Feature Story
New online resource for mental health services for key populations in Kazakhstan
15 June 2020
15 June 2020 15 June 2020The lockdowns and self-isolations imposed to fight the COVID-19 pandemic have affected everyone, key populations and people living with HIV included. Prolonged isolation and limited contact with family and friends have increased anxiety and depression and impacted quality of life, increasing the need for mental health services.
To respond to this need, an online platform that offers psychological services and support for people from key populations has been launched in Kazakhstan. On it, people can get answers to questions related to different aspects of mental health, request professional consultations with psychologists or psychotherapists and receive broader information about health and well-being.
“Anxiety, uncertainty, worries—these feelings are consequences of the quarantine and self-isolation during the coronavirus pandemic. For many people, the time spent in quarantine was difficult. Today, we see a greater need for psychological help and support. It was for this purpose that this platform was created for key populations,” said Nikolay Negay, Director-General of the Republican Scientific and Practical Center for Mental Health of the Kazakhstan Ministry of Health.
The platform was developed with the participation of people from community organizations, representatives of key populations and activists.
“During isolation, we supported each other as best we could through social networks, communication by phone, Skype, but there was a need for qualified professional help. We are glad that such assistance has become available, and for free. The resource is informative and answers many questions,” said Oksana Ibragimova, the acting President of the ALE Kazakhstan Union of People Living with HIV.
“An anonymous rapid needs assessment conducted by UNAIDS in Kazakhstan among people living with HIV and key populations found that around 60% of respondents needed psychosocial support during the COVID-19 lockdown. It was therefore decided to find a way to provide reliable information, advice and professional assistance to those who may need it,” said Gabriela Ionascu, UNAIDS Strategic Information Adviser for Central Asia.
The platform was created as an initiate of the Republican Scientific and Practical Center for Mental Health of the Kazakhstan Ministry of Health, with financial support from UNAIDS and technical assistance from the Kazakh Scientific Institute of Dermatology and Infectious Diseases of the Kazakhstan Ministry of Health.
Our work
Region/country
Related
 Women, HIV, and war: a triple burden
Women, HIV, and war: a triple burden

12 September 2025
 Displacement and HIV: doubly vulnerable in Ukraine
Displacement and HIV: doubly vulnerable in Ukraine

11 August 2025


Feature Story
New HIV community group in Guinea fighting COVID-19
12 June 2020
12 June 2020 12 June 2020Communities have always played an important role in the fight against epidemics in Africa. In the response to HIV, community involvement has been illustrated by a key principle: nothing for us without us. Since the beginning of the AIDS response, civil society has been on the front line, demanding access to treatment, calling for respect for human rights and supporting community-led HIV services.
In Guinea, community engagement has resulted in the continuous improvement of HIV programmes and to considerable progress in testing, prevention, treatment adherence and psychosocial support. The promotion and defence of human rights is also central to communities, and community engagement has contributed to tackling stigma and discrimination and to monitoring the quality of services and addressing challenges.
From the lessons learned from the 2013–2016 Ebola outbreak in the country, the need for the active participation of communities, alongside the public, in the COVID-19 response is clear. This is why the National Platform of Civil Society Organizations on HIV and TB (PNOSC-HIV/TB) was recently set up. Established with technical and financial support from UNAIDS and bringing together 28 associations, PNOSC-HIV/TB played a central role in the development of the Ministry of Health’s contingency plan to reduce the impact of COVID-19 on health services, particularly HIV services.
Focusing on populations that include prisoners, people in refugee camps and solidarity cities— places where people with disabilities live—PNOSC-HIV/TB is active in helping to prevent COVID-19, raising awareness about the importance of physical distancing through community mediators, local artists, the media and door-to-door outreach.
Psychosocial help is being given through a hotline run by two networks of people living with HIV, one of which is focusing on key populations. PNOSC-HIV/TB is also working to promote and scale up nationwide the multimonth dispensing strategy for antiretroviral therapy.
“PNOSC-HIV/TB will enable us to speak with one voice, to assert ourselves even more, to organize and strengthen our contribution to defeating COVID-19 and to the elimination of AIDS in Guinea by 2030,” said Mahawa Diallo Sylla, President of PNOSC-HIV/TB.
PNOSC-HIV/TB also participates in the Community Treatment Observatory, which monitors respect for human rights in the context of COVID-19 and reports violations to the government and the National Institute of Human Rights.
“I am impressed by PNOSC-HIV/TB’s willingness to close the gap in terms of their participation in the national response to HIV. I am confident that the momentum and energy generated since its establishment will have a lasting impact on the responses to HIV and COVID-19 in Guinea,” said Dado Sy Kagnassy, UNAIDS Country Director for Guinea.
