



Feature Story
In Your Hands: Caribbean partners call for HIV self-testing during COVID-19
17 March 2021
17 March 2021 17 March 2021Stakeholders of the Caribbean HIV response have launched the In Your Hands HIV self-testing campaign, which advocates for self-testing policies to be developed and implemented as part of a comprehensive strategy to ensure that HIV diagnosis does not decline during the COVID-19 pandemic.
Even before COVID-19, the Caribbean was not on track to achieve the 90% testing target due at the end of 2020. In 2019, 77% of all people living with HIV in the Caribbean knew their HIV status. A survey conducted by the Pan Caribbean Partnership against HIV and AIDS (PANCAP) and the Pan American Health Organization (PAHO) showed that during 2020 facility- and community-based HIV testing services were reduced in 69% of countries due to COVID-19.
“This decline means that people with undiagnosed HIV are not getting life-saving antiretroviral treatment and, of course, continue to be unaware of their HIV status, with the risk of potentially exposing others,” said Sandra Jones, PAHO’s Technical Advisor for HIV/STI, TB & Viral Hepatitis in the Caribbean.
“The COVID-19 pandemic has presented the opportunity for us to explore new and innovative approaches that are result-oriented,” Rosmond Adams, the PANCAP Director, said.
According to James Guwani, the Director of the UNAIDS Caribbean Sub-Regional Office, it is particularly important to increase testing uptake among men, who are more likely to be diagnosed late. In 2019, 85% of Caribbean women living with HIV were aware of their HIV status, compared to just 72% of men. There is also a need to increase testing coverage among members of key populations, who have reduced access to HIV services due to stigma and discrimination.
The World Health Organization recommends that HIV self-testing be offered as an additional approach to facility- and community-based services. Evidence shows that self-testing is safe and accurate and increases testing uptake among people who may not test otherwise.
Through the campaign, partners are advocating for national policies to include a communication package with information to link testers to HIV prevention and treatment services, as well as minimum standards for the procurement and distribution of HIV self-testing kits in the private and public sectors.
“We strongly believe that HIV self-testing can help close the gap on the first 90. It can be targeted to individuals not being reached by existing HIV testing services, particularly those populations with low testing coverage and at high risk of HIV. It’s not a replacement for all testing services, but it should be included in the toolbox,” said Victoria Nibarger, the Caribbean Regional Programme Coordinator for the United States President’s Emergency Plan for AIDS Relief (PEPFAR).
Under a Global Fund to Fight AIDS, Tuberculosis and Malaria project for the region, work is under way to conduct a verification and feasibility assessment for the introduction of HIV self-testing across countries. Already Guyana has announced plans to roll out HIV self-testing this year, while several countries have either made a commitment to develop policies or are now in the process of doing so.
UNAIDS is helping to coordinate the campaign in the Caribbean, with a focus on supporting a knowledge management strategy that ensures all stakeholders have the information, messages and tools they need to successfully lobby at the national level. A key priority is ensuring civil society engagement and addressing community concerns about how self-testing policies will be implemented.
While representatives of communities of people living with HIV and key populations endorsed the call for HIV self-testing, they have advised that increased investments are needed in post-test counselling and adherence counselling for the entire HIV response.
Deneen Moore, a Caribbean representative of the International Community of Positive Women, said, “We need to improve peer navigation so that when people test positive they have someone there to help them. We also need more social contracting so that civil society organizations can help reach people who test positive. There is definitely a need for us to be involved in the process.”
The advocacy initiative is jointly endorsed by UNAIDS, PAHO, PANCAP, PEPFAR and the Caribbean Med Labs Foundation.


Feature Story
UNAIDS renews partnership with the African Union for a stronger and more resilient AIDS response in Africa
17 March 2021
17 March 2021 17 March 2021UNAIDS and the African Union have signed a new memorandum of understanding (MoU) to reinforce their partnership and to recommit member states to end AIDS through the Catalytic Framework to End AIDS, TB and Eliminate Malaria in Africa by 2030.
The MoU commits partners to work towards addressing the socioeconomic and political impact of HIV in Africa and accelerate the goal of reaching universal health coverage to take AIDS out of isolation. It will pave the way for more resilient, agile and inclusive health systems in Africa.
“The renewed MoU between the African Union and UNAIDS opens new windows of cooperation and new opportunities for ending AIDS in Africa. We need to deliver on this promise—it is doable,” said Amira Elfadil Mohammed Elfadil, Commissioner for the Department of Health, Humanitarian Affairs and Social Development, at the signing ceremony.
The Department of Health, Humanitarian Affairs and Social Development, formerly known as the Department of Social Affairs, will coordinate African Union Commission departments and organs to ensure that HIV remains a continental priority and is integrated into the broader development, human rights, humanitarian and peace and security agenda of the African Union.
