
Update
HIV financing gap widening
16 November 2020
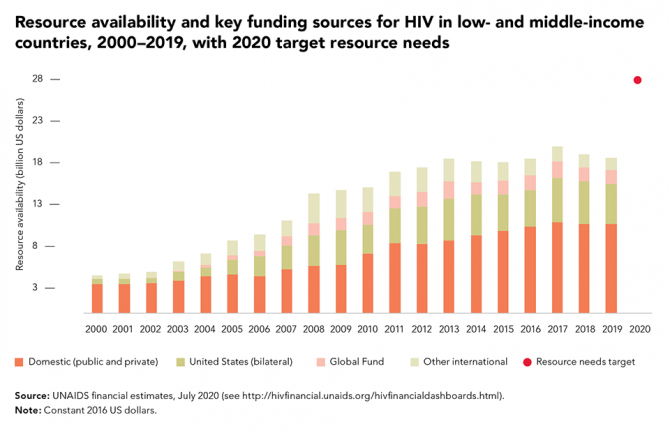
16 November 2020 16 November 2020The funding gap for HIV responses is widening. Momentum established following global agreement on the Millennium Development Goals in 2000 has been lost in the Sustainable Development Goal era. Increases in resources for HIV responses in low- and middle-income countries halted in 2017, with funding decreasing by 7% between 2017 and 2019 (to US$ 18.6 billion in constant 2016 United States dollars).
The total funding available in 2019 for HIV in these countries amounted to about 70% of the 2020 target set by the United Nations General Assembly.
In the light of the theme of this year’s World AIDS Day, global solidarity, shared responsibility, it’s interesting to note that domestic investments in HIV responses in low- and middle-income countries have grown by 50% since 2010. Financial support for those countries provided through the Global Fund to Fight AIDS, Tuberculosis and Malaria increased by 26% between 2010 and 2017, but then declined by 15% over the next two years, leaving a 7% total increase over the nine-year period. Bilateral funding provided to those countries by the United States Government increased by 50% between 2010 and 2017 before declining by 8% over the next two years, leaving a 38% total increase since 2010 (in constant 2016 United States dollars). Contributions from other international sources declined by 50% between 2010 and 2019. Resource availability is presented in constant 2016 United States dollars in order to be comparable with the target for 2020 adopted in the 2016 High-Level Meeting on Ending AIDS.


Update
Little progress in increasing comprehensive knowledge of HIV among young women in eastern and southern Africa
09 November 2020
09 November 2020 09 November 2020A critical component of HIV responses is ensuring that young people know both how to prevent HIV infections and where they can safely access HIV prevention and sexual and reproductive health services.
An analysis of population-based surveys conducted since 2000 suggests that comprehensive knowledge of HIV among young women and men in western and central Africa—and men in eastern and southern Africa—has steadily risen. However, comprehensive knowledge of HIV among young women in eastern and southern Africa has increased at a slower rate.
Recent surveys show that there is still significant work to be done. Among surveys conducted between 2011 and 2018, just 39% of young women (aged 15 to 24 years) in eastern and southern Africa—and 28% in western and central Africa—demonstrated comprehensive knowledge of HIV, compared to 46% and 31% of young men in the same age group, respectively. In 2001, countries committed in the Declaration of Commitment on HIV/AIDS to ensure that, by 2005, 90%, and, by 2010, 95% of young people aged 15–24 years have information, education, services and life skills that enable them to reduce their vulnerability to HIV infection.
Our work
Region/country
- West and Central Africa
- Benin
- Burkina Faso
- Burundi
- Cameroon
- Cape Verde
- Central African Republic
- Chad
- Congo
- Côte d'Ivoire
- Democratic Republic of the Congo
- Equatorial Guinea
- Gabon
- Gambia
- Ghana
- Guinea-Bissau
- Guinea
- Liberia
- Mali
- Mauritania
- Niger
- Nigeria
- Sao Tome and Principe
- Senegal
- Sierra Leone
- Togo
- Eastern and Southern Africa
- Angola
- Botswana
- Comoros
- Eritrea
- Ethiopia
- Kenya
- Lesotho
- Madagascar
- Malawi
- Mauritius
- Mozambique
- Namibia
- Rwanda
- Seychelles
- South Africa
- South Sudan
- Eswatini
- Uganda
- United Republic of Tanzania
- Zambia
- Zimbabwe

