

Feature Story
We are off track to meet the 2020 targets on the number of voluntary medical male circumcisions
01 February 2021
01 February 2021 01 February 2021Voluntary medical male circumcision provides lifelong partial protection against female-to- male HIV transmission, reducing heterosexual male vulnerability to HIV infection by approximately 60%.
Voluntary medical male circumcision can also act as an entry point for providing adolescents 15 years and older and adult men in settings with generalized epidemics with broader health packages to improve their health outcomes. When combined with high levels of treatment coverage and viral suppression, evidence shows that the impact of voluntary medical male circumcision is particularly significant.
However, annual circumcisions in the 15 priority countries have remained relatively stable since 2017, falling short of the annual amounts needed to reach the 2020 target of 25 million additional circumcisions since the beginning of 2016.
Our work




Feature Story
Central African Republic: producing HIV estimates in the context of crisis
28 January 2021
28 January 2021 28 January 2021The presidential and legislative elections in the Central African Republic on 27 December 2020 were meant to mark the consolidation of democracy and bolster economic and social recovery in a country tormented by decades of conflict and humanitarian challenges. However, the electoral process has given way to a serious political and military crisis, with the resurgence of armed conflict and a blockade of the main trade and supply routes to the landlocked country by rebel groups.
It is in this context of crisis, and in the aftermath of bloody clashes between armed groups and government forces on the outskirts of the capital, Bangui, that the UNAIDS country office in the Central African Republic hosted a workshop to produce HIV estimates for the country from 18 to 22 January. This important annual exercise is conducted by UNAIDS with national authorities in all regions of the world to provide countries and HIV stakeholders with essential data on the pandemic and the response.
Marie Charlotte Banthas, the Director of Disease Control at the Ministry of Health, oversees HIV and tuberculosis treatment programmes in the Central African Republic. Over the past three years, her services have been at the forefront of efforts to accelerate access to antiretroviral therapy from some 25 000 people on treatment in 2016 to more than 48 000 in June 2020. A former head of monitoring and evaluation at the Ministry of Health, she considers the HIV estimates workshop a priority, despite the deteriorated security situation. “There is no effective response to HIV without data. We need to hold this workshop to provide the country with reliable data to better guide our efforts and improve the care of our patients,” she said.
Civil society also considers HIV estimates as a crucial endeavour. Bertille Zemangui is the President of the National Network of Free Girls, a sex workers’ organization representing key populations. To attend the HIV workshop, Ms Zemangui had to travel long distances each day through sensitive areas. The increased cost of public transport due to the crisis was not enough to discourage Ms Zemangui and other workshop participants. “The current situation is difficult. Everything has become expensive: transportation, food. But we have to be there to make our voice heard because it is sex workers and other key populations that are most affected by HIV in the Central African Republic,” she said. According to data from a 2019 survey, HIV prevalence among sex workers is 15% and 6.5% among gay men and other men who have sex with men, compared to 3.5% among all adults in the country.
For security reasons, the estimates workshop was moved to the UNAIDS office and participation was reduced to national and international experts and members of civil society. “This workshop provided us with a clearer idea of the magnitude and trajectory of the epidemic for 2021. These are essential to measuring our progress towards achieving the 95–95–95 goals,” said Marcel Massanga, the Deputy National Coordinator of the National AIDS Control Council. The workshop also served to identify approaches to improve the quality and completeness of HIV data in the Central African Republic. Thus, the participants agreed on the need to integrate HIV data into the District Health Information System 2 (DHIS2) platform with a view to strengthening the health system.
There are concerns that the volatile security situation could jeopardize the Central African Republic’s efforts to accelerate its HIV response. In 2020, the country launched an ambitious National HIV Strategic Plan 2021–2025, which aims to eliminate discrimination, halve new HIV infections and ensure that 95% of people living with HIV access antiretroviral therapy by 2025. “It will not be possible to achieve these ambitious goals without peace and stability. Already we have information that in several areas people living with HIV have fled into the bush and are without treatment. We must quickly implement contingency plans to respond to these emergencies,” said Patrick Eba, the UNAIDS Country Director for the Central African Republic.
