
Multisectoral resilience to funding cuts in Guatemala


03 October 2016
03 October 2016 03 October 2016New York City was the first city in the world to have its own municipally branded condom, and it currently maintains the largest free condom programme in the United States of America. Even in this high income, cosmopolitan city, free condom distribution is instrumental in preventing HIV, other sexually transmitted infections and unintended pregnancies among key populations. Free condom distribution is included as a cost-saving and cost-effective prevention strategy within the 2015 Blueprint for ending the AIDS epidemic in New York State by 2020.
New HIV diagnoses in New York City, 2001-2014
Source: New York City Health Department
New York City’s free condom programme started in 1971, with free condoms distributed through the city’s clinics for sexually transmitted infections. In 2007, the Health Department launched the NYC Condom. Since then, every National Condom Awareness Day (held on St Valentine’s Day) has included a change in the look of the NYC condom packaging or the addition of a new layer of social marketing to the programme.
The Health Department supplies male condoms, female condoms and lubricant freely to any New York City organization or business that wishes to distribute them. In 2011, the Health Department created the NYC Condom Finder, a mobile phone application that uses GPS to assist users to find condom outlets across the city; this app has been downloaded by tens of thousands of people.
New York City’s Condom Availability Program (NYCAP) has over 3500 condom distribution partners and in 2014 distributed over 37.1 million male condoms and almost 1.2 million female condoms across the five boroughs. These partners focus distribution on neighbourhoods with the highest rates of HIV in the city, and to locations that serve people living with HIV and key populations, such as gay men and other men who have sex with men.
The programme works to increase the awareness, availability and accessibility of condoms to the residents of New York City by maintaining a strong community presence. In 2014, NYCAP participated in over 105 community events, provided 825 presentations in the Health Department’s clinics for sexually transmitted infections, and participated in all official and unofficial Gay Pride events in the city, reaching over 53 500 individuals.
Awareness and access to NYC Condoms is high among key populations. Over 75% of individuals polled at Gay Pride events and an African American Day Parade had seen or heard of NYC Condoms and had obtained them.
At the Health Department’s clinics for sexually transmitted infections, 86% of people surveyed were aware of NYC Condoms and 76% had obtained them. Condom use was also high, ranging from 69% to 81% among people who obtained NYC condoms.
Since the launch of the NYC Condom, more than 300 million NYC Condoms have been distributed. The trend in new diagnoses of heterosexually transmitted HIV infections has been reversed with a reduction of 52% between 2007 and 2014.


03 October 2016
03 October 2016 03 October 2016The UNAIDS Prevention gap report shows that HIV prevention efforts must be reinvigorated if the world is to stay on the Fast-Track to ending the AIDS epidemic by 2030. To achieve the global Fast-Track Target of reducing the number of new HIV infections to fewer than 500 000 by 2020, more political commitment and increased investment in HIV prevention, including condom promotion, are needed.
In 2015, an estimated 1.9 million [1.7 million–2.2 million] adults aged 15 years and over were newly infected with HIV—the vast majority through sexual transmission—and an estimated 500 million people acquired chlamydia, gonorrhoea, syphilis or trichomoniasis. Every year, more than 200 million women have unmet needs for contraception, leading to approximately 80 million unintended pregnancies. Condoms effectively prevent all of these.
Male and female condoms are highly effective and the most widely available prevention tool, even in resource-poor settings, for people at risk of HIV infection, other sexually transmitted infections and unintended pregnancies. Condoms are inexpensive, cost-effective and easy to store and transport, their use does not require assistance of medical or health-care personnel and they can be utilized by anyone who is sexually active. A recent global modelling analysis estimated that condoms have averted up to 45 million new HIV infections since the onset of the HIV epidemic. For many young people worldwide, condoms remain the only realistic option to protect themselves.
The promotion of consistent use of condoms is a critical component of HIV combination prevention. Condom utilization complements all other HIV prevention methods, including a reduction in the number of sexual partners, voluntary medical male circumcision, pre-exposure prophylaxis (PrEP) and treatment as prevention for serodiscordant couples.
