UGA
Documents
Expanding the HIV response to drive broad-based health gains: Six country case studies
15 April 2024
As progress lags in achieving most of the health targets of United Nations Sustainable Development Goal 3 (SDG 3), efforts to end AIDS as a public health threat by 2030 stand out as a beacon of hope. Since 2010, annual new HIV infections and AIDS-related deaths have declined globally by 38% and 51%, respectively. Although the world as a whole is not currently on track to reach all the SDG targets, evidence clearly indicates that ending AIDS as a public health threat by 2030 is achievable and that clear pathways exist to reach this goal.
Related
 Comprehensive update on HIV programmes in South Africa
Comprehensive update on HIV programmes in South Africa

25 February 2025
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
UNAIDS data 2024
02 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024


Press Statement
UNAIDS notes the judgment of the Constitutional Court of Uganda which has struck down certain parts of the Anti-Homosexuality Act, 2023
03 April 2024 03 April 2024GENEVA/JOHANNESBURG, 3 April 2024—The Constitutional Court of Uganda has today struck down certain sections of the Anti-Homosexuality Act, 2023.
“The Constitutional Court of Uganda made a judgment today to strike down certain sections of the Anti-Homosexuality Act, 2023. Evidence shows that criminalizing populations most at risk of HIV, such as the LGBTQ+ communities, obstructs access to life-saving health and HIV services, which undermines public health and the overall HIV response in the country,” said Anne Githuku-Shongwe, UNAIDS Regional Director for Eastern and Southern Africa. “To achieve the goal of ending the AIDS pandemic by 2030, it is vital to ensure that everyone has equal access to health services without fear."
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.


Press Statement
Joint Statement by the Leaders of the Global Fund, UNAIDS and PEPFAR on Uganda’s Anti-Homosexuality Act 2023
29 May 2023 29 May 2023GENEVA | WASHINGTON, D.C., 29 May 2023— The Global Fund to Fight AIDS, Tuberculosis and Malaria (the Global Fund), the Joint United Nations Programme on HIV/AIDS (UNAIDS), and the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) are deeply concerned about the harmful impact of the Ugandan Anti-Homosexuality Act 2023 on the health of its citizens and its impact on the AIDS response that has been so successful up to now.
Uganda’s Leadership Towards Ending the AIDS Pandemic as a Public Health Threat
Uganda and President Yoweri Museveni have been leaders in the fight to end AIDS. Progress has been made thanks to the implementation of large-scale prevention, diagnosis, treatment and care programs, all provided on the principle of access to health care for all who need it, without stigma or discrimination. This approach has saved lives. The strong health systems built to support the AIDS response serve the entire population of Uganda. This was evident as community health workers and health systems developed for the AIDS response played a key role in tackling COVID-19 and other disease threats. Maintaining this is vital: Failures in the HIV public health response will have system-wide impacts that could negatively affect everyone.
Success Is Possible
We know that we will be able to overcome this public health threat when we ensure that 95% of people living with HIV know their status, 95% of them are on treatment, and 95% of those on treatment have achieved viral suppression. Uganda can reach that. By 2021, 89% of people living with HIV in Uganda knew their status, more than 92% of people who knew their HIV status were receiving antiretroviral therapy, and 95% of those on treatment were virally suppressed. Uganda is well on track to achieve the UNAIDS HIV treatment targets if progress can be maintained.
Discrimination Threatens Progress in the AIDS Response
Uganda’s progress on its HIV response is now in grave jeopardy. The Anti-Homosexuality Act 2023 will obstruct health education and the outreach that can help end AIDS as a public health threat. The stigma and discrimination associated with the passage of the Act has already led to reduced access to prevention as well as treatment services. Trust, confidentiality, and stigma-free engagement are essential for anyone seeking health care. LGBTQI+ people in Uganda increasingly fear for their safety and security, and increasing numbers of people are being discouraged from seeking vital health services for fear of attack, punishment and further marginalization.
Uganda has repeatedly demonstrated leadership and commitment to ending AIDS – and has achieved great success – by leaving no one behind. Together as one, we call for the Act to be reconsidered so that Uganda may continue on its path to ensure equitable access to health services and end AIDS as a public health threat by 2030.