Our work
Region/country




Feature Story
Hand sanitizer donated by Reckitt Benckiser to people living with HIV
25 January 2021
25 January 2021 25 January 2021Russian HIV community centres in Moscow, Voronezh, Kaluga, Kursk, Orel and Vladimir have received 35 000 bottles of Dettol hand sanitizer donated as part of an initiative by Reckitt Benckiser. The donation was made in the light of the increasing COVID-19 pandemic in the country and the increase in other viral diseases, and is a joint effort of the Reckitt Benckiser office in the Russian Federation and the UNAIDS Regional Support Team for Eastern Europe and Central Asia. The nongovernmental organizations Medical Volunteers, Volunteers to Help Orphans and Center Plus also partnered in the initiative, distributing the donations to the community centres.
“This is very timely support for people from key populations, those who are at risk and work on the front lines of the fight against both pandemics, HIV and COVID-19, as well as those who do not have an opportunity to take care of themselves on their own,” said Vladimir Mayanovsky, head of Center Plus.
A study conducted by the Central Research Institute of Epidemiology of Rospotrebnadzor (the Federal Service for Surveillance on Consumer Rights Protection and Human Wellbeing), in cooperation with the Treatment Preparedness Coalition with the support of UNAIDS, found that the number of people living with HIV with COVID-19 markers was four times higher than that of HIV-negative respondents. And people living with HIV were two times less likely than HIV-negative respondents to be tested for coronavirus and less often sought medical help, even if they had symptoms.
The study also found that the majority of respondents living with HIV were found to have a higher risk of contracting COVID-19, owing to the significant number of infections in their neighbourhood and their low level of use of personal protective equipment, and underestimated their personal risk of COVID-19 disease. Hand sanitizer can help to protect people from contracting the coronavirus.
“Reckitt Benckiser’s mission is to protect, heal and nurture, creating a cleaner and healthier world. In the countries where we operate, we strive to promote the idea of a responsible attitude to health and consider hygiene to be the basis of a healthy lifestyle. Keeping hands clean is one of the most important simple habits. For Reckitt Benckiser, this is more than a business, it is a contribution to a healthier and happier future,” said Igor Radakovich, the General Director of Reckitt Benckiser Healthcare in the Russian Federation, Ukraine and the Commonwealth of Independent States countries.
“UNAIDS welcomes and supports such initiatives from the private sector in the fight against the colliding epidemics. We are ready for further cooperation with Reckitt Benckiser in the field of health. We share Reckitt Benckiser’s vision given in its slogan for educational initiatives in the Russian Federation, “Your health is your responsibility”, not only in terms of COVID-19 prevention but also HIV prevention by the promotion of condom use,” said Alexander Goliusov, Director, a.i., of the UNAIDS Regional Support Group for Eastern Europe and Central Asia.
Region/country
Related

Feature Story
New guidance on ethical HIV prevention trials published
27 January 2021
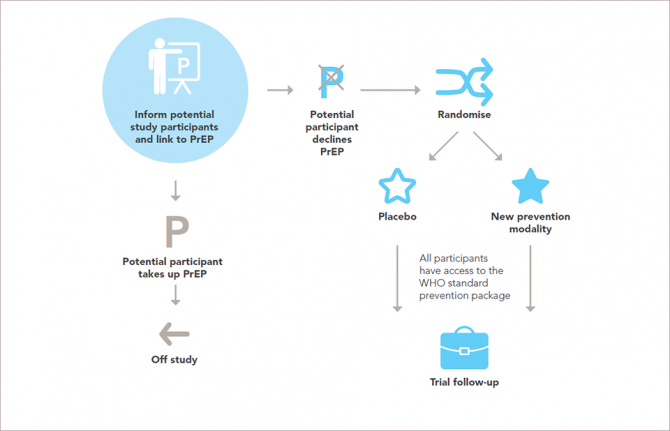
27 January 2021 27 January 2021UNAIDS and the World Health Organization have published updated guidance on ethical considerations in HIV prevention trials. The new guidance is the result of a year-long process that saw more than 80 experts and members of the public give inputs and is published 21 years after the first edition appeared.