Despite increased use of condoms over the past two decades, studies show that reported use of condoms during a person’s most recent sexual encounter with a non-regular partner ranged from 80% in some countries to less than 30% in others. There is an urgent need for countries to strengthen demand for and supply of condoms and water-based lubricant. Countries agreed in the 2016 Political Declaration on Ending AIDS to increase the annual availability of condoms in low- and middle-income countries to 20 billion by 2020.
Many countries have not yet set ambitious condom distribution and use targets and condoms are suboptimally programmed, with gaps in demand creation and supply. Few condom programmes adequately address the barriers that hinder access and the use of condoms by young people, in particular adolescent girls and young women, gay men and other men who have sex with men and sex workers. In many countries, condoms are not easily available to young people in schools or anywhere outside health facilities. In some contexts, sex workers have unprotected sex with their clients, as carrying condoms is criminalized and used as evidence by the police to harass or prove involvement in sex work. Some programmes only provide a handful of condoms to each sex worker at each visit, but sex workers may have many more clients than condoms supplied. There is also insufficient access to lubricants—less than 25% of men who have sex with men in 165 countries have easy access to free lubricant, and many sex workers, too, desire but lack access to lubricants. Most countries do not plan for the provision of lubricants in their national strategic plans and condom programmes.
International funding for condom procurement in sub-Saharan Africa has stagnated in recent years, and domestic funding has not sufficiently increased. Funding for condom distribution and promotion has even declined. In 2015, there was an estimated gap of more than 3 billion condoms in sub-Saharan Africa against a total need of 6 billion.
To be successful, comprehensive condom programming must address components such as leadership and coordination, supply and commodity security, demand, access and promotion of utilization, and technical and logistic support. It is critical for governments to create an enabling environment among policy-makers and service providers so that users will be made aware of their risks, feel free to demand and access male and female condoms and have the knowledge to use them correctly and consistently. Young people and key populations are strong allies in the promotion of access to condoms. At the last International AIDS Conference in Durban, South Africa, for example, South African youth demonstrated for access to condoms and other sexual and reproductive health services and commodities such as sanitary pads.
Effective condom promotion should be tailored for people at increased risk of HIV and other sexually transmitted infections and/or unintended pregnancy, including young people, sex workers and their clients, injecting drug users and gay men and other men who have sex with men. Many young women and girls, especially those in long-term relationships and sex workers, do not have the power to negotiate the use of condoms, as men are often resistant to their use. Condoms should also be made available in prisons and other closed settings and in humanitarian crisis situations.
There also needs to be a greater leverage of social networks, social media and new technologies to promote condom use and improved focusing. The UNFPA’s CONDOMIZE! campaign to destigmatize and promote condom use is being rolled out in nine countries, led by national governments, with two more national rollouts planned for 2016. The campaign actively involves young people as ambassadors, bloggers and peer educators. In the United States of America, condoms are increasingly promoted and freely distributed in schools in order to address health matters such as unintended teenage pregnancies, sexually transmitted infections and HIV. Cities such as New York and Washington, DC, have established targeted free condom distribution to reach key populations and people at higher risk. In France, condom distribution machines have been placed in schools and the South African Department of Education is in the process of revising its policies in order to allow condom promotion and distribution in schools.
In Zimbabwe, the government has supported large-scale condom distribution through social marketing and free distribution channels. In 2014, 104 million male condoms were distributed in Zimbabwe, one of the highest numbers in the world. Increases in condom use are credited as being one of the reasons that new HIV infections were halved for adults from 2009 to 2015. The South African government has funded a nationwide female condom distribution programme with over 300 distribution sites. In Brazil, public health officials have developed one of the largest condom distribution and promotion campaigns in the world. Despite some objections, the Brazilian government has remained steadfast in its commitment to sharing medically accurate information regarding the benefits of condom use.
