Update
New HIV infections rising in Latin America―key populations particularly affected
14 October 2019
14 October 2019 14 October 2019Although several countries in Latin America have shown impressive declines in HIV incidence, the number of new HIV infections in the region increased by 7% between 2010 and 2018, with 100 000 people contracting HIV in 2018.
Roughly half of the countries in the region saw increases in incidence between 2010 and 2018, with the largest increases occurring in Brazil (21%), Costa Rica (21%), the Plurinational State of Bolivia (22%) and Chile (34%). At the same time, there were impressive declines in El Salvador (–48%), Nicaragua (–29%) and Colombia (–22%).
Forty per cent of new HIV infections in Latin America in 2018 occurred among gay men and other men who have sex with men―key populations and their sexual partners account for the majority of new infections in the region.


Update
Criminalization of same-sex sexual relationships decreasing
07 October 2019
07 October 2019 07 October 2019Fifty years after the Stonewall riots in New York, United States of America―a major milestone in the modern struggle to recognize the human rights of lesbian, gay, bisexual, transgender and intersex people―more people are benefiting from the rights that the Stonewall protesters campaigned for. The number of people living in countries that criminalize consensual same-sex sexual relationships has steadily declined since 1969.
In June 2019, Botswana became the latest country to decriminalize same-sex relationships, but Africa still accounts for about half of the world’s population living in countries with anti-homosexuality laws. In 2018, the proportion of the world’s population that lives in countries that criminalize same-sex sexual relations plummeted from about 40% to 23% following the Indian Supreme Court’s decision that decriminalized all consensual sex among adults. This was the largest annual decline since China decriminalized same-sex sexual relationships in 1997.
Prohibitive laws and policies against key populations increase their vulnerability to HIV. It is therefore vital to ensure the full respect of the human rights of all people, regardless of their sexual orientation and gender identity, including through repealing laws that prohibit sex between consenting adults in private, enforcing laws to protect people from violence and discrimination and addressing homophobia and transphobia.
Consensual same-sex sexual relations remain criminalized in at least 67 countries and territories worldwide.
Related information


Update
Civil society engagement in universal health coverage
26 June 2019
26 June 2019 26 June 2019Achieving universal health coverage in a country is an ambitious, but transformative, goal. Communities are essential to the AIDS response and will be essential to the successful roll out of universal health coverage (UHC). When national governments establish a committee to coordinate UHC, it is important to ensure that all relevant communities are involved—civil society, including people living with HIV, should be included in decision-making. If civil society is not engaged early in the development of initiatives for UHC, decisions will be made about health services without the voice of the people most affected by those decisions. The graph below shows four ways in which communities contribute to the design and implementation of UHC.
Related information


Update
Young women more affected by HIV than young men in western and central Africa
18 June 2019
18 June 2019 18 June 2019In western and central Africa, survey data suggest that HIV prevalence among women aged 20−29 years is higher than that among men of the same age in all countries, and between five and nine times higher in some countries, including Côte d’Ivoire, the Gambia and Ghana. However, by the time they are 40−49 years old, men have similar HIV prevalence; exceptions to this are in the Democratic Republic of the Congo, Ghana and Gabon, where HIV prevalence among women is still almost twice as high in that age range.
The difference in HIV prevalence between men and women in the 20−29-year age group in western and central Africa is greater than that observed in eastern, and some southern, African countries. Possible reasons for this difference include the high rates of voluntary medical male circumcision in western and central Africa, which has been shown to have a 60% protective effect on female-to-male HIV transmission. Other possible reasons for the difference in western and central Africa might be the very low use of condoms and low uptake of antiretroviral therapy among men in the region.
Related information
Related


Update
Women who inject drugs more likely to be living with HIV
11 June 2019
11 June 2019 11 June 2019Drug use is more common among men, with women accounting for just one in three people who use drugs and one in five people who inject drugs. However, women who use drugs face special health risks.
Although few countries report sex-disaggregated data to UNAIDS on people who inject drugs, the majority of publicly available data suggest that women who inject drugs have a greater vulnerability than men to HIV, hepatitis C and other blood-borne infections. In 16 of the 21 countries that reported such data since 2013, women who inject drugs were more likely to be living with HIV than their male peers. In Germany, Uganda and Uzbekistan, HIV prevalence among women who inject drugs was almost twice as high as among their male peers.
Related information
Related

