



Feature Story
Protecting prisoners from HIV and COVID-19 in Mexico
14 May 2021
14 May 2021 14 May 2021“AIDS came to my door as a surprise. It all started in 1988, when my partner, Rafael, started to get sick. We were both 28 years old at the time,” said Georgina Gutiérrez, who has been a human rights activist for people living with HIV in Mexico for more than 30 years.
Today, she is a representative of the Mexican Movement for Positive Citizenship, which aims to promote the empowerment of people living with HIV in prison. She is also part of the Latin American and Caribbean Movement of Positive Women.
“In those years, stigma and discrimination were widespread. I knew about HIV only through television and many women who had HIV-positive partners assumed they were living with HIV without ever having been tested,” she said.
Her partner was imprisoned in Santa Martha Acatitla Penitentiary in Mexico City, where he spent eight years. This was when she got to know the reality inside prison, and it was this experience that would set the course of her life towards working with jailed people living with HIV.
“People living with HIV in prison are invisible to society. I remember many years ago, as a protest they would burn their mattresses, just to demand dignity in their access to HIV treatment,” Ms Gutiérrez recalled.
Ms Gutiérrez knew that there was a need for action to protect the physical and mental health of people living with HIV in prison. This is how she and others started a project against HIV and COVID-19 in the Santa Martha Acatitla Penitentiary.
The project is one of 30 initiatives selected from more than 190 applicants for the UNAIDS 2020 call for proposals for community-based organizations working on HIV in Latin America and the Caribbean that received funding. The project received an award of US$ 5000 to help its work.
The Santa Martha Acatitla Penitentiary houses around 2000 inmates, including 180 people living with HIV, some in the advanced stages of AIDS-related illnesses. People living with HIV are concentrated in Dormitory 10 in the prison.
“Dormitory 10 is overcrowded and physical distancing is difficult. Hygiene standards were low. In addition, most of them had not received COVID-19 personal protective equipment—the very few who were able to access such equipment did so through their families,” said Ms Gutiérrez.
In addition to the 180 people living with HIV in the prison, each of whom received personalized face coverings and other personal protective equipment and who attended a series of trainings, approximately another 1000 staff and inmates benefited from the project.
“I have been able to see them change. They have told me many times that they feel safer with the tools and knowledge they have gained,” said Ms Gutiérrez. “They feel good to know there are people concerned about them during this health crisis.”
“With our trainings and donations, the prisoners can now keep their rooms clean and can frequently wash their hands, clothes and personal belongings.”
Working for HIV prevention is, “A commitment I have in every drop of my blood,” she said. “With these actions, we are giving life to forgotten people. I thank UNAIDS for financing this project—with it we are supporting a population that is being left behind.”
On any given day, approximately 11 million people worldwide are incarcerated. The risk of sexual violence among prisoners—and their inadequate access to condoms, lubricants, pre-exposure prophylaxis and harm reduction services—increases their chances of contracting HIV, hepatitis C and other sexually transmitted infections.
Region/country
Related

Feature Story
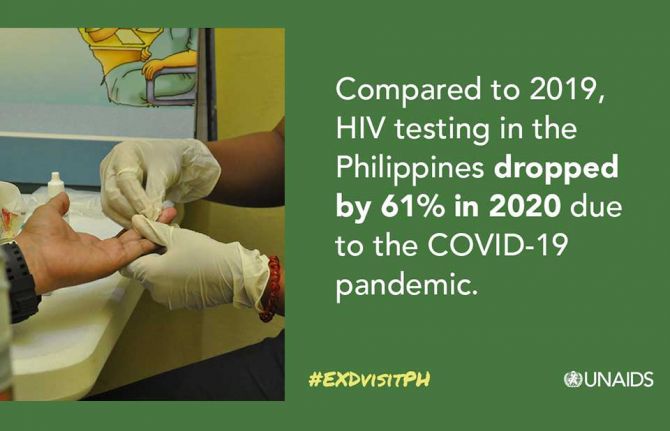
Community-led HIV services stepped up in the Philippines during the COVID-19 pandemic
11 May 2021
11 May 2021 11 May 2021The HIV response in the Philippines has been hit by the COVID-19 pandemic, especially access to HIV prevention and treatment services. According to the Global Fund to Fight AIDS, Tuberculosis and Malaria, in Metro Manila coverage of HIV prevention services for gay men and other men who have sex with men has decreased by 74% since 2019. Government figures show that compared to 2019, in 2020 HIV testing decreased by 61% and enrolment in HIV care reduced by 28%. The COVID-19 pandemic has drawn attention to socioeconomic divides, highlighting failures within the health system to adequately deal with not one pandemic but two.