Peter Sands, Executive Director, The Global Fund
Winnie Byanyima, Executive Director, UNAIDS, and Under-Secretary General of the United Nations
Ambassador John Nkengasong, U.S. Global AIDS Coordinator and Special Representative for Global Health Diplomacy, U.S. Department of State
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Our work
Region/country


Press Statement
Uganda’s new Anti-Homosexuality Bill would harm public health
03 May 2023 03 May 2023GENEVA/JOHANNESBURG, 3 May 2023—Responding to the passing of the Anti-Homosexuality Bill by the Ugandan Parliament, UNAIDS has warned that its passing into law would undermine Uganda’s efforts to end AIDS by 2030, by violating fundamental human rights including the right to health and the very right to life.
UNAIDS East and Southern Africa Director Anne Githuku-Shongwe said:
“Uganda has made excellent progress in tackling the AIDS pandemic. This new Bill, if passed into law, would undercut that progress.
It would drive communities away from life-saving services, and obstruct health workers, including civil society groups, from providing HIV prevention, testing and treatment.
The evidence is crystal clear: the institutionalization of discrimination and stigma will further push vulnerable communities away from life-saving health services. Research in sub-Saharan Africa shows that in countries which criminalize homosexuality HIV prevalence is five times higher among men who have sex with men than it is in countries without such laws.
By undermining public health, this law would be bad for everyone.
The harmful Bill stands in marked contrast to a positive wave of decriminalization taking place in Africa and across the world, in which harmful punitive colonial legislation is being removed in country after country. Decriminalization saves lives and benefits everyone.
Public health organizations welcomed the President’s rejection of the earlier Bill. As this new Bill, like the earlier Bill, would hurt public health, it too should not be enacted.”
Region/country


Press Statement
UNAIDS urges the Government of Uganda to not enact harmful law that threatens public health
22 March 2023 22 March 2023GENEVA/JOHANNESBURG, 22 March 2023 — Responding to the passing of the Anti-Homosexuality Bill by the Ugandan Parliament, UNAIDS has warned that, if the Bill is enacted into law, it will have extremely damaging consequences for public health, by curtailing the human rights of people living with HIV and some of the most vulnerable people of Uganda to access life-saving services.
UNAIDS East and Southern Africa Director Anne Githuku-Shongwe said:
“If enacted, this law will undermine Uganda’s efforts to end AIDS by 2030, by violating fundamental human rights including the right to health and the very right to life.
It will drive communities away from life-saving services, and obstruct health workers, including civil society groups, from providing HIV prevention, testing and treatment.
The evidence is crystal clear: the institutionalization of discrimination and stigma will further push vulnerable communities away from life-saving health services. Research in sub-Saharan Africa shows that in countries which criminalize homosexuality HIV prevalence is five times higher among men who have sex with men than it is in countries without such laws.
By undermining public health, this law will be bad for everyone.
This law, if enacted, will hurt Ugandans. It will cost lives and it will drive up new HIV infections. We urge Government to not enact this harmful law.”
The law would impose a penalty of life imprisonment for homosexual acts and the death penalty for so-called “aggravated offences”. It even includes a duty to report acts of homosexuality, with failure to do so punishable by up to 6 months in prison.
The harmful Bill stands in marked contrast to a positive wave of decriminalization taking place in Africa and across the world, in which harmful punitive colonial legislation is being removed in country after country. Decriminalisation saves lives and benefits everyone.
Although the Anti-Homosexuality Bill has been passed by parliament, it is not yet enacted as a law and can, in the interest of promoting public health and equal rights of Ugandan citizens, be rejected by the President. It is not too late for this Bill to be rejected and lives to be saved.