“I am delighted to sign the renewed MoU with the African Union,” said UNAIDS Executive Director, Winnie Byanyima. “The African Union is one of UNAIDS’ most important partners. I look forward to reinforcing our relationship to put communities at the centre of the response to HIV, address other health challenges such as COVID-19 and reduce inequalities that increase people’s vulnerability.”
This year is a pivotal year as United Nations Member States are expected to recommit to the HIV response with the adoption of a new political declaration in June. The partnership agreement with the African Union is being signed as the continent grapples with overburdened and insufficiently financed health systems in the face of the COVID-19 pandemic.
Region/country
- West and Central Africa
- Benin
- Burkina Faso
- Burundi
- Cameroon
- Cape Verde
- Central African Republic
- Chad
- Congo
- Côte d'Ivoire
- Democratic Republic of the Congo
- Equatorial Guinea
- Gabon
- Gambia
- Ghana
- Guinea-Bissau
- Guinea
- Liberia
- Mali
- Mauritania
- Niger
- Nigeria
- Sao Tome and Principe
- Senegal
- Sierra Leone
- Togo
- Middle East and North Africa
- Afghanistan
- Algeria
- Bahrain
- Djibouti
- Egypt
- Iraq
- Islamic Republic of Iran
- Jordan
- Kuwait
- Lebanon
- Libya
- Morocco
- Oman
- Qatar
- Saudi Arabia
- Somalia
- Sudan
- Syrian Arab Republic
- Tunisia
- United Arab Emirates
- Yemen
- Eastern and Southern Africa
- Angola
- Botswana
- Comoros
- Eritrea
- Ethiopia
- Kenya
- Lesotho
- Madagascar
- Malawi
- Mauritius
- Mozambique
- Namibia
- Rwanda
- Seychelles
- South Africa
- South Sudan
- Eswatini
- Uganda
- United Republic of Tanzania
- Zambia
- Zimbabwe
Related


Feature Story
Stranded in Nepal without HIV medicine
15 March 2021
15 March 2021 15 March 2021Wang Tang (not his real name) had never been to Nepal before, but at the end of March 2020 it was one of the few countries that had not closed its borders with China. Since he was desperate to get away from Beijing after having had to stay at home for months after the coronavirus outbreak spread throughout China, he bought a ticket.
But days after he arrived, while he was staying in Pokhara, the fourth stop on his trip, the local government announced that the city would be shut down. He heard that the lockdown would not last longer than a month.
As someone who is living with HIV, he had brought along enough HIV treatment to last for a month. However, he soon learned that the re-opening of the city was to be postponed, which meant that he was at risk of running out of the medicine he needed to take regularly in order to suppress his HIV viral load and stay healthy.
Mr Wang swallowed hard while counting the remaining tablets. He had no idea how to get more.
As the lockdown dragged on, it seemed that no end was in sight. Mr Wang started to take his medicine every other day so that his supply would last a little bit longer.
He contacted his friends back at home, hoping that they could send medicine to Nepal, but they couldn’t. The country was under lockdown—nothing could be imported.
Then, Mr Wang contacted his friend Mu-Mu, the head of Beijing Red Pomegranate, a nongovernmental organization providing volunteer services for people living with HIV. It was with Mu-Mu’s help that Mr Wang learned how to obtain HIV treatment after he was diagnosed as living with HIV. Having known each other for many years, Mu-Mu had the trust of his friend. Mu-Mu contacted the UNAIDS Country Office for China to see if it was possible to deliver medicines to Mr Wang. A UNAIDS staff member quickly got in touch with the UNAIDS Country Office for Nepal.
Everything happened so quickly that Mr Wang was shocked when he received a message from Priti Acharya, who works for AHF Nepal and had been contacted by the UNAIDS Nepal office, saying that she would bring the medicine to him.
The next day, Ms Acharya rode her motorbike for 15 km on a dusty road before reaching the place where she would meet Mr Wang. When he came down from the mountains to meet her, Ms Acharya, drenched in sweat, was waiting under the midday sun.
“I was so happy and thankful for her hard work. She gave me a sunny Nepalese smile in return, as well as detailed instructions on the medicine’s dosage,” said Mr Wang.
They took a photograph together, then Mr Wang watched Ms Acharya as she left on her motorbike. Her image, disappearing in the distance, is carved into his memory. To attend the five-minute meeting, Ms Acharya had to ride a round trip of more than 30 km.
“For half a month or so, I had been suffering from pain and anxiety almost every day due to the lack of medication and the loneliness of being in a foreign country on my own. I could not believe that I got the HIV medicine in such a short time,” said Mr Wang. After the trip, he wrote to thank Ms Acharya, explaining how important the medicine he now had in his hand was: “it’s life-saving.”
At the end of his stay in Nepal, Mr Wang wanted to do something for UNAIDS. As he is an experienced photographer, he volunteered to carry out a photo shoot for UNAIDS’ Nepal office.
The subject he chose was former soccer player Gopal Shrestha, the face of an HIV charity in Nepal and the first person living with HIV to reach the summit of Mount Everest. After his HIV diagnosis in 1994, Mr Shrestha launched the Step-Up Campaign and spent many years climbing mountains worldwide, hoping to give strength and hope to people living with HIV.
