Feature Story
Protecting men and boys’ health in Swaziland
21 October 2016
21 October 2016 21 October 2016The Centre for HIV/AIDS Prevention Services (CHAPS) leads a consortium that supports the Swaziland Ministry of Health to implement the national strategic voluntary medical male circumcision plan, which is part of the country’s efforts to keep men and boys free from HIV.
The centre’s work demonstrates how voluntary medical male circumcision programmes can be an important entry point to expanded health programming for men and boys, helping to ensure they are reached with a broad spectrum of vital health messages.
Swaziland has been particularly affected by the AIDS epidemic. In 2015, more than a quarter of 15-49-year-olds were living with HIV. As part of efforts to reduce new HIV infections, Swaziland has developed a plan that it hopes will help to keep young men and boys free from HIV.
Swaziland estimates that its Male Circumcision Strategic and Operational Plan for HIV Prevention 2014–2018 will avert 31 000 new HIV infections by 2028, which will result in cost savings of approximately US$ 370 million by 2035.
Studies have shown medical male circumcision to be around 60% effective in preventing female-to-male sexual transmission of HIV. Swaziland is taking a new and innovative approach to engaging men and boys in HIV prevention efforts and encouraging them to take up the offer of voluntary medical male circumcision to help protect them from becoming infected with HIV.
Lihawu three-day camps
In April 2016, CHAPS and Kwakha Indvodza, a male mentoring project in Swaziland, piloted a new initiative to encourage young men and adolescent boys to become respectful and responsible adults. The initiative, Lihawu (“shield”), is a three-day camp where 25 to 30 adolescent boys and young men aged 15–29 years are guided, mentored and encouraged to hold open and honest discussions about sexuality, sex and sexual health, relationships, gender equality and respect.
The camps are rooted in a Bantu rite of passage tradition and promote the Swazi cultural heritage of ubuntu. They use the traditional Swazi lisango, men’s meeting spaces, where they take part in challenges, games and goal-setting, as well as talking openly about the values of traditional and modern practices.
The camps also provide the opportunity for the men and boys to talk about HIV and participants are offered voluntary HIV counselling and testing. Voluntary medical male circumcision is also offered to participants should they wish to undergo the procedure to help protect them against HIV infection.
To date, more than 350 adolescent boys and young men have participated in Lihawu camps, with many taking up the opportunity to have an HIV test. People testing positive for HIV are directly linked to treatment and care programmes as part of the camp’s services. The Lihawu camps have also seen an uptake in voluntary medical male circumcision, with almost half of all participants opting for the procedure.
Saving lives through soccer
CHAPS also run a successful soccer programme to disseminate information about HIV prevention in the hope of increasing uptake of voluntary medical male circumcision in Swaziland. Through support from the United States President’s Emergency Plan for AIDS Relief, uptake among 15–29-year-olds increased from 2770 in 2015 to 4490 in 2016.
The centre has also appointed a local hero, international soccer player Dennis Yuki Masina, as an ambassador for voluntary medical male circumcision.
Empowering health advisers
CHAPS has also conceptualized and rolled out a unique training programme for health outreach workers. The programme uses best practices and tools from a number of sectors to empower outreach workers as a trusted source of health-care information in the community, particularly on HIV prevention, treatment, care and support and tuberculosis. The health advisers are equipped with a number of approaches to engage people, especially older men, and link them to essential health services, including voluntary medical male circumcision for HIV prevention.
Hands up for #HIVprevention — World AIDS Day campaign
Region/country

Feature Story
Tireless Indian doctor dedicated to women’s health
28 October 2016
28 October 2016 28 October 2016Gita and her husband arrived at the Sir Jamsetjee Jeejebhoy (Sir J.J.) Hospital more than 15 years ago desperately wanting to have children. Because they were living with HIV, doctors had discouraged them from becoming parents, so they travelled five hours to bustling Mumbai, India, to see Rekha Daver, with the hope of finding a solution. Any solution.
