
Update
The high possible cost of COVID-19 on new HIV infections among children
19 May 2020
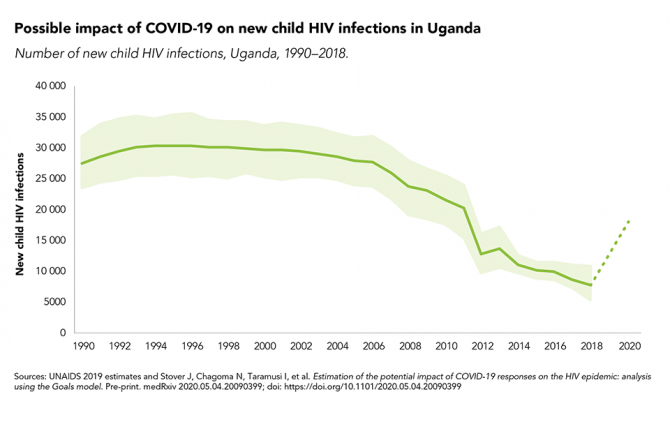
19 May 2020 19 May 2020New modelling has shown that the COVID-19 pandemic could have a major impact on new HIV infections among children in sub-Saharan Africa.
Since 2010, new HIV infections among children in sub-Saharan Africa have declined by 43%, from 250 000 in 2010 to 140 000 in 2018, owing to the high coverage of HIV services for mothers and their children in the region. However, if those services were disrupted because of the COVID-19 response, those gains would be reversed, with a six-month curtailment seeing new child HIV infections rising drastically, by as much as 83% in Mozambique, 106% in Zimbabwe, 139% in Uganda and 162% in Malawi.
There were approximately 30 000 new HIV infections among children (aged 0–14 years) per year in Uganda in the 1990s and early 2000s. The provision of antiretroviral medicines to prevent mother-to-child transmission scaled up from just 9% of expectant mothers living with HIV in 2004 to more than 95% by 2014, and that high coverage has been maintained since. New HIV infections among children (aged 0–14 years) plummeted to an estimated 11 000 in 2014; they further declined to 7500 in 2018. But the impact caused by COVID-19 could be high.
Our work
Related

Update
People with disabilities often left behind by HIV responses
12 May 2020
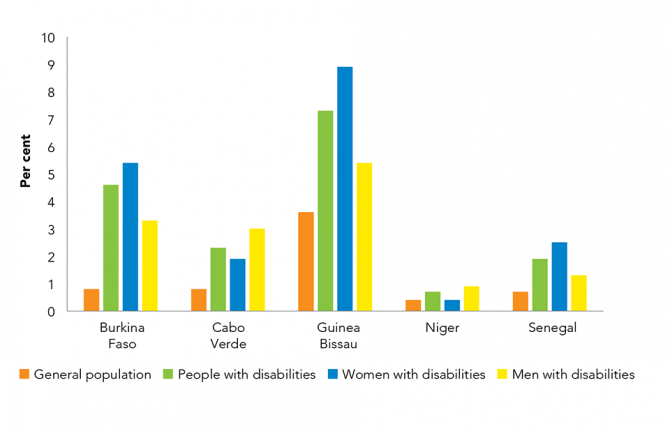
12 May 2020 12 May 2020Worldwide, there are 1 billion people living with a disability. The majority live in low- and middle-income countries and face multiple barriers, leading to inequalities. They are overrepresented among people living in poverty and among key populations affected by HIV and have lower participation in social, economic and public life and have lower economic, health and education outcomes. People living with a disability are also often left behind by HIV responses.
Between 2016 and 2018, biobehavioural surveys of people with disabilities were undertaken in Burkina Faso, Cabo Verde, Guinea-Bissau and Niger, while a broader biobehavioural survey was conducted in Senegal. They found that HIV prevalence is on average three times higher among people with disabilities than it is among the general population. In Burkina Faso, Guinea-Bissau and Senegal, women with disabilities were considerably more likely to be living with HIV than men with disabilities.
Our work

Update
HIV-related discrimination still widespread
04 May 2020
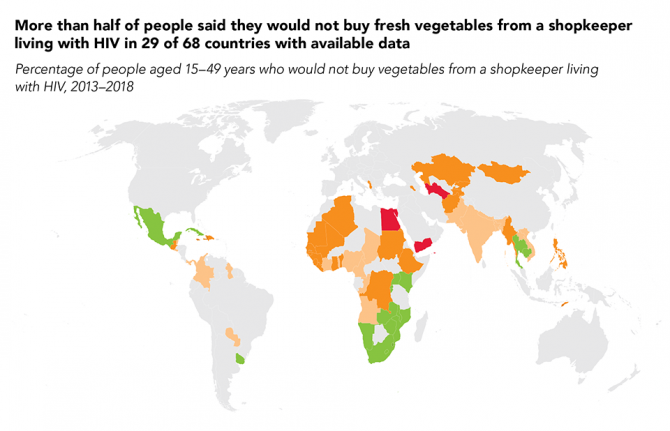
04 May 2020 04 May 2020Discriminatory attitudes towards people living with HIV remain extremely high in far too many countries. Across 26 countries with recent population-based survey data for a composite indicator developed by UNAIDS, more than half of respondents expressed discriminatory attitudes.
In 29 of 68 countries with available data on one of the two questions within the composite indicator between 2013 and 2018, more than half of people aged 15–49 years said they would not buy fresh vegetables from a shopkeeper living with HIV; in three of these countries, more than three quarters said they would not do so.
Resources
Related

