VNM


Feature Story
Community networks extend arms to connect people to medicine in Viet Nam
17 April 2020
17 April 2020 17 April 2020When the Vietnamese Government introduced social distancing mid-March 2020 to respond to COVID-19, Binh Nam (not his real name), already on distance learning from his college since February, lost his part-time job at a small company. He decided to leave Ho Chi Minh City, which had a cluster of confirmed COVID-19 cases, to settle back in his home town, about 300 kilometres away.
“Going home seemed like the best option for me at the time,” Mr Nam said.
He arrived at his parents’ home just before buses shuttling people back and forth across the provinces stopped. With stricter lockdown measures taking effect in early April, he realized he was in a bind. He would run out of HIV treatment.
“I considered going to a local HIV clinic, but feared my HIV status would be disclosed,” he said. “I also could not buy antiretroviral medicine at private clinics because that would clear out my savings.”
And he definitely did not want to ask his parents, because they didn’t know he was living with HIV.
“I felt desperate,” he said. As a last resort, Mr Nam texted a man who runs a social media channel on HIV information, education and counselling that he follows.
Upon learning of Mr Nam’s situation, Nguyen Anh Phong, a representative of the Viet Nam Network of People Living with HIV (VNP+) in the south of Viet Nam and co-founder of the Lending a Helping Hand Fund, mobilized some funds to get him an antiretroviral therapy refill.
“This was among the first calls for help that made us notice more and more people were stuck in their home province with a limited amount of antiretroviral medicine,” Mr Phong said.
He and his VNP+ peers decided to form a group on one of the most popular social media chatting platforms in Viet Nam to find ways to connect people and help them collect medicine at clinics other than their own. More than 150 community members joined the group across the country.
Community feedback filtered back to the Viet Nam Authority for HIV/AIDS Control (VAAC) at the right time as it was drawing up emergency contingency plans. It was dealing with a hospital closed because of a temporary COVID-19 quarantine in Hanoi, so people couldn’t access HIV services or treatment. And with so many people stranded in the provinces, something had to be done.
VAAC issued new guidelines on HIV care and treatment during the pandemic developed with technical support from the United States President’s Emergency Plan for AIDS Relief, the Global Fund to Fight AIDS, Tuberculosis and Malaria and the United Nations.
“We invited the Viet Nam Network of People Living with HIV to join our technical discussions and to give us feedback because they know the challenges faced by people living with HIV,” said Phan Thi Thu Huong, VAAC Deputy Director in charge of HIV care and treatment.
The guidelines allow for multimonth antiretroviral therapy refills for all people on HIV treatment and for the provision of pre-exposure prophylaxis and tuberculosis medicines.
Provinces have been assigned focal points and hotline numbers for people who experience unusual symptoms.
More importantly, the standard referral requirements were eased in order to allow clients temporary access to alternative HIV clinics for antiretroviral therapy refills. VAAC also proactively resolved procurement challenges in order to avoid stock-outs, so Mr Nam and others could access HIV clinics of their choice for refills.
Viet Nam’s HIV epidemic is concentrated mostly among gay men and other men who have sex with men, transgender women, people who inject drugs and female sex workers and their intimate partners, with a rising HIV prevalence among gay men and other men who have sex with men .
“I believe that by joining hands, we can help all people get their refills so that no one misses their treatment because of COVID-19,” said Mr Phong.
Working hand in hand and getting results is what communities do best, according to Marie-Odile Emond, the UNAIDS Country Director for Viet Nam. “These networks are pillars of peer support and resilience and now more than ever they’re like an extended arm of the public health sector,” she said.
Resources
Region/country
Related






