Feature Story
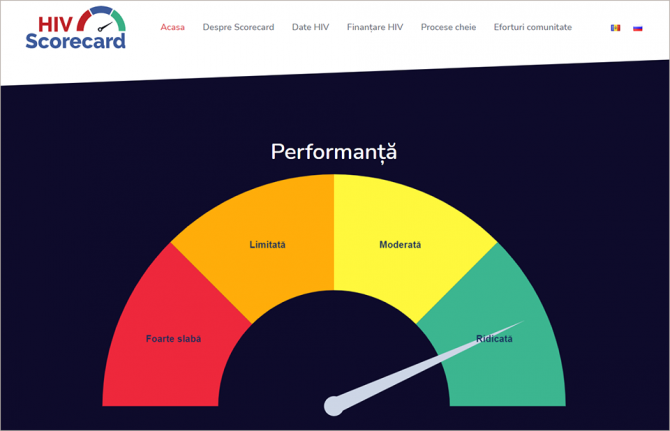
Republic of Moldova is pioneering high-tech community-led monitoring
31 May 2021
31 May 2021 31 May 2021The Republic of Moldova has launched an online platform, ScorecardHIV, to measure progress in the country's HIV response.
The new tool includes indicators and data on epidemiology, funding and procurement, programmes, human rights and community-led services. It will allow governmental institutions, health programme managers, HIV service organizations, communities and other stakeholders to track the progress and assess the effectiveness of HIV programmes in the country. A data filtering system allows the customization of indicators in accordance with the user’s interests and needs.
“The ministry will take the lead and provide political support to make sure further implementation of the tool is as effective, systematic and sustainable as possible,” said Denis Chernelya, the Secretary of State at the Ministry of Health, Labour and Social Protection. “It will be an extremely useful tool for internal monitoring as well as for understanding the main factors that contribute or impede the achievement of the set targets.”
The scorecard aims to ensure open, transparent and collective state and community-led monitoring of the HIV response. It will contribute to real-time data analysis and a rapid evidence-informed HIV response. The platform was developed by the UNAIDS Country Office for the Republic of Moldova together with the Positive Initiative nongovernmental organization and other local civil society organizations under the auspices of the Ministry of Health, Labour and Social Protection and the National Programme for the Prevention and Control of HIV/AIDS and Sexually Transmitted Infections.
The indicator map of the scorecard, which was discussed and agreed upon by all stakeholders, is sourced from the national HIV programme, ministries and government agencies and civil society organizations and is updated regularly, depending on the selected indicator—once a month, quarterly or half yearly. The platform allows data to be aggregated from different applications and sources and visualizes progress and failures in HIV programme implementation almost in real time. A task force consisting of several community organizations will update the scorecard and periodically review it.
The scorecard demonstrates how real-time data, technology and innovation can be of service for evidence-informed decisions and can strengthen cooperation between the government and communities.
“If we need to make decisions today, then we need the most recent data today. All our efforts were aimed at digitizing all possible processes, creating an infrastructure and finding IT solutions where everything can be accumulated, and then creating an analytics tool that will show us the main indicators,” said Ruslan Poverga, the Director of the Positive Initiative.
“We welcome such an important development in the Republic of Moldova,” said Alexander Goliusov, Director, a.i., of the UNAIDS Regional Support Team for Eastern Europe and Central Asia. “The scorecard was developed in line with the core principles of the new global AIDS strategy, including significant and measurable participation of civil society, a national response based on the available scientific evidence and technical knowledge, and respect for human rights and gender equality. I believe that the ability to track progress in real time, identify priority areas for rapid measures and political will and buy-in by the county’s national authorities will enable the Republic of Moldova to significantly accelerate progress towards the goal of ending AIDS by 2030.”
Learn more
Region/country
Related


Feature Story
UNAIDS supports the Partnership for Accelerated COVID-19 Testing in Ghana
25 May 2021
25 May 2021 25 May 2021The UNAIDS Country Office for Ghana is supporting the Millennium Promise Alliance, the Network of People Living with HIV and the Young Health Advocates Ghana in a partnership to strengthen community engagement in the COVID-19 response.
Aimed at reducing the community spread of COVID-19 and minimizing its effects on reaching the national HIV targets, the Partnership for Accelerated COVID-19 Testing (PACT) in Ghana will encourage the adoption of COVID-19 preventive behaviours, such as physical distancing, wearing face coverings and hand hygiene, reduce COVID-19-related stigma, promote vaccine uptake and strengthen the capacities of communities.
The PACT initiative in Ghana targets the two regions with the heaviest COVID-19 burden: the Ashanti and Greater Accra regions. Launching the project, the Director-General of the Ghana Health Service, Patrick Aboagye, commended the initiative and highlighted the urgent need for an all-hands-on-deck approach to end the COVID-19 pandemic.
The UNAIDS Country Director for Ghana, Angela Trenton-Mbonde, emphasized the importance of galvanizing HIV civil society to strengthen community engagement in the fight against COVID-19. “PACT will generate evidence for advocacy from communities, including people living with HIV, women’s groups and other vulnerable populations, to identify and inform health authorities of any disruption of essential health services, particularly HIV-related services at the community level, and will mobilize for greater uptake of those services,” she said.