Update
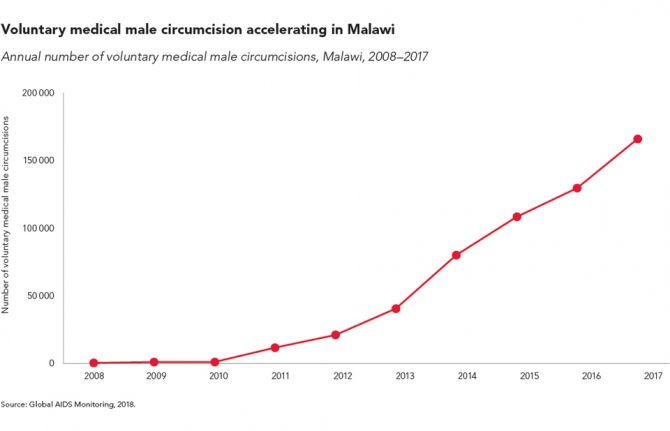
Voluntary medical male circumcision accelerating in Malawi
29 May 2019
29 May 2019 29 May 2019Voluntary medical male circumcision (VMMC) remains the only one-time intervention for reducing the risk of HIV infection. The procedure provides lifelong partial protection against female-to-male HIV transmission and should be used as part of wider sexual and reproductive health service provision for boys and men.
Scaling up VMMC in combination with condom promotion, pre-exposure prophylaxis, HIV testing and prompt initiation of antiretroviral therapy can have a major impact on HIV epidemics in high-prevalence settings. In Malawi, more than 165 000 circumcisions were conducted in 2017, more than double the number conducted in 2014 and up from just 589 in 2008.
In 2016, the United Nations General Assembly set a target of voluntarily circumcising an additional 25 million men in high-incidence countries by 2020, or 5 million men per year.
Related information
Region/country
Related
 “Who will protect our young people?”
“Who will protect our young people?”

02 June 2025
 Impact of US funding cuts on HIV programmes in Malawi
Impact of US funding cuts on HIV programmes in Malawi

15 April 2025


Update
TB-related deaths among people living with HIV falling, but not by enough
03 June 2019
03 June 2019 03 June 2019Even though tuberculosis (TB) is preventable and curable, it is the top infectious killer worldwide, claiming around 4400 lives a day. TB also remains the leading cause of death among people living with HIV, causing one in three AIDS-related deaths. However, progress has been made―TB-related deaths among people living with HIV peaked in 2005, at 600 000 deaths; since then, they have halved, to 300 000 in 2017.
Countries pledged in the 2016 United Nations Political Declaration on Ending AIDS to reduce TB deaths among people living with HIV by 75% by 2020. By 2017, five low- or middle-income countries had achieved or exceeded that target―a further 18 countries reduced TB deaths among people living with HIV by more than 50% and are on track to achieve the target by the end of 2020, provided that scale-up of services is maintained. However, the estimates also show that most countries are not on track and that deaths are rising in some regions and countries.
More on TB and HIV
Related information
Related
 Government ensures continuity of treatment in Malawi
Government ensures continuity of treatment in Malawi

10 February 2025


Update
People who inject drugs falling behind in access to HIV treatment
20 May 2019
20 May 2019 20 May 2019Progress has been made towards achieving the 90–90–90 targets whereby United Nations Member States committed to ensuring that, by 2020, 90% of people living with HIV know their HIV status, 90% of people who know their HIV-positive status are accessing treatment and 90% of people on treatment have suppressed viral loads.
However, people who inject drugs and other key populations are often being left behind. Among 13 countries that recently reported data to UNAIDS on treatment coverage among people living with HIV who inject drugs, eight stated that treatment coverage was lower among people who inject drugs than it was among the wider population of adults living with HIV.
Related information
Related


Update
HIV infections among children falling
13 May 2019
13 May 2019 13 May 2019The continuing fall in the number of children becoming infected with HIV is a major public health triumph. Globally, 1.6 million new child infections were averted between 2008 and 2017, an achievement that stems from a steep increase in the percentage of pregnant women living with HIV who receive antiretroviral medicines to prevent mother-to-child transmission of HIV or as lifelong therapy, from 25% in 2008 to 80% in 2017.
However, much remains to be done. Efforts to prevent mother-to-child transmission have been slowed by inconsistent treatment adherence among expectant and breastfeeding mothers living with HIV and by the significant numbers of pregnant and breastfeeding women with undiagnosed HIV. A high risk of HIV acquisition faced by women in Africa during pregnancy and breastfeeding has also been underappreciated.
Related information
Related


Update
Out-of-pocket expenses hamper access to HIV services
06 May 2019
06 May 2019 06 May 2019User fees and other out-of-pocket expenses―defined as direct payments made by people to health-care providers at the time of service use―are a major barrier to people getting tested for HIV, to people living with HIV being treated and to people living with HIV being retained in treatment and care.
Even if antiretroviral medicines are available free of charge, fees for diagnostic tests, consultations and medicines for opportunistic infections have a huge impact on people living on a lower income. User fees have also been shown to reduce access to health services more broadly among the more vulnerable within society. Out-of-pocket payments make up substantial proportions of total health expenditure in all regions, and in some low- and middle-income countries private out-of-pocket spending is estimated to account for more than 60% of total health expenditure.
According to the World Bank, around 3.4 billion people globally who earn US$ 5.50 a day or less are just one medical bill away from sinking into poverty.