Update
Women are more likely to be on HIV treatment
28 April 2020
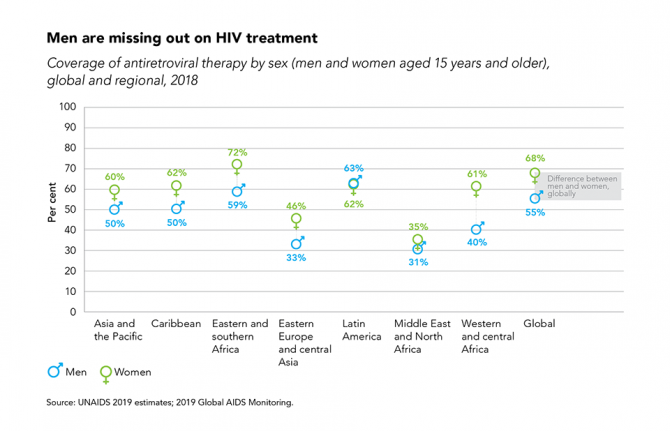
28 April 2020 28 April 2020Globally, among people living with HIV aged 15 years and older, coverage of antiretroviral therapy in 2018 was higher for women than for men. Numerous studies have shown that men are less likely than women to take an HIV test and to initiate and adhere to HIV treatment, which results in poorer clinical outcomes and a greater likelihood that they will die of AIDS-related causes. The low utilization of HIV services among men reflects general patterns of male health-seeking behaviour, which have been attributed to prevailing norms of masculinity, stigma, opportunity and other costs of attending health facilities, and inconveniently designed services (among other factors).
The disparity is seen across a range of geographic and epidemic settings. Regional estimates indicate that coverage of antiretroviral therapy was higher among women than men in all but one region with sex-disaggregated data. The disparity was most pronounced in western and central Africa, where an estimated 61% [32–67%] of women living with HIV were receiving HIV treatment in 2018, compared with 40% [18–41%] of their male peers. Treatment coverage for men and women differed by at least 10% in Asia and the Pacific, the Caribbean, eastern and central Africa, and eastern Europe and central Asia—trends that may reflect the fact that antenatal services have been a key entry point for HIV testing and treatment services in many regions.
Resources

Update
Wide differences in incidence–prevalence ratio by region
20 April 2020
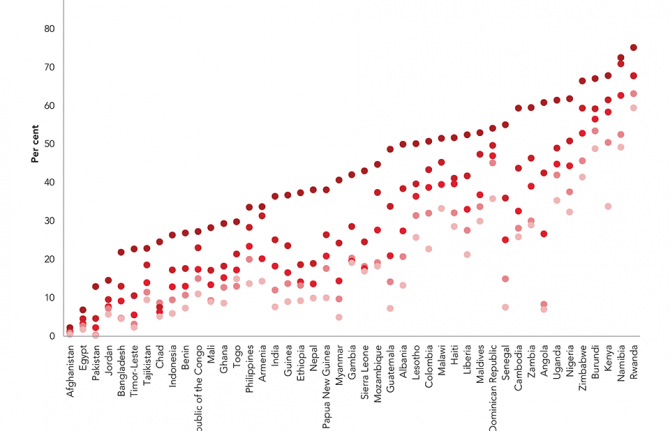
20 April 2020 20 April 2020While important progress has been made against the global incidence–prevalence ratio—which, while declining from 11.2% in 2000 to 6.6% in 2010 and to 4.6% in 2018, still leaves the world not on track to end AIDS as a public health threat by 2030—the progress is uneven across regions.
Western and central Europe and North America, where treatment coverage is generally high and a comprehensive set of HIV prevention options is available to a large percentage of people at risk of HIV, had an incidence–prevalence ratio of 3.1% in 2018. Performance in other regions ranged from 3.9% in eastern and southern Africa, 4.6% in the Caribbean, 5.4% in both Latin America and Asia and the Pacific, 5.5% in western and central Africa, 8.0% in the Middle East and North Africa and 9.0% in eastern Europe and central Asia.
Resources
Related