Ms Daver is a doctor who heads the gynaecology department at the state-run hospital. Under her leadership, the hospital has become a referral centre for HIV-positive pregnant women, who are often turned away from other health facilities.
“Back then I could not guarantee that their child would not be HIV-positive, but I enrolled Gita on our antiretroviral therapy programme,” Ms Daver recalled. Subsequently, Gita’s husband was enrolled on the programme. Within a year Gita gave birth to a baby girl at the hospital.
“They never missed an appointment and when their daughter was born HIV-negative you should have seen their happiness,” she said. The couple, with their teenager in tow, still visit Ms Daver, which delights her. “It is not just a question of preventing mother-to-child transmission of HIV, it’s also having two adults living healthy lives.”
Ms Daver knows all about giving life. Since 2000 her team has performed more than 1 000 deliveries of HIV positive women. As of late there is cause to celebrate because in the last two years 100 women on the new three-drug regimen have had children born HIV-free.
Sarita Jadav, the New Delhi United Nations Educational, Scientific and Cultural Organization Focal Point for HIV and School Health Education, praised Ms Daver. “Maternal and child health is one of her passions and she has dedicated more than 37 years to servicing underprivileged women,” she said. Ms Jadav stressed the fact that despite having studied and worked in the United States of America and obtained a green card, Ms Daver chose to return to India and work in state hospitals and to train thousands of medical students.
“Her tireless efforts to bring about change and to save lives have been admired by all,” Ms Jadav added.
Ms Daver talked about the importance of counselling. “When I see women who are HIV-positive and their husbands HIV-negative there are often societal pressures on the couple, not so when the man is HIV-positive and the woman is negative,” she said. “My team and I have been trying to raise awareness about safe sex practices and family planning.” She credits her work at the Human Reproduction Research Centre and at the Indian Council of Medical Research in broadening her scope regarding women’s health.
Supporting women has driven Ms Daver’s career. She always knew she wanted to be a doctor and had set her sights on being a surgeon, but growing up in a small town she realized that helping women was key and that she could make a bigger impact as an obstetrician/gynaecologist.
After attending medical college in India, she spent three years at the Texas Medical Center in Houston, United States. When she decided to move back to India her husband Dr Gustad (medical school sweetheart) and two children moved back with her.
In 1990, she started at the Sir J.J. Hospital and it was then that she started to see more and more women living with HIV.
“I realized there was no cure and that perhaps my best bet was to focus on prevention, especially from mother-to-child.”
After studying programmes in Thailand and Uganda, Ms Daver’s team started providing access to antiretroviral medicine to mothers living with HIV during their pregnancy. Without antiretroviral medicine, between 33% and 45% of infants born to women living with HIV will become infected with HIV. The Sir J.J. Hospital project became a pilot programme and Ms Daver trained other doctors from across India.
With the success of programmes to prevent mother-to-child transmission of HIV, Ms Daver can once again promote breastfeeding. “Before I worried so much because I was saving the child but mortality rates remained high because of a lack of antibodies,” she said. “Now women can safely breastfeed, which makes me so happy,” she said.
Her enthusiasm for her work is infectious, explains her daughter. “I always saw my mother’s devotion to people living with HIV, as well as her passion regarding women’s issues,” said the New York based Roshni Daver. “In fact she inspired me to become a doctor.”
“The key to my mother’s long and successful career is her excellent time management, or perhaps it’s because she wakes up very early,” said her daughter.
Her mother sees it another way, saying, “It gives me a great sense of satisfaction to help all these underprivileged women as well as to train the future generation of doctors.”
Hands up for #HIVprevention — World AIDS Day campaign
Region/country

Feature Story
Lives changed on the way to zero
26 October 2016
26 October 2016 26 October 2016It never crossed Khonjiswa Mdyeshana’s mind that she could be HIV-positive. So, in 2006, when she tested positive for HIV while pregnant with her first child, she couldn’t believe it. She insisted on taking the test three times. Much to her shock, every result came back positive. “In my mind, it was the end of the world for me and my child,” she says.