Putting condoms on the Fast-Track and achieving 90% condom use by people at risk who are having sex with a non-regular partner would avert an additional 3.4 million new HIV infections by 2020 and would also have a significant impact on preventing other sexually transmitted infections and unintended pregnancies.




23 September 2016
23 September 2016 23 September 2016Côte d’Ivoire’s engagement in the future of global health, and in particular in ending the AIDS epidemic, is a strong demonstration of the progressive leadership of the country.
Côte d’Ivoire has been working closely with UNAIDS for many years to scale up its domestic response to HIV, stop new HIV infections and ensure access to treatment. Now, Côte d’Ivoire is expanding its reach and efforts to improve the lives of people living with and affected by HIV, not just in its own country but across the globe.
Côte d’Ivoire has recently announced a US$ 1 million donation to UNAIDS to support UNAIDS’ efforts to Fast-Track the response to HIV and end the AIDS epidemic as a public health threat by 2030. The announcement was made at the Fifth Replenishment Conference of the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund), where Côte d'Ivoire was among nine African countries that made pledges to the Global Fund, a greater number than ever before and an encouraging sign that countries across Africa are becoming more engaged in improving global health outcomes.
The President and First lady of Côte d'Ivoire, were in New York, United States of America this week for the 71 United Nations General Assembly. The First Lady, Dominique Ouattara, met with the Executive Director of UNAIDS, Michel Sidibé, to discuss future projects and ways of advancing her personal efforts in stopping new HIV infections among children.
Putting children and families first has been a long-term commitment of Ms Ouattara. Through her multiple platforms, she has championed the rights of children for access to health and education for a number of years. In 2014, UNAIDS appointed Ms Ouattara as a Special Ambassador for the Elimination of Mother-to-Child Transmission and the Promotion of Paediatric Treatment for HIV. The next phase of UNAIDS’ work with Ms Ouattara will be on further integration of HIV and health programmes, particularly those concerning young people.








12 September 2016
12 September 2016 12 September 2016The village of Jiele is where China’s first HIV cases were reported in 1989. Located in Dehong prefecture in Yunnan province, the village experienced an AIDS epidemic that resulted in almost 200 deaths. However, a quarter of a century later, the village is now brimming with hope and renewed energy.
“In the past, everyone was so scared of HIV, but now we are getting great health services and we are living normal healthy lives. We are not afraid of HIV anymore,” said a resident of Jiele.
The more than 100 people currently living with HIV in the village are receiving regular check-ups and almost all are on HIV treatment. The village’s success is echoed across Dehong prefecture, which was at the heart of China’s early AIDS epidemic.
Located near the opium producing areas of the Golden Triangle and the major drug trafficking routes, Dehong’s initial HIV cases were among people who inject drugs, as well as sex workers and their clients. In the past 15 years the prefecture has worked with community organizations, the central government and international organizations and has implemented a wide range of innovative measures, leading to a remarkable turnaround in the AIDS epidemic.
During a week-long mission to China, UNAIDS Executive Director Michel Sidibé witnessed the achievements made in Dehong. He met with officials and community groups and visited a range of sites, including Ruili Hospital on 7 September. He saw how the city hospital provides one-stop-shop HIV prevention and treatment services, including health education, HIV testing, methadone for people who inject drugs and prevention of mother-to-child transmission of HIV services.
In 2009, Dehong started to decentralize antiretroviral therapy management down to the community level for people living with HIV who had been accessing treatment for more than a year. Ruili Hospital provides assistance and technical support to the community-level antiretroviral therapy sites, which in 2014 were providing treatment to more than 600 people living with HIV.
“Ruili Hospital is a model of how one-stop-shop HIV services save lives and money,” said Mr Sidibé. “It’s remarkable how the hospital is spreading its know-how down to the community level and ensuring that quality health care is available in even the most remote corners of China.”
“The fourth round of the People’s War against AIDS has just been launched in Yunnan,” said Gao Feng, Vice-Governor of Yunnan. “We are confident we will achieve the 90–90–90 targets by 2020 in Yunnan.”
