
Feature Story
Explaining harm reduction with hard hats, seatbelts and sunscreen
23 June 2017
23 June 2017 23 June 2017Fastening a seatbelt when driving, wearing a hard hat on a construction site and slapping on sunscreen when out in the sun all lessen potential harms from the risks being taken. This is how the Harm Reduction Action Center (HRAC), based on Colorado, United States of America, introduces the principles of harm reduction for drug use in a video entitled Harm Reduction 101.
The video—a stick-figure animation—explains that 47 000 people died from drug overdoses in the United States in 2014. According to StoptheClockColorado.org, every 9 hours and 24 minutes someone dies from a drug overdose in Colorado—such deaths are preventable with harm reduction. Harm reduction includes linking people to health services, giving people access to naloxone—a drug that reverses the effects of an opioid overdose—and making sterile needles and syringes available to prevent the spread of HIV and viral hepatitis.
“Harm reduction keeps people alive, that is the nature of the business we are in,” said Lisa Raville, Executive Director of HRAC, which has provided emergency and health services to injecting drug users in Colorado since 2002. HRAC offers sterile syringes, proper syringe disposal and access to HIV testing, as well as health education classes, street outreach and referrals to mental health and substance abuse treatment.
The video, Ms Raville explains, allows people to understand the framework and the logical next step, which is installing supervised injection facilities. The video notes that in the 102 supervised injection facilities across the world, there has yet to be a single fatal overdose.
Matt Slaby and the creative agency Luceo produced the video with the aim of making a complex issue accessible to all. “Harm reduction has struggled with normalization and has been misrepresented for decades, so we pointed to other things that have come to be the norm in our society, like seatbelts, designated drivers and hard hats,” Mr Slaby said.
“Our aim is to reduce the negative impact of years of archaic drug policy, because jailing and repression only drives drug use underground, increases overdoses and leads to the spread of HIV,” Mr Slaby added.
Millions of people who use drugs continue to be criminalized and marginalized in the United States and other countries. Despite this, levels of drug use have remained unchanged. However, countries that have moved away from punitive laws and policies against drug users and have increased investment in harm reduction have seen a drop in new HIV infections and improved health outcomes. These policies have lowered levels of drug-related crime and reduced pressure on the health-care and criminal justice systems.
Harm reduction is cost-effective. According to the Harm Reduction Coalition, the lifetime cost of medical care for each new HIV infection is more than US$ 400 000, but if the same amount of money was spent on needle–syringe exchange programmes at least 30 new HIV infections would be prevented.
UNAIDS believes that the world cannot continue to ignore the evidence. Michel Sidibé, UNAIDS Executive Director, said, “We must reduce the impact of HIV and other harms related to drug use and adopt a new course of action—to treat people who use drugs with dignity and respect and to provide them with equal access to health and social services.”
UNAIDS calls for the global adoption of a people-centred, public health and human rights-based approach to drug use. Reducing the harms of drug use will contribute to the end of the AIDS epidemic and the achievement of the Sustainable Development Goals.
HARM REDUCTION 101 from LUCEO on Vimeo.
Video
Region/country
Related
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025

Feature Story
New survey finds high levels of HIV discrimination in Republic of Korea
22 June 2017
22 June 2017 22 June 2017N.C. Cho started feeling run down, with muscle aches and a high fever, in 2014. At the time, he was 32 years old and working in the fashion industry in Seoul, Republic of Korea.
“I went to several hospitals, but nobody could come up with a diagnosis,” said Mr Cho. “Finally, I went to see a third doctor, who did a whole series of tests.”
Little did he know that among the battery of blood work, he was also being tested for HIV.
“I was really angry when the doctor came back and told me I had HIV,” said Mr Cho. “I was educated enough to know that such tests should not be conducted without my consent. “The doctor basically told me you may be able to stay healthy, but you could also get very sick, lose a lot of weight and then die. He gave me some medicine for a cold and made it pretty clear that I should not come back.”
Mr Cho was active in Seoul’s gay community and could turn to peers who introduced him to quality HIV services. He was able to access HIV treatment shortly after his diagnosis and is now feeling fine.