Feature Story
Catalysing zero discrimination in health-care settings in Thailand and Viet Nam
23 July 2018
23 July 2018 23 July 2018Stigma and discrimination in health-care settings is a major obstacle to ending AIDS. Widespread across the world, stigma and discrimination seriously reduces the quality of life of people who experience it and hinders their access to health and HIV services.
How to catalyse country initiatives and reduce stigma and discrimination in health-care facilities was the focus of a session at the International AIDS Conference on 23 July in Amsterdam, Netherlands. The session, Catalyzing Thailand and Regional Initiatives on Zero Discrimination in Healthcare Settings and Building Bridges Towards a Global Compact to Eliminate all Forms of HIV-Related Stigma and Discrimination, brought together representatives of the Governments of Thailand, Viet Nam and the Netherlands and representatives of regional civil society networks, the United States Centers for Disease Control and Prevention and UNAIDS.
Thailand is acknowledged as a pioneer in reducing stigma and discrimination in health-care settings in Asia through its innovative system-wide response. The event heard that the Thai stigma and discrimination reduction package is based on global measuring tools and contains a permanent monitoring system, evidence-informed actions at health facilities and community engagement at all levels.
Viet Nam piloted a stigma and discrimination reduction programme in Ho Chi Minh. At the session, Huu Thuy Do, Head of the Information, Education and Communication Department of the Viet Nam Administration for AIDS Control, explained how Viet Nam learned from cooperation with Thailand and how the Thai model was translated to the city level in Viet Nam.
Based on the experiences of Thailand and Viet Nam, speakers encouraged countries to foster cross-border links on stigma and discrimination reduction efforts in health-care settings in order to achieve more effective and efficient joint global action.
The participants also learned from the Dutch approach, which directs attention to the inequality of access to HIV prevention and treatment services while promoting an enabling legal environment to prevent stigma and discrimination.
The participants heard that the greater engagement of communities, people living with HIV and key populations in the development and monitoring of programmes against stigma and discrimination is a core element for successful stigma and discrimination reduction programmes. Their participation not only increases access by hard-to-reach communities, but also helps ensure that a rights-based approach is used.
The event concluded with the presentation of the Global Framework for Action, an initiative led by civil society that aims to catalyse and accelerate the implementation of commitments made to end HIV-related stigma and discrimination in different settings.
Quotes
“Thailand is a pioneer in the Asia region in developing a comprehensive programme to create health-care settings free from stigma and discrimination, leading to better health outcomes that go beyond HIV. In Thailand, we developed an intervention package that adapted global tools to our local context to stop stigma and discrimination. Stigma and discrimination is now systematically measured through surveys as part of that intervention package. The collected data are subsequently used to increase awareness, inform interventions and serve as a catalyst for system-wide actions.”
“What we should do is talk with religious leaders and talk with traditional leaders to make them see that discrimination and stigmatization is also a threat to society.”
“Discrimination at work links with health care. We find that people living with HIV all over the world face huge fears about disclosure, losing their jobs. Young people living with HIV have extremly high levels of unemployment.”
“Human rights, including stigma and discrimination and gender related vulnerabilities, are among the reasons for the serious HIV prevention gap and the insufficient progress that has been made in reducing new HIV infections in many regions of the world.”
"While HIV related stigma and discrimination are far from over, our experiences show that stigma and discrimination are both measurable and actionable. Reduction tools are available and when combined with collective leadership from key stakeholders and partners, we can end HIV related stigma through evidence based monitoring and effective interventions. Vision without action is just a dream but with action can make a difference. The world should unite to eradicate stigma and discrimination in all its forms."
"In the Thai model, the involvement of CSOs, PLHIV and KP’s goes beyond just an invitation to speak at a S&D reduction training. Communities are significantly involved in the entire process, from the programme consultation, planning over the implementation to the monitoring of progress."
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025