“UNAIDS is committed to working with the people and populations affected by HIV, promoting and protecting their rights,” said Peter Godfrey-Faussett, UNAIDS Science Adviser. “This guidance sets out how to carry out ethical trials on HIV prevention while safeguarding the participants’ rights during scientific research and promoting the development of new HIV prevention tools.”
With 1.7 million people becoming newly infected with HIV in 2019, there is still an urgent need to develop new ways of preventing HIV and make them available so that people can protect themselves from the virus. While new methods of preventing HIV have been developed over the past few years, for example pre-exposure prophylaxis, taken orally, in the dapivirine ring or in long-acting cabotegravir injections, the demand for easy-to-use and effective HIV prevention tools remains strong.
However, the need to develop new HIV prevention methods needs to be balanced with the need to protect the people who participate in scientific studies of the safety and efficacy of the prevention tools.
Research on people is governed by a well-established framework of ethical standards. The new report sets out in 14 guidance points the ethical standards for research on HIV prevention and upholds and explains the universal principles of ethics for research involving people in ways that are relevant to the participants and to developments in research for HIV prevention.
“The World Health Organization must ensure that policymakers and health implementers keep ethics at the heart of their decision-making. This collaboration with UNAIDS in convening a wide range of stakeholders for the review is a model for the future development of ethics guidance,” said Soumya Swaminathan, Chief Scientist at the World Health Organization.
The ethical considerations surrounding HIV prevention research are complex. Research must be conducted with the populations for which the new methods might have the most impact—such as key populations and adolescent girls and young women in locations where there is a high incidence of HIV—but members of those populations often live in situations that make them vulnerable to discrimination, incarceration or other harm, which can limit their participation in research and makes ethical research more challenging. The updated guidance seeks to set out how to ethically incorporate the needs of the people who could most benefit from HIV prevention research.
The updated guidance includes a number of key revisions to the previous edition. The importance of community members being involved at all stages of research projects is highlighted—there must be an equal partnership among research teams, trial sponsors, key populations, potential participants and the communities that live in settings where trials are taking place.
The issue of fairness, with an inclusive selection of study populations without arbitrary exclusion on the basis of characteristics such as age, pregnancy, gender identity or drug use, is emphasized. The guidance also underlines contexts of vulnerability—people and groups should not be labelled as vulnerable, but rather the emphasis should be on the social or political contexts in which people live that may render them vulnerable.
That researchers and trial sponsors should, at a minimum, ensure access to the package of HIV prevention methods recommended by the World Health Organization for every participant throughout the trial and follow-up is set out in the updated guidance, along with the need for post-trial access by participants to products that are shown to be effective.
“This revised guidance will support all stakeholders in designing and conducting ethically and scientifically sound HIV prevention trials that advance the AIDS response towards the goal of zero new HIV infections,” added Mr Godfrey-Faussett.
This guidance document is also available in Portuguese.
Our work


Feature Story
Remembering Andrew Mosane, AIDS activist and progressive “radical”
21 January 2021
21 January 2021 21 January 2021South Africa has lost one of its most gutsy social justice and AIDS activists—Andrew Mosane. Mr Mosane died on 15 January 2021, at the age of 45 years, and was laid to rest on 20 January.
He was a seasoned AIDS activist who brought the voice of marginalized people and communities to the centre of the AIDS response. He was known to many in South Africa and around the world as a tireless advocate for human rights.
