Feature Story
“We cannot provide only HIV services while sex workers are hungry”: Thai community organization steps in
01 June 2020
01 June 2020 01 June 2020When the Thai government ordered the closure of entertainment venues in the country in March, it didn’t just signal an end to pulsating music and rounds of drinks shared with friends. It also signalled the start of difficult times for an estimated 145 000 sex workers living in Thailand.
Initially, Service Workers in Groups (SWING), a Thai national organization providing HIV services and advocating for sex workers’ rights, received requests from sex workers for the most basic of needs—food. As requests began flooding in, it became clear that without a source of income many sex workers were unable to cover the cost of daily expenses, housing and medicine.
“When the COVID-19 outbreak began, nobody was talking about sex workers, and no measures were in place to help them,” said Surang Janyam, Director of SWING.
Spurred by growing concerns about how the outbreak has impacted the lives of sex workers, SWING, in collaboration with Planned Parenthood Association Thailand and Dannok Health and Development Community Volunteers, with support from UNAIDS, launched a community-led rapid assessment of 255 sex workers from Bangkok, Pattaya and Dannok and community-based organizations throughout the country.
The outbreak has had a severe socioeconomic impact on the lives of sex workers, further exacerbated by the lack of social protection measures. According to the findings from the rapid assessment, 91% of respondents became unemployed or lost their source of income following the start of the COVID-19 outbreak. Three quarters of the respondents could not make enough money to cover daily expenses and 66% could no longer cover the cost of housing.
Ms Janyam spoke about the difficulties faced by sex workers and how the priorities for SWING’s work have shifted. “As a sex worker-led organization, we cannot provide only HIV services while sex workers are hungry and lack the basic needs to survive,” she said. She explained that many of the sex workers expressed that they were not eligible for the government assistance of 5000 baht. Answering the call for help, SWING staff have taken to the streets to raise donations and deliver food to sex workers in their network.
Widespread coverage in the media and on personal blogs has catalysed a public conversation about the lack of social protections for sex workers. Ms Janyam also points to donations from local businesses and visits from younger people wanting to help as promising signs of how wider audiences are becoming more engaged on the topic of supporting sex workers in their communities.
The COVID-19 outbreak has also contributed to new challenges for HIV prevention. Fears of COVID-19 have deterred people from visiting clinics to be tested for HIV. Additionally, the rapid assessment findings revealed that almost half of the sex workers surveyed had difficulty accessing sexually transmitted infection screenings. In response to those observations, SWING partnered with a hospital capable of conducting COVID-19 testing, thereby drawing in sex workers interested in being tested for COVID-19 and creating an opportunity to counsel them about HIV tests. These changes in practice show possible synergies in prevention measures for both COVID-19 and HIV prevention and treatment.
“The results from the rapid assessment have proven to be a strong tool for advocacy and decision-making. Stakeholders of the AIDS response have collectively identified and started to implement priority actions as an immediate response to the needs of sex workers during the COVID-19 pandemic,” said Patchara Benjarattanaporn, UNAIDS Country Director for Thailand.
Ms Janyam reflects on what this will mean for SWING’s work and recalls the ways in which sex workers were not afforded the same social safeguards as others—they were forgotten. “We must transform ourselves. Community-led organizations must apply a holistic and comprehensive approach, providing immediate basic needs, integrating a package of prevention for both COVID-19 and HIV health services, as well as mental health support for sex workers,” she said.
She affirms that SWING and other charitable groups will continue to seek donations and provide basic provisions for sex workers, recognizing that the need for assistance will remain long after the situation eases, long after the bars and restaurants have reopened.
Our work
Region/country





Feature Story
“My biggest concern is to get my antiretroviral medicines”: HIV and COVID-19 in Latin America
28 May 2020
28 May 2020 28 May 2020Since the start of the COVID-19 pandemic, Marcela Alcina, of the Latin American and the Caribbean Movement of Positive Women (MLCM+), has received more than 20 calls a day asking for help, either for food, medicine or advice on how to cope with the lockdown.
Yesenia Rodriguez (not her real name) made one of those calls. A Colombian by birth, she lived for more than 24 years in the Bolivarian Republic of Venezuela, but owing to the humanitarian crisis in that country, she had to return to Cali, Colombia, six months ago to access her treatment for HIV.
“There’s eight of us: my four children, my husband, my two grandchildren and me,” she said.