Update
Highly effective HIV prevention option not reaching those who need it
02 November 2020
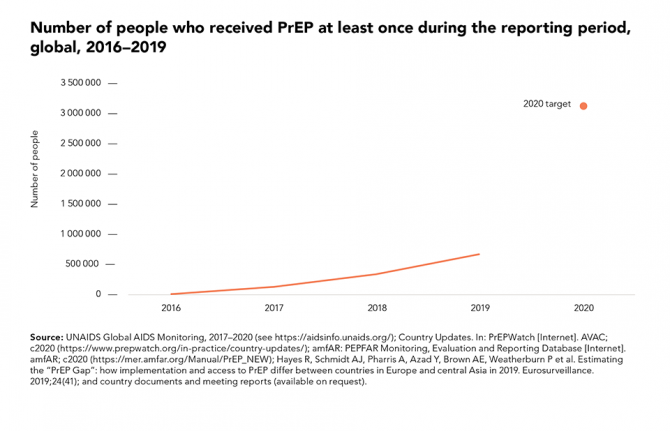
02 November 2020 02 November 2020Pre-exposure prophylaxis (PrEP), an HIV prevention option whereby someone who is HIV-negative takes antiretroviral medicines prior to possible exposure to HIV, has been shown to be highly efficacious across all populations. The offer of PrEP as part of a combination approach to HIV prevention has been recommended by the World Health Organization for all people at substantial risk of HIV since 2015.
The number of people reported to have received PrEP at least once in the previous year has increased dramatically in recent years, from fewer than 2000 in 2016 to more than 590 000 in 2019. In several cities in North America, Europe and Australia where PrEP is widely available, this relatively new prevention tool has contributed to steep reductions in HIV infections among gay men and other men who have sex with men. Global coverage, however, is still far short of the 2020 target of 3 million people receiving PrEP.
Our work


Update
Key populations have suboptimal knowledge of their HIV status
26 October 2020
26 October 2020 26 October 2020There are significant gaps in HIV testing among key populations at higher risk of HIV infection, resulting in suboptimal levels of knowledge of their HIV status. HIV testing is a critical gateway to HIV prevention and treatment services. Without knowledge of HIV status, people cannot access life-prolonging HIV treatment services.
Analysis of data from special surveys shows that, on average, about two thirds of sex workers and gay men and other men who have sex with men globally either had taken an HIV test and received the results within the past 12 months or had previously tested positive for HIV—meaning that about one third did not know their HIV status. This testing gap was even larger for people who inject drugs. These surveys are often conducted where key population-friendly services are available and may overstate overall testing coverage.
Our work

Update
New HIV infections: men outnumber women
12 October 2020
12 October 2020 12 October 2020Men living with HIV are less likely to access HIV testing and antiretroviral therapy, and they also experience higher levels of new HIV infections.
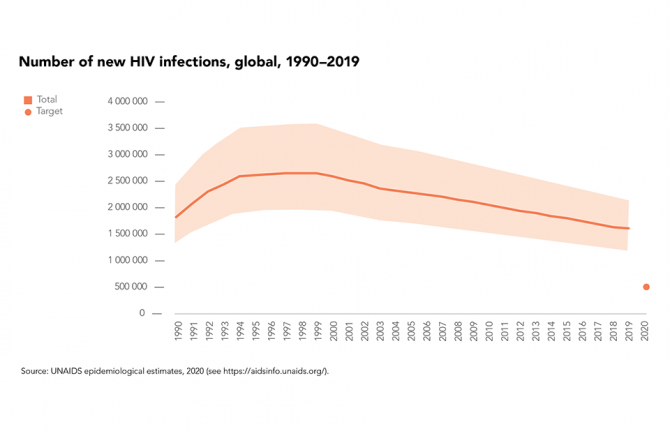
In 2019, the estimated 1.7 million people who acquired HIV worldwide marked a 23% decline in new HIV infections since 2010, although progress on HIV prevention remains far too slow, with the estimated total number of new infections in 2019 more than three times higher than the milestone of 500 000 that was set for 2020.
There were fewer new HIV infections in 2019 worldwide among women and girls (48% of total infections) than among men and boys (52%) in 2019—globally the annual number of new infections has been falling more rapidly among women and girls (a 27% decrease since 2010) than among men and boys (an 18% decrease).
Number of new HIV infections by sex, global, 2019-2019. Source: UNAIDS epidemiological estimates, 2020
RESOURCES