In 2019, Mr Shrestha reached the peak of the world’s highest mountain, Mount Everest, recording a historic breakthrough for people living with HIV. “If 28 000 people have already climbed Mount Everest, why can’t I?" he said. “By climbing the highest mountain in the world, I want to prove that we are no different from anyone else and that we can all make a difference.”
“The moment I saw him, I could tell he was a sophisticated man,” said Mr Wang. Without instructions, Mr Shrestha posed naturally in front of the camera. He displayed confidence and charm. His eyes, content and clear, reflected nature’s beauty. “The eyes surely are the window to the soul,” Mr Wang said.
Mr Wang is looking forward to his next trip to Nepal. After the pandemic, Pokhara’s lakeside will be flooded with tourists, and he looks forward to seeing the mountain town bustling with people like it used to.
Our work


Feature Story
Addressing inequalities can decrease HIV prevalence
15 March 2021
15 March 2021 15 March 2021The gaps in HIV responses and resulting HIV infections and AIDS-related deaths lie upon faultlines of inequality.
Data from 46 countries in sub-Saharan Africa show a positive relationship between HIV prevalence and income disparity. After controlling for education, gender inequality and income per capita, a one-point increase in a country’s 20:20 ratio—which compares how much richer the top 20% of a given population is to the bottom 20% of that population—corresponds to a two-point increase in HIV prevalence.
HIV prevalence and income inequality, sub-Saharan African countries, 2019
Our work
Related


Feature Story
Monitoring HIV/TB services in the Democratic Republic of the Congo
16 March 2021
16 March 2021 16 March 2021UCOP+, the Congolese Union of Organizations of People Living with HIV, through funding and technical support from UNAIDS, set up the Observatory project, designed to collect and analyse data to guide action to improve the quality of HIV services.
“The Observatory, which looks at access to and the quality of HIV and HIV/tuberculosis services, is a community-based initiative. Its main objective is to help the government and civil society define and implement national policies in accordance with international norms and standards,” said Natalie Marini, Human Rights and Gender Adviser at the UNAIDS Country Office for the Democratic Republic of the Congo.
The Observatory was set up following repeated stock-outs of HIV and tuberculosis medicine, requests for payment for services that are supposed to be free, the persistence of stigma and discrimination and human rights violations and the long distances that people have to travel to access health care. Three areas are monitored monthly—the availability of services, the quality of care, including the availability of medicine, and accessibility of care.
The initiative shows the importance of collaboration between civil society, health services and donors in the HIV response and has led to an improvement in HIV/tuberculosis services in health facilities. “The Observatory is an indispensable tool that gives us the first clues about supply,” said Aimé Mboyo, director for the National AIDS Control Programme. “It helps us enormously.” The data from the Observatory complements the data of the National Health Information System (SNIS).
Since its launch in 2013, the Observatory has contributed to reducing the cost of access to health care in some health facilities and has anticipated stock-outs and helped to reduce their frequency. The Observatory has also reduced self-stigma by valuing the people who use the services and putting them at the heart of the system. “Before, I didn’t have anything to say about the care offered to me,” said Joséphine Ntumba (not her real name), who is living with HIV. “Now I can give my opinion and make a difference.”
The concept of a “community observatory” has been shown to be a success and is now integrated in the concept note for the Democratic Republic of the Congo of the Global Fund to Fight AIDS, Tuberculosis and Malaria. However, there is still a long way to go—only three out of 23 provincial health departments are covered.
Our work
Region/country


Feature Story
Global Partnership members commemorate Zero Discrimination Day around the world
17 March 2021
17 March 2021 17 March 2021On Zero Discrimination Day this year, governments, civil society organizations and communities highlighted the urgent need to take action to end the inequalities that continue to persist around the world.
Among them were several countries and partners of the Global Partnership for Action to Eliminate all Forms of HIV-Related Stigma and Discrimination (Global Partnership) that commemorated the day by organizing webinars, launching initiatives to accelerate the implementation of commitments to end HIV-related stigma and discrimination or raising awareness about the imperative need to achieve dignity for all.
At the global level, the Global Network of People Living with HIV (GNP+) launched #MoreThan, a global online campaign to celebrate and showcase the diversity of the lives, achievements, interests and dreams of people living with and affected by HIV. And UNAIDS, the United States President’s Emergency Plan for AIDS Relief and the Global Fund to Fight AIDS, Tuberculosis and Malaria organized a webinar to showcase the potential of evidence-informed programmes as well as community-led responses to end HIV-related stigma and discrimination. The event used best practices from countries as diverse as the Democratic Republic of the Congo, Jamaica and Ukraine.