Despite this, what has been clear from the onset of the COVID-19 outbreak is that civil society and communities have stepped up to the challenge to provide HIV services while navigating through restrictions on movement and lockdowns. One example is the Family Planning Organization of the Philippines (FPOP), a civil society health service provider and advocate of sexual and reproductive health and rights with a network of more than 1000 community-based services across the country. One of those service providers is the Rajah Community Center, a primary HIV clinic located in Iloilo City in the Western Visayas region of the Philippines, which provides HIV services for key populations, including young key populations, in a friendly and stigma-free environment.
“When I tested positive for HIV, I knew nothing about it. I did not know how to protect myself from it and talking about sex was taboo in my house. My friends and I were clueless about condoms,” said Jhenard Jude, a young person from Iloilo City. After receiving his positive diagnosis, Mr Jude learned about the Rajah Community Center. “I heard from my friends that Rajah provides youth-friendly services. I was worried about how others would look at me because of my status, but the staff at the clinic were non-judgemental and very friendly. I was given a care worker who supported me every step of the way to access antiretroviral therapy,” he said.
“This is home to me. I got my HIV self-test kit here in June 2020. Rajah is safe and convenient,” said Lloyd Legario, a young person who regularly visits the clinic for HIV testing and prevention services.
Winnie Byanyima, the UNAIDS Executive Director, has been learning about the Rajah Community Center during a two-day virtual mission to the Philippines to engage with communities, civil society and the government about the country’s response to HIV and COVID-19. During her virtual visit, Ms Byanyima was given a pre-recorded tour of the community clinic and had an open dialogue with Mona Liza S. Diones, the Chapter Program Manager of FPOP Iloilo, Robert Figuracion, the Rajah Community Center Clinic Officer, and three clinic clients from key populations.
“I had the pleasure to speak with some very courageous people who were very open about their experiences at the Rajah Community Center. I extend my deepest gratitude and solidarity to community-based organizations and frontline workers for stepping up and providing essential services during COVID-19,” said Ms Byanyima.
To ensure the continuity of HIV services during COVID-19, FPOP Iloilo worked closely with the Philippines Department of Health, local government units and other treatment hubs and support groups to serve key populations and people living with HIV. Blended services that included online counselling and onsite services covered prevention commodities, testing services, treatment and medical care. This also included providing psychosocial services, which have seen a sharp rise in demand since the first COVID-19 outbreak. Telemedicine and mobile clinics became new channels for differentiated care. Innovative programmes to deliver antiretroviral therapy to clients were established and pre-exposure prophylaxis (PrEP) and condoms were frontloaded to community champions for distribution.
During the virtual visit, Ms Byanyama also learned about the HIV & AIDS Support House (HASH), another renowned community-led service provider, which in coordination with the Department of Health has worked to prevent disruption to HIV services during COVID-19. HASH offers community-based screening, PrEP, HIV referral services, medical assistance to children living with HIV and psychosocial support to key populations. “Civil society organizations were quick to respond to the situation by coming out with innovative courses of action, such as online counselling, alternative modes of antiretroviral therapy delivery and mobilization of volunteers and partners to assist those who were affected by the COVID-19 pandemic,” said Desi Drew Ching, the President of HASH.
