AIDS, communities mobilize to engage men and boys
To end AIDS, communities mobilize to engage men and boys

04 December 2024
UNAIDS data 2024
02 December 2024


Update
Action on sexual and reproductive health and rights critical say leaders
24 September 2014
24 September 2014 24 September 2014Promoting sexual and reproductive health and rights must be at the heart of the post-2015 development agenda, global leaders said during a high-level meeting in New York on 23 September.
During a side event at the 69th session of the United Nations General Assembly, participants stressed that key sustainable development goals, such as poverty eradication and ending the AIDS epidemic by 2030, could not be achieved without such rights becoming a reality for everyone, everywhere.
It was argued that the freedom to determine what happens to one’s own body and make decisions about sexuality, relationships and childbearing are fundamental facets of life. Yet far too many people, especially women and youth, are being denied these rights and are unable to fulfil their potential, resulting in an irreplaceable loss to individuals, families, communities and societies.
The negative consequences of sexual and reproductive health and rights not being protected are widespread and often devastating, noted the participants. For example, every day 800 women and girls around the globe die from largely preventable causes related to pregnancy and childbirth, and 2100 young people aged 15-24 become infected with HIV.
Organized by the Aspen Institute, the event was attended by a number of former heads of state, including the former President of Finland, Tarja Halonen, and the former President of Malawi, Joyce Banda. They were joined by United Nations representatives as well as current ministers and heads of global nongovernmental organizations.
Several leaders shared their personal stories with the audience, highlighting their own individual reasons for supporting reproductive health and rights as a key component of sustainable development. This sharing built on the Why we Care initiative, spearheaded by the Aspen Institute, which encourages global leaders to champion global family planning.
Quotes
"Sexual and reproductive health and rights must be affirmed as a non-negotiable aspect of the post-2015 agenda."
"Even one woman dying giving life is one too many. I don’t know about you, but I am ready to get the job done."
"Why is it that something that is so fundamental to women ends up being the most controversial in the development agenda?"
"The message from young people is clear—there is no way we can justify a new development framework that does not put young people’s issues at the centre of the agenda, including sexual and reproductive health and rights."
"We have seen it time and time again in the AIDS response. If you put rights, equality and dignity of women first you will see results."
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
Documents
Eliminating forced, coercive and otherwise involuntary sterilization - An interagency statement
01 May 2014
Like any other contraceptive method, sterilization should only be provided with the full, free and informed consent of the individual. However, in some countries, people belonging to certain population groups, including people living with HIV, persons with disabilities, indigenous peoples and ethnic minorities, and transgender and intersex persons, continue to be sterilized without their full, free and informed consent. This statement aims to contribute to the elimination of forced, coercive and otherwise involuntary sterilization. It reaffirms that sterilization as a method of contraception and family planning should be available, accessible, acceptable, of good quality, and free from discrimination, coercion and violence, and that laws, regulations, policies and practices should ensure that the provision of procedures resulting in sterilization is based on the full, free and informed decision-making of the person concerned.
Related
Joint Evaluation of the Global Action Plan for Healthy Lives and Well-being for All (SDG 3 GAP)
16 December 2024
UNAIDS data 2024
02 December 2024
 Resilience amid crisis: strengthening the HIV response for displaced communities in Ethiopia
Resilience amid crisis: strengthening the HIV response for displaced communities in Ethiopia

02 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
 Peru approves groundbreaking law to extend health coverage for migrants with HIV and TB
Peru approves groundbreaking law to extend health coverage for migrants with HIV and TB

21 October 2024
 Women living with HIV in China unite to confront discrimination
Women living with HIV in China unite to confront discrimination
14 October 2024
 UNAIDS statement on anti-LGBTQ+ legislation in Georgia
UNAIDS statement on anti-LGBTQ+ legislation in Georgia

01 October 2024


Update
Joining efforts to improve the health of young women and girls in South Africa
05 September 2014
05 September 2014 05 September 2014The First Lady of South Africa, Thobeka Madiba-Zuma, pledged to improve the health of young women and girls in South Africa during a meeting with UNAIDS Executive Director Michel Sidibé on 4 September at the President’s official residence.
Mr Sidibé acknowledged the First Lady’s role in lobbying for a price reduction for the human papillomavirus vaccine and ensuring better access to the vaccine in developing countries. The First Lady works extensively on health issues related to breast and cervical cancer and HIV, including prevention initiatives for young women and girls.
During his four-day visit to the country, Mr Sidibé also met with the South African Minister of Health, Aaron Motsoaledi, to discuss Africa’s response to the Ebola virus outbreak and the lessons African leaders can learn from the AIDS response. Mr Sidibé said that strengthening health systems and bridging the gap between health systems and the community are critical to addressing the outbreak effectively.
In a round-table dialogue with Mr Sidibé, members of the South African National AIDS Council’s Civil Society Forum reiterated the need to form a stronger and strategic partnership with the Government of South Africa and the critical role that civil society plays in creating demand for the services that the government provides to respond to HIV and tuberculosis.
Quotes
“We can build a hundred hospitals, but, if we don’t empower people with knowledge on healthy lifestyles and responsible behaviour, we won’t make progress.”
“In the absence of a cure or vaccine for Ebola, we need a deliberate and non-emotive response which learns lessons from AIDS in Africa.”
“We need to innovate on HIV prevention for young women and girls and find ways to reach them earlier with solutions like cash transfers and address intergenerational sex.”
"There is a serious need to focus on local initiatives in creating sustainability and coherence of strategies in South Africa. Civil society remains committed to the HIV response and we are encouraged by UNAIDS’ commitment in ensuring that communities access quality and competent health-care services."
Related
 Comprehensive update on HIV programmes in South Africa
Comprehensive update on HIV programmes in South Africa

25 February 2025






Update
Challenging parental consent laws to increase young people’s access to vital HIV services
23 July 2014
23 July 2014 23 July 2014There remain serious challenges in reaching the world’s adolescents with HIV, sexual and reproductive health and harm reduction services. The situation is especially worrying given that this is the only age group in which AIDS-related deaths are increasing, and AIDS-related deaths are the number two contributor to global adolescent mortality.
A session at the International AIDS Conference in Melbourne, Australia, on 23 July explored one of the key barriers preventing young people from accessing interventions: the need for parental consent before they are allowed to benefit from services such as HIV counselling and testing and needle–syringe programmes. The session heard that in sub-Saharan Africa, for example, at least 33 countries had age-based or other specific criteria for consenting to HIV testing and counselling.
While acknowledging that parents, guardians and the state have an obligation to protect young people from harm, participants discussed adolescents’ evolving capacity to independently consent to accessing potentially life-saving programmes. Daniel McCartney, of the International Planned Parenthood Federation and a member of the pact for social transformation, a coalition of 26 youth-led organizations, supported by UNAIDS, presented the findings of a global online youth survey on parental consent laws and requirements at the session.
It was found in the survey that 72% of respondents said laws requiring parental consent were not a good way of involving their parents in decision-making about their sexual and reproductive health and harm reduction. Thirty-eight per cent said that they have not always been able to access relevant services without restrictions when they needed them, a situation that left them feeling discriminated against and disempowered.
Participants agreed to use the results of the survey to advocate for countries to review their policies on age-related legal, regulatory and social barriers to specific health services and to strive to ensure that young people feel empowered and in charge of their own sexual health and well-being.