Our work
Region/country
Related
 Impact of the pause of US foreign assistance in Côte d'Ivoire
Impact of the pause of US foreign assistance in Côte d'Ivoire

19 February 2025


Feature Story
Five UNAIDS country directors taking the lead in the COVID-19 response
11 June 2020
11 June 2020 11 June 2020The experience of the UNAIDS Country Director for El Salvador, Celina Miranda, a trained medical doctor, has been very useful during the COVID-19 outbreak. When the United Nations Resident Coordinator nominated her to be the COVID-19 response team leader within the United Nations in the country, she was honoured.
“I accepted the challenge, since the experience of working at UNAIDS on HIV has given me the skills needed to handle these types of situations,” she said.
To date, she has handled six confirmed COVID-19 cases of United Nations personnel from different agencies. “Some went to hospital, while others self-quarantined, and all are already emerging from the acute stage,” Ms Miranda said.
A main task for COVID-19 coordinators is to determine whether local hospitals could admit and treat United Nations personnel and their dependents. El Salvador was not ready for the pandemic, she said, which added to the pressure.
Ms Miranda, along with four other UNAIDS country directors, has been nominated by the United Nations Country Teams as COVID-19 coordinators in their respective countries.
Vladanka Andreeva in Cambodia, Yafflo Ouattara in Chad, Job Sagbohan in Burkina Faso and Medhin Tsehaiu in Kenya have all felt honoured to take on such a responsibility.
Ms Andreeva explained how in early March the United Nations in Cambodia set up a United Nations Internal COVID-19 Preparedness and Response Team, and she was asked to lead the efforts in ensuring that more than 2500 United Nations staff and their dependents have access to the latest COVID-19 information, treatment, care and support. She developed a contingency plan for the United Nations family and supported the establishment of a medical evacuations process and mental health support services for staff.
Mr Sagbohan, a trained medical epidemiologist who has worked for the World Health Organization during Ebola and yellow fever outbreaks, said he spent a lot of time reassuring employees in order to overcome stress and fear. “Staff were scared, so during the lockdown period I got up to 300 calls a week despite the regular virtual town hall briefings for staff across Burkina Faso.”
He explained that despite UNAIDS’ size and lack of resources compared to other agencies, knowing about infectious diseases has helped greatly. He quickly requested focal points from different organizations and set up a United Nations taskforce against COVID-19. “I have been able to tap into a solid group of motivated people to help me and it has made all the difference.”
For Yafflo Ouattara, the COVID-19 coordinator role suits UNAIDS country directors perfectly. “We are used to getting buy-in from our Cosponsors, so joint teamwork is part of our DNA,” he said. His main task in Chad has been expanding intensive care units and setting up a strong referral system for the management of severe cases. Nearly 7000 United Nations employees and dependents are spread out across the country, some in places where there is no overnight care.
Like others, he also helped out with the national COVID-19 contingency plan to ensure that people living with HIV have access to treatment and care.
He said that the pandemic highlighted gaping holes in the country’s health system. “Not only were key investments in intensive care never made, some of the basics, like gloves, masks, soap, have been missing all along.”
Living in a COVID-19 world means a lot of readjustments. “We have an opportunity to step in and make our voices heard to overhaul systems,” Mr Ouattara said.
Medhin Tsehaiu agrees. She has been proud to see UNAIDS be part of the greater discussion.
“We are present and we are very actively and willingly doing our share,” she said. But she believes that COVID-19 has forever changed how people work.
All the virtual meetings and no travel has meant that people were much more available, so there was non-stop communication, but it was very time-consuming, she explained. “The crisis brought us together, whether we like it or not, and that has required a lot of collaboration,” Ms Tsehaiu said.
Aside from her long list of tasks as a COVID-19 coordinator, she and a few others started the United Nations Kenya solidarity fund. After much back and forth, they opened a bank account where staff can choose to contribute money during a three-month period that will be dispatched to people in need.
“It’s a way for employees to show empathy and support to the Kenyan people during these difficult times,” she said.
Speaking of solidarity, Ms Andreeva said that the pandemic really tested United Nations reform at the country level, not just in terms of responding to the pandemic but also regarding duty-of-care issues. According to a survey in May, 90% of the staff in Cambodia said that the United Nations leadership at the country level is making the right decisions managing the crisis.
During a virtual town hall meeting of 300 United Nations staff members in El Salvador recently, there was also positive feedback. Ms Miranda said she doesn’t ask for accolades or additional thanks. “I just enjoy helping people and seeing them recover, living their lives fully.”