Update
Ratio of new HIV infections to number of people living with HIV improving
14 April 2020
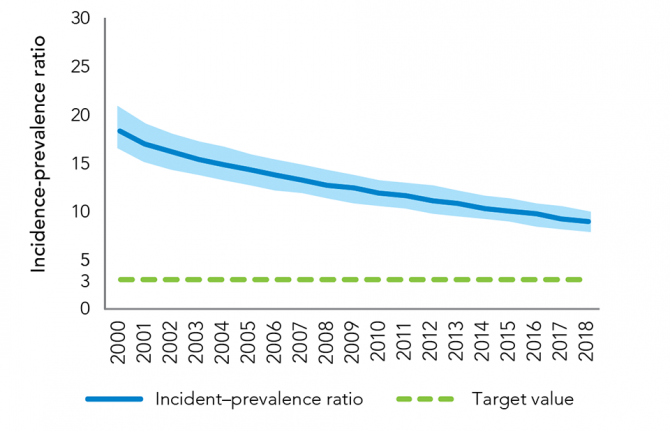
14 April 2020 14 April 2020Recent trends in new HIV infections and AIDS-related mortality can only show part of the story of the AIDS response. Epidemic transition metrics have been developed by UNAIDS and its partners as measures that countries can use to better track their progress towards ending AIDS as a public health threat.
One such metric, the incidence–prevalence ratio, uses the number of new HIV infections and the number of people living with HIV within a population. An epidemic transition benchmark of 3.0%—three HIV infections per 100 people living with HIV per year—corresponds to an average life expectancy after infection of 30 years. At this average life expectancy, the total population of people living with HIV will gradually fall if the country is below the 3% benchmark. The 3.0% benchmark thus combines two desirable conditions: long, healthy lives among people living with HIV and reductions in new infections.
The global incidence–prevalence ratio has declined from 11.2% in 2000 to 6.6% in 2010 to 4.6% in 2018, showing that important progress has been made against the HIV epidemic. Despite this, the world is not yet on track to end AIDS as a public health threat by 2030.
Resources

Update
HIV knowledge greater among women with higher incomes
06 April 2020
06 April 2020 06 April 2020Universal access to quality comprehensive sexuality education is crucial, especially for young people. It enables young people to make informed decisions and be empowered as they explore their sexuality and relationships. It helps them acquire the skills and values of mutual respect, tolerance, gender equality and non-violence, and it equips them with the knowledge they need to protect their health and well-being more effectively.
Levels of HIV knowledge vary across countries, depending on the national and local context, and they often are associated with social and economic inequities. In many countries, levels of comprehensive and correct knowledge of HIV among adolescent girls and women are low, but they tend to be lowest among those who live in poverty and those with lower levels of education. They also are lower among rural women than those in urban areas.
Resources

Update
Big shift to domestic funding for HIV since 2010
31 March 2020
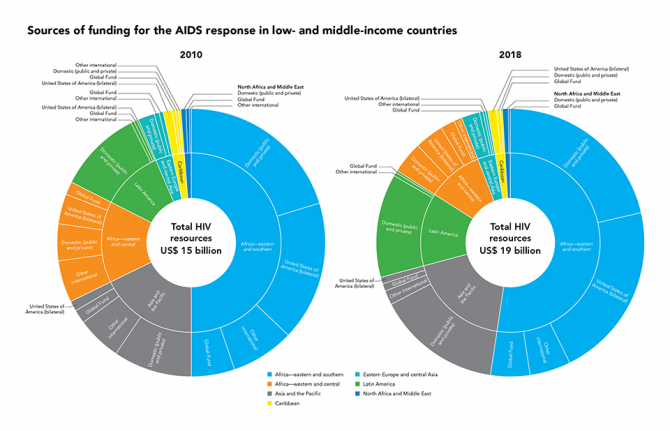
31 March 2020 31 March 2020There have been big changes in the landscape for funding the AIDS response since 2010. In constant 2016 United States dollars, overall funding in low- and middle-income countries increased from US$ 15 billion in 2010 to US$ 19 billion in 2018.
Within that increase in funding, there have been big changes in the sources of the funding. The amount of money that countries have invested in their own response to HIV has increased hugely, from US$ 7.1 billion to US$ 10.7 billion, equivalent to 56% of all funding. Bilateral aid from the United States of America increased from US$ 3.5 billion in 2010 to US$ 5.1 billion in 2018.
Other sources of funding have either stayed still or decreased, for example all bilateral funding other than that from the United States and all multilateral funding other than from the Global Fund—a worrying trend.
Even more worrying, however, is that UNAIDS estimates that US$ 26.2 billion will be required annually for the AIDS response in 2020—US$ 7 billion more than that available in 2018.
More information can be found on the UNAIDS HIV financial dashboard.
Resources
Video