Region/country



Feature Story
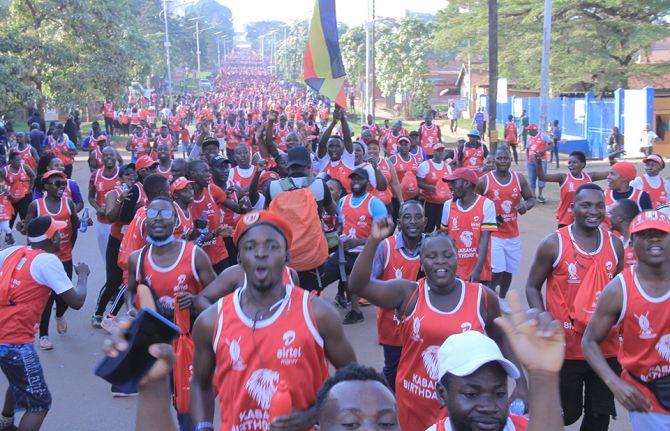
Thousands take part in the Kabaka Birthday Run to support the HIV response in Buganda
04 July 2022
04 July 2022 04 July 2022An estimated 80 000 people have taken part in the Kabaka Birthday Run, an annual event that forms part of the celebrations to mark the birthday of Kabaka Ronald Muwenda Mutebi II of Buganda. For the last three years, the run’s theme has been “Men for Good Health and Ending AIDS by 2030.”
The run is part of the Kabaka’s five-year campaign to increase the uptake of HIV testing and treatment services, with a particular focus on men and boys. It has yielded remarkable results in the Buganda region, with new HIV infections down more than in any other region of Uganda over the last few years.
The campaign is called “Men are Stars - Abaami Munyeenye” and connects men and boys aged 15—49 years old to HIV testing, treatment and care services, especially in the areas most affected by the pandemic. Through events such as the Kabaka Birthday Run, the Masaza football cup, the royal boat regatta, traditional campfire centres, school camps, radio and television shows, men and boys learn about the importance of going for regular health check-ups, including for HIV testing.
UNAIDS Executive Director, Winnie Byanyima, who attended the run in Mengo paid tribute to the Kabaka’s contribution to reducing the impact of HIV in Buganda.
“Your Majesty, under your leadership and through your messages to men and boys, Buganda has made remarkable progress against the AIDS pandemic in the last five years,” said Ms Byanyima, “UNAIDS looks forward to strengthening our partnership to reach other vulnerable groups such as young women and adolescent girls and to get Africa on track to end AIDS as a public health threat by 2030.”
In recognition of his significant contribution to the AIDS response, Ms Byanyima confirmed the Kabaka in his role as UNAIDS Africa Goodwill Ambassador.
Region/country
Related




Feature Story
Empowering people who inject drugs in Uganda
18 January 2022
18 January 2022 18 January 2022The hardships caused by the COVID-19 pandemic have magnified the challenges that people who use drugs face.
In Uganda, during the COVID-19 lockdowns there was limited access to HIV treatment and other health services, including access to medically assisted therapy, which provides daily doses of methadone to people who use drugs. Access to support systems, such as drop-in centres, was also affected.
“During the COVID-19 lockdown, access to medically assisted therapy for a daily dose was really hard for me, since movement was restricted and we required permission from the area local council. However, getting permission for a travel permit from the local council was very hard and took time, so it became challenging to sustain without access to these crucial services,” said Nsereko Joshua (not his real name), who is currently undergoing medically assisted therapy.
An analysis conducted by the Uganda Harm Reduction Network (UHRN) in July 2020 on the effects of the COVID-19 pandemic showed a decline in access to condoms, pre-exposure prophylaxis, counselling, psychosocial support, HIV testing, sexual and reproductive health services and legal aid services. It also highlighted a 25% increase in human rights violations reported among people who inject drugs during the COVID-19 lockdown. Issues included an increase in arrests and detentions, gender-based violence and eviction from their houses by the police at night.
When the UNAIDS Solidarity Fund for key populations was announced in December 2020, Wamala Twaibu, the founder and Chairperson of the Eastern Africa Harm Reduction Network and UHRN, saw an opportunity to empower people who inject drugs. He envisioned a transformed community that could support one another when in need, managing their own income sources.
“I was an injecting drug user for more than seven years, and I know what a drug user goes through daily. My aspiration is to improve the health, human rights and socioeconomic well-being of people who use drugs,” he said.