Dehong’s HIV response has evolved to meet the new challenge of providing quality health care to cross-border migrants. While in most parts of China access to key HIV services, such as treatment and methadone, require a Chinese identification card, in Dehong, HIV treatment is available to non-Chinese people who can present residence and employment permits and health certificates.
Mr Sidibé visited Jiegao, which is a district of Ruili where around 50 000 Burmese people are estimated to live. The Needle Exchange and Methadone Maintenance Treatment Extension (MMT) sites provide services to mainly migrants who inject drugs. Truck drivers crossing the China and Myanmar borders are provided with comprehensive services at a government-funded truck driver action spot. The services include health education, HIV counselling and testing, condom distribution, and referral to HIV treatment.
The local government in Dehong has a strong partnership with community-based organizations, which have played a key role in reaching migrants and people who use drugs, engage in sex work or are living with HIV.
Owing to these effective strategies, Dehong is the only prefecture in Yunnan province to receive public recognition for having reversed its AIDS epidemic. Health authorities report that HIV treatment coverage is around 60% of all people living with HIV, while prevention of mother-to-child transmission of HIV programme coverage is 100%. In Ruili, among people living with HIV eligible for antiretroviral therapy, the mortality rate has decreased by 95% compared to 2005. There were zero new HIV infections reported among people who use drugs attending MMT clinics from 2008 to 2014 and no babies born to pregnant women living with HIV have been reported to be HIV-positive since 2008. Dehong’s success is all the more remarkable as neighbouring prefectures in Yunnan province continue to experience expanding epidemics.
“Political leadership and engagement with communities and programmes based on scientific evidence can inspire other communities in China to end the AIDS epidemic,” said Mr Sidibé.

07 September 2016
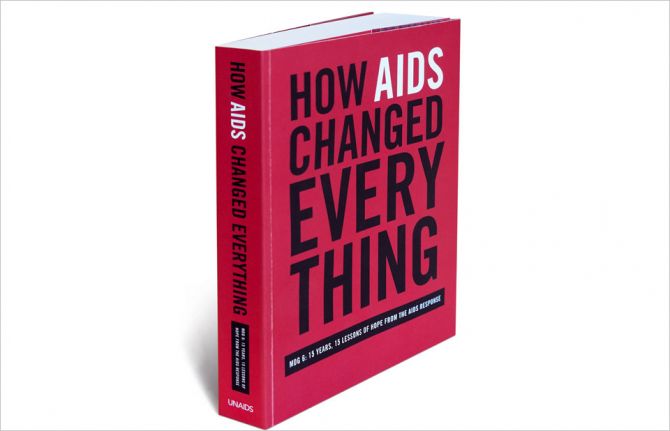
07 September 2016 07 September 2016For the second year in a row and for a third time, UNAIDS has been awarded prizes in the British Medical Association (BMA) Book Awards for its book How AIDS changed everything, which was runner up in the BMA President’s Choice Award and was Highly Commended in the Public Health category. A personal award from the BMA’s past President, Sir Al Aynsley Green, the President’s Choice Award is for the two books in the past year that most impressed him.
How AIDS changed everything—MDG 6: 15 years, 15 lessons of hope from the AIDS response is about how the world achieved and exceeded the AIDS targets of the Millennium Development Goals (MDGs) in 2015.
The book covers the 15 years of the MDGs and was launched in July 2015 as the world reached 15 million people on HIV treatment, a major milestone met ahead of schedule.
“The world has delivered on halting and reversing the AIDS epidemic,” said Ban Ki-moon, Secretary-General of the United Nations, at the launch. “Now we must commit to ending the AIDS epidemic as part of the Sustainable Development Goals.”
The BMA judges noted that, “This is an excellent book, written and presented to a high standard. It contains a comprehensive history of AIDS, its prevention and the suggested plans for the future.”
Michel Sidibé, UNAIDS Executive Director, said, “This award recognizes the achievements the AIDS response made under the Millennium Development Goals and the men and women who worked to help bring those achievements about.”
