Update
Decline in new HIV infections has stalled
13 September 2021
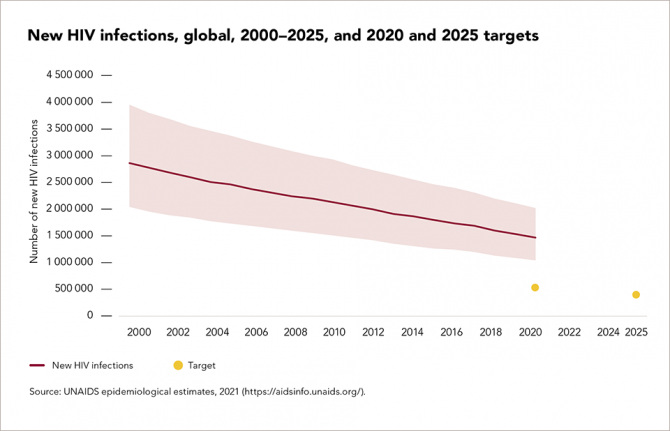
13 September 2021 13 September 2021While the global roll-out of HIV treatment has saved millions of lives, efforts to prevent new HIV infections have been less successful. The annual number of new HIV infections among adults globally has hardly changed over the past four years, and total new infections have declined by just 31% since 2010, far short of the 75% target for 2020 that was set by the United Nations General Assembly in 2016.
Too many countries have failed to put in place the combination of structural, behavioural and biomedical approaches to HIV prevention focused on those at greatest risk that experience shows has the maximum impact. Consistent condom use, although possible, has proved difficult to achieve among all populations: women in many countries, for example, need greater agency and support to negotiate consistent condom use. Coverage of pre-exposure prophylaxis and of voluntary medical male circumcision in 2020 also were well below the targets set five years earlier.
Reductions in new infections were strongest in sub-Saharan Africa and the Caribbean, but no region achieved the 75% declines that were agreed by the United Nations General Assembly in 2016. Epidemics in large parts of eastern Europe and central Asia expanded in the face of serious legal and policy barriers and inadequate attention to the needs of people who inject drugs and gay men and other men who have sex with men. The annual number of new HIV infections also climbed in the Middle East and North Africa, and Latin America did not achieve any reduction in infections over the course of the last decade.
Our work

Update
Global roll-out of HIV treatment has saved millions of lives
06 September 2021
06 September 2021 06 September 2021The 90–90–90 targets, agreed by the United Nations General Assembly in 2016, called for the vast majority of people living with HIV to be tested, start treatment and have the HIV within their bodies reduced to undetectable levels by 2020. Achieving these targets means that a minimum of 73% of people living with HIV have suppressed viral loads, which helps to keep them healthy and prevents the further spread of the virus.
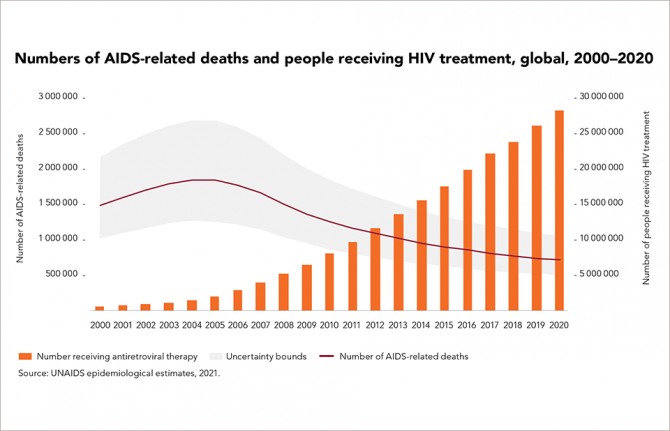
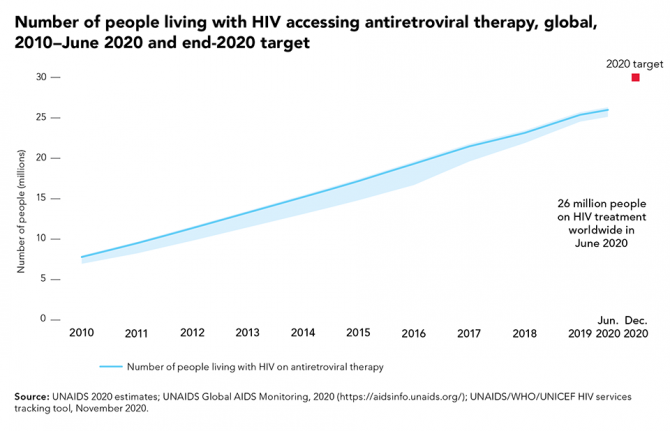
At the end of 2020, 84% of people living with HIV knew their HIV status, 73% were accessing antiretroviral therapy and 66% were virally suppressed. Among the 37.7 million people living with HIV globally in 2020, an estimated 27.5 million people living with HIV were on treatment—a number that has more than tripled since 2010, but that is still short of the 2020 target of 30 million.
