

Update
Adolescent girls and young women in sub-Saharan Africa more than twice as likely to acquire HIV
09 March 2020
09 March 2020 09 March 2020Between 1995 and 2018, the steepest decrease in new HIV infections among women occurred among adolescent girls and young women (aged 15 to 24 years)—a decline of 44% globally. Prevention programmes that focus on this age group are having an impact.
Nonetheless, in 2018, approximately 6000 adolescent girls and young women acquired HIV each week, and they accounted for 60% of the estimated 510 000 new HIV infections in that age group. In sub-Saharan Africa, gender-related factors fuelling the epidemic are especially stark: adolescent girls and young women were more than twice (2.4 times) as likely to acquire HIV than their male peers.
The world is still a long way from achieving the global target of reducing new HIV infections among adolescent girls and young women to fewer than 100 000 by 2020: in 2018, that number stood at 310 000, three times higher than the target.
Related information

Update
Decriminalization works, but too few countries are taking the bold step
03 March 2020
03 March 2020 03 March 2020With the United Nations Commission on Narcotic Drugs meeting this week in Vienna, Austria, diplomatic attention is once again being given to drugs. In 2018, people who inject drugs accounted for 12% of worldwide new HIV infections.
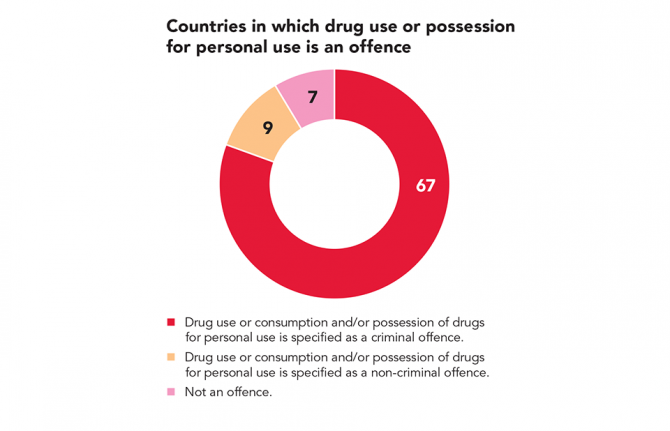
Laws that criminalize key populations or discriminate against people living with HIV undermine efforts to prevent new HIV infections and AIDS-related deaths in dozens of countries across all regions. Decriminalization of drug use and possession for personal use reduces the stigma and discrimination that hampers access to health care, harm reduction and legal services. In countries where drug use is decriminalized and comprehensive harm reduction is available, HIV prevalence and transmission tend to drop sharply among people who use drugs.
Czechia, the Netherlands, Portugal and Switzerland are among a handful of countries that have decriminalized drug use and possession for personal use and that have also invested in harm reduction programmes. Consequently, diagnoses among people who inject drugs in those countries are low.
With drug use or consumption and/or possession of drugs for personal use a criminal offence in at least 67 countries, it’s time for countries to take the bold step towards decriminalization.
Related information
Related


Update
Investing in HIV really does pay off
24 February 2020
24 February 2020 24 February 2020When countries agreed at the United Nations High-Level Meeting on Ending AIDS in 2016 to Fast-Track the response to HIV, one of the commitments they made was to scale up investment in the AIDS response. Although countries agreed to invest at least US$ 26 billion per year by the end of 2020, in 2018 total investments were just US$ 19 billion—a shortfall of some US$ 7 billion and a drop of US$ 1 billion from 2017, a worrying downward trend in overall funding for HIV.
However, the case for investing in the AIDS response is strong, and a recent analysis of costs and benefits using the full income approach by Lamontagne et al. (2019) has demonstrated the economic returns of ending the AIDS epidemic. It has been shown that under the Fast-Track approach—whereby a high upfront investment leads to large reductions in new HIV infections and AIDS-related deaths—each dollar invested brings up to US$ 6.44 of economic returns in low- and middle-income countries. Even under a more conservative constant-coverage scenario—whereby investment is such that coverage of HIV-related services were kept constant at 2015 levels and new HIV infections and AIDS-related deaths don’t fall—the economic return on each dollar is still positive, at US$ 2.55 in low- and middle-income countries.
The analysis shows variations among different world regions, ranging under the Fast-Track approach from US$ 1.05 in eastern Europe and central Asia to US$ 6.58 in Asia and the Pacific, but the central message remains: investing in HIV really does pay off.
Related resources