At the country and regional levels, Zero Discrimination Day was marked by a number of initiatives. For example, in western and central Africa, Senegalese artist Coumba Gawlo launched a single to raise awareness of and promote action to respond to HIV in the region, together with fellow artists Wally Seck (Senegal), Djelly Mady Kouyate (Gambia) and Nestor Lendjy (Guinea Bissau).
In Senegal, the Network of People Living with HIV (RNP+) held a dialogue to raise awareness on the impact of HIV-related stigma on women and girls. The dialogue brought together people living with HIV and representatives of women’s movements, key populations, human rights advocates, policymakers and health service providers. The outcomes of the dialogue will be used to inform the advocacy strategy that RNP+ will develop on human rights and gender issues to better respond to the expectations of its members and communities affected by HIV.
Evidence shows that in Senegal women living with HIV face obstacles in accessing reproductive health services, that sex workers face high levels of stigma in health-care settings and that the economic and social vulnerability of women living with HIV is not sufficiently considered in HIV programming. “Discrimination continues to affect women and girls and this is the reason why they are often excluded from the labour market, are isolated in their communities or experience stigma in health centres. Key populations are also historically the target of discrimination in Senegal,” said Soukèye Ndiaye, President of RNP+.
In Côte d’Ivoire, UNAIDS, in collaboration with the Programme National de Lutte contre le Sida, the Alliance Côte d’Ivoire, Enda Santé Côte d’Ivoire and Ligue Ivoirienne des Droits de l’Homme, presented the Global Partnership and its added value to representatives of the Ministry of Health and the Ministry of justice, as well as to civil society partners. The meeting led to a report that will inform Côte d’Ivoire’s strategy to eliminate stigma and discrimination.
In the Central African Republic, which was the first country to join the Global Partnership, the Minister of Health and Population, Pierre Somse, above, issued a declaration recalling the government’s commitment to non-discrimination and equality. “It is only by addressing inequalities that we can achieve the Sustainable Development Goals, including those related to well-being and health for all,” said Mr Somse.
Other events in the Central African Republic included a civil society consultation to identify priorities for eliminating stigma and discrimination and a round-table discussion on a radio show to highlight that stigma and discrimination is a barrier to people taking up HIV prevention, treatment, care and support services. Dedicated trainings on the National Charter for Quality of Care and Patients’ Rights took place for medical staff in two major health-care centres in Bangui. In the Central African Republic, more than 80% of people living with HIV in the country have reported experiencing discrimination or stigma.
In the Islamic Republic of Iran, the country’s new anti-discrimination regulation was disseminated on social media to mark Zero Discrimination Day. In Thailand, UNAIDS, the Ministry of Foreign Affairs and the Ministry of Public Health cosponsored a panel discussion on the Global Partnership to showcase the power of governments, civil society and the United Nations to tackle HIV-related stigma and discrimination in Asia and the Pacific. And in the Republic of Moldova, an updated road map was developed to address the remaining barriers related to stigma and discrimination, gender mainstreaming and equality, considering the commitments made under the National AIDS Program and the Global Partnership.
Finally, on the eve of Zero Discrimination Day, Kazakhstan officially joined the Global Partnership. For Baurzhan Baiserkin, the Director of the Kazakh Scientific Center for Dermatology and Infectious Diseases of the Ministry of Health of Kazakhstan, the initiative will make a positive difference for people living with HIV, prisoners, migrants and other key populations.
“Kazakhstan supports the Global Partnership initiative to eliminate all forms of HIV-related stigma and discrimination. I am confident that it will help to achieve the Sustainable Development Goals,” said Mr Baiserkin.
The Global Partnership for Action to Eliminate All Forms of HIV-Related Stigma and Discrimination is an initiative whose goal is to catalyse and accelerate the implementation of commitments made to end HIV-related stigma and discrimination by United Nations Member States, United Nations agencies, bilateral and international donors, nongovernmental organizations and communities.

Feature Story
Towards 10–10–10 in eastern Europe and central Asia
15 March 2021
15 March 2021 15 March 2021The recent regional launch of the global AIDS report 2020, Prevailing against pandemics by putting people at the centre, in eastern Europe and central Asia provided a platform for the proposal of a joint revision of social and legal enablers in the region to achieve the proposed 2025 targets. UNAIDS Cosponsors, governments and civil society partners presented their views on the issue and the joint action to be taken.
Based on the regional data, the 90–90–90 treatment cascade in the region is far off the targets, having reached only 70–44–41. Lev Zohrabyan, the UNAIDS Strategic Information Adviser for Eastern Europe and Central Asia, noted that one of the reasons for this is late diagnosis: in 2019, 53% of all new HIV cases in the region were registered in the later stages. In his opinion, it shows that testing strategies need revision and require enabling societal conditions.
Societal and service enablers have been given prominence in the proposed 2025 targets; in particular, it is outlined in the 10–10–10 targets that:
- Less than 10% of countries have punitive legal and policy environments that deny access to justice.
- Less than 10% of people living with HIV and key populations experience stigma and discrimination.
- Less than 10% of women, girls, people living with HIV and key populations experience gender inequality and violence.