An openly gay black man living with HIV, Mr Mosane experienced stigma and discrimination, yet he worked tirelessly to address the many challenges facing people living with HIV. Activism was in his blood and he naturally weaved into this the politics of race, class and gender. As part of the Civil Society Forum of the South African National AIDS Council, he represented the sectors of people living with HIV, lesbian, gay, bisexual, transgender and intersex people and sex workers.
Embracing his reputation as a radical, he had an infectious laugh and a sharp intellect, and he conducted himself with sincerity and precision. He was a loud and unapologetic human rights defender. His fellow activists remembered him as “feisty, dedicated, chaotic, lovely, unwavering and passionate.”
Mr Mosane engaged with UNAIDS as he did with networks and institutions across South Africa and beyond, advocating for sexual and reproductive health and rights and encouraging young people in the response to HIV and gender-based violence. He would reach out to UNAIDS, wanting to interrogate and better understand the content of our work and how that reflects the lived experiences of people living with HIV and communities broadly.
UNAIDS Country Director for South Africa, Mbulawa Mugabe, said Mr Mosane had made a lasting contribution to the AIDS response. “He had strong facilitation skills that were honed in the trenches of the Treatment Action Campaign treatment literacy programme—an organization he proudly led and worked for. His talent to make scientific information accessible to communities was the hallmark of his advocacy, and that will be missed,” Mr Mugabe said. “We have lost a giant in social justice and the AIDS movement who touched the lives of so many.”
Mr Mosane engaged with UNAIDS as he did with networks and institutions across South Africa and beyond. Above, with UNAIDS Executive Director Winnie Byanyima.
Region/country


Feature Story
Challenge the stigma, pursue your right to health
20 January 2021
20 January 2021 20 January 2021Adolescent girls and young women must boldly and unapologetically seek sexual and reproductive health and rights information and services. The stigma and harmful gender norms associated with sexual and reproductive health and rights are not going anywhere, says Nyasha Phanisa Sithole, a Zimbabwean sexual and reproductive health and rights leader.
“If you are afraid of stigma, then you will not be able to access these services because we are not going to have a stigma-free environment any time soon,” she says.
Working as a sexual and reproductive health and rights advocate and a regional lead for young women’s advocacy, leadership and training at the Athena Network, Ms Sithole believes everyone has a role to play in changing the status quo and influencing decision-making.
“My story is common. It is that of a 16-year-old adolescent girl who needed access to HIV prevention commodities, but only had condoms available and, in rare cases, pre-exposure prophylaxis,” Ms Sithole says, reflecting on her experience as an adolescent.
Despite this common story, the need for comprehensive HIV, sexual and reproductive health and rights and sexual and gender-based violence services in the eastern and southern African region is critical.
Adolescent girls and young women aged 15–24 years account for 29% of new HIV infections among adults aged 15 years and older in the eastern and southern African region, when they only comprise 10% of the population. This means that there are 3600 new HIV infections per week among adolescent girls and young women in the region, which is more than double that of their male peers (1700 weekly).
The stigma and discrimination that young people face, particularly adolescent girls and young women, to access sexual and reproductive health and rights services creates barriers at various levels, including the individual, interpersonal, community and societal levels.
Furthermore, documented health rights abuses include the unauthorized disclosure of health status, being denied sexual and reproductive health and rights services and related psychological violence.
In 2014, Ms Sithole went undercover as a secret client at a youth-friendly health centre in Harare, Zimbabwe’s capital city, in a district with residential areas and schools. The first person she encountered at the centre was a nosy security guard.
“He asked me: ‘What do you need?’ A health screening, I replied. Then he asked, “Asi wakarumwa?” Meaning, “Have you been bitten?” In Shona, this is street language for someone who has a sexually transmitted infection,” she recalls.
Had she not been well-informed, Ms Sithole says she would have felt scared. “It’s something that can scare you or put you off to say, “It’s just a security guard, why are they mocking me or my situation?” Because imagine if I really had a condition that I wanted to manage, what would happen then?”