Update
Women living with HIV are more likely to access HIV testing and treatment
05 October 2020
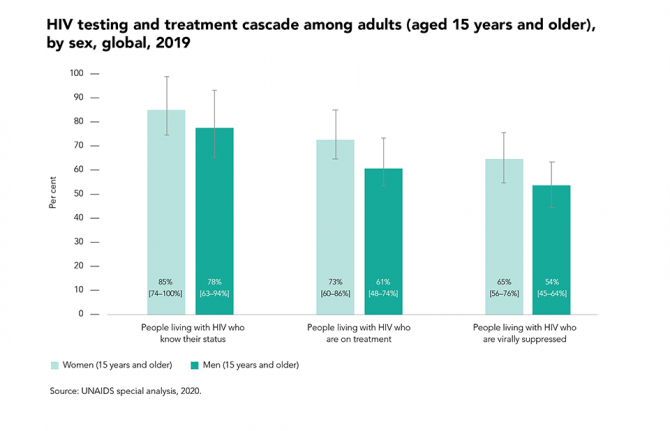
05 October 2020 05 October 2020In nearly all regions, women living with HIV are more likely to access HIV testing and antiretroviral therapy than men, in part due to better health-seeking behaviour among women and the existence of HIV-related services designed specifically to reach women (such as services to prevent mother-to-child HIV transmission that are provided during antenatal care).
In 2019, treatment coverage globally was 12 percentage points higher among women living with HIV than among men living with HIV, and viral suppression was 10 percentage points higher. This treatment gap among men living with HIV contributes to the higher number of new HIV infections among women in sub-Saharan Africa. Recent longitudinal studies have shown how closing these gaps accelerates declines in the incidence of HIV among women, especially young women.
Resources

Update
New HIV infections increasingly among key populations
28 September 2020
28 September 2020 28 September 2020In 2019, the proportion of new adult HIV infections globally among key populations and their sexual partners was 62%. This shift to an HIV epidemic increasingly among key populations is a result of the strong progress in HIV prevention in settings with high HIV prevalence in eastern and southern Africa, combined with a mixture of progress and setbacks in lower-prevalence regions.
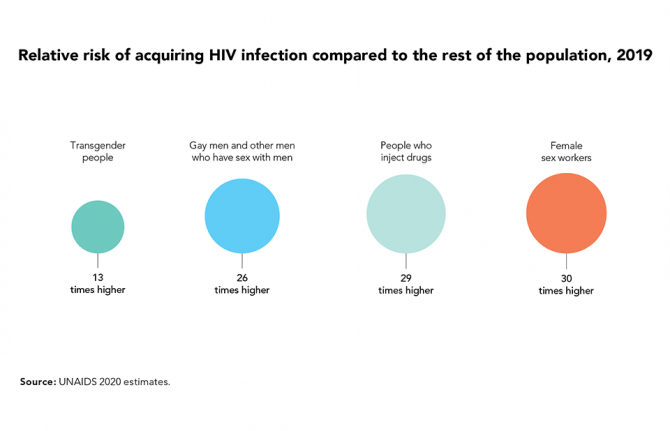
Key populations—which include sex workers, people who inject drugs, prisoners, transgender people, and gay men and other men who have sex with men—constitute small proportions of the general population, but they are at elevated risk of acquiring HIV infection, in part due to discrimination and social exclusion.
Learn more
Related