What Ms Mdyeshana didn’t know was that working alongside the doctors and nurses at her health clinic were HIV-positive Mentor Mothers, employed and trained by Africa-based nongovernmental organization mothers2mothers (m2m). The Mentor Mothers provided women just like her with education and support to initiate and adhere to their HIV treatment.
“The women at m2m made me feel welcome and unafraid. They told me their own stories of living with HIV. They taught me how to prevent spreading the virus to my baby and live positively. I have to be honest, I was not 100% sure about everything, but somehow I had new hope that it was not the end,” Ms Mdyeshana says.
Since m2m was founded in 2001, it has become a global leader in efforts to bring paediatric HIV infections to zero and improve the health and well-being of mothers, families and communities.
The m2m Mentor Mother model has been proven to reduce the number of infants who become infected with HIV and improve the health outcomes of mothers and babies, while also saving money in averted HIV treatment costs. A recently released annual evaluation of m2m’s programmes found that, in 2015, m2m achieved significant results:
- m2m virtually eliminated mother-to-child transmission of HIV among its clients for the second year in a row, with a mother-to-child transmission of HIV rate of 2.1% after 24 months.
- In South Africa, m2m’s transmission rate was even lower—1.1% after 18 months.
- Mothers who met two or more times with a Mentor Mother were more than seven times more likely to have their babies tested for HIV at six weeks compared to mothers who had met a mentor just once.
“It’s a joy to go into a site and hear a nurse or the head of the clinic say, “You need to know that it’s been three years since we have had a baby born in this clinic with HIV because of mothers2mothers,”” says m2m President and Chief Executive Officer, Frank Beadle de Palomo.
However, children are still becoming infected during the breastfeeding period. And there is a rising number of infections and deaths among adolescents, particularly adolescent girls and young women.
Responding to this need, m2m now engages mothers and their families over a longer period of time with a family-centred approach. m2m looks beyond survival, focusing on giving children the opportunity to thrive through its early childhood development and paediatric case finding and support programmes. And the new DREAMS initiative in South Africa is providing adolescents with the skills and knowledge necessary to protect themselves and the next generation from HIV.
As for Ms Mdyeshana, she has come a long way since 2006. She now works as a Mentor Mother, helping other women realize that living with HIV is not the end of their world. She is a proud mother to two HIV-free children, who are full of life, happiness and big dreams.
Her oldest, Luthando, now nine years old, tells his mother he is studying hard so that when he grows up he can get a good job and buy them a bigger house. That job? He says he is going to become a doctor, because he sees “a lot of sick people around” and wants to help them. While he works towards that dream, he is practising his medical skills at home, reminding his mother, who he describes as “strong and beautiful,” to take her HIV medicine every day.
Hands up for #HIVprevention — World AIDS Day campaign
Related

Feature Story
France opens its first safe injecting site for drug users
13 October 2016
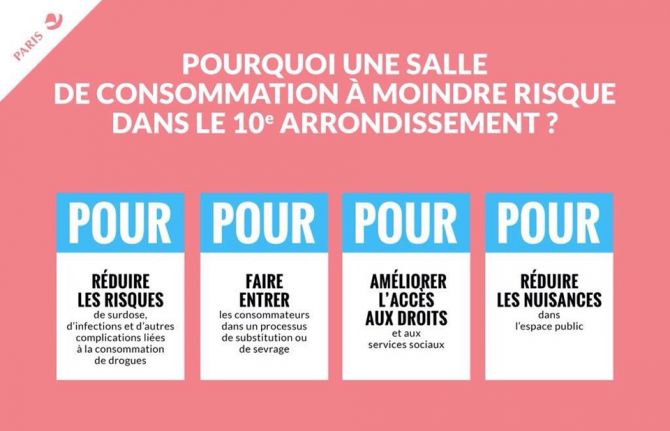
13 October 2016 13 October 2016France’s first safe injecting site for people who inject drugs has opened in Paris.
Linked to the city’s Lariboisière Hospital, the facility can accommodate up to 400 people a day and is staffed by a full team of doctors, nurses and social workers. It is made up of three areas: a waiting room, a consumption room and a place where people can rest before leaving the site.