Update
Hospitals in South-East Asia ramp up efforts against HIV-related stigma
02 March 2017
02 March 2017 02 March 2017The Bamrasnaradura Infectious Disease Institute in Nonthaburi is one of Thailand’s premier hospitals in AIDS treatment and care. Its waiting rooms welcome many patients. This month, people waiting for appointments will see on hospital screens stories about people living with HIV who overcame stigma thanks to support from their communities. Bamrasnaradura is one of around 1000 hospitals in Thailand that have joined the zero discrimination in health-care settings campaign.
The Ministry of Public Health of Thailand, the Thai Network of People Living with HIV/AIDS (TNP+) and UNAIDS launched the campaign on 2 March at Bamrasnaradura.
“More than 30 years since HIV was detected in Thailand, stigma still remains a major challenge,” said Jessada Chokdamrongsuk, Director-General, Department of Disease Control, Ministry of Public Health. “Thailand is committed to ensuring health-care settings are safe and supportive environments.”
The campaign features a video with a short message from the popular Thai singer and UNAIDS National Goodwill Ambassador for Thailand, Chalatit Tantiwut, in which he encourages everyone to join the zero discrimination movement.
“Discriminating against anybody for any reason is always out of bounds,” said Mr Chalatit. “Making music is what I do best and I think it’s my duty to contribute to society and make some noise about zero discrimination.”
This initiative is part of an ongoing effort by the Ministry of Thailand to tackle stigmatizing behaviours and attitudes among staff towards people living with HIV. A survey of 1600 Thai health-care workers showed that more than 60% of workers feared an HIV infection while performing routine tasks and 90% admitted to at least one stigmatizing attitude.
The Ministry of Public Health, with support from civil society, UNAIDS and the United States Agency for International Development, has developed a comprehensive stigma reduction programme that is gradually being scaled-up to include all public hospitals.
“Thailand is showing how to tackle HIV-related stigma and discrimination in hospitals and clinics, “said Tatiana Shoumilina, UNAIDS Country Director for Thailand. “This problem is persistent and pervasive in many parts of the world. Only by overcoming this challenge will we Fast-Track the response to HIV and end the AIDS epidemic as a public health threat.”
“Zero Discrimination Day on 1 of March is now a well-recognized event both in Thailand and globally,” said Apiwat Kwangkaew of TNP+. “However, I would like to urge people to practice zero discrimination every day. Fear of HIV transmission and prejudice against people living with HIV are holding back access to treatment and care, employment and education.”
Thailand’s HIV-related stigma reduction programme for health-care workers is one of the world’s most ambitious initiatives and it has been such a success that it is being adapted and implemented in other South-East Asian countries.
After a survey in 2014 of people living with HIV found that stigma and discrimination in health-care settings was a significant issue in Viet Nam, health officials started exploring best practices and the Thai model seemed a good example.
In Ho Chi Minh City, the Viet Nam Administration for AIDS Control, with support from UNAIDS, has started pilot-testing the programme. The initiative began with a survey of three hospitals in the city, which led to a programme for health workers tailored to the Vietnamese context. A training in how to capacitate health-care workers to reduce stigmatizing attitudes and behaviours is under way in the city from the 28 February to 3 March.
“We will conduct an assessment at the end of this pilot project. I hope the lessons learned from this pilot will help further improve the methodology of measuring HIV-related discrimination in health-care settings and programme approaches, so we can expand the practice nationwide,” said Hoang Dinh Canh, Vice-Director, Viet Nam Administration for AIDS Control.
The Lao People’s Democratic Republic is also adapting Thailand’s initiative and Myanmar has expressed an interest in a similar approach. Discrimination is a barrier to accessing health services for people living with HIV globally, which is why UNAIDS dedicated this year’s Zero Discrimination Day on 1 March to elimination discrimination in health-care settings.
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025


Feature Story
Viet Nam opens its first opioid substitution therapy service for prisoners
25 November 2016
25 November 2016 25 November 2016“In 2010, I participated in a study visit to learn about prison-based methadone programmes in Spain. Witnessing the positive impacts of the programme on prisoners as individuals and prisons as a whole, I reported the results and recommendations of the visit to the Ministry of Public Security,” said Nguyen Xuan Truong, Chief Prison Officer at Phu Son Prison. “It has been quite a wait since then, but I am happy that Phu Son is the first prison in Viet Nam to provide methadone services for prisoners.”
The launch of the pilot opioid substitution therapy service in Phu Son Prison marks a significant milestone in the efforts of the United Nations Office on Drugs and Crime (UNODC) and the Government of Viet Nam for HIV prevention, treatment and care in Viet Nam’s prisons.
“Since 2009, the United Nations Office on Drugs and Crime has worked with the Government of Viet Nam to provide opioid substitution therapy as part of a comprehensive HIV service package for people who are living and working in prisons,” said Christopher Batt, UNODC Officer-in-Charge.
Opioid substitution therapy is an evidence-informed service for opioid dependence. It reduces opioid use by eliminating withdrawal symptoms and drug craving, decreasing the risk of the transmission of HIV or other bloodborne infections and criminal behaviour. In addition, it integrates the patient into a continuum of care during and after his or her stay in prison.
“The opioid substitution therapy service unit is expected to enhance the quality of life of prisoners, reducing transmission of HIV and other diseases and decreasing the rate of relapse and overdose in prison settings,” Mr Batt added.
The Viet Nam Ministry of Public Security estimates that three out of 10 prisoners use drugs.
Prisoners are at higher risk of becoming infected with HIV or other bloodborne infections, including viral hepatitis B or C, relapse or overdose if their treatment needs are not met.
A second opioid substitution therapy service unit will soon be launched in Thanh Xuan Prison, and there are plans for the service to expand to other prisons.
Hands up for #HIVprevention — World AIDS Day campaign
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025