Update
90–90–90: good progress, but the world is off-track for hitting the 2020 targets
21 September 2020
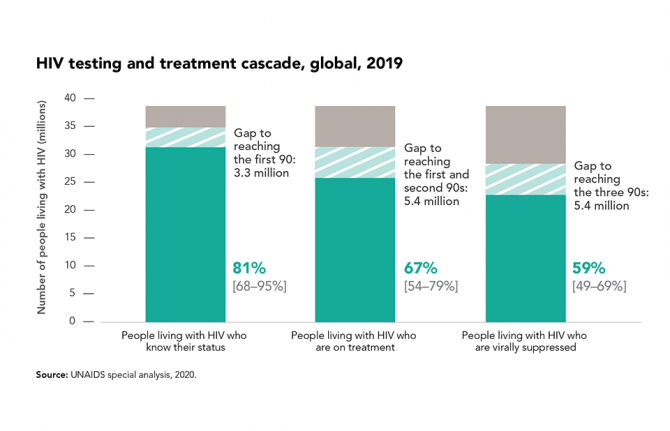
21 September 2020 21 September 2020In 2016, the United Nations General Assembly’s Political Declaration on Ending AIDS committed countries to the 90–90–90 targets, which aim to bring HIV testing and treatment to the vast majority of people living with HIV by the end of 2020 and to reduce the amount of HIV in their bodies to undetectable levels, so they keep healthy and to prevent the further spread of the virus.
Globally, there have been remarkable gains across the HIV testing and treatment cascade. At the end of 2019, 81% of people living with HIV knew their HIV status, and more than two thirds (67%) were on antiretroviral therapy, equal to an estimated 25.4 million of the 38.0 million people living with HIV—a number that has more than tripled since 2010.
Gains in treatment effectiveness, as well as increases in the number of people who know their status and are on treatment, are reflected in the fact that viral load suppression levels among all people living with HIV increased by 18 percentage points between 2015 and 2019. Almost 59% of people living with HIV globally had suppressed viral loads in 2019. However, achieving the 90–90–90 targets results in a minimum of 73% of people living with HIV having suppressed viral loads, so the global target for the end of 2020 is unlikely to be met.
The COVID-19 pandemic also could have an impact on viral load. Early modelling showed that a severe disruption in HIV treatment could result in additional AIDS-related deaths in sub-Saharan Africa. Some countries have reported reductions in medicine collections of up to 20% in some areas and there have been multiple reports of people living with HIV not having enough antiretroviral medicine for a lockdown of more than 60 days, as well as reports of people having abandoned their HIV treatment due to a lack of food. However, monthly data from January to June 2020 reported by countries to UNAIDS have not shown substantial declines in the numbers of people currently on treatment over the six-month period.
Related

Update
Evaluation of UNFPA support to the HIV response
04 September 2020
04 September 2020 04 September 2020Within the UNAIDS Joint Programme, the United Nations Population Fund (UNFPA) is a co-convenor, together with other United Nations funds and programmes, on HIV prevention among adolescents, young people and key populations, as well as on decentralizing and integrating sexual and reproductive health and rights and HIV services. UNFPA also plays a technical role in prevention and condom programming within the Global HIV Prevention Coalition.
The UNFPA Evaluation Office undertook an evaluation to assess the performance of UNFPA in integrating its approach to supporting the response to HIV within the broader context of sexual and reproductive health and rights, population dynamics, gender equality and human rights for the period 2016–2019, the results of which have recently been published.
“The lessons and recommendations from this evaluation will strengthen the organization’s HIV response, to deliver stronger results during the United Nations Secretary-General’s Decade of Action to achieve the Sustainable Development Goals. The evaluation results are also particularly relevant as UNFPA channels its efforts to align its programming to respond to and recover from the COVID-19 pandemic,” said Marco Segone, Director of the UNFPA Evaluation Office.
Related

Update
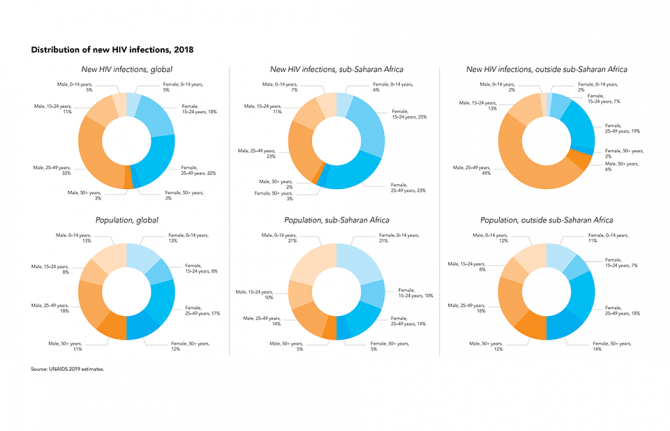
New HIV infections differ by sex and by region
08 June 2020
08 June 2020 08 June 2020In sub-Saharan Africa, where 61% of all new HIV infections occur, women are disproportionally affected by HIV, accounting for 54% of all new HIV infections in 2018. Young women aged 15–24 years were the hardest hit, accounting for 25% of new HIV infections in the region but representing only 10% of the total population.
Outside of sub-Saharan Africa, however, the situation is different, with men aged 25–49 years accounting for almost half of all new HIV infections, although they represent only 18% of the total population.
