Ms Rodriguez does not have a job and needs help to feed her family and to access antiretroviral medicine. “I came back to Cali only to find myself living another crisis. My biggest concern is to get my antiretroviral medicines, but I don’t have access to health care in Colombia,” she said. “It’s been extremely tough for me and my partner, since we’re both living with HIV. My children and my husband are unemployed. Kids can’t put up with hunger the way we grown-ups do.”
Ms Rodriguez was put in contact with Yani Valencia of the Lila Mujeres Organization, part of the MLCM+ network. She was given a food package for her and her family, and she is being put in contact with someone who is able to ensure that she can access antiretroviral therapy. “I was about to pass out when they brought me these groceries, I was extremely happy.”
UNAIDS is recommending that, especially during the COVID-19 pandemic, people living with HIV keep necessary medical supplies on hand. The World Health Organization HIV treatment guidelines now recommend multimonth dispensing of three months or more of HIV medicines for most people at routine visits. However, according to a recent survey carried out by UNAIDS in Latin America and the Caribbean on the community needs of people living with HIV in the context of the COVID-19 pandemic, only one in 10 people reported having a three-month supply of antiretroviral therapy.
“We have met people who have no access to health care. A colleague of ours in Colombia borrowed a neighbour’s motorcycle to distribute medicines. We notice communities are overlooked quite often, but we must be a part of the answer. We couldn’t wait any longer, we had to do something,” said Ms Alcina.
Communities have played and continue to play a fundamental role in the AIDS response at the local, national and international levels. And now communities are playing a major role in the fight against COVID-19. MLCM+ has developed a network of 850 volunteers working in 17 countries in the region whose aim is to spread solidarity during the COVID-19 pandemic, keeping the focus on people living with HIV.
“We are distributing food and cleaning products, we are making masks that will later be distributed along with antiretroviral therapy, we are teaching people some prevention methods, we are giving condoms away and helping people find shelter in domestic violence situations,” said Ms Alcina.
MLCM+ is working across the region with UNAIDS, UN Women, the United Nations Population Fund and the United Nations Educational, Scientific and Cultural Organization, all of which are offering technical or financial support.
“UNAIDS provides us with resources, specialists and training webinars. The United Nations Educational, Scientific and Cultural Organization, on the other hand, helps us financially. That way, we are putting together a mechanism that intends to support the government’s actions, not replace them,” said Ms Alcina.
“We see how inequalities have become more evident during the COVID-19 pandemic. Inequality, and especially gender inequality, is exacerbated in times of crisis. Women living with HIV must be in the centre of the responses to both HIV and COVID-19, and must not be left behind,” said César Núñez, Director of the UNAIDS Regional Support Team for Latin America and the Caribbean.
Related links
Region/country


Feature Story
Pia Wurtzbach on how she is helping the response to COVID-19
27 May 2020
27 May 2020 27 May 2020Pia Wurtzbach, Miss Universe 2015 and UNAIDS Goodwill Ambassador for Asia and the Pacific, has long been an advocate for the AIDS response in the Philippines and the rest of the region. Recently, however, her work has taken in support for the COVID-19 response, including starting a fundraising effort with the aim of distributing 25 000 face masks to hospitals in Manila and supporting social media campaigns on preventing both COVID-19 and HIV.
UNAIDS spoke to Ms Wurtzbach about her work during this challenging time.
How did you organize the drive to donate face masks to health facilities in Manila?
To begin with, I ordered 5000 masks with my own money to identify an affordable and reputable supplier. I found one and ordered the masks and then delivered them to four hospitals. Once I was ready and confident, I started the fundraising drive, reaching out to the private sector in the Philippines and my network of contacts. So far, I have been able to donate masks to 30 hospitals in Metro Manila. We wanted to deliver masks to other hospitals outside the capital city, but because of the lockdown this hasn’t been possible yet. In addition, I have been able to donate meals to an intensive care unit in one of the hospitals in Metro Manila. Nurses and doctors working in the unit have been living in the hospital and do not go home. With the donations, I feel I am supporting them.
How do you continue to support the response to HIV in your role as a UNAIDS Goodwill Ambassador?
Every day I am in contact with LoveYourself, the civil society organization I volunteer for in the Philippines, to update each other on what is going on and to monitor the needs of people living with HIV. I post information on my social media platforms about HIV and COVID-19 prevention and how to stay healthy. I keep my followers informed of the services provided by LoveYourself to support people living with HIV during the COVID-19 pandemic, such as home delivery of antiretroviral medicines.
What questions do you receive from people living with HIV or from key populations in relation to HIV and COVID-19?