“To sustain community-led services, government and development partners have to optimize collaborative partnerships with civil society. This will strengthen their leadership capacities and enhance civic space funding through social contracting programmes,” said Louie Ocampo, the UNAIDS Country Director for the Philippines.

Feature Story
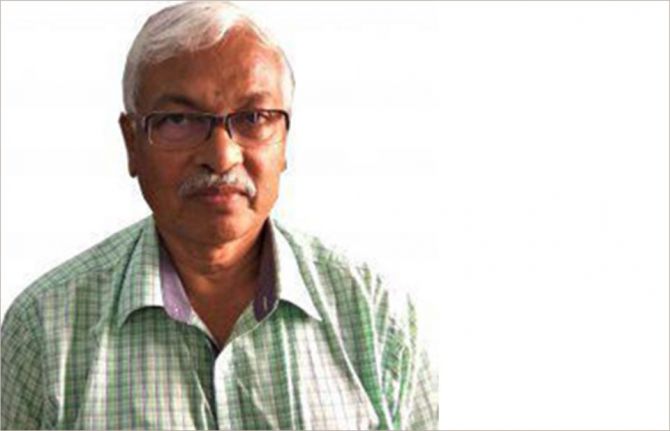
UNAIDS saddened by the death of Smarajit Jana
10 May 2021
10 May 2021 10 May 2021By Nandini Kapoor, Community Support Adviser, UNAIDS Country Office for India
The death of Smarajit Jana has left us shaken. True to his nature, he fought COVID-19 valiantly, but sadly the champion for the response to HIV succumbed to the coronavirus.
How do you begin to describe Mr Jana? A medical doctor, a public health specialist, an epidemiologist, a researcher and academician, an ardent advocate for the response to HIV and the architect of India’s national HIV response for key populations, a champion of human rights and the dignity of sex workers, the founder of the Durbar Mahila Samanwaya Committee (DMSC) collective of sex workers, a winner of national and international honours and accolades, a distinguished voice in domestic and global forums, and much more.
A great leader, an incomparable professional and, above all, a human being par excellence, he gave voice to the most vulnerable and the most marginalized to ensure they were heard and their dignity respected. He touched innumerable lives. Words are not enough to capture the range of his work and the difference he made to so many lives. What he did is etched in the hearts of the lives he touched—with warmth, with love, with affection.
He was a man of science, with his heart firmly anchored in the community he served. He brought science to the community level simply and brilliantly. And the reverse was true—he could easily translate policy and science in simple words for the community to understand.
I first met Mr Jana when I joined UNAIDS 18 years ago. We had organized a meeting for key populations and invited representatives of DMSC, since it had been key to the sex worker movement in India. We were told that they would attend, but not without Mr Jana, their guide, mentor and father figure. That was the level of trust and confidence they had in him. He spoke for their rights and ensured that the reality in the field was brought to the meeting table.
His skill at listening to the community and overlaying what he heard with policy discourse helped to move community-friendly strategies as part of the national HIV response. His presence at every meeting was full of energy and passion.
I have had several conversations with Mr Jana on a range of programmatic issues—the changing nature of sex work, preexposure prophylaxis, collectivization, decriminalization and much more, and each conversation was a learning experience for me.
I will miss him, above all his sage counsel and mentoring. But he will live on—in the work that he did and in the hearts of the vast numbers he impacted.
Our prayers are with his family and the thousands of people whose lives he touched and made better. Om Shanti.
Our work
Region/country


Feature Story
UNITY Platform publishes annual report on violence against sexual and gender minorities in Cameroon
05 May 2021
05 May 2021 05 May 2021The UNITY Platform, a network of 34 organizations for lesbian, gay, bisexual and transgender (LGBT) people, has just published its 2020 annual report on violence against sexual and gender minorities in Cameroon. The report, produced annually by all the associations that the platform covers, shows more than 2000 cases of violence and violations of the rights of sexual and gender minorities affecting 930 people in 2020, compared to just less than 1400 in 2019. More than half of the reported cases involved psychological violence, with the rest consisting of cases of physical, sexual, economic or legal violence and hate speech. Gay men were the most affected victims of violence (552), followed by lesbians (214) and transgender people (64).