Update
Crisis in childhood HIV treatment in western and central Africa
17 February 2020
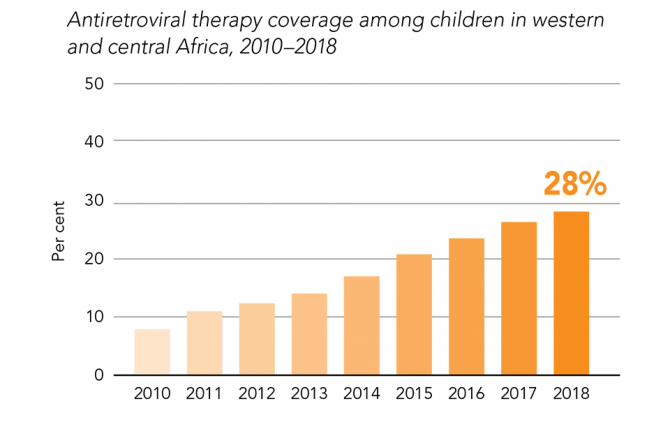
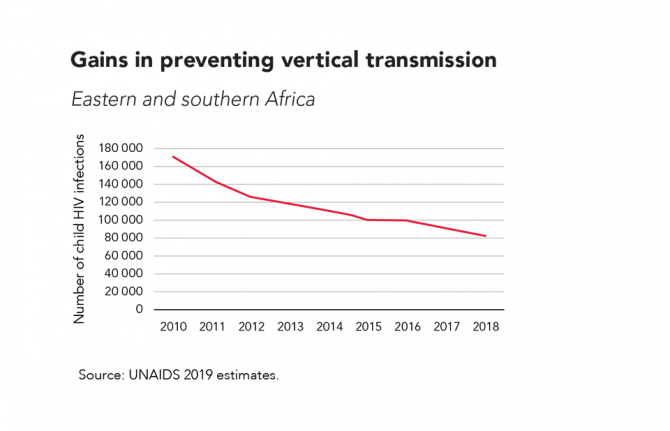
17 February 2020 17 February 2020In 2018, coverage of antiretroviral therapy among children living with HIV in western and central Africa was just 28%, far lower than the global average, which itself was only 54%.
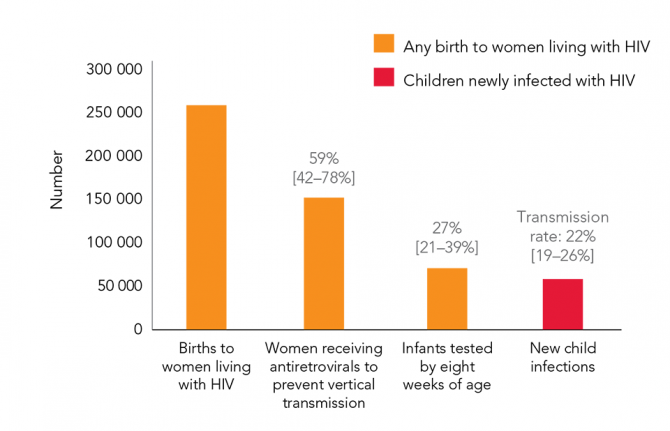
There are many reasons for the low childhood antiretroviral therapy coverage in western and central Africa. Too few children are being diagnosed in the region—with only 27% of infants exposed to HIV being tested for HIV infection within eight weeks of birth in 2018, there is an urgent need to expand access to early infant diagnosis.
The lack of accessible health services in many countries in the region results in children living with HIV being missed. If a pregnant woman doesn’t interact with antenatal care services, she isn’t tested for HIV, isn’t offered services to prevent vertical (mother-to-child) transmission of HIV and her baby isn’t tested for HIV—without a diagnosis, HIV treatment can’t be provided.
Even if a woman does see a health-care professional, the woman and her child are often lost to follow-up after delivery, with the HIV status of the child remaining unknown. HIV-exposed children need to be tested within two months of delivery and regularly re-tested up to the end of the breastfeeding period. Finding the missing children needs a scale-up of family index testing and HIV testing being offered where children get other health services.
Keeping mothers and children on treatment if they do start taking antiretroviral therapy is also important—far too many mothers and children begin HIV treatment only to later stop it. New and improved HIV treatments for children would also help to increase treatment coverage.
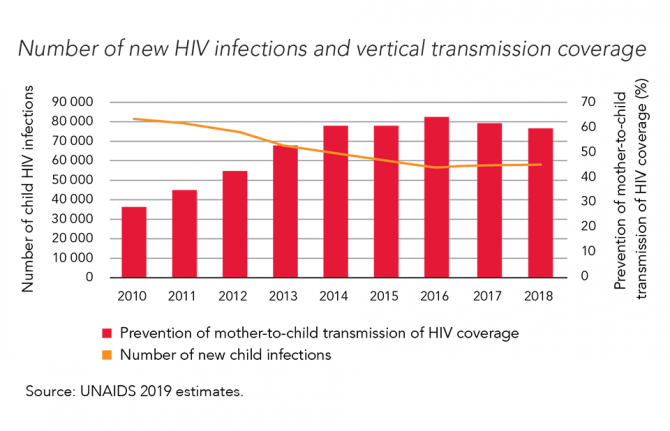
With no progress in recent years in preventing vertical transmission of HIV in the region, it’s no wonder that children living with HIV in western and central Africa are being left behind.