A new survey conducted by the Korean Network of People Living with HIV/AIDS (KNP+) finds that Mr Cho’s experience is far too common for people living with HIV in the Republic of Korea. The Korean People Living with HIV Stigma Index, which is the first peer-led survey in the country to detect and measure how HIV-positive people experience stigma and discrimination, was released on 22 June. Its development was supported by the Global Network of People Living with HIV, the International Community of Women Living with HIV and UNAIDS.
The survey, which was conducted from March to June 2016, found that 62% of people questioned reported that they were tested for HIV without their knowledge. This is high compared to other countries in Asia that have conducted similar peer-led surveys. In Viet Nam, 13% of people living with HIV reported similar experiences and in Nepal the figure was 9%. In addition, 17% of people surveyed in the Republic of Korea said their status was disclosed by medical staff to others without their consent.
“For too long, the voices of people living with HIV have been absent in policy-making,” said Son Mun Soo of KNP+. “This study documents their experiences and shows that the government, employers, health-care workers and communities must do much more to guarantee the rights of people living with HIV. A comprehensive anti-discrimination law must be enacted to protect their rights.”
UNAIDS and the World Health Organization strongly recommend that HIV testing only be undertaken with a person’s informed consent.
“Health-care settings should be stigma-free environments that ensure people living with HIV not only stay healthy, but their loved ones and community are also protected from HIV,” said Steve Kraus, Director of the UNAIDS Regional Support Team for Asia and the Pacific. “It is imperative that we have protective laws and empowered communities.”
The study found that while the general level of education of survey respondents was slightly higher than that of the general population, their employment was more precarious. Only 43% of respondents were full- or part-time employees and 42% were living on less than the Republic of Korea’s minimum household income. About one in 10 respondents who were full- or part-time employees said they had disclosed their HIV status to their employer and about half reported discriminatory reactions.
The survey found that while most respondents disclosed their HIV status to their families out of a sense of obligation, almost 40% reported isolating themselves from loved ones because of their HIV status. Self-stigma was also high among respondents, with 75% feeling self-blame and more than a third experiencing suicidal thoughts.
As the first research of its kind into the stigma and discrimination experienced by people living with HIV in the Republic of Korea, KNP+ views the Korean People Living with HIV Stigma Index as a positive step forward to ensuring that the rights and needs of people living with HIV are protected and met. The study calls for more research on how to strengthen anti-discrimination protection in the workplace and demands training for health-care providers that emphasizes the rights of patients, as well as strong measures and penalties to prevent patient privacy violations.
Mr Cho participated in the study as a peer educator and found the experience empowering.
“There is a lot of self-stigma among people living with HIV,” said Mr Cho. “So I try to portray a positive outlook. I want others to feel positive about their life and to know that they can be HIV-positive but continue to live their life to the fullest.”
UNAIDS is working to empower people living with, at risk of and affected by HIV to know their rights and to access justice and legal services to prevent and challenge violations of human rights.




Feature Story
Faith-based organizations vital to the response to HIV
19 June 2017
19 June 2017 19 June 2017Stepping up the role of faith-based organizations in the response to HIV can present new opportunities to save the lives of children living with HIV in western and central Africa, agreed the participants at a meeting held in Abuja, Nigeria, on 14–16 June.
The Regional Consultation on Early Diagnosis and Treatment for HIV-Positive Children: Strengthening the Engagement of Faith-Based Organizations saw more than 100 representatives of faith-based organizations, governments and organizations of people living with HIV come together to discuss the role of faith-based organizations in the response to HIV. The participants, who were mainly from the Democratic Republic of the Congo, Nigeria and Zimbabwe, agreed that churches, mosques, religious leaders and the health facilities they support are critical to ensuring that HIV among children is diagnosed and treated.
The participants developed plans to create demand for testing and treatment, as well as to support people living with HIV to stay in care. The participants also planned to build the capacity of faith-based service providers to deliver quality HIV services for children and discussed the strengthening of age-appropriate HIV and sexual health education in faith schools.