The report, Transphobie: le visage d’une nouvelle crise, places particular emphasis on violence against transgender people, which is being increasingly documented. According to a survey conducted by Réseau Indépendant des Trans d’Afrique, the results of which are published in the report, 53% of transgender people surveyed had experienced gender-based violence in health facilities. The perpetrators of violence could be strangers on the street (45%), family (41%), close or distant relatives (33%), intimate partners (26%) or ex-partners (10%).
The response to the violence by the UNITY Platform, which is hosted by the Cameroonian Foundation for AIDS (Camfaids), is presented in the annual report and includes services available within member organizations and external services offered in partnership with other organizations as needed.
The response mechanism starts with documentation and investigation and continues through medical care (consultations, examinations, care, treatment, provision of medication), psychological care (counselling, assessment of mental state, psychological consultations and follow-ups), social care (provision of means of subsistence, support in finding employment, admission to temporary housing as appropriate) and legal care (legal advice, assistance in drafting and filing a complaint) provided by one or more of the platform’s organizations.
“We have a system of focal points on gender-based violence issues within each UNITY member organization who are the first point of contact for victims. This is reassuring for the victims, who feel safe and understood simply because they are in a space that is well known to them,” said Nickel Liwandi, the Executive Director of Camfaids.
External mechanisms can include legal assistance through the intervention of a lawyer or police officer, medical assistance through specialized medical consultations, examinations, minor or major surgery and forensic certification or social assistance through referral to a partner organization’s shelter.
UNAIDS recently supported the efforts of the UNITY Platform and other civil society organizations in creating a space for exchange between LGBT organizations and other civil society organizations implementing HIV programmes with key populations, such as CAMNAFAW (Cameroon National Association for Family Welfare) and CARE Cameroon, to review the assistance provided to people prosecuted because of their real or perceived gender identity or sexual orientation.
Action continues to be taken to mobilize United Nations agencies and “champions” identified within governments, nongovernmental organizations and partner institutions to support civil society advocacy, as well as to institutionalize a platform for regular coordination and review of progress in implementing Cameroon’s recently adopted Five-Year Plan 2020–2024 to reduce human rights-related barriers to accessing HIV services.
“The mobilization of Cameroonian LGBT organizations within the Unity Platform is valuable because it provides us with the evidence needed for advocacy and action. The Unity Platform’s new report will serve to assess progress in reaching the targets of the Five-Year Plan 2020–2024. UNAIDS is committed to supporting the country’s efforts in line with our vision to achieve zero new HIV infections, zero discrimination and zero AIDS-related deaths,” said Steave Nemande, UNAIDS Strategic Intervention Officer for Cameroon.
Our work
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


Feature Story
Pioneers of the harm reduction response in Uganda
07 May 2021
07 May 2021 07 May 2021The drop-in centre of the Uganda Harm Reduction Network (UHRN) looks lonely from the deserted suburban pavement. It is a non-descript house, hidden behind an imposing solid pink steel gate, in an equally non-descript neighbourhood.
It looks like so many other drop-in centres in eastern Africa that serve key populations—anonymous and low-key. Necessary characteristics, perhaps, in a region that mostly criminalizes people who use drugs, gay men and other men who have sex with men, sex workers and transgender people.
Once through the gate, visitors are greeted with a hive of activity that belies the quiet exterior. Clients and staff are buzzing around, setting up chairs under the makeshift gazebo in the verdant garden. In a few minutes, a group of people who use drugs will take part in a harm reduction workshop run by one of the centre’s staff. There is also a consulting room at the front of the drop-in centre; and at the back, is the office of Wamala Twaibu.
Mr Twaibu is the founder and chairperson of the Eastern Africa Harm Reduction Network and UHRN. A self-styled “former drug user with roots in Uganda and the pioneer of the harm reduction movement in eastern Africa,” Mr Twaibu has a kind face and a penetrating gaze that tells a story of adversity, resilience and triumph.