The aim of the facility, which is open to adults aged 18 and over, is to lessen the risks associated with injecting drug use, including HIV infection. Research shows that supervised injection sites also reduce crime and other social disorders linked to the public consumption of drugs.
The UNAIDS Executive Director, Michel Sidibé, congratulated France’s Minister of Health, Marisol Touraine, and the Mayor of Paris, Anne Hidalgo, on the opening of the site.
Additional drug consumption rooms are planned to open in other French cities, including Strasbourg and Bordeaux, in the near future.
Paris is a founder signatory of the Paris Declaration, which commits cities to ending the AIDS epidemic by 2030 by adopting a Fast-Track approach to their HIV epidemics.
Region/country
Related


Feature Story
Voluntary medical male circumcision: a core campaign to reach the Fast-Track Targets
17 October 2016
17 October 2016 17 October 2016AIDS-related illnesses remain the single largest cause of years of life lost among adolescent boys and men of reproductive age in eastern and southern Africa, although few policies and programmes focus on HIV services for men and boys or on improving their access to health care. However, one type of programme, voluntary medical male circumcision (VMMC), stands out, as it has had reached men and boys in large numbers and is 60% effective in preventing against female-to-male transmission of HIV.
In 2007, the powerful evidence of the preventive impact of VMMC led the World Health Organization (WHO) and UNAIDS to recommend VMMC, particularly in high-burden countries with a low prevalence of male circumcision. They urged the scale-up of voluntary medical male circumcision in 14 countries—Botswana, Ethiopia, Kenya, Lesotho, Malawi, Mozambique, Namibia, Rwanda, South Africa, Swaziland, the United Republic of Tanzania, Uganda, Zambia and Zimbabwe—guided by the actions of ministries of health and other stakeholders.
The highly aspirational target set was to provide VMMC services to more than 20 million men by the end of 2016 in the priority countries. By the end of 2015, 11.7 million adolescent boys and men had been circumcised, and by the end of 2016 that number is projected to reach 14 million, a huge success by any measure. Some countries are attaining and surpassing targets. In 2015, the Gambella province in Ethiopia, Kenya and the United Republic of Tanzania all exceeded their targets set in 2011.
Today, governments and partners, such as UNAIDS, WHO and the United States President’s Emergency Plan for AIDS Relief, are focused on continuing to scale up and maintain this successful programme, but there is cause for concern. Following years of rapid increase, the annual number of circumcisions performed within eight of the 14 priority countries stayed level or decreased in 2015.
There is guidance, however, for a way forward. A new WHO and UNAIDS report, Effective HIV prevention and a gateway to improved adolescent boys’ & men’s health in eastern and southern Africa by 2021, describes the new strategic directions for the years to come. In order to reach the Fast-Track Targets, the annual number of VMMCs needs to increase to 5 million per year. At the same time, a comprehensive people-centred approach to service delivery for men and boys needs to be adopted at the country level, with tailored services to be offered to individuals in different age groups and with different risk profiles.
The report lists the following as the key elements that all stakeholders are encouraged to work together to achieve:
- Promoting VMMC as part of a wider package of sexual and reproductive services for men and boys, including comprehensive sexuality education, the use of condoms and communication around gender norms, including positive notions of masculinity.
- Using new integrated service delivery models.
- Using approaches that are tailored for various age groups and locations.
- Increasing domestic funding to ensure the sustainability of VMMV and expanding sexual and reproductive health services for men and boys.