The event was organized by Caritas Internationalis, UNAIDS and the United States President’s Emergency Plan for AIDS Relief, with the support of Caritas Nigeria.
Quotes
“Zimbabwe’s theme remains prevention, prevention, prevention as we close the tap on new HIV infections. Appropriately, the faith-based organizations are now fully at the centre of the HIV prevention agenda.”
“If the United States President’s Emergency Plan for AIDS Relief, UNAIDS and governments are prepared to invest in a conference like this one, it is because they believe faith-based organizations have a specific and important role to play in the HIV response.’’
“We have to be connected—faith-based organizations with faith-based organizations, governments with governments—in order to deal with paediatric AIDS. After these consultations, now is the time to work.”
“This forum shows a desire to do things differently and explore new opportunities in addition to what already exists. Where is our humanity if we continue to allow children to be born with HIV?”
“I am excited to hear about the potential integration of pastoral care, clinical care and education: linking people living with HIV and their families to support systems in communities of faith. This provides a comprehensive continuum of care that not only helps get people tested and on treatment, but helps them to stay in care.”
“We need faith-based organizations to help Fast-Track the response to HIV for children because they are closer to the communities than the rest of us.”
Region/country





Feature Story
United States leadership crucial in ending AIDS
19 June 2017
19 June 2017 19 June 2017The Executive Director of UNAIDS, Michel Sidibé, has spoken out about the need for continued leadership in global health from the United States of America to end the AIDS epidemic. During a speech at the Foundation for AIDS Research (amfAR) Capitol Hill Conference, Mr Sidibé said, “What scares me is the move to a conspiracy of complacency. People think that AIDS is done, that we can move on. Now is not the time to lose our momentum.”
Senior United States officials, researchers, implementers, policy-makers and advocates were present at the event, which was held to review the substantial progress in the response and what is required to end the AIDS epidemic by 2030.
The conference, Making AIDS History: a Roadmap for Ending the Epidemic, was chaired by Susan Blumenthal, amfAR’s Senior Policy and Medical Advisor and former United States Assistant Surgeon General. Speakers acknowledged the strong bipartisan commitment and leadership of successive United States Administrations and the Congress, which have saved millions of lives and made it possible to begin envisaging a world without AIDS. It was noted that cuts to international assistance, multilateral organizations and United States global AIDS programmes would have irreversible and devastating consequences.
Deborah Birx, United States Global AIDS Coordinator and Special Representative for Global Health Diplomacy, presented data illustrating dramatic results, including progress towards reaching the 90–90–90 targets among adults in Malawi, Zambia and Zimbabwe and corresponding declines in new HIV infections.
“It is remarkable what we have achieved, bringing together governments and communities, with the support of UNAIDS and collaboration with the Global Fund to Fight AIDS Tuberculosis and Malaria,” said Ms Birx. “These essential partnerships make hard-earned United States taxpayer dollars go so much further and amplify our results.”
Mr Sidibé emphasized that partnership and global solidarity are paying off—in both economic terms and in the number of lives that have been saved. “The generosity and compassion of the American people has helped us move from despair to hope,” he said.
Kenneth Cole, Chief Executive Officer of Kenneth Cole Productions, Chairman of amfAR and International Goodwill Ambassador for UNAIDS, referred to commitments made by governments to Fast-Track the response to the epidemic and said that strong, continued United States leadership is essential to seizing the moment and dramatically scaling-up access to HIV treatment and prevention services. “We are at a tipping point and tipping points can go one of two ways—we have to end up on the right side. We have come too far to see 35 years of hard won progress grind to a halt,” said Mr Cole.
UNAIDS is leading global efforts to end the AIDS epidemic and is working with countries, donors, civil society and partners to increase action and Fast-Track the response to HIV over the next four years to end AIDS as a public health threat by 2030.



Feature Story
Young influencers debate HIV and discrimination in Brazil
16 June 2017
16 June 2017 16 June 2017YouTubers, influencers and virtual activists took part in inspirational conversations about HIV and discrimination in São Paulo, Brazil, on 30 May.