The most popular questions are how to access medicines and whether there are going to be enough refills. It is great that organizations like LoveYourself in the Philippines help people living with HIV to access their medicines. I am really impressed with Vinn (Ronivin Garcia Pagtakhan), the founder of LoveYourself, because he has been using his own car driving around everywhere delivering medicines to people’s homes. He is like a modern-day superhero.
How have you kept motivated to continue your work in these trying times?
I am so blessed because I have a lot of friends in the industry who are nurses too. You will be surprised that my makeup artist is a registered nurse, and there are photographers who are registered nurses. In the Philippines, there are so many nurses that somehow end up doing other careers, but they are all still in the medical field and they know people in the medical field. I hear so many stories from them, and I know these are real stories about what the hospitals are like and about their environment.
Hearing their stories made me feel like I needed to do something. I feel very fortunate that I am able to stay at home. So, I thought to myself, what can I do to make myself useful? This is why I started my donation drive. The medical staff sent me messages of appreciation and even a video of them saying thank you. When I see that the people on the frontline take the time to say thank you, I want to help even more.
The fundraising campaign gave me a sense of mission and purpose. That is what I tell people. If you are at home and you have followers on Instagram, or maybe you are an influencer or a celebrity, or maybe you are just popular in school, use it! Now is the time! We cannot just sit and wait for this to be over. The solution has to come from us.
What do you miss most from your life before the COVID-19 pandemic?
I feel like I took the little things for granted. I took for granted the little commute going to work, I took for granted the travelling, I took for granted how busy I was with my work. I remember before the lockdown I got burnout because I was doing so much work. I was not getting any free days or any weekends—I was working from Monday to Sunday. And I said to myself that I needed some time alone. And then suddenly this all happened. I am just taking the time now to reflect and think about what is really important to me.
I miss everything. I miss being able to walk outside, I miss the traffic, I miss seeing other people. I feel that the lockdown is really giving us time to think about what is important for us. I feel like when we get out of the quarantine and self-isolation, we will know what to prioritize.
How do you spend your leisure now being at home in quarantine?
You know, the good thing about the lockdown is that I have more time for myself. Every day I go to the roof deck of my building to work out, so I bring my yoga mat up there and spend a few hours trying to get some sunlight and exercise. I have a routine every day, and I feel like if you have a little routine, you will feel like your days have direction. When I wake up in the morning, I try to get emails done and some work done. In the afternoon, I will work out. And at night I can bake, or watch television, watch Netflix. So, it is work, sunlight and then “me time”. I feel like this is a nice balance, because it is making yourself productive and taking care of yourself.
What are your next steps after you reach the target of donating 25 000 masks?
It is not set in stone, but my team and I are thinking of ways to help people who need economic support and donate them food. In addition, I would like to focus on social media messages on mental health to give people tips on how to control or manage their anxiety. People are at home and on their phones, so maybe they can read something that will help them manage their stress.
Video
Region/country
- Asia and Pacific
- Australia
- Bangladesh
- Bhutan
- Brunei Darussalam
- Cambodia
- China
- Democratic People's Republic of Korea
- Federated States of Micronesia
- Fiji
- India
- Indonesia
- Islamic Republic of Iran
- Japan
- Kiribati
- Lao People's Democratic Republic
- Malaysia
- Maldives
- Marshall Islands
- Mongolia
- Myanmar
- Nauru
- Nepal
- New Zealand
- Pakistan
- Palau
- Papua New Guinea
- Philippines
- Republic of Korea
- Singapore
- Solomon Islands
- Sri Lanka
- Thailand
- Timor-Leste
- Tonga
- Tuvalu
- Vanuatu
- Viet Nam
- Samoa


Feature Story
“When people are asked to isolate themselves, we also need to make sure that they have food and medicine”
26 May 2020
26 May 2020 26 May 2020When non-essential shops and markets were closed in Senegal in response to the COVID-19 outbreak in the country, and movement between regions in the country was stopped, many people working in the informal sector, including people living with HIV, lost their income. Hunger was dangerously near for many.
Within days, the National Network of Associations of People Living with HIV in Senegal (RNP+) mobilized, setting out to its members the food aid options available from the government for 1 million eligible households and offering advice on how people should prevent themselves from becoming infected by the coronavirus.
“When people are asked to isolate themselves, we also need to make sure they have food and medicine. Communities of people living with HIV help each other to take care of themselves, isolate themselves, access medication when needed and take care of each other’s families,” said Soukèye Ndiaye, the Chairperson of RNP+.