Feature Story
Decentralization of HIV testing services to increase access for people who inject drugs in Viet Nam
12 October 2016
12 October 2016 12 October 2016In Viet Nam, the Authority for HIV/AIDS Control and the Ministry of Health piloted outreach HIV testing services to increase uptake among people who inject drugs and their partners. Bi-monthly HIV testing was offered in villages where there were large communities of people who inject drugs.
The outreach team included two health service staff, one village health worker and one peer educator. People who inject drugs and their partners were invited to a convenient location and offered HIV counselling and rapid HIV tests. Reactive test results were sent for confirmatory testing and clients with a confirmed diagnosis of HIV were counselled and linked to clinics for treatment and care.
From September 2014 to January 2015, 8.9% of people tested were newly diagnosed with HIV—approximately four times higher than the percentage observed at district primary health-care facilities. The results of this pilot programme suggest that the provision of community-based HIV testing services is a feasible and efficient method of increasing knowledge of HIV status among people who inject drugs and their partners, as well as other key populations. Peer educators and village health workers were instrumental in reaching the target population. This model will inform the development of national guidelines on community-based HIV testing. Source: http://who.int/hiv/pub/guidelines/hiv-testing-services/en/.
To find out more about harm reduction, please go to the World Health Organization harm reduction page at http://who.int/hiv/topics/idu/en/ .
Resources
Consolidated guidelines on HIV testing services
Do no harm - Health, human rights and people who use drugs
Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations
Guidance on prevention of viral hepatitis B and C among people who inject drugs
Harm Reduction International “Global State of Harm Reduction”
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025
Documents
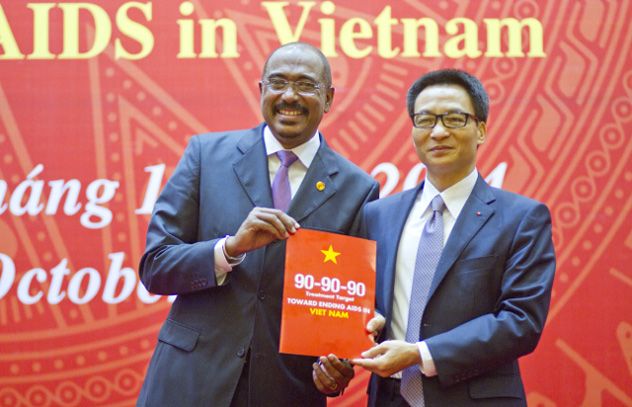
90-90-90: A transformative agenda to leave no one behind
25 October 2014
This bold new set of targets, 90-90-90, will do more than reduce new HIV infections and AIDS-related deaths. It will be a transformative agenda for reaching people who are left behind. We have heard from Minister Tien that—with a lot of effort—they have been able to put 38 percent of people in Vietnam who need it on HIV treatment. By 2020, our cascading targets are to have at least 90 percent of all Vietnamese living with HIV know their diagnosis; 90 percent of those people to be receiving antiretroviral treatment; and 90 percent of those on HIV treatment to have an undetectable viral load.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
29th Ordinary General Assembly of the Organization of African First Ladies for Development
16 February 2025




Feature Story
Viet Nam gets more value for money through integration of HIV services
24 October 2014
24 October 2014 24 October 2014A “one-stop-shop” health centre in Hanoi is providing integrated HIV and other healthcare services that are achieving progress and maximizing investments in the AIDS response in Viet Nam. Hanoi’s South Tu Liem district health centre is a model that the Viet Nam Authority for HIV/AIDS Control plans to replicate in high-burden areas of the country.
“Today I saw three things which will help not only Viet Nam but also other countries; integration and decentralization of services; a patient-centred approach; and peer support,” said UNAIDS Executive Director Michel Sidibé during a tour of the health centre. “It is important to bring people together from different social backgrounds and support them to become actors for change for HIV.”
The health centre provides a full range of HIV services to key populations, including people who inject drugs, sex workers and men who have sex with men. It is also the primary healthcare centre for the district’s general population. More than 500 people are receiving antiretroviral treatment and more than 300 people who inject drugs are on methadone maintenance therapy. The health centre also has peer outreach services, including needle and syringe distribution, HIV counselling and testing, tuberculosis diagnosis and treatment, prevention of mother-to-child transmission, as well as home-based care and peer support for treatment adherence.
Integration and decentralization of HIV service delivery systems, including health systems strengthening, is one of the strategic priorities put forward by Viet Nam’s new Investment Case for an optimized HIV response. The Investment Case, developed by the Minister of Health with support from UNAIDS and other development partners, aims to improve the effectiveness, efficiency and sustainability of the national response as international donors reduce their support to rapidly developing Viet Nam.
During a meeting with Mr Sidibé the Minister of Health Nguyen Thi Kim Tien said that Viet Nam is committed to following the Investment Case and increasing the domestic budget for the HIV response. However, she said Viet Nam needed the continued support of the international community to achieve global HIV targets. “We are faced with some challenges and difficulties, but we will try our best and work to sustain the HIV response and make greater achievements,” said Nguyen Thi Kim Tien.
The Investment Case finds that integration and decentralization will save money and help sustain HIV services by avoiding parallel spending on infrastructure, human resources and commodities; taking advantage of the health system’s existing cost efficiencies; creating links between related services; and facilitating referrals.
This approach will also help address some of the concerns that civil society have in Viet Nam. People living with HIV and key populations at higher risk of HIV infection worry that less donor funding could mean reduced access to affordable services.
“I’ve been on antiretroviral treatment for 10 years and I feel very good, like many other people,” said Nguyen Xuan Quynh, 41. “I heard that international support will end soon and maybe we must pay. But most of us are very poor.”
As part of his two-day official visit to the country, Mr Sidibé also met with leaders of civil society networks. He urged them to continue raising their voice on the issues that matter most, and to work closely with the public healthcare system to play a greater role in the provision of lower-cost and higher-impact HIV services.