Achieving these goals includes having enabling laws, policies and public education campaigns that dispel the stigma and discrimination that still surrounds HIV, empower women and girls to claim their sexual and reproductive health and rights and end the marginalization of people at higher risk of HIV infection.
“Interventions in these areas create conditions for people to be more active in HIV testing, seek help and start antiretroviral therapy immediately upon diagnosis, adhere to a treatment regimen or proactively seek HIV prevention services, including pre-exposure prophylaxis,” said Mr Zohrabyan.
Rosemary Kumwenda, the Regional HIV/Health Team Leader at the United Nations Development Programme Istanbul Regional Hub, presented an analysis of the legislation in the eastern Europe and central Asia region on the criminalization of HIV and key populations, noting that the situation in the region remains unfavourable for an effective HIV response. The criminal codes have changed in many countries, but discriminatory laws are changing very slowly. Although many countries revisited their legislation regarding HIV exposure, HIV transmission is criminalized in virtually every country in the region. The Russian Federation and Belarus remain “leaders” in the criminalization of HIV and key populations. Criminal penalties for sex between adult men remain in Uzbekistan and Turkmenistan. The biggest challenge for the region, where more than 48% of new HIV cases are among people who inject drugs, is the criminalization of drug use and possession.
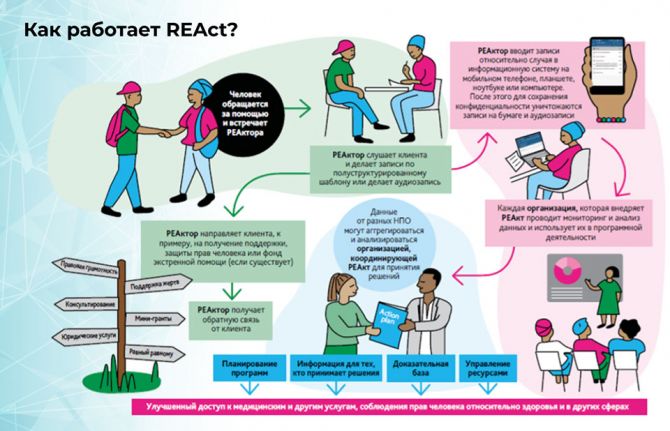
In the presentation An Inventory of Existing Tools for Creating a Favourable Social and Legal Environment in the Eastern Europe and Central Asia Region, given by Tatiana Deshko, the Director of the Department of International Programs, ICF Alliance for Public Health, Ukraine, the ReACT mechanism, which comprehensively works for the rights of key populations, was presented. ReACT (Rights, Evidence, Actions) is the programme’s principle for monitoring violations of rights and is being implemented in 37 cities in seven countries of the region with the support of the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund). Cases of rights violation are registered in a mobile application and then lawyers work with specific cases at the individual level or at the system level of revising legislation. Last year, about 2000 cases were registered. The analysis shows that law enforcement agencies are the primary violators of the rights of key populations in almost all countries, using threats, intimidation, illegal detention and abuse of authority. The health-care system, with denials of medical services, discrimination based on HIV status or disclosure of HIV status, is ranked after law enforcement. “Strategic analysis of cases based on the ReACT-collected data allows not only help for specific people to protect their rights but also formulating recommendations for revising legislation in countries,” said Ms Deshko.
As part of the discussion of the second 10, Alexandra Volgina, the Manager of the Global Partnership for Action to Eliminate All Forms of HIV-Related Stigma and Discrimination, Global Network of People Living with HIV, spoke about the People Living with HIV Stigma Index 2.0 study and the role of the Global Partnership for Action to Eliminate All Forms of HIV-Related Stigma and Discrimination.
Four countries of the region, Kazakhstan, Kyrgyzstan, the Republic of Moldova and Ukraine, have entered the Global Partnership for Action to Eliminate All Forms of HIV-Related Stigma and Discrimination. “If we compile the ReACT system, the Stigma Index and other instruments you’ll get a clear picture of what exactly needs to be done to make a difference. We need to address this issue jointly, all partners together. If we change the situation in the area of stigma and discrimination, we will be able to stop the epidemic,” said Ms Volgina.
An example of such an integrated approach, from data to policies and action, was shared by Evghenii A. Golosceapov, a member of the Equality Council in the Republic of Moldova, the first state institution in the post-Soviet countries dealing with discrimination against various groups.
As part of the Equality Council’s work, studies on the People Living with HIV Stigma Index were carried out, where, through public opinion polls and in-depth interviews, categories of people who are marginalized by society were determined. People living with HIV ranked the second among those categories, after lesbian, gay, bisexual, transgender and intersex people. The Equality Council also uses data from the People Living with HIV Stigma Index, the ReACT registration system and research on the legal environment on HIV.