UNAIDS Director of Communications and Global Advocacy Annemarie Hou, accepting the award on behalf of UNAIDS, said, “The AIDS response brought the world together and this award is for all the people who are making a difference to end this epidemic.”
Major milestones met
Released in Addis Ababa, Ethiopia, on the sidelines of the Third International Conference on Financing for Development, the report demonstrates that the response to HIV has been one of the smartest investments in global health and development, generating measurable results for people and economies. It also shows that the world is on track to meet the investment target of US$ 22 billion for the AIDS response by 2015 and that concerted action over the next five years can end the AIDS epidemic by 2030.
How AIDS changed everything—MDG 6: 15 years, 15 lessons of hope from the AIDS response celebrates the milestone achievement of 15 million people on antiretroviral treatment—an accomplishment deemed impossible when the MDGs were set in 2000. It also looks at the incredible impact the AIDS response has had on people’s lives and livelihoods, on families, communities and economies, as well as the remarkable influence the AIDS response had on many of the other MDGs. The report includes specific lessons to take forward into the Sustainable Development Goals, as well as the urgent need to increase and front-load investments and streamline programmes.
Achieving MDG 6: halting and reversing the spread of HIV
In 2000, the world witnessed an extraordinary number of new HIV infections. Every day, 8500 people were becoming newly infected with the virus and 4300 people were dying of AIDS-related illnesses. How AIDS changed everything describes how, against all odds, huge rises in new HIV infections and AIDS-related deaths were halted and reversed.
Countries invested heavily in monitoring and evaluating their responses to HIV. In 2014, 92% of United Nations Member States reported HIV data to UNAIDS. State-of-the-art epidemic monitoring, data collection and reporting have made HIV data the most robust in the world, far more complete than data for any other disease. This has not only enabled the world to have a clear picture of HIV trends, it has also enabled HIV programming to be tailored to the specific dynamics of each country’s epidemic.
How AIDS changed everything—MDG 6: 15 years, 15 lessons of hope from the AIDS response is both a look back on the journey of the 15 years and a look forward to the future of the AIDS response and the path to ending the AIDS epidemic by 2030.
The flagship publication from UNAIDS was released at a community event at Zewditu Hospital in Addis Ababa on 14 July 2015 by United Nations Secretary-General Ban Ki-moon, the Ethiopian Minister of Health, Kesetebirhan Admassu, the Executive Director of UNAIDS, Michel Sidibé, and Abiyot Godana, Case Manager at the Entoto Health Center.
The prestigious awards were announced at a ceremony on 7 September 2016 at BMA House in London, United Kingdom. An annual event, the awards aim to encourage and reward excellence in medical publishing, with prizes given out in categories and an overall BMA Medical Book of the Year Award and a President’s Choice Award made from the shortlisted books.



05 September 2016
05 September 2016 05 September 2016The First Lady of China, Peng Liyuan, and her counterparts from other Group of 20 (G20) countries have taken part in an event at Zhejiang University in Hangzhou to raise awareness of HIV among students. The Red Ribbon Health Ambassador’s Campus Tour campaign event took place on the sidelines of the 2016 G20 summit, where leaders of the world’s foremost economies have gathered for their annual meeting.
The first ladies, China’s Minister of the National Health and Family Planning Commission, Li Bin, and UNAIDS Executive Director Michel Sidibé also participated in the event. They met students and made a symbolic gesture of placing red ribbons on a banner.
“This meeting is another expression of China’s strong commitment towards ending AIDS by 2030,” said Ms Li.
Mr Sidibé expressed his appreciation for China’s efforts following the event. “We will not end the AIDS epidemic unless we stop new HIV infections among young people. China’s HIV campaign in universities is a great start,” he said.
The Red Ribbon Health Ambassador’s Campus Tour campaign was launched in November 2014 to improve knowledge of HIV prevention and to promote a healthy lifestyle among students. Nearly 20 colleges and universities and 10 medical schools have participated in the campaign, reaching around 400 000 students.