Ms Sithole said health-care workers sometimes look at adolescent girls and young women accessing sexual and reproductive health and rights services with disdain and judgement and ask, “How old are you and what do you need the condom or contraception for?”
Considering the stigma attached to accessing sexual and reproductive health and rights services, community organizations play a critical role for adolescent girls and young women. Organizations empower them with sexual and reproductive health and rights information and service referrals.
However, COVID-19 greatly impacted how these organizations work in Zimbabwe, which enforced lockdown restrictions to curb the spread of the virus.
“I think all governments weren’t fair when they clamped down restrictions on each and every organization that was working in communities,” Ms Sithole says, adding that it negatively impacted young people’s access to sexual and reproductive health and rights services.
To mitigate these risks, the Global HIV Prevention Coalition, co-convened by UNAIDS and the United Nations Population Fund, came on board to provide financial and technical support to the Athena Network in 10 countries, including Zimbabwe, to establish What Girls Want focal people in each country. During the COVID-19 pandemic, the focal people, who are adolescent girls and young women, mobilized their peers to conduct dialogues via WhatsApp to discuss the issues they face and seek peer support.
Ms Sithole says governments should invest in policy change and development to create an enabling environment where adolescent girls and young women can access sexual and reproductive health and rights and HIV information and services.
Despite the stigma and discrimination attached to seeking sexual and reproductive health and rights services, Ms Sithole says adolescent girls and young women should realize their power and use their agency to get what they need.
“Think about your life because your life is more important than anything else. So, no matter what happens, if you know there is a service you can access, go for it,” she advises.
Region/country
Related


Feature Story
The road to PrEP in Guyana
19 January 2021
19 January 2021 19 January 2021This year, Guyana will roll out a comprehensive plan for pre-exposure prophylaxis (PrEP). The Guyana Minister of Health, Frank Anthony, announced that the national strategy will be implemented in collaboration with clinics across the country and nongovernmental organizations.
“We want to expand to ensure anyone who is at risk for HIV would have access,” Mr Anthony said. “We believe that with a comprehensive programme for PrEP we can prevent many infections.”
This move marks the culmination of years of advocacy and partial PrEP implementation. The existing PrEP policy is a programme for serodiscordant partners only, so couples in which just one person is living with HIV have been able to access PrEP through the public health-care system to avoid transmission to the HIV-negative partner.
Since 2015, the World Health Organization has recommended that “people at substantial risk of HIV infection” should be offered PrEP. Several countries have prioritized key populations, including gay men and other men who have sex with men, sex workers and transgender people, for PrEP programming. In Guyana, those groups also have higher HIV prevalence: 8% for transgender women, 6% for sex workers and 5% for gay men and other men who have sex with men.
Last year, Guyana’s Society against Sexual Orientation Discrimination (SASOD Guyana) moved from calling for a more inclusive PrEP programme to offering the service itself. The group teamed with the Midway Specialty Care Centre to fill this gap in the country’s HIV prevention response.
“We want combination prevention to take the front burner,” said Joel Simpson, the SASOD Guyana Managing Director. Through this private sector/civil society partnership, for the first time people in Guyana from any population group were able to elect to initiate PrEP. The medicine was sold to clients at cost price and those accessing the service through the nongovernmental organizations paid no consultation fees.
A 2018 SASOD Guyana assessment of gay men and other men who have sex with men and transgender people supported by the International HIV and AIDS Alliance (now called Frontline AIDS) found that, when sensitized, there was a high level of interest in taking PrEP. However, just around 60% of focus group participants were willing to pay to do so.
“We need politicians and technical people to base decisions on science and research. At times we have encountered a moralistic approach to setting public policy,” Mr Simpson reflected. “It’s not about whether you belong to a particular population group. It’s about responding to reality and lowering risk.”
Guyana’s HIV programme results are among the Caribbean’s best. The country surpassed the 2020 testing target, with 94% of people living with HIV diagnosed in 2019. Seventy-three per cent of people who knew their status were on treatment. Of those, 87% were virally suppressed. Over the past 20 years, new HIV infections have been reduced by half in the South American nation.