The PACT initiative, launched by the Africa Centres for Disease Control and Prevention in April 2020, aims to conduct 10 million COVID-19 tests on the African continent. PACT has three pillars: test, trace and treat, which cover the procurement and distribution of COVID-19 test kits, the deployment and training of one million community health-care workers to support contact tracing and monitoring, and COVID-19 sensitization measures.
Our work
Region/country
Related
 Impact of US funding cuts on HIV programmes in Ghana
Impact of US funding cuts on HIV programmes in Ghana

08 April 2025




Feature Story
The world can only beat AIDS by ending the inequalities that drive the epidemic
21 May 2021
21 May 2021 21 May 2021By Winnie Byanyima, UNAIDS Executive Director; and Tomas Tobé MEP, Chair of the European Parliament’s Development Committee
Forty years since the first cases of AIDS were diagnosed, the fight against HIV goes on. Although the world has developed the scientific knowledge and medical expertise to keep people living with HIV alive and healthy and prevent new HIV infections, we are not on track to end the AIDS epidemic as a public health threat by 2030.
In 2019, almost 700,000 people died from AIDS-related illnesses. A staggering 1.7 million people were newly infected by HIV - more than three times the target set in 2016, which would have put us on course to end the AIDS epidemic.
The medicines, information, and prevention tools are simply not reaching the people who need them most. We need a new approach that reduces the inequalities that drive the AIDS epidemic and puts people at the centre, prioritising human rights, respect, and dignity.
Social injustices and inequalities fuel epidemics. For example, the AIDS epidemic is having a devastating impact on an entire generation of young women and girls in sub-Saharan Africa. Around 4500 adolescent girls and young women aged 15-24 acquire HIV every week in this region, and they are twice as likely to be living with HIV as their male peers.
At the same time, girls and young women face sexual and gender-based violence, unintended pregnancy and may be forced to drop out of school. Yet, completion of a high school education, including comprehensive sexuality education, is one of the surest ways to keep young women and girls free of HIV.
It is also deeply concerning that more than 60 percent of new HIV infections globally occur among key populations (gay men and other men who have sex with men, people who use drugs, sex workers, transgender people, prisoners, and migrants) and their sexual partners. Entire communities and groups of people are being locked out of the right to health, well-being and to dignity because they are marginalised and criminalised.
This can - and must - change.
The UNAIDS Global AIDS Strategy 2021-2026 provides clear and effective guidance on what needs to be done to create fairer societies to get the world back on track to end the AIDS epidemic as a public health threat by 2030.
The strategy aims to put people at the centre, removing social and structural barriers that prevent people from accessing HIV services, empowering communities to lead the way, strengthening and adapting systems so they work for the people who are most acutely affected by inequalities, and fully mobilising the resources needed to end AIDS.
The European Union has the political weight, the financial clout, and the policy tools to significantly contribute to the global fight against HIV/AIDS. The European Parliament has just adopted a Resolution on Accelerating progress and tackling inequalities towards ending AIDS as a public health threat by 2030 in response to the Global AIDS Strategy.
It outlines concrete actions that the EU should take to end AIDS once and for all. These include supporting partner country efforts to build strong and resilient health systems able to deliver HIV-sensitive universal health coverage, to prioritise health as part of EU-Africa relations and to scale-up investments in UNAIDS and the Global Fund to Fight HIV, Tuberculosis and Malaria.
The resolution also seeks to mobilise EU leadership in addressing the human rights and gender inequality drivers of HIV/AIDS and to ensure that the EU supports community-led responses as key components in an effective HIV/AIDS response.
Next month, countries will gather for the United Nations General Assembly High-Level Meeting on HIV/AIDS where they are expected to back a bold new plan to end the AIDS epidemic, including new targets for 2025.
By achieving these targets, the number of people newly infected with HIV will fall to 370,000 by 2025, and the number of people dying from AIDS-related illnesses would be reduced to 250,000. Tackling the intersecting inequalities that fuel the HIV epidemic will be crucial to success.
The COVID-19 pandemic has exposed profound social and economic inequalities, underfunded public health systems, and the fragility of global responses. Certainly, COVID-19 is threatening to undermine hard-won gains made by the HIV/AIDS response, further threatening progress towards ending AIDS by 2030.
At the same time, countries are leveraging the HIV infrastructure and lessons learned from dealing with the HIV epidemic for a more robust response to both pandemics. Indeed, we have a unique opportunity to translate the right to health into rights-based, equitable, people-centred systems.
We must utilise this window to intensify global solidarity, including sustained investments in development, to build more resilient societies that reinforce everyone’s security.
The EU and UNAIDS share core values of humanity and equality to ensure that no one is left behind. Ending the AIDS epidemic by 2030 remains within the world’s reach but it cannot be done without creating stronger societies built on the principles of gender equality, social justice, and the recognition of universal human rights, including sexual and reproductive health and rights.