Our work
Related




Feature Story
Peer consultants helping the AIDS response in Kyrgyzstan
10 June 2020
10 June 2020 10 June 2020When the son of Kymbat Toktonalieva (not her real name) was finally diagnosed with HIV after numerous visits to the hospital over many months, it was only the beginning of the fight.
Her husband left her, leaving her to look after their child on her own. She fought for her son and his rights, for justice. She went to court, attended rallies, wrote letters, worked with other like-minded people and helped other women in the same situation.
For the past six years, Ms Toktonalieva has channelled that campaigning zeal into working as a peer consultant in a multidisciplinary team in a family medical centre in Osh, Kyrgyzstan, helping people living with HIV to get services, providing support and motivating them to adhere to their HIV treatment. There are 10 multidisciplinary HIV teams in the country, which were formed by UNAIDS in 2013; they all include a specialist in infectious diseases or a family doctor, a nurse and peer consultants.
The peer consultants come from the same environments and backgrounds as the people who they work with and have faced similar problems. They may be people who are living with HIV or people who have been affected by HIV. They have decided to act, helping themselves and others, often serving as a bridge between the medical workers and people living with HIV.
“Working as a peer consultant has given me an opportunity to help people to overcome their problems, many of which I have come across myself in the past,” said Ms Toktonalieva.
The peer consultants work with the medical staff, directing, prompting, helping, talking and listening. They are trained to be non-judgemental and help people who have recently been diagnosed as HIV-positive to accept their status and to learn to live with the virus.
The role of the peer consultants is being expanded by the COVID-19 pandemic. From the very beginning of the pandemic they were in contact with people living with HIV, delivering medicine to people’s homes so they could stay on treatment during the lockdown, distributing food packages and providing psychological support.
Another peer consultant, Kalmurza Asamidinov, who works in Kyzyl-Kiya, said, “My work brings good, but I can’t say that everything works out perfectly. We work with different people. Some need to be persuaded to adhere to their HIV treatment because they don’t believe in the treatment, while others are tired of taking antiretroviral therapy—we have to find a different approach for everyone. People are increasingly in need of simple human communication. Many clients miss mutual help and the support groups, which we cannot provide during the COVID-19 lockdown.”
The peer consultants working in the 10 multidisciplinary teams each have a different story to tell. Mannap Absamov, one of the peers in the multidisciplinary team in Osh, said, “Initially it was difficult. We were not able to understand the medical staff, and they could not understand us. But slowly we found points of contact. The main thing is that almost simultaneously, both on our side and the doctors’ side, there became a clear understanding that we all have one goal. It is important that their patient and our client go to the medical facility and start getting treatment.”
Both during COVID-19 and after, one thing is certain—peer consultants will continue to play a vital role in bringing HIV services to people living with HIV in Kyrgyzstan.
Our work
Region/country
Related
 Women, HIV, and war: a triple burden
Women, HIV, and war: a triple burden

12 September 2025
 Displacement and HIV: doubly vulnerable in Ukraine
Displacement and HIV: doubly vulnerable in Ukraine

11 August 2025


Feature Story
Targeting sex workers is not the answer
08 June 2020
08 June 2020 08 June 2020When the Government of Cameroon ordered everyone to stay at home as part of the COVID-19 response, Marie-Jeanne Oumarou (not her real name) rushed to buy groceries and to gather her three children and move them the countryside.
With her children in safe hands, she hoped she could still work.
“I didn’t realize how hard it would be during confinement,” she said. “It doesn’t make sense for us sex workers.”
Ms Oumarou has learned the ins and outs of the couloirs—the avenues of small hotels where sex workers work—in Cameroon’s capital city, Yaoundé, over the past 10 years. Abandoned with her young children, she became a sex worker in 2010. She has grown to know the various older women, former sex workers themselves, who she pays to access safe places to work. COVID-19 changed her life overnight, though.
“Hotels closed, clients were rare, the police constantly around, I cannot survive,” she said.
Denise Ngatchou, Executive Director of Horizons Femmes, a nongovernmental organization that helps vulnerable women, said she was shocked to see how sex workers suddenly became a target.
“Police arrested and held women, disclosing zero information,” she said. “We felt powerless because the government had the upper hand with all the COVID-19 measures.”
Rosalie Pasma, a manager at one of the Horizons Femmes drop-in health centres, shrugged her shoulders in agreement during a Skype interview.
“Everything became much more complicated during COVID-19,” she said. “From women missing health check-ups because of transport issues to our legal expert not being able to access the police stations to defend arrested female sex workers, we felt the confinement in more ways than one.”