In the consulting room, 25-year-old Kemigisa Sandriano, a heroin user and sex worker, is taking an HIV test conducted by the centre’s resident doctor, Mukiibi Grace Nickolas. The night before, Ms Sandriano was assaulted by a client after he took off the condom during sex. She protested, telling him to leave. Her swollen, bloodshot right eye attests to what happened after that. She is smiley and talkative, seemingly unbothered by yet another instance of violence at the hands of a client. She is happy that in his battle to get his money back, she won.
Ms Sandriano was introduced to heroin by her ex-husband, who she says “ruined” her life. Nevertheless, she is upbeat about her recovery.
“I have the hope that I can stop. I even went to rehab for three months. When I saw my days of rehab coming to an end, I saw no plan and I started again,” she says.
“I am ready to go to rehab again,” she continues. “But when I come out, I don’t want to be idle. When they take us out of rehab, we need a job. They can say to us, “Work in a supermarket, work in this shop, so you can stabilize.””
Employment aside, Mr Twaibu says medically assisted treatment for people with opioid dependence is critical for rehabilitation. And, since, December 2020, with advocacy from UHRN and financial support from the United States President’s Emergency Plan for AIDS Relief and the Centers for Disease Control and Prevention, the first medically assisted treatment services in Uganda have been available at the Butabika National Mental Referral Hospital in Kampala.
UHRN screens and provides initial preparation for eligible clients and refers and links them to the hospital and provides them with ongoing psychosocial support services. In December 2020, there were 81 people who use drugs enrolled in medically assisted treatment.
Besides medically assisted treatment, through its drop-in centre UHRN offers a comprehensive package of health services, including behaviour change communication, a needle–syringe programme, psychosocial support, overdose management, HIV testing and counselling and sexually transmitted infection screening.
The COVID-19 pandemic posed a major challenge to UHRN’s clients, who even under normal circumstances face high levels of stigma and discrimination, police abuse and harassment, alienation and limited access to health and social services.
Sex workers, transgender men and women, people who use drugs and gay men lost livelihoods and faced even more violence and detention under the guise of lockdown measures. Movement was severely limited as motor vehicles required a special permit to operate.
UHRN rose to the challenge. A team of 25 peer educators used bicycles, funded by Frontline AIDS, and motorcycles to reach their clients where they were, providing antiretroviral medicine refills and condoms to clients who could not reach health facilities.
The organization rolled out virtual counselling services on risk reduction and addiction management through phone calls and WhatsApp. As part of personal protective equipment procurement, UNAIDS, through the National Forum of People Living with HIV/AIDS Networks in Uganda, provided soap and bleach to prevent COVID-19 infection among the drop-in centre’s dedicated staff, who worked right through the pandemic.
Despite the constraints of the pandemic, UHRN’s needle–syringe programme reached 287 clients in 2020, providing more than 15 000 clean needles and syringes, tourniquets, cotton balls, swabs, water ampoules, condoms, lubricant and safe-injecting information notes.
“I’m proud that harm reduction issues are taking a centre stage in Uganda,” says Mr Twaibu. “Community-led means ownership. Usually when the community is at the centre, accountability and community needs are prioritized,” he says.
Our work
Resources
Region/country




Feature Story
Specialized medical waste management equipment for Republic of Moldova’s harm reduction programme
06 May 2021
06 May 2021 06 May 2021The Union for HIV Prevention and Harm Reduction is a nongovernmental organization located in Balti, in the Republic of Moldova. It provides integrated services to people who use drugs and other affected populations throughout the north of the country.
Each year, more than 3000 people benefit from its services, which including mobile testing for HIV, sexually transmitted infections and hepatitis, harm reduction services, including a needle–syringe programme, the distribution of condoms and psychological and social support. The organization’s outreach and medical workers work closely with state clinics and hospital departments that offer opioid substitution therapy to people who use drugs.