Failure to do so will put the lives of millions at risk and undermine the common mission of achieving the 2030 Sustainable Development Agenda, including the end of AIDS as a public health threat.
This op-ed was first published on theparliamentmagazine.eu
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Related


Feature Story
How the LGBTI community is surviving the COVID-19 pandemic in Indonesia
25 May 2021
25 May 2021 25 May 2021For Vanessa Chaniago, a young transgender woman living in Jakarta, Indonesia, the first few months of the COVID-19 pandemic were filled with fear. “I was really struggling to make ends meet. I had been working for a civil society organization, which was a great place to learn and develop strong networks, but unfortunately the income was not sufficient to sustain me and my family. My income drastically declined,” she said.
According to a survey conducted by the Crisis Response Mechanism (CRM) Consortium of 300 lesbian, gay, bisexual, transgender and intersex (LGBTI) people in Indonesia, the COVID-19 pandemic has caused most LGBTI people to have experienced layoffs or reductions in income or to close their businesses. Most LGBTI people work in sectors with a higher risk of COVID-19: 20.5% in the beauty industry, 19.5% in the health sector and 12.8% in the service industry. Unfortunately, most of the respondents do not have long-term savings—30% would only be able to survive for two to three months on their savings, and 64% are not able to access loans.
Reflecting back on more than a year of the pandemic, Ms Chaniago said that the situation didn’t rapidly improve and instead got more challenging as time went on. “I decided to start a small business, selling beef rendang and other Indonesian street food. Opening a business during the pandemic wasn’t ideal, and not long after the opening I had to close down my store. Now I continue my small business on the streets.”
Ms Chaniago is determined to survive these trying times and she recognizes that many of her fellow transgender women face bigger hurdles. Many transgender people in Indonesia do not have identity cards, leaving them unable to access social support from the government. The CRM survey found that 51% of respondents did not receive social support from the government and those that tried to receive it faced many challenges in accessing it.
On top of the socioeconomic struggles they face, discrimination and violence towards the LGBTI community continues—transgender women in Jakarta have even been pranked with aid packages filled with garbage. The CRM survey also found that violence against LGBTI people increased.
Keeping in touch virtually among the community has been essential. Ms Chaniago said, “I want to tell my fellow LGBTI peers that they are not alone. As a community, we must continue to help each other out and fight for what is right.” Unfortunately, the CRM survey found that the community cannot always turn to peers for support, as many don’t have devices or enough Internet data to contact their friends.
Despite the huge hardships, there is a strong sense of optimism and hope for a better life after the pandemic. To get there, however, the LGBTI community needs support, including form the government and the public.
“Everyone has been affected by COVID-19. In Indonesia, many vulnerable groups have struggled to survive not only the pandemic but the devastating impact of loss of livelihoods and income. UNAIDS works with partners to strengthen the protection of vulnerable groups from stigma and discrimination in order to increase equitable access to support and services,” said Krittayawan Boonto, the UNAIDS Country Director for Indonesia.
The CRM Consortium consists of UNAIDS Indonesia and four national civil society organizations—Arus Pelangi, the Community Legal Aid Institute, Sanggar Swara and GWL-Ina. In addition to the survey, the CRM Consortium has mobilized resources for LGBTI people affected by the pandemic through the distribution of food packages, sanitation packages and rent allowances.
The results of the survey are highlighted in a video here.
Our work
Region/country


Feature Story
Integrated services and inclusion key to eliminating mother-to-child HIV transmission in Dominica
19 May 2021
19 May 2021 19 May 2021Over four consecutive years, no child in the eastern Caribbean country of Dominica was born with HIV, including in 2017 when, within two weeks, the island braved back-to-back hurricanes that ultimately damaged 90% of its infrastructure.
Dominica has now received validation from the World Health Organization (WHO) for the elimination of mother-to-child transmission of HIV and syphilis. It is the eighth Caribbean country or territory to have achieved this dual elimination goal—joining Cuba, which achieved it in 2015, and Anguilla, Antigua and Barbuda, Bermuda, the Cayman Islands, Montserrat and Saint Kitts and Nevis, which achieved it in 2017.
During a virtual ceremony, partners reflected on the mix of political, health-care and community components required to create a sustainable framework for preventing HIV and other illnesses in the maternal and child health context.
Roosevelt Skerrit, the Prime Minister of Dominica, reiterated the importance of the government’s commitment to the Sustainable Development Goal health agenda. He noted that the investments made in health infrastructure and systems would help Dominica reach other targets, including a “reduction in maternal and child mortality, universal access to sexual and reproductive health services and universal health coverage.”
“Dominica’s journey to this ambitious achievement represents a cumulation of years of expanding the capacity of its primary care services to address communicable diseases and adopting harmonized and integrated approaches to improving the health outcomes for women and their children within maternal and child health services,” said Carissa Etienne, WHO Regional Director for the Americas and Director of the Pan American Health Organization.