Community leaders and nongovernmental organizations are playing an active role in Senegal in giving out clear and accurate information in order to avoid panic and in combating stigma and discrimination, against both HIV and COVID-19. RNP+ is monitoring the response to COVID-19 as it unfolds, mapping how COVID-19 is affecting the most vulnerable and bringing urgent issues to the attention of the government and service providers.
Advocacy with the National Alliance of Communities for Health and ENDA Santé enabled RNP+ to distributed more than 200 food and hygiene packs to the poorest families of people living with HIV. The UNAIDS country office in the country has stepped in by providing a grant to ensure that the One Family–One Kit programme continues to distribute aid to the people most in need.
RNP+ is also advocating for funding for people living with HIV to help them to travel to health centres, since transport costs have increased, and for financial support for the scaling up of the work of community health workers, who are active in the delivery of antiretroviral therapy.
During the COVID-19 pandemic, ensuring continuity of HIV treatment by distributing multimonth supplies of antiretroviral therapy is vital. Although RNP+ has called on the government for all people living with HIV to get multimonth refills, weaknesses in the supply chain, including inadequate assessments of the needs at some clinics for supplies of antiretroviral therapy and irregular supplies centrally, has meant that not all people who need such supplies are getting them. UNAIDS is supporting the government in tracking orders of antiretroviral medicines and in strengthening the supply chain.
The role of communities, especially communities of the most vulnerable, is critical in the time of COVID-19. “The history of the HIV epidemic has made it clear that the response to an epidemic is only effective if affected communities are fully involved in the response, from its planning through to its implementation and monitoring. Only then can a response be based on the realities and needs of all,” said Demba Kona, the UNAIDS Country Director for Senegal.
Region/country
Related


Feature Story
“We are in this together”: Uganda Young Positives respond to COVID-19
25 May 2020
25 May 2020 25 May 2020Kuraish Mubiru wakes up at dawn every day to get refills of antiretroviral therapy from different health facilities before making deliveries to his peers and other members of the community living with HIV. This has been his routine for the past seven weeks.
Mr Mubiru is the Executive Director of Uganda Young Positives (UYP), a community-based organization that brings together young people living with HIV, mainly from the informal sector. With more than 50 000 registered members, UYP focuses on scaling up HIV prevention, care and support services for its members.
When Yoweri Museveni, the President of Uganda, first addressed the nation on 18 March on the global COVID-19 pandemic, among the measures put in place were restrictions on mass gatherings, the closure of most businesses and the cessation of public transport. Since then, people living with HIV and tuberculosis have found it difficult to access their routine medical care or essential medicine refills.
Following the measures, Mr Mubiru started receiving calls from young people whose livelihoods and HIV treatment were dependent on facilities that had been closed. The impact of the restrictions was beginning to be felt. Young people were no longer able to move to their respective health facilities to access care and treatment nor afford a meal.
Although there have been efforts by health centres and civil society organizations to transport antiretroviral medicines closer to the people, a good number, as reported by the community support groups and health centres, have not received their antiretroviral medicines owing to fear of stigma and discrimination by the community and family members.
“This was a trying time for the community and a huge test of our resilience because our peers needed us more than ever,” said Mr Mubiru. “We had to come out of our comfort zone, act and think fast not to lose all our gains in the national HIV response in the wake of COVID-19.”
Mr Mubiru volunteered to support his fellow peers to access HIV treatment using his own car. In the beginning, he used his own resources to fuel his car and purchase food, but he soon ran out of money.
Initially, one of his biggest challenges was being able to fuel his car to continue with the daily refills, but the further tightening of restrictions on private transport meant that Mr Mubiru could not continue with deliveries. Through the support of UNAIDS, the Infectious Disease Institute and the Ministry of Health, he obtained a permit granting him permission to enable him to continue supporting his community.
During one of his routine deliveries, Mr Mubiru’s car was impounded by the police for more than four hours and he was made to wait. It took the involvement of the police leadership to have the car and Mr Mubiru released. On many occasions, he has been stopped by the police, demanding to know where he is going—those delays at times force him to get home past the curfew time of 19:00.
Mr Mubiru’s resolve to support his community is unwavering. He knows that not everybody would be comfortable visiting the nearest health facility for their antiretroviral refills, disclosing the reason to the local authorities for them to be granted movement or have a community organization’s branded car parked outside their home.
“Instances like these propel me to get out of bed every morning. We are still in this together. COVID-19 will end, and life will continue,” he says.
On average, he delivers eight antiretroviral refills per day to his peers. Besides the long distances and hard-to-reach places he has to go to, food is one of the biggest challenges, since hunger compromises people’s adherence to their medication. Stigma and non-disclosure also pose a great challenge for people to access HIV treatment from a nearby facility.