“No one in my group of friends and very few of my generation know anyone who died because of AIDS. Because past generations lived and witnessed so many AIDS-related deaths, there was this culture of fear, which is no longer present among us. However, we have not replaced this culture of fear with anything more positive,” said young Brazilian YouTuber Murilo Araújo, who describes himself in his channel, Muro Pequeno, as, “Proud to be gay, black, catholic, proud to be resistance in a society that tells me all the time that I cannot be any of that.”
Taboos, stigma both within and against the gay community, discrimination against people living with HIV and communicating to a highly connected generation were some of the topics debated. The event was moderated by renowned journalist and UNAIDS Goodwill Ambassador for Brazil Glória Maria, who asked, “Why do you think the HIV epidemic seems to be rebounding among young people, especially among gay men?” to trigger the first conversation.
“We saw all this in our biology classes, we saw it in campaigns. But it’s really hard to associate what they teach us with our real life, with relationships, with affection and with sexual experiences. I think this is the missing link we are trying to connect with our work on YouTube,” said actor and YouTuber Gabriel Estrela, from the Projeto Boa Sorte channel. “It seemed like something very distant from my reality, something that only happens in the movies.”
New HIV infections have grown substantially among young men, especially young men who have sex with men, in Brazil in the past decade. According to data from the Ministry of Health, they almost tripled among youth aged 15 to 19, and more than doubled among those aged between 20 and 24.
Nathan Fernandes, the Editor of Galileu Magazine, one of Brazil’s most influential monthly magazines among young people, said that, “The press played a very important role at the beginning of the epidemic. The first cases were reported even before civil society was able to organize itself for a common response. The problem is that the same press also reinforced stigma and discrimination by describing AIDS as the “gay plague” or “gay cancer”, among other things. We are now very aware that we have to be very careful with what and how we report,” he added.
As gay social networks become popular, discussions about HIV and prevention tend to gain the spotlight, said André Fischer, Director of Hornet Brazil. “We can’t run away from the fact that AIDS is still an important issue for the gay community. It is still a strong taboo subject. But we see more and more people being able to come out and reveal their HIV-positive status.”
Digital activist Matheus Emilio said it is possible to include HIV in the discussions of social networks and help break stigma and discrimination around the subject. Mr Emilio runs the Facebook page Menino Gay, with a focus on the lesbian, gay, bisexual, transgender and intersex community, whose posts reach more than 600 000 followers. “Besides talking about culture, music and lesbian, gay, bisexual, transgender and intersex rights, I also include information on HIV, health and prevention”, said Mr Emilio, who was diagnosed HIV-positive two years ago.
“Our goal is to promote connections among people and to promote a debate on HIV, with a focus on young gay men and other men who have sex with men, going beyond the point of view of science, health and public management. We want to create a debate involving young people, society, digital culture and human rights within the universe of young gay people,” said Georgiana Braga-Orillard, UNAIDS Country Director for Brazil.
The series of debates, #EseFosseComVocê? (What if it happened to you?), was organized by UNAIDS in partnership with the British Embassy in Brazil, Ogilvy Brazil, Hornet and Cultura Inglesa. The event, which was live-streamed on several accounts on Facebook, reached more than 300 000 online viewers.