All pregnant women in Dominica are offered HIV and syphilis testing when they enrol for antenatal care. For those found to be positive, treatment is provided free of charge. Access to health services is available to everyone regardless of nationality. And Dominica now provides early infant diagnosis in-country, thereby ensuring accurate and timely care for infants exposed to HIV.
Health-care workers, including a cadre of community health nurses and staff of the National HIV and AIDS Response Unit, who coordinated psychosocial support and care services, were critical for the strategy’s success.
Critically, Dominica worked to strengthen its health information system so it could provide evidence relating to the coverage of antenatal care, testing and treatment services and their impact. The validation process also included assessments on human rights, gender equity and community engagement.
Meeting the rigorous data and reporting requirements for elimination of mother-to-child transmission certification is a key next step for several Caribbean countries that have already achieved remarkable gains in the prevention of mother-to-child transmission of HIV. Since 2010, the proportion of pregnant women living with HIV in the region receiving antiretroviral therapy to prevent transmission to their babies has doubled.
The Director of the UNAIDS Caribbean Sub-Regional Office, James Guwani, noted during the ceremony that next month the world will adopt a new United Nations political declaration on AIDS.
“One of the most powerful testaments to our capacity to end the AIDS epidemic is success in ensuring that children are not born with HIV. But the work does not end there,” Mr Guwani said. “We must shift the attitudes and prejudices that make it difficult for families affected by HIV to live, learn, work and play freely. We must give all young people the education, empowerment and access to services they need to remain HIV-free throughout their lives. And we must do a better job at preventing HIV infections at all age groups and among all communities. By putting people first, we can end the AIDS epidemic.”
Region/country


Feature Story
Support to countries’ equitable and resilient recovery from the pandemic towards the health SDGs: The 2021 SDG3 GAP progress report
21 May 2021
21 May 2021 21 May 2021This story was first published by the WHO
WHO and 12 other signatory agencies to the Global Action Plan for Healthy Lives and Well-being for All (SDG3 GAP) have released their second progress report, Stronger collaboration for an equitable and resilient recovery towards the health-related SDGs. This report presents progress achieved, especially at country level, where SDG3 GAP is being implemented in 37 countries, with its long-term, forward-looking SDG focus and as a platform to support countries’ equitable and resilient recovery from the COVID-19 pandemic. The report also identifies challenges encountered over the last year, acknowledging the important roles that countries, agencies’ boards and donors play in setting the right incentives for effective collaboration among SDG3 GAP agencies.
“The GAP partners have shown their unwavering commitment to countries during the pandemic," said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. "Collaboration is now more relevant than ever. The GAP provides the platform to improve collaboration in the multilateral system to support countries to recover from the pandemic and drive progress towards the health-related SDGs, with a focus on equity and enabled by stronger primary health care.”
The report highlights ways in the which SDG3 GAP agencies are integrating work at country level, reducing fragmentation through joint work in support of national priorities and plans, creating synergies and increasing alignment within the broader health ecosystem – for example, incorporating parts of the Every Woman, Every Child agenda and working jointly with the Health Data Collaborative (HDC) in countries. Many countries are prioritizing primary health care (PHC) and sustainable financing as well as data for improving equity to understand people’s lives and to know where investments need to be made to reach the most left behind.
At a recent “PHC for UHC Mission to Pakistan”, SDG3 GAP agencies renewed their commitment to better align their support for the roll-out of a universal health coverage (UHC) benefit package. Dr Faisal Sultan, Minister of Health, Special Assistant to the Prime Minister, expressed his appreciation of the mission's work, noting that “implementation of the UHC benefit package will facilitate the strengthening of PHC services and securing sustainable financing will further support us to achieve UHC, ensuring no one is left behind.”
Looking ahead, the agencies will support additional countries under the SDG3 GAP approach. The agencies are committed to reviewing progress and have recently developed a monitoring framework to enable continued learning and enhance shared accountability.
Quotes from SDG3 GAP agencies
Dr Seth Berkley, CEO, Gavi, the Vaccine Alliance:
“The COVID-19 pandemic is exacerbating inequities in many countries. The poorest and most marginalised communities have been hardest hit. Today, in the 68 countries Gavi supports, nearly 10 million children still go without any basic, routine vaccines every year. Equitable and resilient recovery will require us to work together to reach these zero-dose children, so that no one is left behind.”
Dr Muhammad Pate, Director of the Global Financing Facility for Women, Children and Adolescents:
Partnership is at the heart of the GFF's country-led model. COVID-19 has made it even clearer that collaboration is critical to fight the pandemic and achieve the health-related SDGs. Working together GAP agencies have accelerated their efforts for stronger partner alignment, engagement and accountability behind country-led response and recovery efforts to reclaim the health gains and build a more inclusive and resilient recovery.”
Peter Sands, Executive Director of the Global Fund:
"Today’s global health challenges call for an integrated approach and intensive collaboration between all partners. We are committed to working together to deliver more effective and efficient support to countries, build the path towards an equitable and resilient recovery from the COVID-19 pandemic and accelerate progress towards achieving Sustainable Development Goal 3: health and well-being for all."