Mr Twaibu noted that injecting drug use and drug dependence often have long-term impacts on a person’s socioeconomic status and health outcomes. The lack of work skills, past criminal histories, stigma and discrimination and the criminalization of drug use are some of the main issues that people who inject drugs face regularly.
UHRN applied for the UNAIDS Solidarity Fund grant to kickstart the Empowered PWID Initiative for Transformation (EPIT) project, which was awarded in 2021. Through the EPIT project, community members currently on medically assisted therapy will be equipped with skills in craft-making for a sustained livelihood. Mr Twaibu noted that knowledge and skills in small-scale business management for people who inject drugs will form the core of the project.
About 80 people who inject drugs on medically assisted therapy will be engaged in the EPIT project, clustered in 16 cohorts with five members in each cohort and with at least six women-led cohorts across the five divisions of Kampala.
To ensure the sustainability of the initiative, a “Save, take and return” approach will be used. This strategy encourages beneficiaries to save some of the profits of the social enterprises every day, which they can get back after a few months.
“This fund looks at the socioeconomic empowerment of key populations, led by the affected community. That is the catch. Community ownership of the initiative is important because nothing for us without us,” said Mr Twaibu. “Change is possible when we support each other without discrimination and stigma. I wish to see a transformed and empowered people who inject drugs community that can support one another when in need,” he added.
Thinking about the effects of the COVID-19 pandemic so far, Mr Twaibu worries that the next wave of COVID-19 might affect the programme. However, he envisions a fully established and functional craft-making programme in the five divisions of Kampala and a scale-up in other regions where UHRN works.
Now that he is a part of the EPIT project, Mr Joshua expresses hope for a brighter future. “I yearn to have a complete recovery from drug addiction, and I believe that medically assisted therapy will do this for me,” he said. “And I believe the EPIT programme will give me an opportunity to develop and demonstrate my readiness for my recovery with the ability to earn something for my survival and for transport to seek my treatment. I think even after this programme, the skills will help me to sustain my family and myself as well.”
Our work
Region/country
Related


Feature Story
Pioneers of the harm reduction response in Uganda
07 May 2021
07 May 2021 07 May 2021The drop-in centre of the Uganda Harm Reduction Network (UHRN) looks lonely from the deserted suburban pavement. It is a non-descript house, hidden behind an imposing solid pink steel gate, in an equally non-descript neighbourhood.
It looks like so many other drop-in centres in eastern Africa that serve key populations—anonymous and low-key. Necessary characteristics, perhaps, in a region that mostly criminalizes people who use drugs, gay men and other men who have sex with men, sex workers and transgender people.
Once through the gate, visitors are greeted with a hive of activity that belies the quiet exterior. Clients and staff are buzzing around, setting up chairs under the makeshift gazebo in the verdant garden. In a few minutes, a group of people who use drugs will take part in a harm reduction workshop run by one of the centre’s staff. There is also a consulting room at the front of the drop-in centre; and at the back, is the office of Wamala Twaibu.
Mr Twaibu is the founder and chairperson of the Eastern Africa Harm Reduction Network and UHRN. A self-styled “former drug user with roots in Uganda and the pioneer of the harm reduction movement in eastern Africa,” Mr Twaibu has a kind face and a penetrating gaze that tells a story of adversity, resilience and triumph.
In the consulting room, 25-year-old Kemigisa Sandriano, a heroin user and sex worker, is taking an HIV test conducted by the centre’s resident doctor, Mukiibi Grace Nickolas. The night before, Ms Sandriano was assaulted by a client after he took off the condom during sex. She protested, telling him to leave. Her swollen, bloodshot right eye attests to what happened after that. She is smiley and talkative, seemingly unbothered by yet another instance of violence at the hands of a client. She is happy that in his battle to get his money back, she won.
Ms Sandriano was introduced to heroin by her ex-husband, who she says “ruined” her life. Nevertheless, she is upbeat about her recovery.
“I have the hope that I can stop. I even went to rehab for three months. When I saw my days of rehab coming to an end, I saw no plan and I started again,” she says.
“I am ready to go to rehab again,” she continues. “But when I come out, I don’t want to be idle. When they take us out of rehab, we need a job. They can say to us, “Work in a supermarket, work in this shop, so you can stabilize.””