Region/country
Related




Feature Story
Protecting the rights of sex workers
02 June 2017
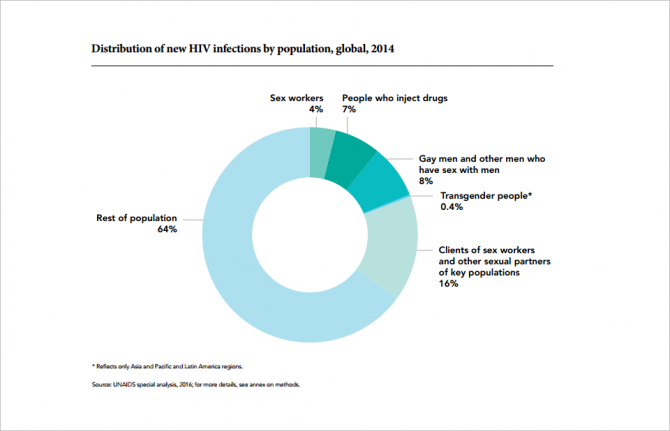
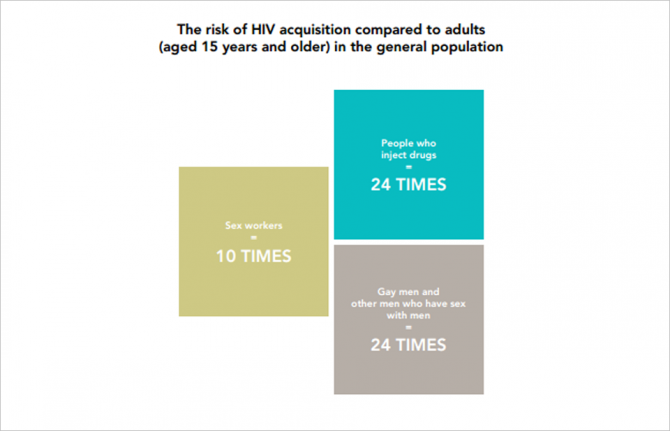
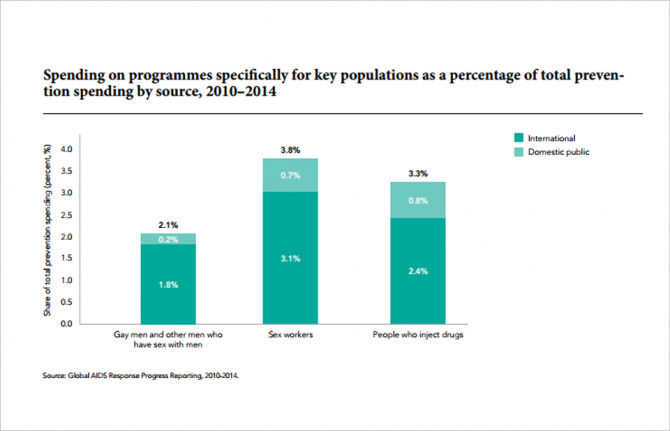
02 June 2017 02 June 2017Sex workers continue to face criminalization, violence, discrimination and other forms of human rights violations which increase their risk of acquiring HIV.
Sex workers—female, male and transgender adults who have consensual sex in exchange for money or goods, either regularly or occasionally—are among the populations that are being left behind in the HIV response. HIV prevalence among sex workers is 10 times higher than among the general population, and sex workers are poorly served by HIV services.
Many of the human rights challenges, vulnerabilities and barriers sex workers face in accessing HIV services are due to criminalisation and the restrictive laws, regulations and practices they face. Selling and/or buying sex is partially or fully criminalized in at least 39 countries. In many more countries some aspect of sex work is criminalized, and in other countries general criminal law is applied to criminalize sex work (for example, laws against loitering and vagrancy).
The threat of detention, as well as laws that allow for the use of condoms as evidence of sex work, are serious barriers to the availability and uptake of HIV prevention programmes and services. When possession of condoms is used by the police as evidence of sex work, this greatly increases the risk of HIV among this key population. Even where sex work is not criminalized, sex workers are rarely protected under the law
Furthermore, studies have shown that female sex workers are subjected to high levels of violence—in Haiti, for example, 36.6% of female sex workers report physical violence and 27.1% report sexual violence.
However, sex worker organizations are leading efforts to advance their human rights and access to HIV services in many countries. In South Africa, sex worker-led organizations worked closely with the Ministry of Health to develop the South African National Sex Worker HIV Plan 2016–2019, which calls for an enabling environment for the protection of, and access to HIV services for, sex workers. The nationwide programme enlisted peer motivators to assist in the distribution of condoms and lubricant, information on sexually transmitted infections and HIV prevention, paralegal services and health service referrals. Community empowerment services that aim to reduce violence, stigma and discrimination included sensitization training and a helpline for sex workers.
In India, sex worker organizations are working with the police and the community to reduce violence against sex workers, and to establish health and social services for themselves and their families.