- Developing new approaches for adolescent and early infant circumcision.
- Breaking down myths and misconceptions about circumcision.
The Clearinghouse on Male Circumcision for HIV Prevention is a collaborative effort among partners, including UNAIDS, for sharing information and resources with the international public health community. The resource library has more than 900 entries and can be searched by topic or country.
“Voluntary medical male circumcision provides a much needed entry point for reaching men and boys with other HIV prevention and health services, which would in turn benefit women and girls,” said UNAIDS Executive Director, Michel Sidibé. “We cannot reach our goals without it,” he added.
Related videos
Related


Feature Story
Ending AIDS by 2030 requires investment in harm reduction for people who inject drugs
10 October 2016
10 October 2016 10 October 2016To end the AIDS epidemic by 2030, the global response to HIV must leave no one behind, including people who inject drugs. It requires drug policies and HIV-related prevention, treatment, care and support services that meet both the human rights and the health needs of people who inject drugs.
Estimates show that worldwide there are approximately 12 million people who inject drugs, 1.6 million (14%) of whom are living with HIV and 6 million (50%) of whom are living with hepatitis C. HIV prevalence among women who inject drugs is often greater than among their male peers. UNAIDS estimates that 140 000 people who inject drugs were newly infected with HIV globally in 2014 and there has been no decline in the annual number of new HIV infections among people who inject drugs between 2010 and 2014.
The UNAIDS report Do no harm: health, human rights and people who use drugs shows that having laws and policies that do no harm to people who use drugs and increasing investments in harm reduction programmes and services results in a decrease in new HIV infections and improved health outcomes and delivers broader social benefits.
The United Nations Office on Drugs and Crime, the World Health Organization (WHO) and UNAIDS recommend using these programmes and services as a comprehensive package, as outlined in the WHO’s consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations.
Harm reduction works
The evidence is overwhelming—harm reduction works. Opioid substitution therapy has been associated with a 54% reduction in the risk of HIV infection among people who inject drugs and has been shown to decrease the risk of hepatitis C infection, to increase adherence to antiretroviral therapy for HIV, to lower out-of-pocket health expenditures and to reduce opioid overdose risk by almost 90%.
In Australia, 10 years of needle–syringe programming has reduced the number of cases of HIV by up to 70% and decreased the number of cases of hepatitis C by up to 43%.
The evidence is also clear that laws and policies that hinder access to health services for people who use drugs do not work. For example, police surveillance of health-care and harm reduction service providers discourages people who inject drugs from accessing those services.
“Putting the AIDS response on the Fast-Track requires promoting the rights of people who use drugs to access high-quality, evidence-informed HIV harm reduction services and removing barriers to accessing these services,” says Aldo Lale-Demoz, the Deputy Executive Director of the United Nations Office on Drugs and Crime.
Having laws that offer alternatives to prosecution and imprisonment for drug use and possession of drugs for personal use reduces the harmful health effects associated with drug use and does not result in an increased use of drugs.
Community-led harm reduction programmes can reach people who inject drugs with needle–syringe exchange and other services and provide linkages to testing, treatment and care for people living with HIV. In Pakistan, for example, the Nai Zindagi Trust, a peer-led outreach programme, has been in operation for 25 years and reaches about 13 000 street-based people who inject drugs through more than 600 trained peer educators.
The case for investment
Despite the large body of evidence, however, only 80 of the 158 countries in which injecting drug use has been documented have at least one location offering opioid substitution therapy, and only 43 countries have programmes in prisons. Needle–syringe programmes are available in only 90 countries and only 12 countries provide the recommended threshold of 200 sterile needles per person who injects drugs per year.
The combination of unavailability of harm reduction services and inadequate coverage where available puts progress in the response to HIV at risk. It also denies life-saving health services to millions of people who inject drugs.