Update
How are babies becoming infected with HIV in Africa?
11 February 2020
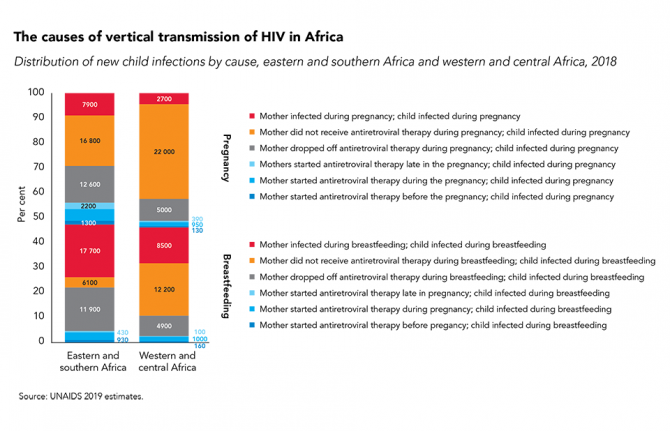
11 February 2020 11 February 2020In Africa, where a pregnant woman living with HIV lives has a big influence on whether her baby will be born HIV-free, and, if not, how her infant will acquire HIV.
There are a many reasons for vertical (mother-to-child) transmission of HIV, including: women not receiving antenatal and prevention of vertical HIV transmission services during pregnancy or breastfeeding; women starting antiretroviral therapy but falling out of care during pregnancy or breastfeeding; and women becoming infected with HIV during breastfeeding or pregnancy. However, not all countries face the same challenges, and to make rapid progress in eliminating vertical transmission it is crucial to know which means of transmission is contributing to the most new HIV infections among children in a country or region.
While the causes of vertical transmission of HIV in different regions vary, one thing is sure: far too many babies are still becoming infected with HIV.
Related