Ms Ngatchou piped in, saying that there was no reason to give up. Horizons Femmes vowed to stay open. A skeletal staff with condensed hours still provided HIV testing and other services by respecting preventive measures.
“People told us to stop all our on-the-ground awareness visits, but we held on as long as we could, giving coronavirus tips to women so they knew of the potential dangers,” she said.
They also kept handing out masks and started a crowdfunding project to purchase more protective gear. What really bothers Ms Ngatchou is how so many things happened before their eyes and they could do so little.
“Easing laws against sex work and ending arbitrary arrests of sex workers would really make an impact,” she said.
In the end, she believes that chastising sex workers only worsens the situation.
“Don’t you think that if sex workers hide they are more likely to work and infect themselves or become infected than if there was an infrastructure to help them?” she asked.
Reflecting on what she said, she added that this applies to COVID-19 as well as HIV.
In early April, UNAIDS and the Global Network of Sex Work Projects sounded the alarm on the particular hardships and concerns facing sex workers globally. They called for countries to ensure the respect, protection and fulfilment of sex workers’ human rights.
“Authorities have got to understand that we are not promoting sex work, we are promoting good health,” Ms Ngatchou said. “That’s the priority.”
Our work
Region/country
Related


Feature Story
The value of integrating HIV prevention and contraceptive services
05 June 2020
05 June 2020 05 June 2020In 2019, the ECHO trial reminded the world of the very high HIV incidence among women in parts of southern Africa. Those high levels of HIV, and of sexually transmitted infections, were found among women accessing routine contraceptive services.
A new joint report by the World Health Organization (WHO) and UNAIDS sets out the steps needed to improve and integrate HIV prevention and contraceptive services in order to reduce new HIV infections among women.
“We need to reflect on the diverse needs of women, including adolescent girls, women with lower levels of education and key populations, who have often been neglected in contraceptive and broader sexual and reproductive health and rights programming. The new approach means more contraceptive choices, additional HIV prevention choices and complementary community activities beyond facilities,” said Paula Munderi, Coordinator of the Global HIV Prevention Coalition at UNAIDS.
The report clearly states that women at the highest risk of HIV and sexually transmitted infections in southern Africa and women from key populations should be the focus for the most urgent action.
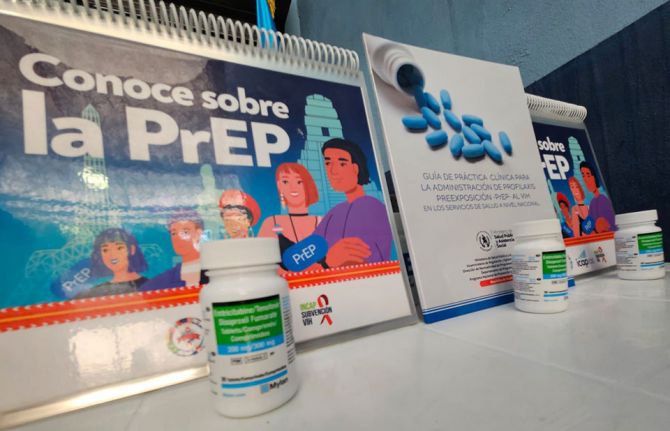
Different approaches in places with different levels of HIV risk are suggested. For example, where there is a high incidence of HIV and sexually transmitted infections, HIV prevention choices, including male and female condoms, and prevention counselling need to be essential elements of contraceptive services and actively promoted. In settings with extremely high HIV incidence in southern Africa, the rapid introduction of pre-exposure prophylaxis (PrEP) within contraceptive services should be considered.
“Sexual and reproductive health and rights and HIV integration have been promoted for more than a decade, yet progress remains limited. Supporting women living with HIV to access contraception in HIV treatment clinics and providing HIV services in contraception services is a critical priority requiring committed funding for concrete action,” said Rachel Baggaley, Unit Head, Testing, Prevention and Populations, Global HIV, Hepatitis and STI programmes at WHO.
In order to understand what women need and want, the report suggests that women be at the centre of decision-making. “HIV prevention and contraceptive choices for women and girls are still not widely available. We need to ensure that the agency and choice of girls and women are promoted by making available a wide range of HIV prevention commodities, ranging from PrEP and microbicides to user-friendly condoms. Women and girls thrive when they are given an opportunity to choose,” said Nyasha Sithole, an advocate for the rights of girls and women from Zimbabwe.