“The COVID-19 outbreak is having a major impact on people living with HIV,” said Karusa Kiragu, UNAIDS Country Director for Uganda. “We must ensure that adherence to HIV treatment is not compromised. This can be achieved through multimonth dispensing of antiretroviral therapy, supported by a strong community-led response,” she said.
More on COVID-19
Region/country
Related

Feature Story
Modelling the extreme—COVID-19 and AIDS-related deaths
25 May 2020
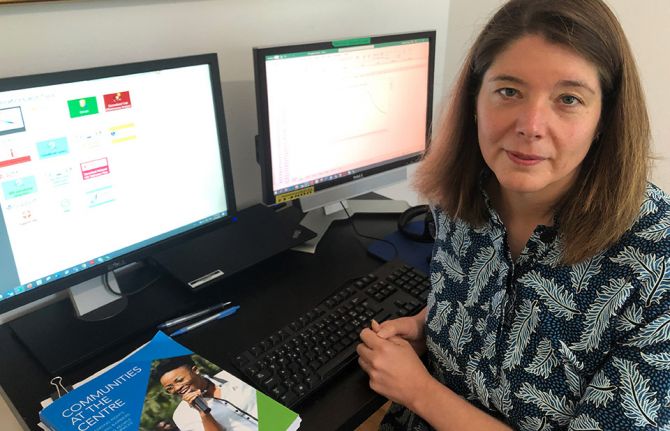
25 May 2020 25 May 2020Kimberly Marsh, a senior adviser on modelling and epidemiology, has worked for UNAIDS for six years. She supports countries in estimating the impact of the HIV epidemic globally and regionally.
Can you tell me more about the latest modelling report that you are a co-author of, which examines the potential for HIV service disruption in times of COVID-19 in sub-Saharan Africa?
This work looks at potential disruptions in sub-Saharan Africa owing to the COVID-19 pandemic on HIV services that might have an impact on HIV incidence—the number of new HIV infections—and on the number of AIDS-related deaths in excess to those we might have observed if we hadn’t had the COVID-19 pandemic.
We are particularly interested in those question because we know that more than two thirds of all people living with HIV worldwide are living in sub-Saharan Africa. That’s 25.7 million people living with HIV, 1.1 million new HIV infections and around 470 000 deaths from AIDS-related causes in 2018. Among all people living with HIV in the region, 64% of people are on life-saving antiretroviral therapy, which also prevents further new HIV infections.
It is really important that we’re able to ensure they will have access to services. In the models, we looked at service disruptions—a complete disruption of any HIV-related services over a three-month and a six-month period of time. And we looked at the impact after one year and five years. Now remember, these are just scenarios, and extreme ones. We don’t expect this to happen, but it helps us to answer two questions: what HIV-related services are most important to prevent additional deaths and new HIV infections and what might happen if we don’t mitigate or address those disruptions.
From this huge amount of work, what are the two key takeaways?
The modelling work predicted that with a six-month disruption in HIV treatment there could be an excess of 500 000 deaths in sub-Saharan Africa. So, when you look at UNAIDS estimates of AIDS-related deaths over time, that would take us back to about 2008, when we had nearly a million deaths.
There is no doubt about it, HIV treatment is critical. Ensuring that HIV treatment is available to people who need it during the three- to six-month periods is the most important thing that countries can do to prevent excess deaths and HIV incidence. All countries should work to ensure that supply chains are providing them with enough medicines to distribute and that people have sufficient medicines so that they can take them over the coming months.
The second thing to say is that these are projections and that there is still time to ensure that people get the HIV treatment services they need.
Let’s prevent what this model potentially predicts and let’s get HIV medicines to the people who are living with HIV.
What about HIV prevention? Does condom availability have an impact?
The models showed that when you look at prevention services, condom availability impacted the results. I think it is important to say that this is a treatment lesson primarily, but things like access to condoms is really important. We saw around a 20–30% relative increase in HIV incidence over one year if condoms were not available for six months. This is definitely something that we should be focusing on.
Can you tell us a little bit more about the impact on mother-to-child transmission of HIV in these scenarios?
In the scenarios, we looked at the potential for HIV testing services to be disrupted as well as for women to not get medicine to prevent transmission of HIV to their children. And what the various models found was that by removing those medicines—which have had an extremely important impact in terms of reducing new child HIV infections over the past five to 10 years—you could see rises in new child HIV infections in selected countries anywhere up to 162%. It really is critical to maintain prevention of mother-to-child transmission of HIV services.