Employment aside, Mr Twaibu says medically assisted treatment for people with opioid dependence is critical for rehabilitation. And, since, December 2020, with advocacy from UHRN and financial support from the United States President’s Emergency Plan for AIDS Relief and the Centers for Disease Control and Prevention, the first medically assisted treatment services in Uganda have been available at the Butabika National Mental Referral Hospital in Kampala.
UHRN screens and provides initial preparation for eligible clients and refers and links them to the hospital and provides them with ongoing psychosocial support services. In December 2020, there were 81 people who use drugs enrolled in medically assisted treatment.
Besides medically assisted treatment, through its drop-in centre UHRN offers a comprehensive package of health services, including behaviour change communication, a needle–syringe programme, psychosocial support, overdose management, HIV testing and counselling and sexually transmitted infection screening.
The COVID-19 pandemic posed a major challenge to UHRN’s clients, who even under normal circumstances face high levels of stigma and discrimination, police abuse and harassment, alienation and limited access to health and social services.
Sex workers, transgender men and women, people who use drugs and gay men lost livelihoods and faced even more violence and detention under the guise of lockdown measures. Movement was severely limited as motor vehicles required a special permit to operate.
UHRN rose to the challenge. A team of 25 peer educators used bicycles, funded by Frontline AIDS, and motorcycles to reach their clients where they were, providing antiretroviral medicine refills and condoms to clients who could not reach health facilities.
The organization rolled out virtual counselling services on risk reduction and addiction management through phone calls and WhatsApp. As part of personal protective equipment procurement, UNAIDS, through the National Forum of People Living with HIV/AIDS Networks in Uganda, provided soap and bleach to prevent COVID-19 infection among the drop-in centre’s dedicated staff, who worked right through the pandemic.
Despite the constraints of the pandemic, UHRN’s needle–syringe programme reached 287 clients in 2020, providing more than 15 000 clean needles and syringes, tourniquets, cotton balls, swabs, water ampoules, condoms, lubricant and safe-injecting information notes.
“I’m proud that harm reduction issues are taking a centre stage in Uganda,” says Mr Twaibu. “Community-led means ownership. Usually when the community is at the centre, accountability and community needs are prioritized,” he says.
Our work
Resources
Region/country
Related


Press Statement
UNAIDS condemns new law that further criminalizes and marginalizes vulnerable groups of people in Uganda
06 May 2021 06 May 2021GENEVA, 6 May 2021—UNAIDS is deeply concerned by the Ugandan parliament’s decision earlier this week to adopt the Sexual Offences Bill 2019, which includes provisions that further criminalize entire groups of people, such as the lesbian, gay, bisexual and transgender community, sex workers and people living with HIV. The bill criminalizes same-sex sexual relations, extends the criminalization of sex work and imposes mandatory testing for HIV and harsher sentences on people living with HIV than the general population accused of some similar crimes.
Although UNAIDS welcomes some aspects of the bill, such as the extension of protection from sexual harassment, violence and sexual exploitation to groups of people such as people in detention and migrant workers, it urges parliamentarians to reconsider the provisions that discriminate against some people.
“I am deeply troubled by the Ugandan parliament’s adoption of portions of this bill that further criminalize and marginalize vulnerable groups of fellow citizens and deny them their human rights, including their right to health,” said UNAIDS Executive Director, Winnie Byanyima. “Targeting people living with HIV, lesbian, gay, bisexual and transgender communities and sex workers increases stigma and discrimination and undermines the HIV response by preventing people from receiving the HIV treatment, prevention and care services that they so urgently need.”
UNAIDS recognizes the good progress that Uganda has made in recent years in reducing the impact of HIV. The number of AIDS-related deaths has fallen by 60% since 2010, with 1.2 million people out of 1.5 million people living with HIV on medicines to keep them alive and well. In addition, the number of new HIV infections has fallen by 43% since 2010. However, many vulnerable groups of people, such as gay men and other men who have sex with men and sex workers, continue to be less likely than the general population to receive the HIV treatment, prevention and care services they need.