Although people living with HIV who are on antiretroviral therapy and are virally suppressed cannot transmit HIV to their sexual partners, millions of women accessing contraception continue to have unprotected sex with men who do not know their HIV status. As the PopART trial showed, high HIV incidence among young women is also the result of men not accessing treatment. The report proposes concrete steps to strengthen partner prevention, testing and treatment services, including HIV self-tests for men combined with community outreach and gender-transformative prevention approaches.
“Effective integration requires multilayered prevention that can—and should—encompass both sexual and reproductive health and HIV services, including multipurpose prevention technologies. Siloed care, stock-outs and too little input from women themselves are among the long-standing barriers to women’s health care, and COVID-19 exacerbates these difficulties,” said Mitchell Warren, Executive Director of AVAC.
With the physical distancing necessary as a result of the COVID-19 pandemic reducing contact with health services, it will be essential that interactions with health-care providers be optimized through integrating services. “Prevention of HIV and sexually transmitted infections should be the standard of care for contraception information and services provided to women at a high risk of acquiring HIV,” said James Kiarie, Unit Lead, Contraception and Fertility Care, Department of Sexual and Reproductive Health, WHO.

Feature Story
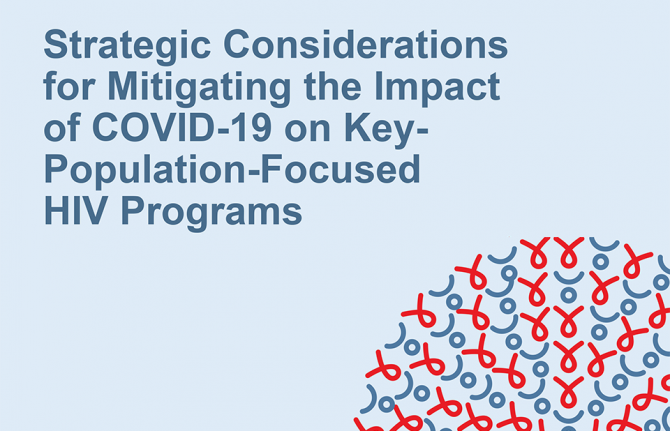
Mitigating the impact of COVID-19 on key populations
04 June 2020
04 June 2020 04 June 2020The COVID-19 pandemic has affected everyone, including key populations at higher risk of HIV. And the gains made against other infectious diseases, including HIV, are at risk of being reversed as a result of disruptions caused by COVID-19. This is the background to a new report published by FHI 360, in collaboration with UNAIDS and the World Health Organization (WHO), which gives advice on how to minimize the impacts of COVID-19 on key populations.
“With a focus on key populations, this guidance complements ongoing efforts to sustain access to HIV prevention services and commodities, sexual health and family planning services, prevention of gender-based violence and HIV counselling, testing and treatment during the COVID-19 pandemic,” said Paula Munderi, Coordinator of the Global HIV Prevention Coalition at UNAIDS. “Preserving essential HIV services for key populations and promoting the safety and well-being of staff and community members during the COVID-19 pandemic is vital to maintaining the hard-fought gains of the AIDS response.”
With practical guidance on how to support the continuation of HIV services for people living with HIV and key populations, the report is aimed at helping the implementers of programmes to carry on their work.
“Key populations are particularly vulnerable to HIV service interruptions and additional harm during the COVID-19 pandemic. We urgently require rights-based solutions that maintain or increase key populations’ access to HIV services while minimizing potential exposure to COVID-19 and promoting individuals’ safety. These must support physical distancing and decongestion of health facilities, but in ways that respond to the current realities of key populations,” said Rose Wilcher, from FHI 360.
The report gives practical suggestions in three main areas.
The first is on protecting providers and community members from COVID-19. HIV services can only continue to be provided during the COVID-19 pandemic if steps are taken to prevent coronavirus infection among programme staff, providers and beneficiaries. Links to COVID-19-related screening and care, and services to support the mental well-being of providers and beneficiaries, can also be given as part of HIV services.
The second area is supporting safe and sustained access to HIV services and commodities. HIV programmes can integrate physical distancing measures, offer virtual consultations and give multimonth dispensing of HIV medicines. Physical peer outreach should be continued where possible.
Monitoring service continuity and improving outcomes is the third area covered by the report. Since there are likely to be service disruptions, HIV programmes will need to adjust their monitoring and evaluation systems in order to allow for regular assessments of continued HIV service delivery and of the impact of COVID-19 on HIV programmes and their beneficiaries. This may require setting up strategic information systems that use physical distancing measures such as virtual data collection and reporting tools.
“The COVID-19 pandemic shouldn’t be used as an excuse to slow momentum in the global response to HIV among key populations. Instead, the pandemic is a time to draw lessons from our work to end AIDS. It is also an opportunity to provide relief to health systems overstretched by COVID-19 by fully funding community-based organizations led by gay and bisexual men, people who use drugs, sex workers and transgender people to ensure improved access to HIV services for key populations,” said George Ayala, Executive Officer of MPact.