On this comprehensive basis, more than 70 recommendations on practical steps in the field of legislative changes were developed. These data were used to develop a new national HIV programme and a country proposal to the Global Fund. In addition, the Equality Council considers specific cases of discrimination and complaints (e.g. dismissal due to HIV status) and supports civil society organizations in defending the rights in court. In recent years, the restriction on artificial insemination for people living with HIV has been lifted in the Republic of Moldova, as well as the ban on adoption and guardianship.
All the data collected shape the Roadmap for the Elimination of Discrimination, a government programme in which people living with HIV play a critical role. In the Republic of Moldova, the ScorCard system has also been launched, which allows real-time tracking of the implementation of recommendations and progress towards the adopted targets in reducing stigma and discrimination.
Regional gender gaps in the context of the HIV response were presented by Enkhtsetseg Miyegombo, a Programme Specialist at the UN Women Europe and Central Asia Regional Office.
According to her, the COVID-19 pandemic has largely erased progress in this area and exacerbated existing inequalities: lockdowns disproportionately affected the workload of women who do unpaid domestic work, reduced women’s economic opportunities due to job losses, limited their mobility and increased documented violence against women. These new circumstances were superimposed on existing problems—a lack of awareness about HIV, barriers to discussing safer sex with a partner, revival of patriarchal stereotypes, religious restrictions—as a result of which, women find themselves under growing pressure. Ms Miyegombo highlighted that investment in gender equality programmes is critical to the effectiveness of the regional HIV response.
A study conducted by the Eurasian Women’s Network on AIDS helped to identify the key characteristics of violence and the specifics of organizing assistance to victims of violence in 12 countries of the eastern Europe and central Asia region. The results of the study supplemented the available international data on violence and equipped national civil society organizations with real facts for political advocacy. Elena Rastokina, a specialist in advocacy and community mobilization from the Almaty Model of HIV Epidemic Control project in Kazakhstan, presented successful practices of community-based monitoring in the eastern Europe and central Asia region, concluding that this approach is important as it allows communities to know their rights and barriers and to have systematic data to advocate for systematic change.
Alexander Goliusov, the Director, a.i., of the UNAIDS Regional Support Team for Eastern Europe and Central Asia, stressed that the new 10–10–10 targets are addressing the inequalities that are fuelling the spread of HIV, COVID-19 and other pandemics. “Testing and treatment remain our priorities; however, now our fast track to them lies in combatting inequalities,” he said.
The recording of the launch in Russian and English, along with all presentations and materials, can be found here.
Region/country
- Eastern Europe and Central Asia
- Albania
- Armenia
- Azerbaijan
- Belarus
- Bosnia and Herzegovina
- Bulgaria
- Croatia
- Cyprus
- Czechia
- Estonia
- Georgia
- Hungary
- Kazakhstan
- Kyrgyzstan
- Latvia
- Lithuania
- Montenegro
- Poland
- Republic of Moldova
- Romania
- Russian Federation
- Serbia
- Slovakia
- Slovenia
- Tajikistan
- North Macedonia
- Türkiye
- Turkmenistan
- Ukraine
- Uzbekistan
Related
 Women, HIV, and war: a triple burden
Women, HIV, and war: a triple burden

12 September 2025
 Displacement and HIV: doubly vulnerable in Ukraine
Displacement and HIV: doubly vulnerable in Ukraine

11 August 2025


Feature Story
Call for nominations of people living with HIV, key populations and other affected communities to join the multistakeholder task force for the high-level meeting on HIV
10 March 2021
10 March 2021 10 March 2021The United Nations General Assembly will hold its first high-level meeting on HIV since 2016 on 8–10 June 2021.
In the run-up to the meeting, before the end of April 2021, an interactive multistakeholder hearing will be held with the participation of communities and other stakeholders, who will also participate in other activities before and during the high-level meeting itself.
To ensure the involvement of civil society and ensure an open, transparent and participatory process, UNAIDS is forming, by the end of March, a multistakeholder task force comprised of representatives of civil society and the private sector. The task force will advise UNAIDS on the format, theme and programme of the multistakeholder hearing and will help to identify speakers for the hearing and high-level meeting plenary and panel discussions.
Different constituency networks are asked to use their own networks and selection processes to nominate people to be considered for the task force. UNAIDS and the Programme Coordinating Board nongovernmental organization delegation will select individuals for each of the categories of members:
- One representative openly living with HIV of networks of people living with HIV.
- One representative openly living with HIV of networks of women living with HIV.
- One representative openly living with HIV of networks of young people.
- One representative of each of the key populations (people who use drugs, sex workers, transgender people, gay men and other men who have sex with men, people in prison settings).
- One member of the UNAIDS Programme Coordinating Board nongovernmental organization delegation.
- A representative of a women’s organization, particularly working on sexual and reproductive health and rights.
- A representative of a young’s people organization, particularly working on sexual and reproductive health and rights.
- A representative of the private sector.
- A representative of a faith-based organization.
- A representative of networks or organizations of indigenous people.
- A representative of networks or organizations of people with disabilities.
- A representative of an organization working with tuberculosis and HIV.