“When it comes to people who use drugs, evidence has been necessary, but insufficient, to catalyse the needed commitments from governments and donors. Harm reduction is one HIV prevention technology that clearly works, that people in need want and that costs little. Disinvestment makes neither scientific nor moral sense,” says Daniel Wolfe, of the Open Society Foundations.
Current investments in harm reduction services are insufficient. And maintenance of current levels is not enough to end the AIDS epidemic by 2030 and meet the commitments made in the 2016 Political Declaration on Ending AIDS. The majority of people who inject drugs live in middle- and upper-income countries, yet current donor policies are transitioning international aid out of middle-income countries, putting in danger the continuation of existing services and risking the reversal of successes to date.
It is hoped that affected country governments, the successful replenishment of the Global Fund to Fight AIDS, Tuberculosis and Malaria, and new initiatives, such as the Key Populations Investment Fund, will contribute significantly to scaling-up evidence-informed programming for people who inject drugs.
“People who inject drugs are among those who have been left furthest behind by the global response to HIV,” says Mauro Guarinieri of the Global Fund, “We need to recognize that the level of criminalization, discrimination and violence that people who use drugs face, can only result in driving risk-taking behaviours, excluding them from the social and health support systems they need. We must move toward treating everyone, including people who use drugs, as fellow human beings.”
Resources
Related


Feature Story
Decentralization of HIV testing services to increase access for people who inject drugs in Viet Nam
12 October 2016
12 October 2016 12 October 2016In Viet Nam, the Authority for HIV/AIDS Control and the Ministry of Health piloted outreach HIV testing services to increase uptake among people who inject drugs and their partners. Bi-monthly HIV testing was offered in villages where there were large communities of people who inject drugs.
The outreach team included two health service staff, one village health worker and one peer educator. People who inject drugs and their partners were invited to a convenient location and offered HIV counselling and rapid HIV tests. Reactive test results were sent for confirmatory testing and clients with a confirmed diagnosis of HIV were counselled and linked to clinics for treatment and care.
From September 2014 to January 2015, 8.9% of people tested were newly diagnosed with HIV—approximately four times higher than the percentage observed at district primary health-care facilities. The results of this pilot programme suggest that the provision of community-based HIV testing services is a feasible and efficient method of increasing knowledge of HIV status among people who inject drugs and their partners, as well as other key populations. Peer educators and village health workers were instrumental in reaching the target population. This model will inform the development of national guidelines on community-based HIV testing. Source: http://who.int/hiv/pub/guidelines/hiv-testing-services/en/.
To find out more about harm reduction, please go to the World Health Organization harm reduction page at http://who.int/hiv/topics/idu/en/ .
Resources
Consolidated guidelines on HIV testing services
Do no harm - Health, human rights and people who use drugs
Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations
Guidance on prevention of viral hepatitis B and C among people who inject drugs
Harm Reduction International “Global State of Harm Reduction”
Region/country





Feature Story
China and Cambodia share successful experience in the AIDS response
13 October 2016
13 October 2016 13 October 2016A Chinese delegation visited Phnom Penh, Cambodia, from 11 to 13 October to promote innovative partnerships between the government and civil society. Both countries have partnered with communities and tailored their AIDS response to the specific needs of key populations at higher risk of HIV.
The mission was organized on the eve of an official visit by China’s President, Xi Jinping, to Cambodia, with support from the UNAIDS China and Cambodia country offices and the Gates Foundation. It included representatives of the National Health and Family Planning Commission, the National Center for AIDS/STD Control and Prevention, the Chinese Preventive Medicine Association and the Chinese Association of STD/AIDS Prevention and Control.
The delegation was welcomed by the National Center for HIV/AIDS, Dermatology and STD, the National AIDS Authority and KHANA, the largest Cambodian nongovernmental organization (NGO) working on HIV.