However, the organization has faced a long-time logistical problem with regard to the collection of used needles and syringes generated by the harm reduction programme. Medical waste disposal in the Republic of Moldova, especially in the north of the country, is problematic. Ala Iatco, the nongovernmental organization’s head, explained that destruction of used equipment was only possible by contracting medical institutions to do the work and that the union had to send boxes with contaminated waste to Chisinau, the capital of the country.
“For the approximately 20 years of the harm reduction programme in the country, this problem was always present and solved through burning needles and syringes or other non-environmentally-friendly ways. We had to find a solution to increase the effectiveness of the comprehensive package of services and enhance the safety and security of personnel and volunteers while operating the needle–syringe programme,” said Svetlana Plamadela, UNAIDS Country Manager for the Republic of Moldova.
The UNAIDS Country Office for the Republic of Moldova, together with the United Nations Office on Drugs and Crime and the union, came together and suggested a solution. In July 2017, specialized modern medical waste management equipment was procured from the Russian Federation and installed within a Union for HIV Prevention and Harm Reduction facility. The total cost of US$ 23 000 was funded with resources from the One UN Joint Action to Strengthen Human Rights in the Transnistrian Region of the Republic of Moldova project, financed with the support of the Swedish Embassy and co-funded by the Center for Health Policies and Studies (PAS Center), which is a Principal Recipient of the Global Fund to Fight AIDS, Tuberculosis and Malaria.
“The availability of the one-stop disposal system provided by the needle smelters and syringe cutters significantly reduces the risk of accidental exposure and contamination with bloodborne diseases by the volunteers and medical personnel,” added Ms Plamadela.
So far, three organizations—the Union for HIV Prevention and Harm Reduction, Young Women Cernoleuca and Adolescent!—have benefited from the needle–syringe destruction equipment. Partner organizations usually make monthly shipments of needles and syringes for destruction, which are collected by field workers in eco-boxes.
According to Ms Iatco, the equipment is easy to use and maintain. “The machine transforms the contaminated syringes and needles into biologically safe waste. We save almost 50% of the cost of destruction. And, most importantly, we face much fewer risks as we avoid transportation, storage and transfer of hazardous material. For our organization, located in a remote area where no such equipment is available in medical institutions, it’s a cost-effective and less risky solution,” she said.
The needle–syringe programme in the Republic of Moldova started in 1999. Its main goal is to prevent the transmission of HIV and other infections among people who inject drugs by avoiding the sharing of injecting equipment and ensuring enhanced access to health-care services and psychosocial support. The programme also aims to curb the sexual transmission of HIV among people who inject drugs and their sexual partners by promoting the use of condoms and raising awareness about the link between drug use and risky sexual behaviours.
Region/country
Related


Feature Story
UNAIDS is saddened by the death of Patrick O’Connell, the founding director of Visual AIDS
04 May 2021
04 May 2021 04 May 2021UNAIDS is saddened by the death from AIDS-related causes of Patrick O’Connell. Mr O’Connell, who lived with HIV for nearly four decades, was the founding director of Visual AIDS.
Visual AIDS was founded in 1988 by arts professionals as a response to the effects of AIDS on the arts community and as a way of organizing artists, arts institutions and arts audiences towards direct action on HIV. The organization also assists artists living with HIV. Perhaps its most high-profile achievement, however, was designing the red ribbon worn by millions of people around the world every World AIDS Day, 1 December.
In 1991, Visual AIDS artists came together to design a visual symbol to demonstrate compassion for people living with HIV and their caregivers. Inspired by the yellow ribbons honouring American soldiers serving in the Gulf War, the artists chose to create a red ribbon to symbolize support and solidarity for people living with HIV and to remember those who had died from AIDS-related illnesses. The colour red was chosen for its, “connection to blood and the idea of passion—not only anger, but love, like a valentine,” the project founders said. The project became known as the Red Ribbon Project.