Young people are at higher risk of HIV. In 2015, globally there were 3.9 million young people aged 15 to 24 living with HIV and there were 670 000 new HIV infections among this age group. To reach the global commitment of ending AIDS by 2030, countries have pledged to ensure that, by 2020, 90% of young people have the skills, knowledge and capacity to protect themselves from HIV and have access to sexual and reproductive health services.
Mr Sidibé is on a week-long mission to China and participated in the G20 summit, which focused on promoting stable economic growth. He also met with international business leaders at the B20 summit, which looked at how the business community could contribute to sustainable and balanced growth in the global economy.
While in China, Mr Sidibé also discussed the financing challenges for the global HIV response with Roberto Azevêdo, Director-General of the World Trade Organization, Jim Yong Kim, President of the World Bank Group, and Christine Lagarde, Managing Director of the International Monetary Fund.






20 July 2016
20 July 2016 20 July 2016Red paper ribbons with inscriptions hang like leaves from a baobab-like papier mâché tree. Standing by her creation in the middle of the Global Village at the 21st International AIDS Conference, being held in Durban, South Africa, Michelle Vogelzang is beaming. Her AIDS SolidariTree has travelled far.
Made of the dense foam used to make surfboards, children in Lesotho covered the 11-part sculpture with paper, giving it a bark-like exterior. School students painted the tree in Pretoria, South Africa, writing words related to solidarity in the 11 official languages of both countries.
Unity, stop discrimination and ubuntu wind their way around the branches in multicoloured lettering.
“SolidariTree is a visual declaration designed by youth as a way for them to communicate on how to end HIV stigma and for everyone else to add their voice,” said Ms Vogelzang.
Originally from Durban, she now works in Lesotho. She said the idea of the interactive ribbon sculpture came to her because, in her opinion, HIV is not the killer, discrimination is.
“There is no way we should not be ending this epidemic because we have treatment and health-care facilities, but if you have stigma you are not going to get people tested, treated or even sharing their status,” she said as passers-by stared at the multiple ribbon leaves.
On opening day, the SolidariTree had 500 “leaves”—red ribbon messages from children who could not attend the conference.
Albertina Nyatsi took one of the red paper strips lying on a table. Without hesitating, she wrote something down quickly. The Durbanite stapled the strip, creating a ribbon, and pinned it on the sculpture.
“I was one of the first women in Swaziland to show what HIV looked like, so I wanted to make sure that I got my message across that we should not discriminate,” she said. “I am here because in 1997 I had tuberculosis and then I was tested for HIV and was found to be HIV-positive.”
The tree has grown and now has more than 4000 ribbons hanging from it. The project, entirely crowdfunded, cost around US$ 4000.
“Contributions came mostly from the United States of America and Canada,” Ms Vogelzang explained. In a way, all those people who supported the art exhibition are in South Africa with the tree,” she added. A true sign of solidarity.
Ms Vogelzang is hoping her tree will grow roots beyond the conference and will live on to inspire children, teenagers and adults alike.







17 November 2016
17 November 2016 17 November 2016Mandie Pakkies is shivering outside in her thin black coat on a chilly Durban winter’s night at a truck stop in the suburb of Marianhill on one of the main trucking routes out of Africa’s busiest port. The steady stream of trucks passing by on the highway do not disturb her. She’s actually eager for some of them to pull in for diesel and even a chat. Her job is to encourage truck drivers to take care of their health, and when they park up for the night she invites them into a clinic constructed out of shipping containers at the far end of the truck stop.
“These drivers have such pressing health needs! It’s encouraging to see them come to have their blood pressure taken or want to know their HIV status,” Ms Pakkies said. “I am even teaching them the basics like “drink water”, or “walk 20 minutes to get exercise before you go to sleep in the parking lot.””