The global roll-out of HIV treatment has saved millions of lives: an estimated 16.5 million AIDS-related deaths have been averted since 2001. In 2020, there were 680 000 deaths from AIDS-related causes, a decline of 58% from 2001 to 2020. At least 40 countries are on track to achieve a 90% reduction in AIDS-related mortality by 2030, including nine countries in eastern and southern Africa.
Our work
Related


Update
Opening remarks by UNAIDS Executive Director Winnie Byanyima at the High-Level Meeting on AIDS
08 June 2021
08 June 2021 08 June 2021Excellencies, distinguished delegates, colleagues, friends.
Thank you, General Assembly President Bozkir, Deputy Secretary-General Amina Mohammed, co-facilitators Ambassador Gertze of Namibia and Ambassador Fifield of Australia, and all Member States; together you’ve drafted, negotiated, and delivered this Political Declaration. It will be the basis of our work to end this pandemic that has ravaged communities for 40 years.
AIDS is not over. It is one of the deadliest pandemics of modern times. Since the start of the epidemic 77.5 million people have been infected with HIV. We have lost nearly 35 million people to AIDS. An AIDS death every minute is an emergency! HIV rates are not following the trajectory that we together promised. Indeed, amidst the fall-out from the Covid crisis, we could even see a resurgent pandemic.
But a never-ending HIV pandemic is not our fate. In spite of all the set-backs, we can end AIDS as a public health threat, as we promised, by 2030, if we come together.
Business as usual, however, would fail. The programmes that have secured substantial progress will not enable us to finish the journey because the road is blocked. The evidence and analysis is clear. Inequalities in power, status, rights and voice are driving the HIV pandemic. Inequalities kill. As the Global AIDS strategy sets out: to end AIDS, we have to end the inequalities which perpetuate it.
There’s another huge benefit to this approach. The same laws, policies and strong people-centred health services needed to end AIDS, will also help the world overcome Covid-19, be ready to tackle future pandemics, and support inclusive economic growth and the human rights of all. We will all do better.
Here are three bold shifts we need to take together:
- We need to end inequalities in access to health technologies, by spurring the best science and getting it to everyone.
COVID-19 showed science moves at the speed of political will. We need to speed up AIDS science by investing in innovations in treatment, prevention, care, and vaccines, as global public goods.
And we need to deploy science in ways that shrink instead of grow inequalities.
For example, let’s get the new long-acting anti-retroviral medicines that will make it easier to treat and prevent HIV to women in all their diversity and key populations in the global South first, not years after people in rich countries have access.
Let us ensure that all medicines which can prevent deaths of people living with HIV are manufactured by multiple producers affordably especially in the global South, where the disease is concentrated
We need funding, but we also need to reform failing rules on intellectual property, and support globally distributed production, so access to life-saving science is no longer dependent on the passport you hold. - We need to end the inequalities in access to essential services, by delivering on guaranteed health and education for everyone. For many communities, new HIV infections have become rare; and living long, fulfilling lives with HIV is the norm. But within and between countries, a widening gap separates those who have prevention, treatment and care services and their rights respected and those who are excluded.
Today we are setting bold, ambitious goals to reach 95% of those in need with HIV treatment and prevention: to get there we need to re-imagine HIV services, making them easy to access and designed around people’s lives.