Mr O’Connell was instrumental in helping to organize the cutting, folding and distribution of thousands of ribbons around his home city, New York. He was part of the campaign to send letters and red ribbons to all the attendees of the 1991 Tony Awards in the United States of America, where actor Jeremy Irons stepped out on national television with a red ribbon pinned prominently on his lapel.
UNAIDS remembers Mr O’Connell for his vital advocacy work. The red ribbon, which today is a symbol of solidarity and support for people living with HIV not only in the United States but internationally, would not have existed without him.
Our work


Feature Story
Big drops in the cost of antiretroviral medicines, but COVID-19 threatens further reductions
03 May 2021
03 May 2021 03 May 2021Civil society activism and competition from manufacturers of generic drugs drove down the prices of antiretroviral medicines from about US$ 14 000 per person per year for first-line regimens in high-income countries in 1990 to about US$ 1200 per year in low- and middle-income countries in 2003. By 2018, the price per person per year in sub-Saharan Africa was under US$ 100 for most fixed-dose combinations that include tenofovir. The prices of other fixed-dose combinations also have continued to decline over the past few years.
UNAIDS estimates that the market value for generic antiretroviral medicines within low- and middle-income countries was about US$ 1.8 billion in 2018. Approximately 80% of generic antiretroviral medicines procured by low- and middle-income countries are currently manufactured in one country: India.
While there remains significant scope for further price reductions in countries where generic antiretroviral medicines are not yet easily accessible, disruptions caused by the COVID-19 pandemic could have the opposite effect. Lockdowns, disruptions to production, border restrictions and transport disruption threaten to affect the supply of materials and the manufacture and distribution of HIV medicines, with tighter supply factors possibly leading to pressure on market prices.
Our work
Related




Feature Story
100% Life: 20 years of fighting
04 May 2021
04 May 2021 04 May 2021100% Life, formerly known as the All-Ukrainian Network of People Living with HIV, the largest organization for people living with HIV in eastern Europe and central Asia, is marking its 20th anniversary on 5 May. Those 20 years have seen it work on the most challenging issues of the HIV response in Ukraine, on health-care reform and overcoming stigma and discrimination and barriers to accessing health services.
The organization works to provide 100% access to treatment to 100% of Ukrainian people living with HIV. It strives to improve the quality of life for people living with HIV and promotes the rights and freedoms of people living with HIV, tuberculosis and hepatitis C, including the right to self-determination and the right to make decisions that directly influence their lives.
Beginning with seven members in 2001, today it has grown to 474 members and 15 000 associate members. The first office was opened in Kyiv and now the organization unites 24 regional offices across the country.
In 2004, the organization, together with partners, prevented interruptions of antiretroviral therapy for 137 patients. At the end of 2019, 100% Life was purchasing HIV medicine for 113 000 people.
“Over the years of work, we have purchased 7 230 000 packs of antiretroviral therapy,” said Dmitry Sherembey, head of the 100% Life Coordinating Council. Think about these figures! Behind each of them is a saved life. We are grateful to all our partners who believed in us and continue to believe.”
In 2016, the first 100% Life medical centre was opened in Kyiv. Five years later, three more centres have been opened in Ukraine, in Poltava, Rivne and Chernihiv. These centres are the first clinics created by patients for patients, where services are provided free from stigma and discrimination.
“I have great respect for the struggle that the organization has waged against stigma and discrimination against people living with HIV and other vulnerable people. It is thanks to 100% Life that the first opioid substitution therapy programmes for people who use drugs in Ukraine started, sex workers began to speak openly about their rights and people living with HIV had hope for a normal life, medical care and help from the state,” said Raman Hailevich, the UNAIDS Country Director for Ukraine.
In 2016, the organization received the United States President’s Emergency Plan for AIDS Relief (PEPFAR) award for the best partnership among the 40 countries in which PEPFAR operates.
The same year, there was a breakthrough in state funding of the HIV response, which was increased by 2.3 times. The success of the 20/50/80 transition plan is partly because of the efforts of 100% Life, which worked with the government and advocated for increases in the HIV budget, access to treatment and the optimization of health-care systems.