The clinic opens in the evenings to coincide with the overnight stop that many truckers make before loading up at the port first thing in the morning. Ms Pakkies, the peer educator, and Thuthuka Xulu, a professional nurse, work side by side welcoming truck drivers and the sex workers from the surrounding streets, who come into the parking lot with the drivers. “We not only provide basic health services, but we test for HIV, tuberculosis and sexually transmitted infections, and of course we distribute a lot of condoms,” said Mr Xulu.
With 2000 trucks passing weekly at the Marianhill site and about 500 trucks parking overnight, the team has plenty to do. Truck drivers come from all over South Africa and neighbouring countries. Owing to their erratic schedules and mobility, truckers face many challenges in accessing basic health services. To respond to these needs and those of the sex workers who work around the truck stop, Truckers Wellness established a network of clinics along the major trucking routes around South Africa.
The Marianhill Trucking Wellness Centre is one of 22 such clinics in the country within a larger network of trucker outreach projects across the region. This programme, launched in 1999, is funded by the freight industry and truck owners and linked to Department of Health services. In the last five years they have tested more than 10 000 people for HIV, averaging around 30 tests per week.
“We are seeing more people get tested and seek our services,” added Mr Xulu, seated behind a cramped desk covered with folders, a box of surgical gloves and HIV testing kits.
The next step for his centre is to be able to adopt the World Health Organization’s guidelines, so that patients can start antiretroviral therapy immediately if they test positive. Grinning he said, “That will really enlarge the scope of our centre.”

20 July 2016
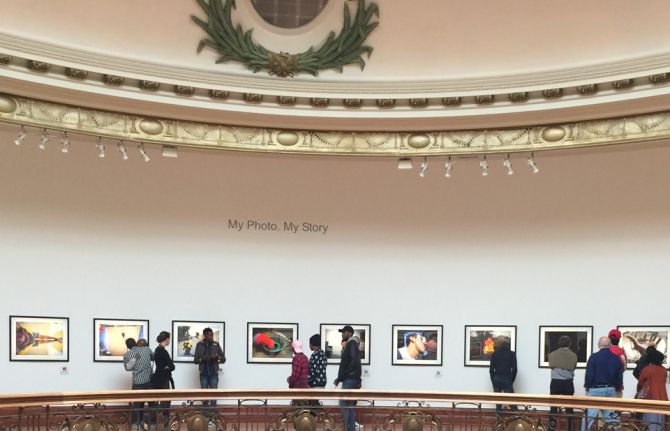
20 July 2016 20 July 2016Photographs line the walls of the rotunda in Durban’s City Hall. The light streams in from the windows of the cupola and recorded voices of the “artivists,” as they are known, speak to all who enter. The exhibition is called Through Positive Eyes: 10 Years. 9 Cities. My Photo. My Story.
Storytelling is revealed in several forms as visitors immerse themselves in the exhibition. Over the course of 10 years, co-directors of the Through Positive Eyes project David Gere and Gideon Mendel have brought together from around the world people living with HIV.
In each of the nine cities, the process began the same way—a group of people, strangers to each other, were given a camera. What started as a foreign object quickly became an extension of themselves.
Mr Mendel, an award-winning photographer, leads photo education workshops alongside his associate, Crispin Hughes. Mr Gere, a professor at the University of California, Los Angeles, conducts the story interviews.
“It was therapeutic to hear other people’s stories,” said artivist Simiso Msoni of Durban. “Overall, it was just fun to tell your story and what it means to live with HIV through pictures.”
The Durban exhibition brings many of the past participants together, as well as their art. An innovative feature is the live dialogue sessions, in which two of the participants speak to each other about their experiences and visitors can listen as their stories unfold.
Edwin Cameron, a Judge of the Constitutional Court of South Africa, called the exhibition extraordinary. “This exhibition is important for what it does for visibility, for what it does for voices,” he said. He underlined the need to listen and learn from people living with and affected by HIV and the need to break down barriers caused by stigma and discrimination.
The exhibition includes works by Adriana Bertini, Mandisa Dlamini, Daniel Goldstein, Ross Levinson, Gordon Mundie and Parthiv Shah and is co-curated by Stan Pressner, Carol Brown and Mr Gere.