We need to ensure all girls complete secondary education and are empowered with the full set of services and rights.
We need to end user fees for essential services and provide these services through public systems funded by taxation. We need to integrate community-provided services. We need to combat tax avoidance, which impedes domestic resourcing for health and education.
Most developing countries are facing severe fiscal crisis, with a revenue loss above 20% in 2020 and health budgets under threat, with Africa under especial pressure.
This is a time to increase revenues, and that requires an end to tax dodging and tax competition that empty public coffers.
We also need debt restructuring to overcome the COVID19 shock and the establishment of a fair debt crisis resolution mechanism. We need to step up, not step back on the commitment to aid as 0.7% of gross national income by all developed countries and ensure that more of the IMF’s USD 650 billion Special Drawing Rights issuance flows to low and middle-income countries. - We need to end the inequalities in the realisation of rights, particularly for people living with HIV, and those vulnerable to or affected by HIV.
I applaud Member States’ commitment to reform laws and protect rights. The evidence shows that when laws are strengthened to support gender equality and the rights of key populations and confront stigmatisation, countries have much greater success in treatment and prevention programmes, benefiting everyone. They’ve rolled back HIV.
We need to keep moving forward in our common journey, away from harmful, punitive, outdated often colonial laws and from all forms of discrimination.
This moment calls for us to work together across sectors, across countries. Populism’s false promises are proving no match to biology: as Covid reminds us, we’re not just interconnected, we’re inseparable.
We cannot end AIDS in one country or one continent, we can only end AIDS everywhere.
I pay tribute to the civil society groups from across the world whose fight against inequalities has been the spur to action. You, communities, women’s groups and grassroots movements, have constantly pushed us; at times that pushing has been uncomfortable; but my message to you is: keep pushing us all. Keep the fight on! Pressure from the power of people is key to ending inequalities and ending AIDS.
Martin Luther King said the moral arc of the universe is long, but it bends towards justice. He didn’t mean this process is automatic. As he noted, “social progress never rolls in on wheels of inevitability; it comes through the tireless efforts of people”. The trajectory of new HIV infections and AIDS deaths will not, through business-as-usual, bend down, but we can pull it down.
We cannot be neutral on inequalities. To get back on track to ending AIDS, we must be deliberate in confronting them. The only alternative is a vicious cycle of injustice, illness, and emergency. The most unrealistic thing we could do now is to imagine we can overcome our crises through minor adjustments or tinkering.
Whether we are remembered as promise-breakers or promise-keepers, as failures or victors, as the people who ended AIDS, or only as the people who could have ended AIDS, is up to us.
Epidemics magnify our worst traits—inequalities, injustices, and fear; but also, our best traits—ingenuity, resilience, and courage.
I’m confident we will win, together. Thank you.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Related


Update
Discriminatory attitudes towards people living with HIV declining in some regions, rebounding in others
25 January 2021
25 January 2021 25 January 2021Among 151 reporting countries, 92 continue to criminalize HIV exposure, transmission and nondisclosure—all grave violations of the rights of people living with HIV that also frustrate efforts to control HIV epidemics. These laws reinforce stigma and discrimination against people living with HIV and those more vulnerable to HIV infection, they disregard up-to-date knowledge on the science of HIV-related risks and harms, and they have adverse impacts on public health.
The most recent data from population-based surveys show that while discriminatory attitudes towards people living with HIV are declining consistently in some regions, they are rebounding in others. In eastern and southern Africa, for instance, discriminatory attitudes have been reduced to historically low levels in some countries. Elsewhere, however, disconcertingly large proportions of adults continue to hold discriminatory attitudes towards people living with HIV. In 25 of 36 countries with recent data on a composite indicator that includes two types of discriminatory attitudes, more than 50% of people aged 15 to 49 years reported having discriminatory attitudes towards people living with HIV.
Our work

Update
Attaining UNAIDS’ proposed societal and legal barrier targets could stop 440 000 AIDS-related deaths
11 January 2021
11 January 2021 11 January 2021UNAIDS has called on countries to make far greater investments in global pandemic responses and adopt a new set of bold, ambitious but achievable HIV targets for 2025.