There is growing evidence of the importance of addressing the structural and legal barriers that affect sex workers. Ending the AIDS epidemic as a public health threat would require translating this evidence into practice, including by ensuring that governments and all stakeholders prioritize and intensify efforts to protect the human rights of sex workers and to increase their access to HIV prevention and treatment services.
Related






Feature Story
Community groups are reducing stigma in health-care settings in Asia
26 May 2017
26 May 2017 26 May 2017Dy Sokha has a ready smile and calls out friendly greetings to doctors, nurses and patients as she walks through the bustling hallways of the Khmer Soviet Friendship Hospital in Phnom Penh, Cambodia. She is brightly dressed in a peach pink shirt and is a full-time counsellor with the ARV Users Association (AUA), a community-based organization providing services to people living with HIV.
“Sometimes at the beginning of a counselling session, the client won’t look at my face,” said Dy Sokha. “They put their face down; they scratch their fingernails. They are so shy. For these difficult cases, I must open up about myself.”
Dy Sokha was diagnosed with HIV about 20 years ago and began taking antiretroviral medicine in 2004. The HIV treatment improved her health significantly and now gives her the strength to lead a busy life as a counsellor.
“I have become a role model for my clients, as they can see I am successful and they understand that just because you have HIV, it does not mean you have to disappear from society,” she said.
AUA, which is active in seven hospitals in two provinces, is one of a few community-based HIV organizations in Cambodia whose staff work directly alongside health-care providers. While the organization provides a range of services, such as counselling on treatment adherence and HIV prevention, it places a particular focus on preventing stigma and discrimination in the hospitals in which it works.
Eighty-five per cent of AUA’s 40 staff members are people living with HIV and so they know first-hand how discrimination can lead to social isolation and negatively affect a person’s health and well-being. The group facilitates connections between clients and health-care providers and holds regular meetings with hospital staff to provide feedback.
“We coordinate with different stakeholders to meet and encourage communication between people living with HIV, service providers and civil society,” said Sienghorn Han, Executive Director of AUA.
In 2015, AUA was trained by Asia Catalyst to document human rights violations in health-care settings. The cooperation was part of a study that Asia Catalyst conducted in four countries in Asia, which found discrimination evident in many areas, from denial of services and segregation to arbitrary additional fees for health services.
When AUA receives a discrimination case, it acts as a mediator, trying to find a solution that is acceptable to both health-care workers and clients.
“We keep good contact with all levels of the hospital,” said Dy Sokha. “The staff and I sit together—the doctor, the client and myself—to understand the problem in order to help the doctor do his or her best.”
AUA also holds counselling sessions with clients that aim to give them accurate information, as well as empower them to advocate for their rights and negotiate with health-care providers.
Bopha, who prefers to use a pseudonym and is living with HIV, found that AUA was especially helpful when she became pregnant in 2013. “AUA explained everything, especially how to take care of my pregnancy and how to disclose my HIV status to my doctor so that I could access antiretroviral medicines to prevent the transmission of HIV to my daughter,” she said.
Cambodian health officials acknowledge that AUA provides services that help busy health-care workers. Ngauv Bora, Deputy Chief, Technical Bureau of the National Centre for HIV/AIDS, Dermatology and STDs, said, “For clients, AUA staff are like friends and they trust them more than the hospital counsellors. AUA is helping to create an enabling environment.”
The organization is one of more than a dozen community groups that, along with health officials and international experts from 12 countries, participated in the first Asia Regional Consultation on Addressing HIV-Related Stigma and Discrimination in Healthcare, which took place on 25 and 26 May in Bangkok, Thailand.
The regional consultation provided a platform for countries to achieve tangible objectives, with technical assistance from partners. Community organizations were recognized as crucial partners in the drive to eliminate stigma and discrimination.
UNAIDS is working with countries to empower people living with, at risk of and affected by HIV to know their rights and to access justice and legal services to prevent and challenge violations of human rights.
Region/country

Feature Story
Immune Nations
23 May 2017
23 May 2017 23 May 2017In a dark room, you see a shadow of yourself on a large screen—white lights create spots that arc across the screen and onto your body.
It’s the deadly Shadowpox trying to infect you.