Guy Ryder, Director-General of the International Labour Organization
“The ILO welcomes the progress for 2020 and as a new member looks forward to engaging with all SDG3-GAP partners in 2021 and beyond. The COVID-19 crisis has clearly demonstrated the interaction between health, social factors and decent work. It has highlighted the critical need for investments in all three areas. This will foster recovery and lead to a more sustainable, equitable development path. Equally, investments in the health of workers and of care workforce are vital to make progress towards universal health coverage. If we are to achieve SDG3, increased cooperation is needed. By joining this partnership the ILO reaffirms its commitment to support countries during this pandemic and beyond, through a multilateral and coherent approach.”
Winnie Byanyima, Executive Director of UNAIDS:
“We have seen with HIV and now with COVID-19 the critical role communities play in connecting key and vulnerable populations to essential health and social services, in ensuring gender equality, inclusion and rights-based approaches to health and social care, and in reducing inequalities. Resilient health systems rely on communities, this is why they feature prominently as a key pillar in the Global Action Plan and why they must be fully engaged, supported and funded."
Achim Steiner, Administrator of the United Nations Development Programme:
The COVID-19 pandemic affects everyone everywhere, but it is having a disproportionate impact on the world’s most vulnerable. By 2030, eight out of ten people pushed into poverty, as a result of COVID-19, will live in low and medium human development countries. Greater cooperation is the only way to defeat COVID-19 and restore and accelerate progress on the SDGs and on the pledge to leave no one behind. The SDG 3 Global Action Plan (GAP) is enhancing collaboration to support countries with their COVID-19 response and to lay the foundation for an equitable and sustainable recovery.”
Dr Natalia Kanem, Executive Director of UNFPA:
“As the world rethinks health and other systems in the wake of the pandemic, we have a chance to address the inequalities, discrimination and exclusion COVID-19 has laid bare. Let us seize this opportunity to aim for universal coverage that upholds the fundamental rights, well-being and dignity of all. With quality disaggregated data to understand who is being left behind and why, and with women and girls at the centre of our rebuilding efforts, we can identify the best investments for strong, equitable health systems and resilient communities.”
Henrietta H Fore, Executive Director of UNICEF:
"Investing in primary health care is critical to keeping children, women and families safe during and beyond the pandemic. These investments will help countries prevent and fight future epidemics and pandemics, while achieving better health outcomes overall. UNICEF is proud to stand with our GAP partners as we help governments around the world design and deliver scaled-up primary health care services that can reach every child in every community.”
Dr Philippe Duneton, Executive Director of Unitaid:
"If the past year has shown us anything, it's that global solidarity is imperative to address the critical health challenges that confront us all, but particularly the world's most vulnerable populations. Alongside work to defeat the pandemic, we must not let progress against TB, malaria, HIV, other infectious diseases and women and children's health slip backwards, but rather double down on the goal of achieving the health-related SDGs. Equitable access to innovation has a vital role to play in getting lifesaving health products to everyone, no matter where they live."
Phumzile Mlambo Ngcuka, Executive Director of UN Women:
"The negative pressures exerted on our societies and economies by the COVID-19 pandemic both demonstrated and exacerbated gender inequalities and their intimate relationship with globally pervasive issues like men’s violence against women and the burden of unpaid caregiving work carried by women and girls. Resolution of these complex problems underpins the achievement of the SDGs. It demands responses grounded in partnerships, such as the collaboration under the Global Action Plan, that rebalance power, realize women’s rights to health, and recognize their leadership roles as active agents of change in their households, workplaces, and communities."
Dr Mamta Murthi, Vice President for Human Development at the World Bank:
“The Covid-19 pandemic has exposed weaknesses in health systems worldwide and set back progress towards SDG3. The World Bank is taking fast, comprehensive action to save lives and protect poor and vulnerable people, including with $12bn for vaccines, drugs and therapeutics. Partnerships and close coordination across all agencies is essential to help countries fight the pandemic effectively. We remain fully committed to working with all partners to strengthen countries’ health systems, including for better pandemic preparedness, and ensuring that no one is left behind.”
David Beasley, Executive Director of the World Food Program:
"The COVID-19 pandemic taught us to adapt, innovate and collaborate to save lives. We need to build on these lessons and step our game up even further. Working together even more effectively is critical so we can we meet increasing needs and build back better for a healthier, more well-nourished future."
Read the full report here
Related




Feature Story
A grandmother’s transformative love for her transgender grandchild
20 May 2021
20 May 2021 20 May 2021Mampolokeng Mosolo is the picture of a dignified, proud African gogo (granny). Dressed in her Sunday best—pressed white shirt, knee-length black pencil skirt, impeccable hair and sensible heels—Ms Mosolo commands a soft power during the Khoelenya Community Council meeting in Mohale’s Hoek, a remote area in the west of Lesotho.
The council members are discussing sexual and reproductive health and rights. Ms Mosolo addresses her peers on the council with the quiet assurance of someone who has been on a life-changing journey she could not have imagined for herself as a younger woman.