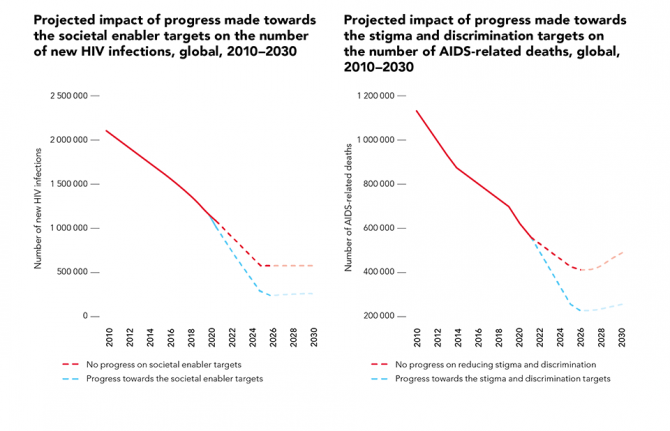
An analysis was performed focused on available studies that have quantitatively measured the negative impact that stigma and discrimination and the criminalization of sex work, drug use and same-sex sexual relationships would have on HIV prevention, testing and treatment efforts.
The analysis suggests that failure to make any progress on HIV-related stigma and discrimination would undermine efforts to reach the HIV testing, treatment and viral suppression targets, resulting in an additional 440 000 AIDS-related deaths between 2020 and 2030, and that failure to make any progress across all societal enablers would undermine efforts to reach HIV prevention targets, resulting in 2.6 million additional new HIV infections over the same period.
Our work

Update
Joint statement calling for urgent country scale-up of access to optimal HIV treatment for infants and children living with HIV
22 December 2020
22 December 2020 22 December 2020Global partners that are committed to ending paediatric AIDS have come together to call on countries to rapidly scale up access to optimal, child-friendly HIV treatment for infants and children. The partners include the United Nations Children’s Fund, the World Health Organization (WHO), UNAIDS, the United States President’s Emergency Plan for AIDS Relief, the Global Fund to Fight AIDS, Tuberculosis and Malaria, Unitaid, the Elizabeth Glaser Pediatric AIDS Foundation, and the Clinton Health Access Initiative (CHAI).
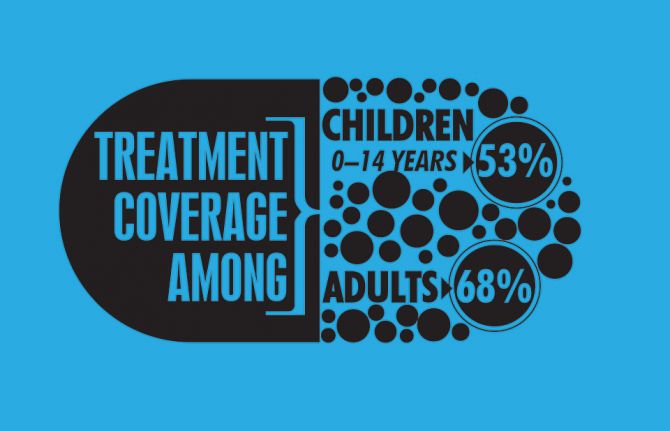
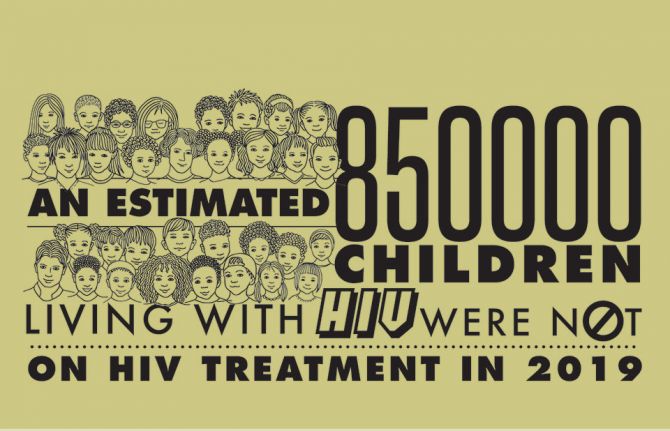
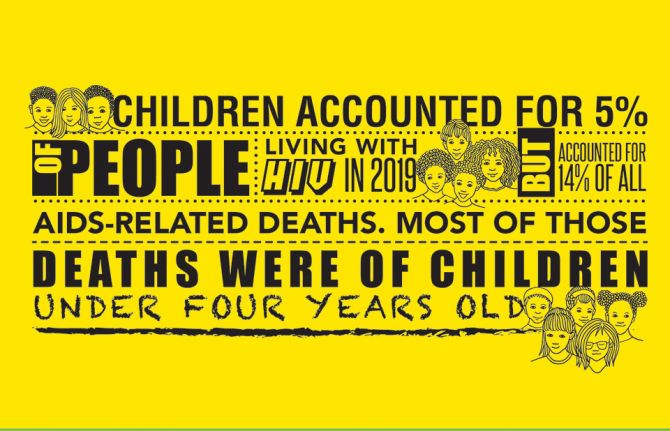
Children living with HIV continue to be left behind by the global AIDS response. In 2019, only 53% (950 000) of the 1.8 million children living with HIV (aged 0–14 years) globally were diagnosed and on treatment, compared to 68% of adults. [1] The remaining 850 000 children living with HIV have not been diagnosed and are not receiving life-saving HIV treatment. Two thirds of the missing children are aged 5–14 years and do not routinely attend traditional health facilities. Engaging communities and the families of people living with HIV, tuberculosis and other related diseases and offering family services are needed in order to find and start on treatment those missing children.
An estimated 95 000 children died of AIDS-related illnesses in 2019, in part due to lack of early diagnosis of HIV among infants and children and immediate linkage to optimal HIV treatment regimens. Untreated, 50% of infants infected with HIV during or around the time of birth will die before the age of two years. [1]