Watching your shadow-self on the screen, you try to sweep the spots off your body. More spots appear and you realize the virus isn’t just attacking you, it’s attacking everyone around you. What do you do now?
This is the type of question people are faced with in Shadowpox, an art installation that is part of the new Immune Nations exhibition. Using interactive projections, Shadowpox gives participants a unique experience of fighting a virus with a vaccine while trying to save the people around them by what public health officials call herd immunity—when enough people are immunized against a disease that other people who are not immunized have some protection against infection, because the spread of contagious disease is contained.
The questions and decisions people face when interacting with Shadowpox are similar to public health scenarios being played out around the world. And it is exactly the kind of thinking a grant by the Research Council of Norway tried to provoke by bringing artists, researchers and policy-makers into a room together to see how they might reframe the current discourse surrounding vaccination.
“We are interested in exploring the role that art and culture could have in informing global health decision-making,” said Steven Hoffman, a law professor at the University of Ottawa and co-lead of the Vaccine Project.
In the summer of 2015, renowned artists and experts gathered at the University of Ottawa, where concepts for the evidence-based art exhibition emerged. Shadowpox was imagined by a group of collaborators led by Alison Humphrey and Caitlin Fisher. The idea started with a new vaccine-preventable disease composed of viral shadows. The concept was part fact and part science fantasy. The mixed-reality installation combines real-world statistical data with live-animated digital effects. “The final work is equally stunning, fun and provoking—everything needed to engage people on the issue of vaccines,” said Natalie Loveless, a co-lead and curator for the exhibition.
The Vaccine Project is a multiyear collaboration that has spanned continents and cultures. “More than 100 people and organizations are collaborating on this exhibition,” said Sean Caulfield, a co-lead of the project. “We have representatives from virtual reality labs and universities to governments and the United Nations.”
The exhibition first premiered at Galleri KiT, Trondheim Academy of Fine Arts, in Norway in March 2017 and travelled to UNAIDS headquarters in Geneva, Switzerland, where it will be opened by the First Lady of Namibia Monica Geingos on 23 May. The works of art will be exhibited at UNAIDS until 30 June 2017.
Resources
Related





Feature Story
Germany—ready to lead by example to end AIDS
23 May 2017
23 May 2017 23 May 2017During a recent visit to Germany, the Executive Director of UNAIDS, Michel Sidibé, met with representatives of the federal government, local government, civil society, communities affected by HIV and the private sector.
Under the leadership of Chancellor Angela Merkel and the Minister of Health, Hermann Gröhe, Germany has prioritized global health on the international agenda, culminating in the first ever Group of Twenty (G20) Health Ministers Meeting, which took place in Berlin, Germany, on 19 and 20 May.
Political commitment
“Ending AIDS is a historic goal and I firmly believe we can reach it. UNAIDS has to maintain its leadership role in the global AIDS response. We have to increase our joint efforts and UNAIDS is central to that work,” said Mr Gröhe. "Health is a prerequisite for social development. This is one of the reasons why Germany made global health a priority under our G20 presidency. With this decision taken by our Federal Chancellor, Angela Merkel, a global health policy is going to be a hallmark of our country’s international responsibility. Only if we cooperate and work together, we can prepare the world for future health crises,” he added.
During the meeting, Mr Sidibé thanked the government, and particularly the Minister of Health, for their longstanding support to UNAIDS and commitment to the AIDS response. “Putting health on the agenda of the G20 and particularly holding a meeting of the G20 Health Ministers for the very first time is revolutionary,” said Mr Sidibé. “It highlights the shared understanding that quality health care is essential to social and economic stability.” They agreed on the danger of complacency and the potential reversal of gains it could bring.
Mr Sidibé also met with the Parliamentary State Secretary for the Ministry of Economic Cooperation and Development, Thomas Silberhorn, where he highlighted the critical role of UNAIDS in ending the AIDS epidemic and the impact it would have on the broader Sustainable Development Goals.