Update
Viet Nam is the first country in Asia to commit to new HIV treatment targets
27 October 2014
27 October 2014 27 October 2014The Government of Viet Nam announced on 25 October its commitment to new targets intended to rapidly expand HIV treatment, thus becoming the first country in Asia to adopt the 90–90–90 targets.
UNAIDS Executive Director Michel Sidibé joined Deputy Prime Minister and Chair of the National Committee for AIDS, Drugs and Prostitution Prevention and Control, Vu Duc Dam, the Minister of Health, Nguyen Thi Kim Tien, and other development partners at the launch of Viet Nam’s 90–90–90 targets in Hanoi.
Around the world, momentum is building behind reaching 90–90–90 by 2020: 90% of people living with HIV will know their HIV status; 90% of people who know their status are on HIV treatment; and 90% of all people on treatment will have undetectable levels of HIV in their body (known as viral suppression). Viet Nam’s commitment to these ambitious targets puts the country on course to ending its AIDS epidemic by 2030.
There were 250 000 people living with HIV and 14 000 new HIV infections in Viet Nam in 2013. In 2014, more than 87 000 people were accessing HIV treatment, a 30-fold increase since 2005, but just one third of all people living with HIV.
Quotes
“Today we have the 90–90–90 targets and we are looking forward to ending the AIDS epidemic by 2030. With the support from the international community and Vietnamese society, we can achieve our goals.”
“The ultimate payoff will be ending the AIDS epidemic by 2030. It will be our greatest gift to the people of Viet Nam, to the world and to generations yet to come. It will be our lasting legacy.”
“We will invest more to increase the number of people on treatment and to increase the quality of the treatment, including ensuring that national social health insurance covers the medical expenses of people living with HIV.”
Related
Documents
UNAIDS' official visit to Viet Nam
UNAIDS Executive Director Michel Sidibé visited Viet Nam on 24 and 25 October 2014.
Related
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
 UNAIDS mourns the passing of Hage Geingob, President of Namibia
UNAIDS mourns the passing of Hage Geingob, President of Namibia

05 February 2024
 New report from UNAIDS shows that AIDS can be ended by 2030 and outlines the path to get there
New report from UNAIDS shows that AIDS can be ended by 2030 and outlines the path to get there
13 July 2023
Checklist and reference list for developing and reviewing a national strategic plan for HIV
16 May 2023
Documents
Children born of hope in Viet Nam
Children born of hope in Viet Nam - Photo feature from the UNAIDS OUTLOOK Report 2010. Photo
Credit: UNAIDS/Justine Mott
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025
 Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment
Lost and link: Indonesian initiative to find people living with HIV who stopped their treatment

21 January 2025
UNAIDS data 2024
02 December 2024
Take the rights path to end AIDS — World AIDS Day report 2024
26 November 2024
 PrEP for her: Cambodia, Indonesia, Papua New Guinea and the Philippines prepare to introduce the Dapivirine ring to help prevent HIV
PrEP for her: Cambodia, Indonesia, Papua New Guinea and the Philippines prepare to introduce the Dapivirine ring to help prevent HIV

22 November 2024
 Can this innovation change the way people think about HIV?
Can this innovation change the way people think about HIV?

16 October 2024
 Women living with HIV in China unite to confront discrimination
Women living with HIV in China unite to confront discrimination
14 October 2024