When Ms Mosolo first found out that her grandchild—who was assigned female at birth and she raised as a girl—identified as a boy, she thought Mpho had been sucked into a satanic cult.
“I didn’t take it very well to hear that my grandchild thought of herself as a transgender boy,” Ms Mosolo says, a term she heard for the first time when Mpho broke the news of his gender identity to her.
When Mpho was 16 years old he would wear trousers to school as the institution’s policy gave girls the option to wear dresses or slacks.
“When girl students were then told to wear dresses, he refused and stopped going to school,” Ms Mosolo says.
Mpho eventually went back to school later that year to take exams but failed his assessments. He dropped out and then went to a local vocation school to learn sewing. That did not last long either, Ms Mosolo says, as her grandchild faced stigma and discrimination from students and teachers for being a member of the lesbian, gay, bisexual, transgender and intersex (LGBTI) community.
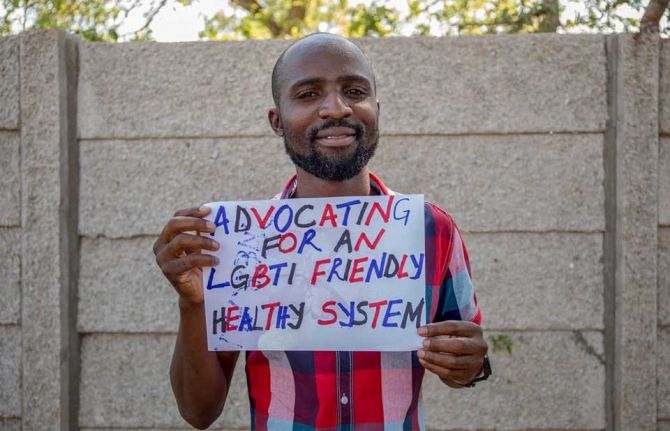
Tampose Mothopeng, a Mosotho activist and human rights defender, says LGBTI people in the small mountainous country often face a backlash from their families, peers and members of the broader community.
“LGBTI people face a lot of challenges daily,” he says. “Rejection, limited access to health-care services, stigma and discrimination and psychological issues. For instance, the health-care system is designed by the very system that rejected you. We must challenge the system until it sees us as human beings,” he emphasizes.
Mr Mothopeng runs the People’s Matrix Association, a community-based organization that advocates for LGBTI and gender-nonconforming people in Lesotho. Mr Mothopeng says it is essential to have a community driving its own mandate, otherwise organizations cannot fully understand, “the true challenges that communities are going through.”
“Without passion there is no way we can sustain volunteerism,” he continues. “Communities can stand up for their rights better than others. We need communities running their own projects.”
Indeed, Ms Mosolo and Mpho’s relationship took a positive turn after Ms Mosolo was referred to the People’s Matrix Association after attending a local HIV and gender-based violence workshop in her community, where issues of sexual orientation and gender identity were raised, and she wanted to know more.
“I received training from the People’s Matrix Association. I then sat Mpho down and said, “My child, I have accepted this because this is something that exists. They say that you are born with it and that you feel it in your blood,”” she says.
The People’s Matrix Association works with a wide range of partners to conduct sensitization workshops on LGBTI issues and works closely with faith-based organizations in Lesotho to foster a culture of acceptance between the church and LGBTI people.
The Khoelenya Community Council works in partnership with Phelisanang Bophelong, a community-based organization that provides HIV prevention and treatment support to people living with HIV. PB, as it is known locally, with the support of UNAIDS, supports the council to run HIV, sexual and reproductive health and rights and gender-based violence sensitization dialogues with the local community.
Through this forum Ms Mosolo was further exposed to LBGTI people and, through this experience, came to understand her grandchild better.
Mpho is now 23 years old and works in Cape Town, South Africa. Ms Mosolo hopes he will return home to Lesotho one day. She says she would like to build him and his future wife a home on her land. “I would rest knowing Mpho has a place to call his own,” she says.
Ms Mosolo’s journey has brought her a great deal of acceptance, a quality she promotes to her peers on the council and to people in her community. She too has become a human rights defender.
“As people we need to accept and embrace that this is here. I have seen with my own eyes that some men fall in love with men. We need to embrace it for children to progress with their lives,” she says.
Region/country


Feature Story
UNAIDS and its partners implement Partnership to Accelerate COVID-19 Testing in Madagascar
18 May 2021
18 May 2021 18 May 2021UNAIDS is partnering with the Africa Centres for Disease Control and Prevention (Africa CDC) to support the roll-out of the Partnership to Accelerate COVID-19 Testing (PACT) in Africa, including Madagascar.
The PACT initiative, launched by the Africa CDC in April 2020, aims to conduct 10 million COVID-19 tests on the African continent. PACT has three pillars: test, trace and treat, which cover the procurement and distribution of COVID-19 test kits, the deployment and training of one million community health-care workers to support contact tracing and monitoring, and COVID-19 sensitization measures.
With funding from PACT, Madagascar is implementing a project to strengthen the engagement of civil society in the national COVID-19 response in the country. The first phase of the project has been initiated in six districts of the former province of Mahajanga, part of the Boeny region in south-west Madagascar.