“The engagement of people living with HIV, key populations and other priority communities is fundamental for the success of the high-level meeting. Communities have led the way in the HIV response since the beginning and know what is needed to make sure that all people everywhere have what they need to prevent new HIV infections and to ensure that people living with HIV can survive and thrive. The task force represents an important platform for participation in the preparatory phase for the meeting. As the task force is necessarily limited in size, we are particularly interested in nominations of people from networks, who are closely linked across their communities and across regions, to be able to bring a deep and broad perspective. Additional opportunities for people living with HIV, key populations and other affected groups to engage with be made available throughout the lead-up to the high-level meeting,” said Laurel Sprague, UNAIDS Chief/Special Advisor, Community Engagement.
Civil society networks and relevant stakeholders are asked to submit nominations here by 16 March 2021 at 18.00 CET. The call for nominations with detailed information can be accessed here.
Learn more
Submit nominations by 16 March 2021
Related




Feature Story
Putting people at the centre brings good results in Nigeria
05 March 2021
05 March 2021 05 March 2021Nigeria has demonstrated that putting people at the centre of the AIDS response works in advancing HIV service delivery. The 2018 Nigeria HIV/AIDS Indicator and Impact Survey identified 10 states with HIV prevalence above 2%, nine of which had a significant unmet need for HIV treatment and were at risk of being left behind if no action was taken. These states were prioritized by the national AIDS response for concerted action with the help of the United States President’s Emergency Plan for AIDS Relief (PEPFAR) and the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund).
In 2020, while many countries experienced HIV service disruptions, the PEPFAR-supported HIV programme in Nigeria experienced significant growth and exceeded some targets.
“The achievements of Nigeria with PEPFAR and the Global Fund in 2020 have significantly moved the needle towards treatment saturation and advanced the hope of epidemic control and the end of AIDS in these states and the entire country,” said Osagie Ehanire, the Minister of Health of Nigeria.
PEPFAR’s leadership and implementing partners took quick action and fast-tracked their community engagement plans, utilizing existing community network machinery to ensure there were no disruptions in the delivery of HIV services.
“Thanks to PEPFAR and its implementing partners, Nigeria was able to ensure not just continuity of HIV services, but was able to expand the reach, despite the country being locked down due to COVID-19,” said Gambo Aliyu, Director-General of the National AIDS Coordination Agency. “A record 279 000 people living with HIV additionally were put on treatment during this period.”
PEPFAR, together with its implementing partners, developed a people-centred package of services that was informed by data, best practices and community intelligence. The package recognized that one size does not fit all and catered for the unique needs of the various populations served.
Existing community networks, including key population networks and social groups, were consulted to determine the best way to make sure that the services that people need were available to them in their homes, at social gatherings or through support groups—thus minimizing contact with facilities.
Community antiretroviral therapy teams (CART teams) went to hard-to-reach areas around the country as well as to areas effected by COVID-19 lockdowns. Programmes such as a minimum three-month provision of antiretroviral therapy and viral load services were provided at treatment pick-up areas, which not only helped community-led providers to ensure that people stayed on treatment but saw a record number of people living with HIV start on treatment. By the end of 2020, the majority of people on treatment were included in the multimonth dispensing programme, which had a large impact on HIV treatment retention and adherence.
Viral load samples were collected in the communities, sent to laboratories for analysis and the results were then sent to health-care facilities, from where people were notified—this had a positive impact on viral load coverage. Index testing was expanded through community networks, ensuring continuity and safety as well as improvements in testing and case finding.
Results were seen across the entire 90–90–90 cascade as follows:
- An increase in people on HIV treatment of more than 279 000 people living with HIV in 2020, with more than 131 000 people being initiated and retained in care during the fourth quarter alone. PEPFAR Nigeria showed excellent success, accelerating efforts to identify people living with HIV and link them to care, with quarter-on-quarter growth. The growth in people on HIV treatment saw an additional seven states moving towards treatment saturation since the initiation of the “surge” programme approach, where intervention efforts are dramatically scaled up. Key populations represented approximately 25% of this overall growth, as the number of people on treatment among most key populations tripled. Key populations also had a testing yield of more than 10%.
- Improvements in pre-exposure prophylaxis (PrEP) uptake, especially among key populations. The number of people newly initiated on PrEP rose from nearly 2000 in the third quarter of 2020 to nearly 23 000 in the fourth quarter.
- Scale-up of multimonth dispensing from 55% in the first quarter to 94% in the fourth quarter 2020 was a key factor in improved continuity of treatment.
- Improvement in viral load coverage (88%) and suppression (93%) by the third quarter, building on previous successes and maintaining those gains to approach the third 90 target in a little over six quarters.
- PEPFAR’s orphans and vulnerable children programme achieved and exceeded all targets set for the year, including more than a million orphans and vulnerable children served by PEPFAR Nigeria by the end of 2020. Additionally, 98% of those under the age of 18 years in the orphans and vulnerable children programme have a documented HIV status, and approximately 100% of those who tested HIV-positive started treatment.