Update
Violence faced by key populations
27 January 2020
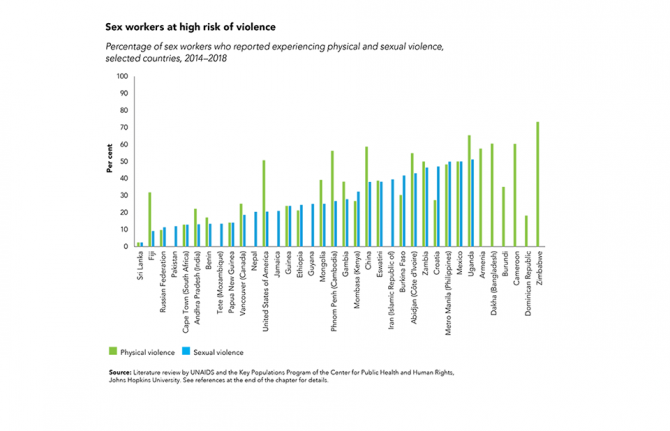
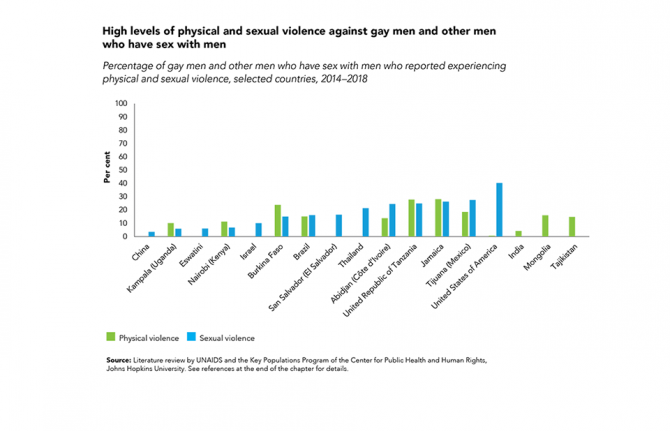
27 January 2020 27 January 2020Gains have been made against HIV-related stigma and discrimination, but discriminatory attitudes remain extremely high in far too many countries. Discrimination can manifest in criminal laws that give license to discrimination, aggressive law enforcement, harassment and violence, pushing key populations to the margins of society and denying them access to basic health and social services, including HIV services.
Surveys and studies across regions show that large percentages of key populations are victims of physical and sexual violence: among 36 countries with recently available data, more than half of sex workers in eight countries reported experiencing physical violence, and in two countries, at least half reported experiencing sexual violence.
In four of 17 countries with recently available data, more than one in five gay men and other men who have sex with men reported experiencing sexual violence.
Related information
Related

Update
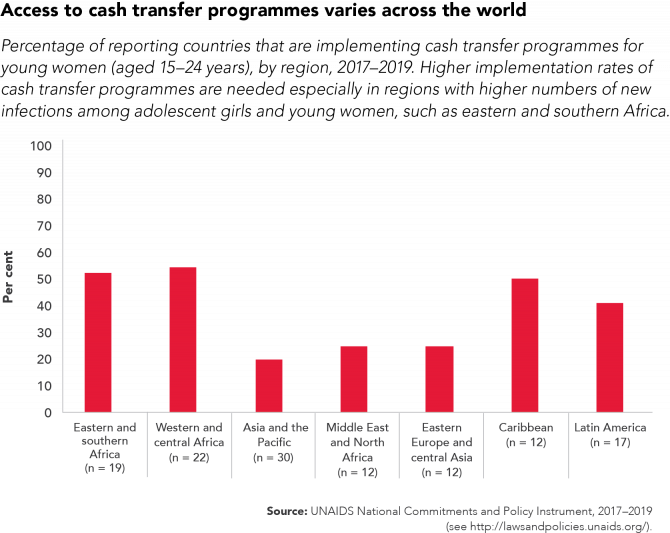
Cash transfer schemes reduce the chances of adolescent girls and young women contracting HIV
20 January 2020
20 January 2020 20 January 2020Efforts aimed at redressing gender inequalities and socioeconomic inequities can mitigate factors that fuel the HIV epidemic.
In a study in Eswatini, cash transfers aimed at keeping adolescent girls and young women in school and giving them greater financial independence resulted in the odds of the recipients becoming HIV-positive being 25% lower than for people who were not eligible for the incentive.
Studies from Eswatini, Lesotho, Malawi and the United Republic of Tanzania show that cash transfers help young people, especially girls, stay in school longer and do better in their studies. Other evidence indicates that cash grants that enable girls to continue their schooling also delay their sexual debut, increase their use of health services, reduce teen pregnancies and early marriage, and can promote safer sexual behaviours.
Related resources


Update
Young people and men less likely to know their HIV status
17 December 2019
17 December 2019 17 December 2019It is vital that people living with HIV know their HIV status. If people know they are HIV-positive, they can access treatment to keep themselves heathy. And when their treatment has reduced their viral load to an undetectable level, they can’t pass on the virus to their sexual partners. However, there are often large disparities in knowledge of HIV status, both geographically and by subpopulation.
In eastern and southern Africa, for example, young people and men living with HIV are much less likely to be aware of their status: while 90% of women living with HIV aged 25 years and above knew their status in 2018 (thanks in large part to the success of efforts to prevent mother-to-child transmission of HIV), that was the case among only 80% of men of the same age, 66% of young women (aged 15–24 years) and 50% of young men (aged 15–24 years). In western and central Africa, the gaps are even larger.
Resources
Related
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025