Mahajanga has been chosen for the first phase because of its high HIV prevalence among key populations. According to a 2016 national survey, HIV prevalence is particularly high among sex workers, at 22.7% in 2016. As the former province is frequented by tourists, there are also concerns that another wave of COVID-19 may occur.
UNAIDS, the National AIDS Council, the Ministry of Health, at least 40 representatives of networks of people living with HIV and networks of lesbian gay, bisexual and transgender people (LGBT), a representative of the Mayor of Mahajanga and representatives of the health centre, local school and prisons attended a launch of the project. During the launch, 60 bottles of bleach were offered to the municipality to assist tuk-tuk drivers in Mahajanga with hygiene, as they and their passengers are at higher risk of COVID-19 infection.
Five community-led organizations have been identified to develop an implementation plan for the PACT project. The plan will be finalized after the results of a situational analysis of the impact of COVID-19 in the Boeny region are made available. The main recipients of the project are an estimated 136 000 people—people living with HIV, adolescents both in and out school, prisoners and key populations.
The project will engage local authorities and beneficiaries to contribute to effective implementation of the PACT project in Mahajanga and to the intensification of COVID-19 tests, with a particular emphasis on strengthening demand generation and contact tracing.
“We are proud to be among the seven African countries to receive funds to support the deployment of PACT,” said Jude Padayachy, the UNAIDS Country Director for Madagascar. “This project focuses on the COVID-19 response among people living with HIV, LGBT people, young people and adolescents, who have difficulty accessing care due to stigma and discrimination. No one should be left behind.”
Our work
Region/country



Feature Story
#NotYetUhuru: 60-year-old Patson Manyati reflects on being gay in Zimbabwe*
17 May 2021
17 May 2021 17 May 2021Patson Manyati cuts an awkward and lonely figure in a room bustling with young people in their twenties. His elegant poise, greying beard and baby blue shirt place him at least 40 years too old for this scene.
Mr Manyati is on one of his first visits to the drop-in centre of Gays and Lesbians of Zimbabwe (GALZ) in Mutare, in eastern Zimbabwe. GALZ is a membership-based association that promotes, represents and protects the rights of lesbian, gay, bisexual, transgender and intersex (LGBTI) people in Zimbabwe.
While Mr Manyati may look out of place, being at GALZ is the most “comfortable” he has ever felt as a gay man living in Zimbabwe in his 60 years.
“When I see people like me, I feel very happy,” says Mr Manyati in his musical, soft-spoken voice. His eyes don’t stop shimmering while he talks. Remarkable for someone who has grown up around pervasive homophobia. The kind of homophobia that, as recently as 2017, saw the former president describe gay people as, “worse than dogs and pigs.”
GALZ maintains that the hatred and fear caused by the late president’s particular brand of homophobia, “is still being felt in Zimbabwe today.”
While being at GALZ makes him happy, as soon as Mr Manyati ventures out beyond the gates of the premises, he must be guarded and vigilant. Beyond the insults, the threat of jail is real, as Zimbabwe punishes same-sex sexual relationships with up to 14 years imprisonment.
Beyond jail, there is the everyday lived experience of discrimination, violence and hate crimes with which LGBTI people must contend—not only in Zimbabwe, but also in the 69 countries worldwide that criminalize same-sex sexual relationships.
And even in countries that don’t, like neighbouring South Africa. While same-sex marriage is legal and LGBTI rights are constitutionally enshrined, being gay is dangerous. In the first half of 2021, there has been a spate of murders of young gay men and an outcry from the LGBTI community for the government, media and public to take hate crimes more seriously.
Under these conditions, it is an act of defiance just to exist and, even more so, to be deliberately happy.
Happiness is something Mr Manyati has tried to carve out for himself, despite the odds.
Born in Mutoko, a small town in Zimbabwe’s Mashonaland East Province, Mr Manyati says his parents expected him to get married in his twenties to a woman and to carry on the family name as one of the seven Manyati sons.
While his parents insisted on marriage for some time, Mr Manyati stood his ground. As the sole caregiver for his parents and siblings, they eventually gave in and he lived his life single, never coming out to his parents.
“I couldn’t get married because I have the body of a male but, inside, I feel like a female. I know I am … I feel … like a female. So why should I marry a female?”, he says, visibly grappling with complex concepts about his gender identity without the vocabulary to do so.
Here at GALZ, everyone tells him “who they are,” says Mr Manyati. Perhaps with a few more visits and more interaction with the young people around him, who are so much more self-assured in their sexual orientation and gender identity, it may not be too late for Mr Manyati to give name to his feelings.
GALZ is a lifeline for its members. It offers regular clinic days at its Harare drop-in centre and referrals at its other drop-in centres, in Mutare and Masvingo, for a range of health-care services, including HIV prevention and treatment. It also provides critical counselling services and safe spaces for LGBTI people to socialize and relax, away from the “harsh” streets.
The leadership at GALZ says that things are slowly getting better for LGBTI people in Zimbabwe.