“HIV treatment has come a long way, and not just for people living with HIV. To close the gaps and ensure that no one is left behind it is critical that best practices for prevention and treatment are implemented fully,” said Michel de Groulard, UNAIDS Country Director, a.i., for Guyana and Suriname. “This is why we are pleased about the direction the Health Ministry is taking this year to ensure that PrEP is made available to all who need it. We have the tools to end AIDS. Now we must use them.”
Region/country

Feature Story
Modelling shows the value of favourable societal environments
19 January 2021
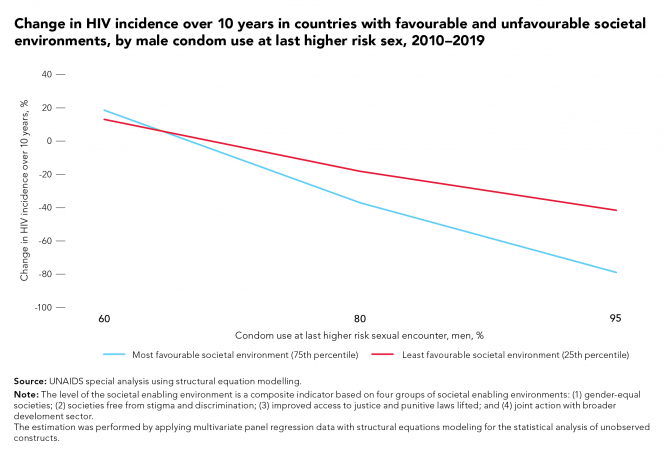
19 January 2021 19 January 2021UNAIDS has proposed a new set of bold, ambitious but achievable HIV targets for 2025. Modelling has shown that if the targets promoting favourable societal environments are met, 440 000 AIDS-related deaths would be averted and 2.6 million additional new HIV infections would be prevented. Related modelling has also shown that countries with more enabling societal and legal environments—defined as societies that are gender-equal, free from stigma and discrimination, and with improved access to justice where punitive laws have been lifted and where joint action is taken with the broader development sector—had stronger positive correlations between HIV service coverage and HIV impacts.
For example, countries with better societal enabling environments are associated with bigger declines in HIV incidence over the past 10 years than countries with worse enabling environments having the same level of condom use by men at the last high-risk sex encounter.
Lower levels of AIDS-related mortality among people living with HIV occur in the countries with the most favourable societal environments, compared to countries with the least favourable societal environments at varying levels of antiretroviral therapy.
Related information


Feature Story
Vulnerability mapping to help sex workers in Bangladesh and Myanmar
12 January 2021
12 January 2021 12 January 2021Warm smiles greet Lily as she approaches her first stop of the day—one of the 11 brothels scattered across the country that Lily, the President of the Bangladesh Sex Worker Network, visits quarterly to check in with the women and see what assistance they need. Though her visits have been limited in recent months due to movement restrictions to curb the spread of COVID-19, Lily knows well enough that those smiles are a brave front for the troubling times that her peers have experienced.
“I see the sex workers as my sisters—I feel their happiness and pain and I try my best to solve any issue they face,” Lily said. During the COVID-19 pandemic, Lily and the 29 community-based organizations serving sex workers in the country have struggled to respond to the increased calls for support. In March, government countrywide movement restrictions meant that sex workers could no longer have clients, leaving most of them without a source of income and unable to provide for themselves or their families.
“Sex workers’ children faced challenges during the COVID situation because their mothers couldn’t arrange to provide them with food. When we [the Bangladesh Sex Worker Network] learned about this issue, we reached out to many organizations and the private sector for assistance,” explained Lily. Responding to the call to action, the network mobilized funds to support 2100 sex workers across the country. Community-led support in Bangladesh has also garnered global recognition. Most recently, a former sex worker, Rina Akter, was recognized by the BBC for her efforts, and those of her team of helpers, to serve 400 meals a week to sex workers in need.