Sun Xinhua of the National Health and Family Planning Commission headed the Chinese delegation and commended the progress achieved by the Government of Cambodia in decreasing HIV prevalence among the general population. Mr Sun noted that, “This visit is a great opportunity to better understand the strategies and approaches for reaching key populations and opens new avenues for South–South cooperation.” Ly Penh Sun, Director of the National Center for HIV/AIDS, Dermatology and STD, explained that, “Cambodia has recently adopted the “treat all” policy, which is a key step forward to achieving the 90–90–90 targets by 2020.”
The Chinese delegation presented the experience of civil society’s participation in the HIV response in China, noting in particular the China AIDS Fund for NGOs funding process for community organizations. Most international funding for the AIDS response in China ended in 2013, which affected civil society’s participation in the response. The Government of China committed to fill the gap with domestic resources, leading to the establishment of the China AIDS Fund for NGOs in 2015, which in its first year awarded US$ 7.5 million to more than 460 civil society organizations, with 41% of the funds going to support programmes for men who have sex with men.
“Learning from China’s transition towards more sustainable national funding was very useful, as Cambodia faces declining international funding. A key factor of success for both countries is the strong cooperation between government and civil society,” said Ieng Mouly, Chair of the National AIDS Authority, at an event organized to highlight civil society’s experience.
In Cambodia, the government works closely with civil society organizations to provide HIV prevention and support for enrolling key populations in treatment and care. Their efforts help bring services closer to key populations. The delegation visited a karaoke bar where peer counsellors provide rapid finger-prick HIV screening for entertainment workers as they wait for customers. The group also toured a club where men who have sex with men can access HIV prevention services.
“China and Cambodia are on the Fast-Track and building the sustainability of their AIDS response. UNAIDS values South–South sharing and cooperation, which promotes the scale-up of innovative approaches to better reach people,” concluded Marie-Odile Emond, UNAIDS Country Director for Cambodia.

Feature Story
A look at community-based harm reduction in Indonesia
11 October 2016
11 October 2016 11 October 2016George started using drugs more than 10 years ago. At the time he lived in Jakarta, Indonesia, and worked as a driver for an international company. About one third of people who inject drugs globally live in the Asia and the Pacific region. (Photo 1)
As George’s dependence on drugs became severe, he lost his job and could no longer provide for his wife and young children. “All I could think about was where I would get my next hit. I lied. I stole. I hated myself,” recalled George. (Photo 2)
One day George heard about a novel programme based in a large house in Bogor, Indonesia. Rumah Singgah PEKA is a community-based harm reduction programme that aims to empower people who use drugs to take back control of their lives. (Photo 3)
Sam Nugraha is the Executive Director of Rumah Singgah PEKA, which he founded in 2010. He said, “Rumah Singgah PEKA is different from other treatment centres, because it is fully voluntary. Every client has made their own decision to participate.” (Photo 4)
Most of the staff at Rumah Singgah PEKA have experience with drug dependence. The facility provides a range of services, including group and individual counselling. (Photo 5)
The organization works with public health facilities to help clients access key services. Deni Subhan, Programme Manager at PEKA, often accompanies clients to get their daily dose of methadone. (Photo 6)
Siti Nurfaiza, Programme Manager at Gedung Badak Health Clinic, finds the collaboration with PEKA good. She said, “Methadone is very helpful for the heroin user, since it helps people with drug dependence to maintain their physical, psychological and social activities.” (Photo 7)
Deni Subhan picks up a five-day supply of methadone for clients, who can then access their daily dose at PEKA, which has much more flexible hours than public health facilities. (Photo 8)
George has gradually decreased his methadone dose. He now works for PEKA and is once again able to provide for his family. (Photo 9)
George said, “All of us are entrusted to make our own decisions. If we wish to make a good decision, the community is here to help.” (Photo 10)
Region/country





Feature Story
Plain speaking: bringing condoms into the open
05 October 2016
05 October 2016 05 October 2016“I want to make it in the corporate world,” says 19-year-old Millicent, known as Milly. A marketing major at the University of Botswana, she exudes sophistication and self-confidence.