“It remains critical to ensure access to HIV prevention, testing and treatment services during COVID-19 and sustain access to life-saving services. This document provides practical guidance and know-how on maintaining essential health services for key populations in these challenging times,” said Annette Verster, the technical lead on key populations at the WHO Department of HIV, Hepatitis and STIs.
The report was developed by FHI 360 as part of the Meeting Targets and Maintaining Epidemic Control (EpiC) project, which is supported by USAID and the United States President’s Emergency Plan for AIDS Relief. UNAIDS, WHO, the Global Fund to Fight AIDS, Tuberculosis and Malaria and partners gave inputs and advice.
Related resources
FHI 360: Five strategies for preserving key population-focused HIV programmes in the era of COVID-19
Global HIV Prevention Coalition
Rights in the time of COVID-19 — Lessons from HIV for an effective, community-led response
Lessons from HIV prevention for preventing COVID-19 in low- and middle-income countries
Condoms and lubricants in the time of COVID-19
Maintaining and prioritizing HIV prevention services in the time of COVID-19
Our work
Related
 Multisectoral resilience to funding cuts in Guatemala
Multisectoral resilience to funding cuts in Guatemala
22 December 2025


Feature Story
Lessons learned from HIV for COVID-19 in Senegal
03 June 2020
03 June 2020 03 June 2020Forty years of responding to the HIV epidemic has provided considerable experience on the importance of a human rights-based approach to all epidemics. UNAIDS spoke to Abdoulaye Ka, who is responsible for human rights issues at the Senegal National AIDS Control Council (known as the CNLS in the country), about the lessons that the CNLS has learned from the response against HIV that can be applied to the fight against COVID-19.
How is Senegal addressing stigma and discrimination during the COVID-19 pandemic?
The experience of the fight against stigma and discrimination related to HIV services has enabled the CNLS to draw the attention of the national COVID-19 management committee and public opinion to the importance of developing communication materials adapted to specific communities. The involvement of affected communities in the definition, implementation and follow-up of COVID-19 programmes has helped to reduce stigma around the disease.
The CNLS Executive Secretary has made several broadcasts to explain the importance of simplifying messages for communities, including to help them develop their own community responses.
The psychosocial care unit in Dakar is also being supported by the CNLS to draw lessons from the experience of HIV and stigma and discrimination in its work against COVID-19.
What measures are being taken to deal with the socioeconomic consequences of COVID-19 in Senegal?
To respond to the socioeconomic impact of COVID-19 on individuals and households, Senegal has deployed an economic and social resilience programme and has earmarked a budget of 1 trillion West African francs (about US$ 1.7 billion) to support the economic sectors most affected by the crisis and to provide food aid to the most vulnerable. A total of 59 billion west African francs (about US$ 100 million) has been earmarked to buy food for one million eligible households.
In particular, the CNLS is partnering with UN Women to increase the resilience of women living with HIV through the provision of food and hygiene kits.
How is the response to COVID-19 in Senegal responding to the specific needs of people living with HIV?
To respond to the needs identified by the national network of people living with HIV, the country is moving to multimonth dispensing of antiretroviral medicines, in accordance with the guidance of the World Health Organization. We are collaborating with service providers and communities in assessing needs in order to avoid stock-outs.
The CNLS has also set up a free telephone hotline for people living with HIV at the Antiretroviral Therapy Treatment Centre of Dakar. It has also set up a WhatsApp network for all antiretroviral therapy care site managers and gives them recommendations on how to adapt the provision of care for people living with HIV, including proceeding with the delivery of at least three months of HIV treatment.
What is the role of community-based organizations today?
Community-based organizations and networks have long been critical to the AIDS response because of their central role in raising awareness, informing, dispelling myths and misinformation and providing services to marginalized and vulnerable populations.
Now more than ever, community actors need to be supported to innovate and be recognized as providers of essential services for HIV and COVID-19.
Community service providers have innovated quickly in the context of COVID-19 in Senegal using appointment systems to prevent too many people being accommodated at the same time in an institution and holding educational sessions virtually.
The CNLS is currently providing logistical support to people living with HIV for the community-based distribution of antiretroviral medicines.
The right to information is a constitutional right in Senegal. What is the role of information in preventing and protecting against epidemics?
The CNLS very quickly developed messages, press releases and banners on social media to draw attention to the preventive steps to be taken against COVID-19, especially for people living with HIV. We also informed people living with HIV in real time regarding the evolving knowledge about HIV and COVID-19.