“While a few sex workers had savings, most could not provide for themselves,” said Rahat Ara Nur, Technical Officer for the United Nations Population Fund in Bangladesh. “Through the United Nations Population Fund, we provided sex workers with COVID-19 prevention commodities, such as masks and handwashing materials, and we also developed public service announcements which were aired on community radio to ensure we raised awareness about COVID-19 precautionary measures among the community."
With the closure of entertainment venues, a classification that includes brothels, some sex workers have resorted to street-based sex work, which increases the risk of violence, condom-less sex and no pay or low pay.
Sex workers are also experiencing increasing vulnerability to gender-based violence. Without a source of income, conflicts about finances arise, and sex worker networks report that their members have experienced abuse at the hands of their spouses, partners and brothel owners.
Some sex workers report that they have become homeless because the brothels have been closed, or in some cases the residents were evicted because rent could not be paid. Many sex workers cite stigma and discrimination as a barrier for other forms of employment. Health outreach services that once provided brothels with sexual and reproductive health services, including HIV testing and prevention, have been suspended due to travel restrictions.
Bangladesh, October 2019. Credit: UNFPA Bangladesh/Naymuzzaman Prince
These developments are not unique to Bangladesh, however. Throughout the Asia–Pacific region, national and regional networks of sex workers are reporting that the COVID-19 outbreak has exacerbated the inequalities faced by sex workers, and many are either not eligible or excluded from social protection services.
“There is no government support specifically targeting sex workers. There is support for the general public, particularly those that are low income, but sex workers are not eligible for these social protections because they work in the informal economy,” said Hnin Hnin Yu, the Chairperson of Sex Workers in Myanmar (SWiM), a nongovernmental advocacy group for sex workers’ rights.
Additionally, many sex workers are migrants (international or internal) and lack the necessary papers or registration with local authorities to access the government’s support. Eligibility criteria for social support, such as documentation of income, proof of residence, national identification, contribution to existing social protection schemes and filing taxes, are all reasons given for excluding sex workers from government support. An online consultation of female sex workers from across the country, organized by UNAIDS and SWiM, revealed that apart from limited funds from humanitarian actors, none of the sex workers had received social support.
“When Global Fund to Fight AIDS, Tuberculosis and Malaria assistance for COVID-19 was allocated, funds for people living with HIV included the most vulnerable sex workers to receive food provisions,” said Mr Myo, Community Support Adviser for UNAIDS in Myanmar. “However, we recognized that this was an ad hoc solution that reached a small portion of the vulnerable population and there is a need for more sustainable support, such as social protection, for sex workers.”
It has become clear that focused support for sex workers must be prioritized. Recognizing that more needs to be known about the gaps in social protection for sex workers, UNAIDS in collaboration with the United Nations Population Fund and the World Food Programme are exploring the possibility of conducting a needs assessment and vulnerability mapping initiative of female sex workers during the COVID-19 pandemic. Data from the community-led mapping initiative will be used to inform programming for livelihood support, food security, improved access to antiretroviral therapy, sexual and reproductive health services and gender-based violence prevention and response services.
Commenting on the prospects of the United Nations agencies joining forces to coordinate a vulnerability mapping exercise with sex worker networks, Ms Nur expressed excitement about how this advocacy tool will not only help to identify the challenges that sex workers face during the COVID-19 outbreak, but it would also catalyse further work to mobilize resources for programmes and address injustices that pre-date the COVID-19 pandemic.
Hnin Hnin Yu cites discrimination and harassment from police as a long-standing challenge facing sex workers’ rights. During the COVID-19 outbreak, communities have reported increased police surveillance, harassment, including physical violence, and demands to pay fees to conduct sex work. In response, SWiM provides community-led, peer-to-peer legal aid for sex workers who have been arrested, educating them about their rights.