But Milly has not always felt so confident about making the right decisions. She has not always felt able to protect herself from sexually transmitted infections, including HIV, or from unintended pregnancy. She was embarrassed to be seen to be sexually active and didn’t feel comfortable taking free condoms at the government clinic. And her boyfriend, Peter, felt self-conscious buying condoms at the pharmacy so they didn’t always have protected sex.
Milly says people tend to link condom use with promiscuity. “There’s a stereotype about teenagers using condoms,” she explains. “Condoms are said to be for adults. People don’t want to talk about them.” At the clinic, “You couldn’t just go in and take one,” she explains. “You were criticized because you were young and wanted condoms.”
Milly’s parents gave her only the most general information about preventing HIV, even though her father is a physician. Cultural norms in Botswana inhibit parents and children from talking openly about sex; it is assumed that if teenagers know about condoms, “they will want to experiment,” says Milly. She and Peter read a little about condoms, but they were still unsure how to use them. “We knew we were taking risks,” she says.
Milly and Peter belong to the age group, 15–24-year-olds, most at risk of HIV infection and UNAIDS reports that females 15–24 years old are twice as likely as males to be living with HIV. Kabo Ngombe of Botswana’s Ministry of Health says that a reluctance to talk about condoms is one reason why more young people do not use them. “A lot of people know about HIV and prevention methods, but they’re not changing their behaviour,” she says. “Young people lack role models. Their parents can’t talk to them about HIV. They prefer to learn from other young people.”
This is what happened to Milly. One day she saw a brightly painted truck moving slowly down the road with the word CONDOMIZE! painted on its side, surrounded by a lively young crowd. Standing in the bed of the truck were other young people, all wearing sleek black T-shirts with the words “Love Smart! Play Safe! CONDOMIZE!” blazoned across the front in electric pink. They wore bright pink hard hats on their heads. Rock music played as they warmly invited passers-by to step up and learn about condoms.
“This truck was really pulling a crowd!” says Milly. “I wanted to know who these people were and what they were doing in our community. It turned out they were educating young people about how to use condoms! And these were young people just like me! As a teenager, I want another teenager to give me information, not someone who criticizes me. This was really great!”
To date, this truck and a smaller one like it have covered some 2000 kilometres throughout Botswana. They are a major feature of the country’s CONDOMIZE! campaign, launched in June 2014 by the United Nations Population Fund and the Condom Project to draw attention to condoms in a user-friendly, welcoming, fun way that attracts young people like Milly. The young people on the truck were among 35 local volunteers trained to educate their peers about condoms. Botswana is one of six African countries where CONDOMIZE! campaigns have been going on since 2011.
The truck pulled up in a park where a table covered with bright displays of condoms had been set up, and the crowd continued to grow. The CONDOMIZE! team passed out baskets full of colourful condoms and packets of water-based lubricant, encouraging everyone to help themselves. “It was amazing!” says Milly “I didn’t know colourful condoms existed!” The condoms she saw that day came in many varieties as well as colours, different sizes and textures (ribbed, studded with little bumps, etc.), different thicknesses and appealing scents (banana, strawberry, chocolate), and had attractive packaging. By contrast, the free government condoms come in one size, shape and colour: orange. They are considered inferior because they are not branded and people say they smell bad and break easily.
But the new condoms went like hot cakes. “I took a lot,” Milly says with a giggle. “It was so much fun! Everybody was very surprised, very impressed and very happy to have such a campaign coming to educate them, to give them free condoms!”
Nowadays, Milly and Peter use condoms consistently and correctly, including the female condom, which was new to them. They enjoy the variety of textures, colours and scents, as well as the lubricants, which they didn’t know about before. Milly has come across other CONDOMIZE! events since then, and she is well-supplied with condoms.