These results could not have been achieved without the support of community-led organizations. “The Network of People Living with HIV/AIDS in Nigeria (NEPWHAN) wishes to thank PEPFAR for the continuous engagement of our members across the country in the provision of HIV services to people living with HIV,” said Ibrahim Abdulkadir, NEPWHAN National Coordinator. “This has increased retention in care and improved quality of life for people living with HIV, as well as viral suppression among people living with HIV on antiretroviral therapy.”
PEPFAR Nigeria has designed its approach so that it can be owned by the Nigerian people. The National Data Repository and the National Alignment Strategy are key building blocks of a long-term and sustainable public health and health services approach to ending the AIDS epidemic in the country.
“I am profoundly impressed by the progress that PEPFAR Nigeria has made, in collaboration with the Government of Nigeria, partners and allies, to identify, enrol and sustain so many Nigerian people living with HIV on life-saving treatment,” said Bill Paul, the Deputy Coordinator for Program Quality, Office of the United States Global AIDS Coordinator. “Their success in sustaining the effort despite the impact of COVID-19 would not have been possible without a supportive policy environment both in the government and in the United States embassy.”
Based on these accomplishments, Nigeria is well-positioned to accomplish the 95–95–95 targets well in advance of 2030.
At the end of 2020, progress on the 90–90–90 treatment targets was 73–89–78—that is, 73% of people living with HIV had been diagnosed, 89% of those diagnosed were accessing treatment and 78% of those accessing treatment were virally supressed.
The proposed new global AIDS strategy calls for putting people at the centre of the HIV response, empowering communities and closing the gap on inequalities. “Nigeria is poised to be the next HIV turnaround country, after South Africa. We have all the ingredients to make this happen and I commend PEPFAR for working with the government, communities and partners to show the world that this is the only way to end this pandemic, by working with the affected communities,” said Erasmus Morah, the UNAIDS Country Director for Nigeria.


Feature Story
Accelerating and expanding HIV services in the Central African Republic
11 March 2021
11 March 2021 11 March 2021The Central African Republic has made significant progress in its response to HIV over the past four years. New HIV infections continue to decline and the number of people on antiretroviral therapy has increased from less than 25 000 in 2016 to more than 47 000 in 2019.
Despite this progress, the Central African Republic remains far from the 90–90–90 targets. Less than half of the 100 000 people living with HIV in the country have access to treatment and the government estimates that less than 20% of people on treatment have an undetectable viral load. For those who are on treatment, the quality of care is insufficient. Recent studies reveal a very high rate of immunological and therapeutic failure among people living with HIV on treatment.
Various factors contribute to this situation, including hospital-based management, the unavailability of biological monitoring in rural areas, the lack of human and material resources in health facilities and laboratories and the absence of community-based approaches that promote treatment adherence and information. In addition to these system-related factors, since December 2020 the country has faced a resurgence of a political and security crisis, which makes access to treatment difficult.
There is a need to simplify and adapt the cascade of HIV-related services to take into account the preferences and expectations of different groups of people living with HIV while reducing unnecessary burdens on the health system. People-centred care is now the goal of the Central African Republic.
The Central African Republic aims to diversify, accelerate and generalize differentiated services. The Catalytic Initiative promoted by UNAIDS with the financial support of Luxembourg is helping the country to achieve this ambition. A first decisive step has been taken with the organization of a round-table discussion, entitled Catalytic Initiative on Differentiated HIV and Tuberculosis Services. The meeting brought together the Ministry of Health, the Comité National de Lutte contre le SIDA, civil society, people living with HIV, tuberculosis stakeholders, key populations, youth organizations, the United Nations, Médecins Sans Frontières and the French Red Cross.
The participants reviewed the existing pilot programmes of differentiated services in the country and the obstacles related to their implementation. They stressed the urgent need to expand differentiated services, particularly in the current context of the increasing insecurity and humanitarian challenges that make it difficult for people to access HIV and tuberculosis services.
“It is in the current context of the security crisis that the differentiated services approach is most valuable in the Central African Republic,” said Patrick Eba, UNAIDS Country Director for the Central African Republic.
The participants agreed on the activities to be implemented and validated the project implementation schedule to improve the quality of care and biological monitoring of people living with HIV and tuberculosis patients by stimulating the implementation of differentiated services.
“I welcome this opportunity offered by UNAIDS to remove bottlenecks to improve the overall management of HIV,” said Marie-Charlotte Banthas Bata, the Director of Communicable Disease Control at the Ministry of Health and Population, Central African Republic, pictured above, centre.
“Community organizations must be at the centre of the implementation of differentiated approaches,” said Bienvenu Gazalima, the President of the National Network of Associations of People Living with HIV in the Central African Republic
The next key steps will be the documentation of existing differentiated approaches in the country and the development of a national guidance document for scaling them up.





