You have said this was an extreme scenario, not a prophecy, but yet you still believe in modelling?
Models are very important for exploring questions that countries routinely pose to UNAIDS and the World Health Organization in terms of thinking of strategic approaches to responding to HIV in their countries. Models aren’t perfect, but they have a lot to tell us and I think in this instance it really highlights some of the strategies that will be important over the coming months as COVID-19 impacts or potentially impacts sub-Saharan Africa.
Related




Feature Story
UNAIDS and civil society helping stranded people living with HIV
22 May 2020
22 May 2020 22 May 2020A day before Deepak Sing (not his real name) planned to return to India, all international travel ground to a halt—he was stuck in Luanda.
Because of his frequent travel, he had extra HIV medicine, but his supplies started to run low.
“I visited more than 10 pharmacies and explored options of delivery of antiretroviral medicines from India to Angola, but without success,” he said.
He decided that reaching out to Indian colleagues would be his best bet.
“I contacted the Humsafar Trust in Mumbai, and they in turn contacted the UNAIDS India office,” he explained.
Bilali Camara, the UNAIDS Country Director for India, immediately followed up with his peer in Angola. The UNAIDS Country Director for Angola, Michel Kouakou, guided Mr Sing towards the national AIDS institute, which organized a conference call with a medical doctor because one of the medicines that Mr Sing took is not yet in use in Angola. The doctor proposed a substitute and in less than 24 hours he picked up his medication. “Due to the change of one medicine, Mr Sing received only a one-month supply, which will be renewed at his discretion,” explained Mr Kouakou, who has helped two other stranded foreigners in the past month.
“I now believe that humanity exists!" Mr Sing said with great relief.
Since the COVID-19 pandemic hit, UNAIDS has helped stranded people to obtain HIV medicine in countries as diverse as Canada, China, Latvia, Myanmar and Ukraine. Mr Camara said that UNAIDS set up a system so that 700 people from India who were living in Myanmar could access their medicine, since they could no longer access it in India because of the COVID-19 lockdown.
Jacek Tyszko, Senior Programme Adviser at UNAIDS’ Geneva headquarters, has never seen anything like this. So far, he has helped 100 people, mostly in eastern Europe, because of his experience in the region.
“Either I connect people to the local AIDS authority or ideally we link them up to civil society, because they usually have readily available treatment,” he explained. Because of demand, some grass-roots organizations have run out of supplies, which meant some readjusting.
“Overall, the response from local partners has been immediate,” Mr Tyszko said. In certain cases, if stranded people could not get treatment locally, UNAIDS helped them to get supplies from the person’s native country.
He cannot believe how people have had to overcome so many hurdles to obtain HIV medicine despite a clear need.
“In times of crisis like COVID-19 or other public emergencies, governments should waive restrictions to make it easier for people to obtain refills and life-saving care, regardless of their legal status, residency or citizenship,” he said.
UNAIDS has been advocating for the right to health and universal health coverage to alleviate problems like this. A better integration of HIV and other health services could help some of the gaps in the AIDS response to be addressed, which will ultimately make it easier for people to access life-saving medicines, care and support.
For now, Mr Tyszko feels that helping people is very satisfying. “It’s been such a boost to do something so concrete with immediate effect,” he said.
Our work

Feature Story
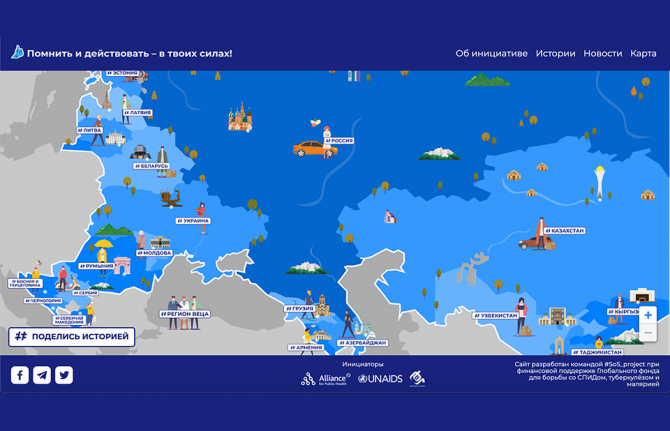
Mapping community responses to COVID-19 and HIV in eastern Europe and central Asia
21 May 2020
21 May 2020 21 May 2020During the COVID-19 crisis, activists and community organizations from across eastern Europe and central Asia are continuing to provide vital HIV prevention, treatment, care and support services.