Update
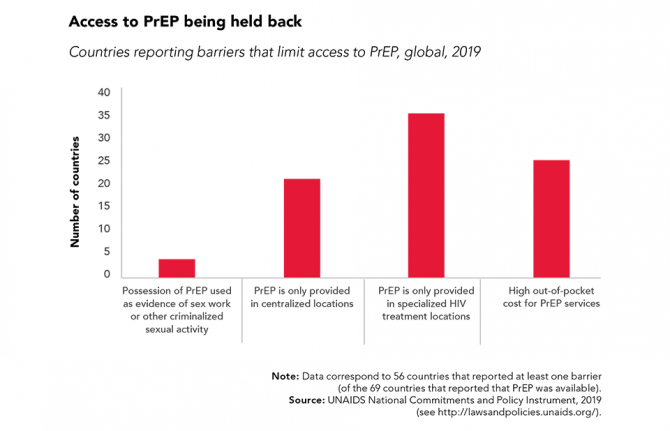
Barriers to PrEP must be removed
09 December 2019
09 December 2019 09 December 2019Oral pre-exposure prophylaxis (PrEP) has shown considerable impact in reducing new HIV infections when provided as an additional HIV prevention choice to gay men and other men who have sex with men, transgender people and sex workers.
PrEP is now being rolled out in sub-Saharan Africa for serodiscordant couples and adolescent girls and young women who are at higher risk of HIV infection. Uptake is high when community-level stigma and misconceptions are addressed, when women and girls are provided with accurate and relevant messaging about PrEP and when PrEP is framed as an empowering prevention method and a positive life choice.
However, further global expansion of PrEP requires countries to address regulatory issues and other barriers that are stopping people who want to use PrEP from doing so.


Update
Ending AIDS is everyone’s business
02 December 2019
02 December 2019 02 December 2019As we commemorate World AIDS Day 2019, we are reminded that despite some remarkable progress, the number of people becoming newly infected with HIV and dying from AIDS-related illnesses is not decreasing fast enough. We are reminded that despite this progress, there remains tremendous unmet needs. Resources for the AIDS response must be sustained. We are reminded that 38 million women, men and children are living with HIV today. We are reminded that despite global efforts, AIDS continues to be one of the greatest health and development threats of our time.
The response to HIV united the world in a way that no other health crisis has. It taught us that we must listen to and learn from the people affected, from the people most at risk. AIDS has taught us that we must address critical linkages―between health, injustice, inequality, poverty and marginalization. AIDS has also taught us that the challenge of ending an epidemic is far too great for any one sector to tackle alone.
Governments, nongovernmental organizations, civil society, communities and businesses each possess important, unique and complementary resources and capabilities to make a difference to the global AIDS response. When different sectors succeed in combining those assets, the impact increases significantly.
Business has been and continues to be integral to the AIDS response, from challenging the stigma surrounding HIV/AIDS, building vital collaborations with companies across industries, conducting treatment, diagnosis and prevention programs within workplaces and the surrounding communities, and more.
In every region of the world, today’s most successful businesses are an integral part of the societies around them. Businesses are recognizing that the well-being of their workforce and their partners, and of the communities they operate in and serve, are essential to their shared futures.
Ending the AIDS epidemic and leaving no one behind in the AIDS response will profoundly affect the lives of millions of people around the world, for generations to come, and businesses can make the difference. This is why we, as business leaders, are determined to play our part. We want to renew our commitment to ending AIDS.
We are urging businesses to engage in whatever way they can, by providing workplace HIV services to workers, dependents and communities, by offering skills, expertise and institutional resources, by partnering with the public sector and local nongovernmental organizations and community groups and by advocating at all levels to support people living with and affected by HIV. Business leadership on HIV has the potential to make a difference from the grass-roots level right up to the highest levels of global decision-making.
The future will be determined by what we do today. Guided by UNAIDS’ vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths, and working together with GBCHealth, we can make the difference, and together we can end AIDS by 2030.