The United States Food and Drug Administration recently gave tentative approval for the first generic formulation of dolutegravir (DTG) 10 mg dispersible tablets. [2] This approval was the result of an innovative partnership between Unitaid, CHAI and ViiV Healthcare, together with generic suppliers, which accelerated the timeline of development by several years. The approval was quickly followed by the announcement on World AIDS Day of a groundbreaking agreement negotiated by Unitaid and CHAI that reduces the cost of HIV treatment by 75% for children in low- and middle-income countries, where the DTG 10 mg dispersible tablets will be available at a cost of US$ 4.50 for a 90-count bottle. [3]
This now means that WHO-recommended, preferred first-line DTG-based antiretroviral treatment is now available in more affordable and child-friendly generic formulations for young children and infants as young as four weeks of age and weighing more than 3 kg. [4] Rapid transition to this treatment, in combination with improved HIV diagnosis for children and other supportive measures, will help to urgently reduce the 95 000 preventable AIDS-related deaths in children.
DTG-based HIV treatment leads to better outcomes for children. DTG is less likely to be affected by drug resistance and achieves viral load suppression sooner; child-friendly dispersible tablets improve adherence due to a lower pill burden and being easier to administer. These factors help children achieve and maintain viral load suppression, the gold standard for measuring the effectiveness of HIV treatment. DTG-based treatment is the standard of care for adults. Starting on this regimen from infancy reduces the need for changes in treatment as they mature through childhood, adolescence and adulthood. Fewer regimens and regimen changes simplifies management of health care, improves stock management and reduces wastage.
WHO has recommended DTG-based HIV treatment for all infants and children since 2018 [4] and provided dosing recommendations for infants and children over four weeks of age and more than 3 kg in July 2020. [5]
Suppliers have indicated their ability to meet global scale-up ambitions. Accurate forecasts of demand are critical to inform production planning and delivery timelines. It is therefore critical that national programmes start including DTG 10 mg dispersible tablets in their new procurement plans, review stocks and orders for existing non-DTG treatment for children, share forecasts with HIV treatment procurement partners and suppliers and place orders as early as possible.
The partners are committed to support national governments as they develop rapid transition plans from existing suboptimal HIV treatment to DTG-based treatment for infants and children, including advocacy for political commitment, mobilizing international and domestic resources, new policies and guidelines, managing medicine supply, distribution and stock, training health-care workers and sensitizing and engaging affected communities to ensure demand and treatment literacy for children living with HIV and their caregivers in order to ensure rapid uptake of these new formulations.