During his visit he also spoke to Bärbel Kofler, Germany’s Commissioner for Human Rights Policy and Humanitarian Aid. She said, “Access to health is a human right.” They discussed the need for continued engagement to break down discrimination and stop exclusion and prejudice, particularly for people who are vulnerable and are being left behind. Mr Sidibé emphasized that fragile communities not only exist in developing countries, but can be found the world over—from Baltimore to Bamako.
Working together to Fast-Track the AIDS response in Germany
Taking the engagement to the local level, Mr Sidibé next met with representatives of the city of Berlin, which joined the Fast-Track cities initiative in 2016. He also met the nongovernmental organization Deutsche AIDS-Hilfe, which recently launched a campaign to End AIDS in Germany by 2020, and its local branch, Berliner AIDS Hilfe, as well as the advocacy group Action Against AIDS Germany.
During the meeting, Mr Sidibé highlighted that city health systems that are inclusive and accessible have the best chance of engaging people who might otherwise be left behind. “Having a strong civil society has made a big difference in the response to HIV,” he said.
Private sector engagement
In addressing the international business community on the eve of the B20 Health Conference Mr Sidibé said. “Today’s global health challenges, including emerging pandemics and antimicrobial resistance, threaten not just individual lives, but impact social cohesion and economic development. The private sector can bring unique innovation, technologies and services and needs to be an integral part of a multisectoral response to build resilient, responsible and responsive health systems.”
As guest of honour, Mr Sidibé congratulated the winners of the newly launched German Global Health Award—the German Healthcare Partnership (GHP), Bio Deutschland and the Voice of German Industry. The initiative exemplifies how the private sector and civil society alike are needed to drive innovation in the health-care sector.
Roland Göhde, Chairman of the Board at GHP, said, “With the German Global Health Award launched in this year of Germany’s G20 presidency, we would like to underline our strong private sector commitment towards multi- and inter-sectoral partnerships engaged in health system strengthening and universal health coverage. We are partners and committed to making the world a healthier and safer place.”
Region/country
Related
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025


Feature Story
Democratic Republic of the Congo on track with its HIV catch-up plan
22 May 2017
22 May 2017 22 May 2017The Democratic Republic of the Congo’s HIV catch-up plan shows that impressive results in the response to HIV can be made when partners work together.
Launched in December 2016, the western and central Africa catch-up plan aims to ensure that 4.5 million people living with HIV in the region will have access to HIV treatment by 2020. In support of the regional plan, the Democratic Republic of the Congo’s country plan—developed and implemented by the Ministry of Health and the National AIDS Commission—aims to increase the number of people on antiretroviral therapy in the country by 80 000 people, to more than 200 000 people by June 2018.
An intensive HIV testing campaign in the country has enabled 2 million people to know their status—essential to enabling people to access HIV treatment.
Coverage of antiretroviral therapy in the country stood at just 33% of people living with HIV in 2015, higher than the region’s coverage (28%), but much lower than the coverage in eastern and southern Africa (54%). According to government estimates, by April 2017, 34 000 more people were on treatment. The increase puts the country on track to reach the June 2018 target, which would see 73% of people living with HIV on treatment.
The encouraging increase in treatment coverage resulted from a range of partners—the Ministry of Health and the National AIDS Commission, United Nations agencies, the Global Fund to Fight AIDS, Tuberculosis and Malaria and the United States President’s Emergency Plan for AIDS Relief, among others—working together to finance and give technical support to the scale-up. By focusing on the three most affected provinces in the country, resources have been maximized where they are most needed.
Community-based antiretroviral medicine distribution points and community-based early warning systems have helped to reduce drug stock-out and improve the quality of HIV services. These community health services are among the best practices that have been scaled up to increase treatment coverage.
UNAIDS is working with countries to ensure that 30 million people living with HIV have access to treatment through meeting the 90–90–90 targets—whereby 90% of people living with HIV know their HIV status, 90% of people who know their HIV-positive status are accessing treatment and 90% of people on treatment have suppressed viral loads—by 2020.
Quotes
“The Democratic Republic of the Congo’s example shows what can be done. UNAIDS encourages other countries to mirror the catch-up plan and accelerate efforts towards ending AIDS in the western and central Africa region, ensuring that no one is left behind.”