Update
Tuberculosis—good progress, but not enough
23 March 2020
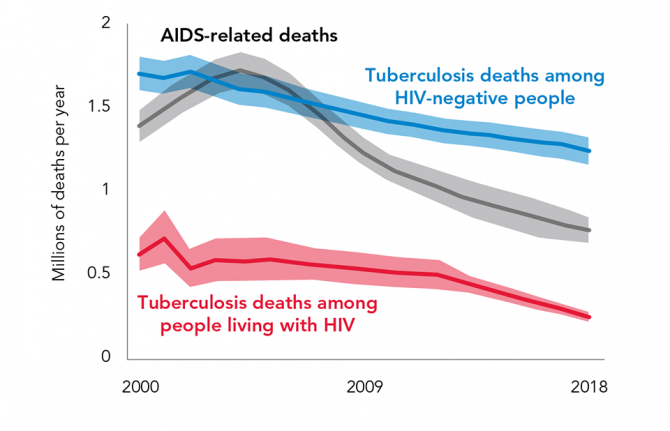
23 March 2020 23 March 2020Tuberculosis (TB) is the 10th leading cause of death worldwide, the worldwide top infectious killer and the leading cause of death among people living with HIV.
The good news is that TB is both preventable and curable, and countries have committed to end TB by 2030. The set of milestones committed to in the 2016 United Nations Political Declaration on Ending AIDS included a 75% reduction from 2010 in TB deaths among people living with HIV by 2020.
The bad news is that, in 2018, 10 million people fell ill with TB worldwide and 1.5 million people lost their lives to the disease, including 251 000 people living with HIV. While there has been a 60% reduction in deaths from TB among people living with HIV since 2000, the world is not on track to reach the 75% reduction by 2020.
As the world is commemorating World TB Day on 24 March in the midst of the COVID-19 pandemic, it is critical to remember that we need to sustain services for addressing TB epidemics and TB/HIV coinfections globally. There is still a US$ 3.3 billion yearly funding shortfall for TB prevention and care.
It is also timely to remember that programmes already in place to combat TB and other major infectious diseases can be leveraged to make the response to COVID-19 more rapid and effective. However, the need for an urgent response to TB, HIV or COVID-19 should not mean that human rights, autonomy and confidentiality are not respected.
The role of communities remains essential, as does the resilience of health system, for ensuring innovative people-centred and community-based and community-led approaches for service delivery, including differentiated service delivery models, digital health and innovative tools to diagnose TB infection and empower people living with HIV-associated TB to manage their treatment and care. Investments in systems for health, including communities, already made will make a real difference in the battle against COVID-19.
Resources
Related

Update
Parental consent undermines the right to health of adolescents
16 March 2020
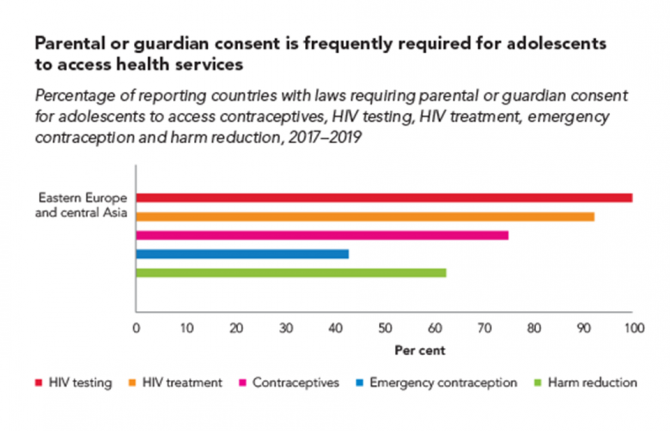
16 March 2020 16 March 2020Many countries have laws or policies that prevent adolescents from accessing essential health services without the consent of a parent or guardian. The original intention may have been to protect minors, but these stipulations often have the opposite effect and increase the risk of HIV and other health problems among adolescents.
A large proportion of countries across all regions restrict access to HIV testing and treatment for adolescents. In 2019, for instance, adolescents younger than 18 years needed explicit parental consent in 105 of 142 countries in order to take an HIV test. In 86 of 138 reporting countries, they needed such consent to access HIV treatment and care. These kinds of laws and policies also may complicate or hinder adolescent access to pre-exposure prophylaxis (PrEP), a highly effective prevention tool.
Research in sub-Saharan Africa shows that in countries where the age of consent is 15 years or lower, adolescents are 74% more likely to have been tested for HIV in the past 12 months compared with countries where the age of consent is 16 years or higher—with girls especially benefiting from the easier access.
Country-level details on which countries have consent laws can be viewed on the UNAIDS Laws and Policies Analytics web page.
