Further guidance for national programmes and partners is available from WHO. [5] The CHAI HIV New Product Introduction Toolkit has dedicated resources to help countries transition to paediatric DTG. [6]
Quotes from partners
“National governments, partners on the ground and affected communities need to work together to find and treat the children and infants whose lives can be saved by these new medicines,” said Shannon Hader, UNAIDS Deputy Executive Director for Programme. “The new medicines are cheaper, more effective and more child-friendly than current treatments for infants and young children. We need to get them into clinics to save lives now.”
“The United States President’s Emergency Plan for AIDS Relief works tirelessly to ensure clients can access the best available HIV treatment, including advanced, paediatric regimens for children living with HIV,” said Deborah L. Birx, United States Global AIDS Coordinator and United States Special Representative for Global Health Diplomacy. “The accelerated introduction and expansion of paediatric DTG has the potential to save and improve the lives of thousands of children around the world. The United States President’s Emergency Plan for AIDS Relief will continue to collaborate with global and local partners to ensure the young children we serve can promptly access paediatric DTG.”
“Providing antiretroviral drugs to people living with HIV is at the core of our support to national HIV programmes,” said Peter Sands, Executive Director of the Global Fund to Fight AIDS, Tuberculosis and Malaria. “This new and affordable child-friendly HIV treatment is a tremendous step forward that will improve and save the lives of some of the most vulnerable in society—young children infected with HIV. We are committed to support countries to make a fast transition to these new drugs.”
“Children in low- and middle-income countries often wait years to access the same medications as adults, hindering their quality of life, or even resulting in preventable deaths. We are proud to have worked with partners on this groundbreaking agreement that will bring quality assured dispersible DTG to children at a record pace,” said Philippe Duneton, Unitaid Executive Director. “Ensuring access to this treatment will transform the lives of children living with HIV, helping them to remain on treatment and saving thousands of lives.”
“For the first time, children living with HIV in low- and middle-income countries will have access to the same first-line antiretroviral medication at the same time as those in high-income countries,” said Iain Barton, Chief Executive Officer of the Clinton Health Access Initiative. “The partnership should serve as a model to remove barriers that hinder development of paediatric formulations to deliver top-line medications quickly and affordably.”
“The persistent treatment gap between adults and children prevents us from achieving an AIDS-free generation,” said Chip Lyons, President and Chief Executive Officer of the Elizabeth Glaser Pediatric AIDS Foundation. “Children living with HIV around the world urgently require age-appropriate, effective and accessible formulations. Approval of dispersible DTG is a momentous step forward, but meaningless if this new formulation doesn’t quickly reach the babies and small children who desperately need it most. The Elizabeth Glaser Pediatric AIDS Foundation is committed to supporting accelerated roll-out, uptake and delivery of new, optimal paediatric antiretroviral medicines in partnership with global, regional and local leaders.”
“The persisting treatment gap between mothers and children is unacceptable with the new scientific breakthroughs that are within our reach to change the trajectory”, said Chewe Luo, Associate Director and Chief of HIV, United Nations Children’s Fund. “The United Nations Children’s Fund welcomes global commitments and progress made in developing better diagnostic approaches and optimal regimens for children to improve their outcomes.”
“This has the potential to be a true game-changer for children with HIV", said Meg Doherty, Director of Global HIV, Hepatitis and STI Programmes at WHO. “We must do all in our power to help countries get this new paediatric DTG 10 mg to all the children who need it."
[1] UNAIDS. Start Free Stay Free AIDS Free - 2020 report. 07 July 2020. https://www.unaids.org/en/resources/documents/2020/start-free-stay-free-aids-free-2020-progress-report
[2] https://www.accessdata.fda.gov/drugsatfda_docs/pepfar/214521PI.pdf
[3] UNITAID press release. Groundbreaking Agreement Reduces by 75% the Cost of HIV Treatment for Children in Low-and Middle-Income Countries. https://unitaid.org/news-blog/groundbreaking-agreement-reduces-by-75-the-cost-of-hiv-treatment-for-children-in-low-and-middle-income-countries/#en
[4] World Health Organization. Updated recommendations on first-line and second-line antiretroviral regimens and post-exposure prophylaxis and recommendations on early infant diagnosis of HIV. Interim guidance. 1 December 2018, https://www.who.int/publications/i/item/WHO-CDS-HIV-18.51.