To map that support, an interactive platform, the Community Initiates Map, has been launched. The website shows how communities are supporting people living with HIV and saving lives during the COVID-19 outbreak in the region, with stories about the services that community organizations are providing. People can learn from the examples of the services developed for key populations and people living with HIV and the impact that they are having on the HIV epidemic and on people’s lives. The map is constantly being updated and people can share their stories on the site.
Vera Brezhneva, UNAIDS Goodwill Ambassador for Eastern Europe and Central Asia, thanked activists for their commitment during the COVID-19 outbreak. “Thank you to every one of you, from all of us. It is in our power to remember and take action. I am with you!” she said.
The experience in eastern Europe and central Asia in the fight against COVID-19 shows that investments made in civil society are good investments. “Communities and nongovernmental organizations have not only come to the forefront of the fight against the new threat, but also in collaboration with medical practitioners and governments continue to provide HIV and tuberculosis services,” said Andrei Klepikov, Executive Director of the Alliance for Public Health.
Nurali Amanzholov, the President of the Central Asian Association of People Living with HIV, said that the coronavirus outbreak and lockdowns had resulted in some people having difficulties in accessing antiretroviral therapy and opioid substitution therapy, and that many people had lost their incomes. “But this situation is also an exam, a test of the strength of our community. And our strength was always in solidarity, the ability to assert our rights, to seek the right solution together,” he said.
Lyubov Vorontsova, of the Central Asian Association of People Living with HIV, said that women living with HIV, especially those in key populations, faced increased gender-based violence and limited access to protection and social services owing to the closure of crisis centres. “We must keep our unity now, so that after the end of the state of emergency, the needs of women remain a priority for the state and civil society,” she said.
“The nearly 40 years of experience in the response to HIV shows that civil society organizations, including communities of people living with HIV, play a crucial role. Today, it is clear that the role of community organizations in emergencies is vital. Countries in the region must recognize those organizations as partners and providers of services for the responses to both HIV and COVID-19,” said Alexander Goliusov, Director, a.i., UNAIDS Regional Support Team for Eastern Europe and Central Asia.
The website was developed by the Alliance for Public Health and the Central Asian Association of People Living with HIV and supported by the UNAIDS Regional Support Team for Eastern Europe and Central Asia.
Interactive platform
Learn more
Region/country
- Eastern Europe and Central Asia
- Albania
- Armenia
- Azerbaijan
- Belarus
- Bosnia and Herzegovina
- Bulgaria
- Croatia
- Cyprus
- Czechia
- Estonia
- Georgia
- Hungary
- Kazakhstan
- Kyrgyzstan
- Latvia
- Lithuania
- Montenegro
- Poland
- Republic of Moldova
- Romania
- Russian Federation
- Serbia
- Slovakia
- Slovenia
- Tajikistan
- North Macedonia
- Türkiye
- Turkmenistan
- Ukraine
- Uzbekistan
Related
 Women, HIV, and war: a triple burden
Women, HIV, and war: a triple burden

12 September 2025
 Displacement and HIV: doubly vulnerable in Ukraine
Displacement and HIV: doubly vulnerable in Ukraine

11 August 2025


Feature Story
Communities strengthening the AIDS response in Nepal
21 May 2020
21 May 2020 21 May 2020From the very beginning, communities were in the vanguard of the AIDS response in Nepal. Still playing a vital role in the response to HIV in the country, communities are making good-quality services more accessible for people living with HIV and key populations and standing up to HIV-related stigma and discrimination.
“Nepal made antiretroviral medicines accessible to all people living with HIV as a result of advocacy efforts led by communities, human rights activists and other national stakeholders,” said Gopal Shrestha, a prominent community leader living with HIV.
Discrimination towards key populations is still deeply rooted in Nepalese society. “Finding people who need services is difficult due to a lack of trust. We work with those communities that fear coming out because of discrimination,” said Simran Sherchan, Operation Head of the Federation of Sexual and Gender Minorities in Nepal (FSGMN).
Although antiretroviral medicines are available to everyone living with HIV in Nepal, a survey conducted in 2018 reveals that more than 30% of transgender people avoid seeking health care because of fear of stigma and discrimination—something that FSGMN is determined to end.
“Community-based organizations play an intricate role in reaching out to those hard to reach,” said Anjay Kumar KC, a community leader who advocates for harm-reduction in Nepal. Recovering Nepal, a community network of people who use drugs, is supporting harm reduction programmes and HIV prevention among young people who use drugs, including a peer-to-peer programme that provides sterile needles and syringes and a campaign that promotes HIV testing. It has also played a key role in advocating with the government to initiate opioid substitution therapy, which is now offered at 12 sites in five provinces in the country.
