Ethiopia has made significant progress in its HIV response in recent years and is on track to reach the UNAIDS 95-95-95 targets with 90% of people living with HIV in the country being aware of their HIV status; 94% of those diagnosed with HIV receiving antiretroviral (ARV) therapy; and 96% of people on ARV therapy achieving viral suppression.
But now, that progress is at risk. The recent pause in United States foreign assistance poses a direct threat to the lives and well-being of thousands of people living with HIV in Ethiopia and millions globally. Critical services are grinding to a halt, leaving people who rely on them facing an uncertain and dangerous future.
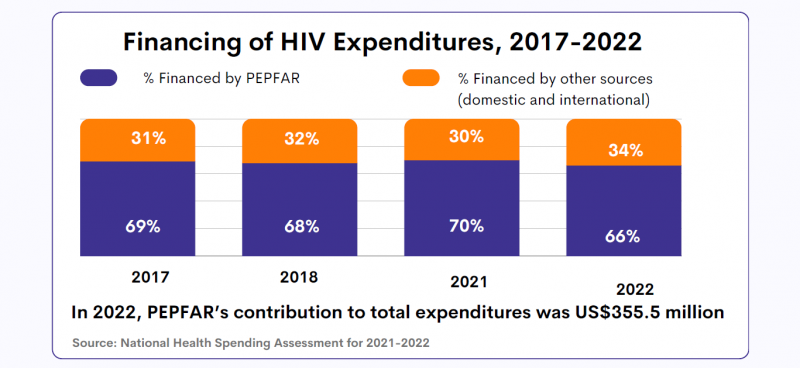
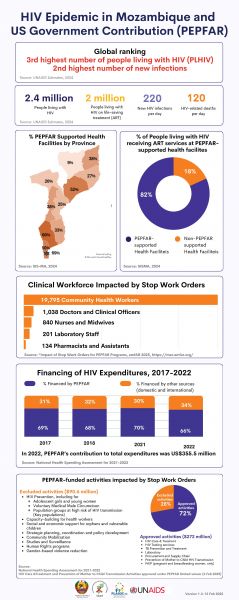
Ethiopia is heavily reliant on external funding for its AIDS response. PEPFAR provides 53% of HIV funding in the country. In 2023, UNAIDS’ estimates show that there were 610 000 people living with HIV in Ethiopia, 510 000 of whom were accessing antiretroviral treatment.
For women living with HIV, uncertainty is growing. Limited and unclear communication from healthcare providers and policymakers has left them in the dark about treatment changes, medication availability, and service disruptions. With no clear answers, they are forced to rely on rumors, fueling fear and anxiety.
“We don’t know what’s happening. Are services being cut permanently? Will we still get our medication next month? No one is telling us anything,” one woman shared.
To make matters worse, case workers and counsellors—once a vital source of medical and emotional support—are disappearing. These professionals were more than healthcare providers; they were trusted confidants who ensured women received care in a stigma-free environment. Their absence is leaving many feeling abandoned.
“They understood our struggles, checked in on us, and made sure we had what we needed,” another woman explained. “Without them, we feel forgotten.”
As services become increasingly unreliable, distress and fear are taking hold.
Shortages and desperate measures
Funding cuts bring shortages, and for women living with HIV, the fear of running out of medication is overwhelming. Access to antiretroviral therapy (ART) is essential—it keeps people alive. Yet many are already facing supply disruptions, and whispers of medication shortages are spreading panic.
“If I can’t get my medicine, what happens to me?” one woman asked. Women living with HIV who have been healthy for years now fear an uncertain future where their treatment is no longer guaranteed. People living with HIV who do not access antiretroviral therapy will eventually develop AIDS and die. To cope, many have resorted to stockpiling medication, traveling long distances and spending entire days at clinics in hopes of securing extra supplies. While understandable, this survival strategy comes at a heavy cost—disrupting work, family life, and daily routines. No one should have to live in fear of their next refill. The urgent need for stable, uninterrupted HIV treatment cannot be overstated.
Adding to the crisis, shortages extend beyond medication. The dwindling supply of test kits, including viral load tests, is threatening the future of diagnosis and monitoring. These tests are crucial to ensure that people living with HIV maintain undetectable viral levels, reducing transmission risks and protecting their health.
Fears have also been expressed around the availability of medications for HIV prevention, particularly for the prevention of vertical transmission of HIV. If the current pause in the supply of medical resources continues, the availability of these vital medications could be severely compromised, putting the lives of women and children at even greater risk. For women living with HIV who are pregnant, a lack of lifesaving medications for themselves also means their children can be born with HIV even though this is entirely preventable.
Without test kits and prevention measures, undiagnosed and untreated cases could rise dangerously. “We can’t afford to go backward,” one woman said.
A Plea for Action
The voices of these women reveal a stark and urgent reality—funding cuts have left people living with HIV in a state of uncertainty, with no clear path forward.
"Urgent intervention is needed,” stressed Tina Boonto, Country Director for UNAIDS Ethiopia. “UNAIDS is gathering information and developing funding solutions to address the shortfall, with proposals for both the government and external partners to ensure continuity of critical services. We hope Ethiopia's government will step up and lead in covering these essential services. We must act now to safeguard gains that have been made and succeed in securing sustainable support to people living with HIV."
While the future remains uncertain, one thing is clear: without swift action, the hard-won progress in Ethiopia’s HIV response is at risk.