[5] World Health Organization. Considerations for introducing new antiretroviral drug formulations for children. Policy brief. 1 July 2020, https://www.who.int/publications/i/item/9789240007888.
[6] Clinton Health Access Initiative. HIV new product introduction toolkit. Pediatric 10 mg dispersible, scored resources, https://www.newhivdrugs.org/.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Our work
Related


Update
New modelling shows COVID-19 should not be a reason for delaying the 2030 deadline for ending AIDS as a public health threat
14 December 2020
14 December 2020 14 December 2020Data reported to UNAIDS by countries have been used to project the potential impact of the COVID-19 pandemic on the global HIV response over the next five years. Several scenarios with different durations of service disruptions of between three months and two years were modelled.
The disruptions included: (a) a rate of increase in HIV treatment half the pre-COVID-19 rate; (b) no voluntary medical male circumcision; (c) 20% complete disruption of services to prevent vertical transmission; and (d) no pre-exposure prophylaxis scale-up. An important assumption across all the scenarios was that the current research pipeline would generate one or more safe and effective COVID-19 vaccines, and that the world will succeed in rolling out vaccines globally.
Results from the model showed that COVID-19-related disruptions may result in 123 000 to 293 000 additional HIV infections and 69 000 to 148 000 additional AIDS-related deaths globally. More positively, however, these projections show that the COVID-19 pandemic’s effects on the HIV response would be relatively short-lived. Using these projections, UNAIDS and its partners have concluded that the COVID-19 pandemic should not be a reason for delaying the 2030 deadline for ending AIDS as a public health threat.
Our work
Related


Update
New HIV infections among gay men and other men who have sex with men increasing
07 December 2020
07 December 2020 07 December 2020In 2019, key populations (including gay men and other men who have sex with men, people who inject drugs, sex workers, transgender people and prisoners) and their partners accounted for 62% of all new HIV infections worldwide, including the largest share of new infections in every region other than eastern and southern Africa.
Globally, new HIV infections declined by 23% from 2010 to 2019. The 1.7 million new infections that occurred in 2019 are more than three times higher than the global target of less than 500 000 new infections in 2020.
However, barely a dent has been made in the number of HIV infections among female sex workers, people who inject drugs and transgender women, and HIV infections among gay men and other men who have sex with men increased by an estimated 25% between 2010 and 2019.
Our work

Update
HIV treatment target for 2020 to be missed
30 November 2020
30 November 2020 30 November 2020At the United Nations High-Level Meeting on Ending AIDS in 2016, countries pledged to increase the number of people living with HIV on treatment to 30 million by the end of 2020.
Treatment scale-up has been impressive, with more than twice the number of people on treatment than in 2010, but as of June 2020 there were only 26 million people on HIV treatment, 4 million short of the target for the end of 2020.
The COVID-19 pandemic has played a role in slowing treatment scale-up in the past six months. The relative change in the number of people on treatment increased by an estimated 2.4% from January to mid-June 2020, compared with 4.8% between January and June 2019.
Our work
Related


Update
Condom use declining
23 November 2020
23 November 2020 23 November 2020The defunding of condom social marketing programmes and decline in sales of socially marketed condoms in sub-Saharan Africa is emblematic of a decreased focus on condom demand generation, reduced emphasis on condoms in family planning services and weak stewardship of condom programmes since 2010, leaving the world far off the 90% target for condom use.
A new generation of sexually active young people has not been exposed to the intense condom promotion that was in place a decade ago. Condom use at last higher risk sex reported by young women (aged 15 to 24 years) declined in five countries in western and central Africa and three countries in eastern and southern Africa. Condom use at higher risk sex among men (aged 15 to 49 years) also declined in five out of nine countries (compared to the previous survey). The use of condoms across all of western and central Africa and eastern and southern Africa remains far too low.