In 2017, GALZ was included as an official participant in the funding proposal developed for the Global Fund to Fight AIDS, Tuberculosis and Malaria. This helped to secure US$ 2 million for programmes that serve gay men and other men who have sex with men, the largest investment ever in an HIV and sexual and reproductive health response for the community. The funding resulted in the three GALZ drop-in centres.
The National AIDS Council (NAC) of Zimbabwe has a key populations forum, supported by UNAIDS, and of which GALZ is a member. The NAC is visibly working to improve the health and well-being of key populations even while their activities remain criminalized.
Despite progress, the lingering stigma and discrimination that the LGBTI community faces in Zimbabwe has resulted in Mr Manyati and people of his generation leading an isolated life.
“It makes me feel safer to rather stay by myself,” says Mr Manyati, adding that all his peers and friends from the LGBTI community have since died. “Sometimes I cry,” he sighs.
When Mr Manyati’s friends were alive, they would live their lives to the fullest, even though the law was a constant threat and they remained unlucky in love with the men they encountered.
“[You would know] he doesn't really like you because he has another love somewhere and you are just one on the side. In the end, he gets married and leaves you,” says Mr Manyati of these encounters.
Mr Manyati is adamant that he is “too old” to look for love now, and that he would rather focus on looking after his health as one of the estimated 1.4 million Zimbabweans living with HIV.
Mr Manyati discovered he was living with HIV when he developed a cough five years ago. He went to a local nongovernmental organization, New Start, for an HIV test and after a course of tuberculosis treatment he was initiated immediately onto HIV treatment. His health is his main priority.
“I continue with HIV treatment. That’s how I’m looking healthy now,” Mr Manyati concludes, eyes still shimmering.
* Not Yet Uhuru is a quote by the Kenyan freedom fighter Oginga Odinga. Uhuru is a Swahili word meaning “freedom”; thus, it loosely means “not yet free”. It is a hashtag routinely used by GALZ in its social media posts.
Our work
Region/country


Feature Story
UNAIDS Executive Director engages with women leaders and young women in Namibia
19 May 2021
19 May 2021 19 May 2021Monica Geingos, the First Lady of Namibia, showcased two flagship programmes of the Office of the First Lady to the UNAIDS Executive Director, Winnie Byanyima, during Ms Byanyima’s recent country visit to Namibia.
Launched in February 2018, the #BreakFree anti-violence campaign aims to contribute towards preventing violence through awareness-raising around various forms of violence in Namibia and finding pragmatic solutions for prevention.
As part of the campaign, Ms Geingos hosted a women leaders’ dialogue to engage Ms Byanyima and women leaders in Namibia on critical discussions about gender inequality and gender-based violence as critical structural drivers of the HIV epidemic.
Women leaders called for collective support and leadership towards achieving gender equality and ending gender-based violence in Namibia through national gender policies and strategies. “We need to use the law as a tool for social justice,” said Yvonne Dausab, the Minister of Justice, during the dialogue.
The Government of Namibia has recently launched a mass media campaign, Nationhood and National Pride, against gender-based violence. This comes at an opportune time, as Namibia recorded an increase in sexual and gender-based violence, femicide and human rights violation cases in 2020, which prompted a series of youth-led countrywide protests against sexual and gender-based violence.
Last year, more than 2300 cases of domestic violence were recorded at various magistrate courts across the country, a considerable increase from 2044 similar cases registered in 2019.
“Even though progress has been made in policy development, women’s representation and other areas, girls are still born in an unequal world and violence against women still remains a challenge,” said Ms Byanyima.
Another separate yet interrelated programme of the Office of the First Lady is the #BeFree movement. It was launched by Ms Geingos in 2016 with the technical and financial support of UNAIDS and the United Nations Population Fund.
The purpose of #BeFree is to create a non-judgemental, inclusive platform that encourages honest and robust dialogue and information-sharing so that young people are free of the issues that stand in the way of their development. This includes HIV, alcohol and drug use, unintended pregnancy, mental health issues and relationships with parents or caregivers.
Ms Byanyima, at the invitation of Ms Geingos, attended a #BeFree dialogue with young people on strengthening HIV prevention and gender equality and addressing stigma and discrimination.
During the event, Ms Byanyima reflected on her activism journey and encouraged young people to build resilience and self-confidence and to empower themselves in order to overcome the challenges they face, especially in tertiary institutions.
Ms Geingos noted the growth and transformation of the #BeFree movement in the past five years. Under the movement, her office has hosted and facilitated more than 35 dialogues and reached more than 100 000 young people and partners from all sectors of society. Ms Geingos asked young people to continue to speak out against violence, abuse and discrimination while also ensuring that they achieve academic excellence and their goals and aspirations.
To conclude her visit to Namibia, Ms Byanyima met with Hage Geingob, the President of Namibia, above, to acknowledge Namibia’s commitment to the AIDS response and the country’s success in attaining the 90‒90‒90 treatment targets ahead of the 2020 deadline and its domestic investment in the HIV and health responses.