UNAIDS urges Uganda to join the growing number of countries in Africa and globally that are removing unjust laws from their penal codes. The Ugandan parliament’s adoption of the new law comes just weeks before the United Nations General Assembly High-Level Meeting on AIDS, which will take place from 8 to 10 June 2021.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.


Feature Story
Fighting transphobia and violence one social media post at a time
30 March 2021
30 March 2021 30 March 2021“If you want to know that [Keem] is a man, just snatch away his phone and run,” taunted an Internet troll under Keem Love Black’s new profile picture on Facebook.
As a transgender woman living in Uganda, Ms Black is no stranger to the homophobia and transphobia that the lesbian, gay, bisexual and transgender (LGBT) community receives in the east African country.
“There is a lot of cyberbullying,” Ms Black says; for example, people often attack her for posting pictures of her in dresses and makeup.
Trolling is one motivation for Ms Black’s social media activism. She runs Trans Positives Uganda, a community organization that cares for transgender women sex workers and refugees who are living with HIV.
The online abuse mirrors the violence most transgender women experience in Uganda at the hands of their partners and even health-care providers. The marginalization has created a myriad of issues for transgender people in the country.
“I have been persistent on social media because I wanted to tell the world about transgender issues,” she says.
HIV disproportionately affects female sex workers and transgender women. The 2020 Global AIDS Update reports that in eight sub-Saharan countries nearly one in three transgender women said they had been physically attacked and 28% had been raped.
It is not only sexual violence that Ms Black relates, but also intimate partner violence.
“Our boyfriends really violate us,” Ms Black says.
She adds that transgender sex workers also meet the same fate at the hands of clients. However, while she believes that violence against transgender women needs to be addressed, the criminalization of LGBT people and sex work in Uganda stops survivors from speaking out.
“Sex work is illegal and our kind of sex is very, very illegal. You might end up getting arrested,” she says.
The stigma and discrimination often follows transgender people to consulting rooms at health facilities, where, while seeking treatment, they can be degraded and shamed.
“You tell a doctor, “I have anal gonorrhoea” and they will all be shocked. They'll call everyone, all the doctors, to see because they don’t believe in anal sex. They’ll say it’s against their religion,” says Ms Black.
When Ms Black lost an HIV-positive transgender friend to medical negligence in 2013, it was the final straw. Her friend was classified as a gay man, resulting in her not accessing health care that could have saved her life.
“I was like, “Okay, I have to start a campaign on social media” because people only knew about lesbians and gays,” Ms Black says.
That campaign grew from about 100 followers on Facebook to 50 000 followers today.
Ms Black’s Facebook page is mix of speaking about contemporary Ugandan issues, advocating for transgender people and fashion.
Despite her success on Facebook, Ms Black is turning to other social media platforms. “I am starting to use my Instagram page to advocate and sensitize people on transgender and health issues. I have noticed that social media is strong for advocacy,” she says.
In the last year, COVID-19 lockdowns had a big effect on women and girls and key populations. Sex workers, transgender men and women, people who use drugs and gay men lost livelihoods, faced violence and often are scapegoated as the transmitters of COVID-19.
“We are still suffering as sex workers who used to get clients from bars and clubs. The president hasn’t decided when bars will officially open yet,” she says. “During the lockdown we were all depressed; it came as a shock to us and we were not prepared at all. Some of us had a few savings, others didn’t have anything.”
Ms Black says people living with HIV faced many challenges in obtaining their treatment as public transport had stopped. “Many people stopped taking their HIV treatment,” she observes.
As with many communities across eastern and southern Africa, the transgender sex worker community displayed remarkable resilience in the face of adversity, somehow surviving the loss of livelihoods and food insecurity.
Without any formal financial support, Trans Positives Uganda teamed up with a sex-worker-led organization called Lady Mermaids, started a GoFundMe page and raised more than €5000 to buy and supply food to their members. They pulled through and, “Now that the lockdown has been eased, we are slowly getting back on our feet,” says Ms Black.
Through it all, Ms Black keeps it playful and often laughs at her naysayers. However, the memes on social media are not just fun and games for her. “Activism happens in many ways,” she says.
Find her on Facebook here and Instagram here.