For those working closely with community-led organizations it has been inspiring to see that although sex worker networks and the sex workers they represent have seen challenges all around them, they have done their best to support their peers. There is hope that the data gathered in a vulnerability mapping exercise would not only generate the evidence needed to advocate for expanding the reach of social protection and humanitarian response services to be inclusive of sex workers, but could also inform the scale-up of community-led programming.
Our work
Region/country




Feature Story
First-ever Jamaica transgender strategy looks beyond health
08 January 2021
08 January 2021 08 January 2021Imagine using a health-care system that has no concept of you as a person, or of your unique needs. Nurses might not ask important questions. Doctors might overlook the solutions you really require. You might feel unwelcome.
That has always been the reality for transgender people in Jamaica. A new strategy seeks to change this.
With support from UNAIDS and the United Nations Population Fund (UNFPA), TransWave Jamaica has launched the Trans and Gender Non-Conforming National Health Strategy, the first of its kind in the English-speaking Caribbean. The five-year plan is a rights-based road map for how the health and well-being of transgender people can be advanced. It moves beyond recommendations for the health-care system to the structural and societal changes necessary to achieve equitable access to services and opportunities for the transgender community.
“Too many transgender people stay home and suffer or change who they are to access public health-care spaces,” explained TransWave Associate Director of Policy and Advocacy, Renae Green. “We need improvement to basic services, including psychosocial support. And we need transgender people to be able to access public health services as their authentic selves.”
Through the Unified Budget, Results and Accountability Framework Country Envelope for Jamaica, UNAIDS collaborated with UNFPA to support a robust year-long process of research, community engagement and strategy development, including a monitoring and evaluation framework. The strategy development process was informed by a multisectorial steering committee composed of civil society organizations, international cooperation partners and government authorities.
HIV is a major priority for the Jamaica transgender community. Around 50% of transgender women participants in two recent studies were living with HIV. But there are other pressing concerns. Two surveys found that around half of transgender respondents were unemployed. One third skip meals. One in ten sells sex to survive. Research conducted in 2020 by TransWave found that half of respondents had been physically assaulted in the past year, with 20% reporting sexual assault. More than 80% had been verbally abused.
“The needs go beyond HIV and health care. Other factors affect people’s ability to be safe, to be adherent or to remain HIV-negative. We should take into account the whole person, not just a part,” said Denise Chevannes-Vogel, HIV and AIDS Officer for the UNFPA Sub-Regional Office for the Caribbean.
“We value the fact that we were able to bring together the community to have a discussion about their needs beyond HIV,” said Ms Green.
The TransWave team led the community needs assessment. Some community requests, such as hormone replacement therapy or gender assignment surgery, are unique. But others are common to all people. They want access to health care and housing, education and employment. And they want to see themselves represented in the civil society spaces where many access care and support.
“We will not reach any AIDS-related targets if we do not prioritize transgender health as a whole. People are dying because of violence, living on the streets, lack of jobs and lack of opportunities. Even the HIV prevention knowledge that most people would acquire through formal education settings is not available to transgender people when they are bullied and forced to drop out. So this process was about reflecting on the impact indicators. What would it take for them to live longer, better lives?” said Ruben Pages, UNAIDS Jamaica’s Community Mobilization Adviser.
But what chance does this comprehensive and forward-thinking strategy have of succeeding in a country famed for its social conservatism? The partners are optimistic. On one hand, the approach calls for longer-term goals, including law reform around issues such as gender identity recognition and decriminalizing sex between same-sex partners. But the strategy is also a practical guide for transgender inclusion in systems and frameworks that are already in place. With targeted action there can be quick wins.
Manoela Manova, the UNAIDS Country Director for Jamaica, said the strategy will help the country accelerate progress to end AIDS.
“Going forward, there will be renewed focus on ensuring that excellent prevention, testing and treatment outcomes are achieved across all communities, especially key and vulnerable populations,” Ms Manova said. “This is an opportunity to make good on our commitment to leave no one behind.”