Information was developed to be expressed in simple terms and to prevent false/fake news that can undermine the use of health services, including vaccination services, that are useful to preserve the health of people, in particular children living with HIV.
Our work
Region/country


Feature Story
Mobilizing COVID-19 relief for transgender sex workers in Guyana and Suriname
02 June 2020
02 June 2020 02 June 2020Twinkle Paule, a transgender activist, migrated from Guyana to the United States of America two years ago. As the COVID-19 crisis deepened, she thought of her “sisters” back home and in neighbouring Suriname. For many of them, sex work is the only option for survival. She knew that the curfew would starve them of an income. And she was worried that some might wind up in trouble with the law if they felt forced to work at night.
After making contact with people on the ground, her concerns were confirmed. She made a personal donation, but knew it was not nearly enough.
“Being somebody who came from those same streets, I knew we had to mobilize to take care of our community. I know about lying down at home and owing a landlord … about getting kicked out because you can’t afford to pay rent,” Ms Paule said.
She collaborated with New York activists Cora Colt and Ceyenne Doroshow, founder of Gays and Lesbians in a Transgender Society (GLITS Inc), to start a GoFundMe campaign. After launching on 12 May they’ve already raised enough money to cover rent subsidies for one month for six transgender sex workers. The money has been forwarded to Guyana Trans United (GTU), the organization for which she worked as a peer educator when in 2015 she left sex work behind.
That she can now use her position of influence to mobilize emergency relief is itself a stunning success. When she migrated, she’d felt herself tottering on the brink of suicide. The emotional weight of exclusion and injustice was bearing down.
One successful asylum claim later, she’s now a full-time communications student at the Borough of Manhattan Community College. She completed her high-school education last year—something she hadn’t been able to do in Guyana. While studying she worked as an outreach officer for GMHC (Gay Men’s Health Crisis).
She seamlessly slipped into advocacy mode, addressing the city council last year about repealing New York State Penal Law § 240.37, a loitering law that is used to target transgender women. She immediately recognized that this was from the same tradition as the vagrancy laws she’d first been victimized by, and later fought against, in Guyana.
Ms Paule is acutely aware of how much her life prospects have changed due to migration.
“It just shows the difference it makes if somebody is given opportunities and the right tools to make other decisions in life. It showed me what I was lacking was adequate resources and the ability to go into an environment without having to worry about discrimination and violence. I am not saying everything is perfect here, but I don’t face the same level of injustice on a daily basis. I was able to access hormone therapy. And to me the most important thing,” she reflected, “is that I was able to go back to school.”
Her mother died when she was a child. Her father moved on with a new family. She was left in the care of his relatives. There wasn’t always enough money for her education. Some weekends she cleaned a church to earn some cash.
But poverty wasn’t the only challenge. Since she was very small she remembered feeling different. She did not have a label for what she felt, but instinctively knew it would not be accepted. At school she strained to stay under the radar. One day her heart skipped when a classmate said she sounded like an “antiman”—a Guyanese derogatory term for a gay person.
Over the years she repeatedly overheard adults in the household agreeing that she should be put out if she turned out to be gay. At 16 years old it happened. A relative spotted her “dancing like a girl” at a party. Now she was homeless.
Ms Paule sought refuge with other transgender women and, like them, used sex work to survive. The burgeoning regional movement to address the needs of vulnerable and marginalized communities had an impact on her life. From the newly formed Guyana Sex Work Coalition she learned about safer sex and accessed safer sex commodities. When some of her peers started going to conferences they found out for the first time that there was a word for their experience. They weren’t “antimen”. They were transgender.
But life on the street was brutal. If someone was robbed or raped they could not report the crime.
“The police tell you plain, “Why are you coming here when you know prostitution and buggery are against the law?”,” she remembered.
She said sometimes rogue police officers threatened to charge them and extort money from them.
Once the police locked up her and other transgender women together with men at the police station and threw condoms into the cell—a green light to the other detainees. She was a teenager at the time.
She accompanied a friend to the police station to make a domestic violence report one day. Instead a policeman told her, “You are involved in buggery. I am locking you up.”
In 2014, a group of them were arrested for sex work in Suriname. Among other indignities, a prison guard forced them to disrobe and squat outside their cell, in the presence of other detainees.
Seven years ago, one of her friends was killed, her body was thrown behind a church. There was no investigation.
Trauma after trauma. It takes its toll.
Even when nothing happens, there is lingering fear. Will I be put out the taxi? Will people insult me on the street? Will I be mistreated because of what I’m wearing?