Community-based organizations mobilize communities to demand services and advocate for their right to health. Recently, the National Association of People Living with HIV/AIDS (NAP+N) successfully advocated to include people living with HIV in the country’s Health Insurance Programme in 57 districts across the country. “NAP+N also entered into an agreement with Prime Life Insurance Limited to guarantee people living with HIV can access life insurance services,” said Rajesh Didiya, President of NAP+N.
Despite these achievements, community-based organizations face challenges. “When I reach out to sex workers, I have to hide my identity, because sex work is still stigmatized by my family and society. That is why it is difficult to publicly raise awareness about sex workers’ rights,” said Bijaya Dhakal, Coordinator of the Nepal Federation of Female Sex Workers.
Parina Limbu, a community leader who advocates for engagement in decision-making by women who use drugs, said, “Being labelled as women who use drugs, women living with HIV and hepatitis and sex workers, we are not within the reach of programmes. Our needs should not be looked at through the lens of males who use drugs. Women who use drugs need more decision-making spaces to make sure that our voices are heard.”
Those challenges can be overcome through partnerships and joint efforts, however. The Right to Health Women’s Group, Right Here Right Now and FSGMN have created a platform to collect and monitor cases of human rights violations against people living with HIV, key populations and young people. They use the evidence that they collect to advocate for programmes on stigma and discrimination reduction in health facilities and raise awareness about the human rights of key populations with law enforcement officers.
UNAIDS in Nepal has played a key role in empowering communities. “The important role that the community plays in the country’s response to HIV should not be underestimated. The gains made are because communities are taking the initiative and acting in ways that ensure that people who need treatment, prevention and related HIV services can access them,” said Masauso Nzima, UNAIDS Country Director for Nepal and Bhutan.
Video
Region/country



Feature Story
Gender-based violence and COVID-19—“When we are silent, we allow these crimes to multiply”
19 May 2020
19 May 2020 19 May 2020UN Women estimates that globally in the past 12 months 243 million women and girls aged 15–49 years were subjected to sexual and/or physical violence perpetrated by an intimate partner. As a result of the lockdowns imposed to stop the spread of COVID-19, emerging data show that such violence has intensified. In France, for example, reports of domestic violence have increased by 30% since the lockdown started on 17 March, and in Argentina emergency calls about domestic violence have increased by 25% since its lockdown started on 20 March. Many other countries have reported such increases.
Recently, the Odnoklassniki social network, known as OK, hosted a broadcast for experts and others to discuss how to survive lockdown and avoid family conflict and gender-based violence. The broadcast was seen by 1.7 million OK network users across eastern Europe and central Asia.
“I live in Kyrgyzstan,” Ulzisuren Jamstran, a representative of UN Women in Kyrgyzstan, said. “Here, according to the government, the level of domestic violence increased by 65%. We see an increase in aggression against women and children in Kyrgyzstan, we see an increase in suicides among children, even young children.”
Lyudmila Petranovskaya, a Russian psychologist, explained how isolation made good relationships become better and problematic relationships become more problematic. She emphasized that people need to be aware of the options if they are locked down with an abuser. “People have to look for contacts, a hotline, call friends, try to find another place to survive isolation. Staying with the abuser is dangerous. This threat is more serious than coronavirus,” she said.
Julia Godunova, Deputy Head of the Board of the Eurasian Women’s Network on AIDS, spoke about studies in eastern Europe and central Asia that show that more than 70% of women who survived violence do not seek help because of the perceived shame.
Dina Smailova, the founder of the #DontBeSilentKZ nongovernmental organization, addressed female survivors of violence. “When we are silent, we allow these crimes to multiply. I urge women not to be silent. Our movement is expanding, we are active not only in Kazakhstan, but also in other countries of central Asia and beyond.”
The broadcast highlighted successful experiences around the world in responding to gender-based violence. The example in Spain, where women in danger can visit pharmacies and use a code word to alert staff that they need help, was praised. The role of the private sector was also shown to be important—since many shelters are not open at present, hotels are stepping in and providing shelter, either for free or at a minimal cost.
The broadcast was part of a joint initiative of the UNAIDS regional office for eastern Europe and central Asia, the UNESCO Institute for Information Technologies in Education and OK, in partnership with the regional office of UN Women for eastern Europe and central Asia.