The struggle of 100% Life won’t stop. New problems come along that need to be addressed.
“We are now facing a new challenge—the COVID-19 pandemic,” added Mr Sherembey. “Our experience gained over the years of interaction with government agencies, partners and donors allows us to contribute to the common cause of the struggle. With the support of the Global Fund to Fight AIDS, Tuberculosis and Malaria and USAID, almost a million pieces of personal protective equipment have been purchased for Ukrainian doctors and social workers, 200 000 tests for COVID-19 have been bought, equipment for oxygen stations at hospitals has been procured, information campaigns on vaccination against COVID-19 have been conducted, and much more is being done.”
Our work
Region/country
Related
 Women, HIV, and war: a triple burden
Women, HIV, and war: a triple burden

12 September 2025
 Displacement and HIV: doubly vulnerable in Ukraine
Displacement and HIV: doubly vulnerable in Ukraine

11 August 2025


Feature Story
UNAIDS Executive Director visits projects in Namibia that empower adolescent girls and young women
05 May 2021
05 May 2021 05 May 2021Winnie Byanyima, the UNAIDS Executive Director, recently visited the Hakahana Clinic in Katutura, Windhoek, Namibia, where she saw the Determined, Resilient, Empowered, AIDS-Free, Mentored and Safe (DREAMS) project in action, a project funded by the United States of America. The clinic is a government health facility and a DREAMS participating clinic that has provided health services to 10–24-year-old adolescent girls and young women since September 2020.
Together with the United States Ambassador, Lisa Johnson, and the Executive Director of the Namibian Ministry of Health and Social Services, Ben Nangombe, Ms Byanyima met with DREAMS girls and community care workers at the facility.
“I am very impressed by the confidence and optimism the young women express as a result of the support they receive through the DREAMS programme,” said Ms Johnson.
The DREAMS project seeks to reduce new HIV infections among adolescent girls and young women in Namibia and other countries in sub-Saharan Africa. In 2019, there were 1400 new HIV infections among adolescent girls and young women aged 15–24 years in Namibia—more than double the number of HIV infections among their male peers. It is therefore critical that the HIV response continues to gain momentum.
DREAMS uses a core package of evidence-informed, multisectoral interventions that are proven to reduce new HIV infections among adolescent girls and young women. This includes empowering them with social protection, safe spaces, education and economic skills and with access to family planning and sexual and reproductive health services.
“The knowledge I learnt from DREAMS has taught me about making the right decision. I feel empowered,” said Johanna Shinana, a DREAMS Ambassador.
DREAMS is implemented in five districts in three regions of Namibia and the Hakahana Clinic provides eight safe spaces for young women mostly between the ages of 19 and 24 years.
Ms Byanyima, together with Sheila Roseau, the Country Representative of the United Nations Population Fund (UNFPA), Aina Heita, the United Nations Educational, Scientific and Cultural Organization National Programme Officer for HIV/AIDS, and Thomas Ukola, the Deputy Director at the Directorate of Special Programmes within the Ministry of Health and Social Services, also visited the Namibia Planned Parenthood Association (NAPPA) clinic, which is also in Katutura.
NAPPA is a welfare organization established in 1996 to complement the Ministry of Health and Social Services to provide sexual and reproductive health services and information to young people aged 15‒24 years and lesbian, gay, bisexual, transgender and intersex people from the marginalized and underserved area around Katutura.
“I encourage young people to take advantage of the services that are offered for them and encourage others to take up these services,” said Ms Byanyima while she was at the NAPPA clinic.
Ms Byanyima was introduced to the Condomise Campaign at the clinic. The campaign, supported by UNFPA, is led by young people and provides young people with key messages on sexual and reproductive health and rights, HIV and skills on how to use condoms correctly.
Klaivert Muandingi, the President of the African Youth and Adolescents Network in Namibia, called on young people to be free in accessing condoms and other commodities. “Condomize, do not compromise. Love smart and play safe,” he said.