“The girls take it like it’s their fault,” Ms Paule reflected. “Even in my personal experience I felt people had a right to do me things because I was not behaving in accordance with societal norms.”
Even as she stepped into advocacy, she didn’t feel whole. She attempted suicide once and began having a drink or smoke before turning up to work. Two years ago she was unravelling. Now she’s rallying forces in the service of her community.
Ms Paule credits the work of organizations like the Society against Sexual Orientation Discrimination and GTU for advancing the dialogue around inclusion in Guyana.
“What is still missing is safety and equity for the community,” she insisted. “We need a state response to say, “These people should be taken care of”. The trans community has no jobs, we are bullied out of school, we suffer police brutality. These things are wrong. We need more robust action from our elected officials.”
Our work
Related


Feature Story
Caribbean community organizations call for decisive action to end homophobic abuse and cyberbullying
29 May 2020
29 May 2020 29 May 2020Ulysease Roca Terry was a gay Belizean fashion designer living with HIV. He had recently lost his mother and was coping with depression. Even without a new pandemic, it was a difficult time.
He was arrested for breaching COVID-19 curfew laws in April. While in custody he suffered homophobic slurs and bullying by a police officer. A video of the abuse was posted to social media. He also claimed that he was physically attacked while detained. Days later he died.
This month in the Bahamas, a video circulated on social media of a gender non-conforming woman being beaten by three men hurling homophobic slurs. One man smashed a piece of wood onto her head. Others slapped and punched her. As the video circulated online, some made fun of the victim.
While countries in the Caribbean focus on combatting COVID-19, community organizations have been raising their voices against the casual verbal, physical and emotional abuse that is a feature of life in the region for far too many lesbian, gay, bisexual, transgender and intersex (LGBTI) people. And they are sounding an alarm that this cruelty is increasingly playing out online.
Caleb Orozco of the United Belize Advocacy Movement (UNIBAM) spoke about Mr Roca Terry’s case with a mix of sorrow and defiance. Mr Orozco is used to tough battles. He was the litigant who successfully challenged Belize’s law banning consensual sex between same-sex partners in 2016.
“The police cannot erode public confidence in its law enforcement role by showing disregard for the dignity and rights of individuals who are members of the most vulnerable groups: those with mental health challenges, those living with HIV and those with different sexual orientation,” Mr Orozco said. “It is the responsibility of the police department to enforce the curfew in a manner that is reasonable. Mocking people does not help to build public confidence that the police are there to protect ordinary citizens.”
UNIBAM is calling for a transparent investigation, a review of the autopsy report and action to improve how the police treat members of vulnerable and marginalized communities, particularly in the context of the COVID-19 restrictions.
In Belize, a national dialogue is under way around a proposed Equal Opportunities Bill. A UNAIDS public opinion survey conducted in 2013 found that Belize was among the more tolerant Caribbean countries, with 75% of respondents agreeing that people should not be treated differently based on their sexual orientation. But this incident is a reminder that notwithstanding strides made in social attitudes and the law, pervasive challenges remain around prejudice and the abuse of power.
The Bahamas Organization of LGBTI Affairs has called the attack circulated on social media a hate crime and demanded that the perpetrators be prosecuted.
“Around the world, this kind of hate crime—the targeting of a person with extreme violence because of who they are—is denounced as among the most reprehensible modes of human conduct imaginable,” Rights Bahamas said.
Alexus D’Marco, Executive Director of the Bahamas Organization of LGBTI Affairs, insisted that there must be a broader dialogue and action to address social attitudes.
“What does it say about us as a people that so many consider this a source of humour and entertainment? What are we to think when so many of the culprits are fellow women, who should be standing together in solidarity to oppose the many injustices faced in common as members of an oppressed gender in this society?” Ms D’Marco demanded.
The Bahamas is the only Caribbean country to have decriminalized sex between consenting adults of the same sex by an act of parliament. Still, lots more work needs to be done to bring social attitudes in line with the law. Advocates insist that hate crime legislation must urgently be enacted and enforced.
In both the Bahamas and Belize, state entities have joined civil society to denounce the attacks. The National AIDS Commission, the Office of the Special Envoy for Women and Children and the Ministry of Human Development, Social Transformation and Poverty Alleviation have called for Mr Roca Terry’s case to be thoroughly investigated. In the Bahamas, the Ministry of Social Services and Urban Development called for a swift prosecution to signal zero tolerance by the government and society for gender-based violence.
“Alongside legislative reform and key population programmes, we must continue the social dialogue and law enforcement to create more peaceful and inclusive Caribbean societies for all,” said James Guwani, UNAIDS Director for the Caribbean.