Press Release
UNAIDS Executive Director and Inequality Council urge G20 to back bold network on medicine production and address the social determinants of pandemics
06 June 2024 06 June 2024SALVADOR, BRAZIL, 6 June 2024—At the G20 preparatory meeting in Brazil, Executive Director of UNAIDS and Under-Secretary-General of the United Nations, Winnie Byanyima, today urged governments to support a new G20 Alliance, proposed by the Brazilian government, to enable life-saving medicines to be produced in every part of the world. Co-Chair of the Global Council on Inequality, AIDS, and Pandemics Sir Michael Marmot also called on G20 delegates to address the social determinants of pandemics, such as education and human rights, as a concrete part of the G20’s pandemic preparedness efforts.
The medicines initiative aims to create a global alliance of local and regional manufacturers of drugs, vaccines and other health technologies and unite a diversified network of local and regional producers to ensure an adequate supply of medicines and technologies for everyone, everywhere.
Ms Byanyima called on the G20 to ensure that the alliance takes a bold approach that strengthens efforts to fight dengue and other neglected diseases, improves global defences against future pandemics, and accelerates access to the latest technologies against HIV.
“Focusing together on neglected diseases and the major killers of vulnerable people is not only strategic, it can deliver during future pandemics,” said Ms Byanyima. “We can be thankful that, for all its devastation, COVID-19 responded to a vaccine, unlike HIV. There is no reason to believe the next pandemic will be like COVID-19. We need to build capacity for vaccines and treatment.”
The responses to many diseases that impact vulnerable populations – from Ebola to Mpox to HIV – would benefit greatly from this initiative, Ms Byanyima told governments today.
“The alliance can supercharge the HIV response. It can supercharge the production pipeline for innovations,” said Ms Byanyima. “An alliance could also build capacity where it is not. The majority of people living with HIV, who get up every day and take that pill, live in Africa. But few of those drugs are actually made in African countries.”
“Brazil’s leadership and experience in this area has inspired this global effort. And we need the support of the whole G20 to make it a success.”
The agenda of the G20 meeting on health is helping to push global health policy towards tackling the systemic inequalities that drive ill-health. UNAIDS is coordinating a Global Council on Inequality, AIDS and Pandemics that is gathering evidence on how inequalities deepen and prolong pandemics, including HIV and COVID-19. That evidence is being shared with policymakers at the G20 and other international forums.
On Monday, world-renowned expert Sir Michael Marmot gave a keynote address the G20 meeting on the potential of focusing concretely on the social determinants to strengthen pandemic preparedness, predict the severity of future pandemics, and improve the efficacy of responses.
“Improving health leads to a better economy. And the way to improve health is not just to invest in healthcare, but in the social determinants of health,” Professor Marmot said. “For example, in Botswana, there is clear evidence that the longer young people remain in education, the lower the rates of HIV.”
Addressing social determinants, building manufacturing capacity, and enabling people everywhere to access the whole range of HIV prevention and treatment options, including the latest long-acting technologies, is vital for ensuring the end of AIDS as a public health threat. The G20 initiatives would play a key role in achieving that objective in a sustainable way, while also contributing to the achievement of the Sustainable Development Goals and supporting efforts to quickly respond to the next pandemic.
Notes for editors
Brazil's main proposal for the G20 Health Working Group is to establish the creation of an Alliance for Regional Production and Innovation. This initiative aims to establish a network that brings together key actors, including countries, academia, private sector, and international organizations, for research and development and production of vaccines, medicines, diagnostics, and strategic supplies to combat diseases with strong social determinants and that mainly affect vulnerable populations, such as dengue, malaria, tuberculosis, Chagas disease, and leprosy. For more information on the G20 Health Working Group, see the G20 website: https://www.g20.org/en/tracks/sherpa-track/health
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Learn more
Op-ed by Winnie Byanyima
Region/country


Press Release
Member States negotiating the pandemic instrument have an opportunity to save lives and keep the world safe, says UNAIDS
18 February 2024 18 February 2024As Member States enter the next stage of drafting and negotiating a new Pandemics Prevention, Preparedness and Response Accord, and the targeted revision of the International Health Regulations (IHR), UNAIDS underscores the importance of protecting the gains made in the AIDS response and encourages Member States to use that experience to help prevent and respond to future pandemics and health emergencies.
As part of the Sustainable Development Goals and the 2021 UN Political Declaration on HIV/AIDS, world leaders have committed to ending AIDS as a public health threat by 2030. COVID-19 increased HIV vulnerability and disrupted HIV service access for millions of people around the world. The colliding pandemics of HIV and COVID-19 also led to significant setbacks in the TB response. This experience illustrated powerfully how the impact of other pandemics has the potential to halt and reverse gains achieved in the fight against AIDS.
HIV remains an ongoing pandemic which would be affected by the impact of future pandemics. The actions necessary to make the world safer from future pandemics are vital for ensuring the end of AIDS as a public health threat and for protecting people living with and affected by HIV. Equally, doing what is needed to end AIDS will help keep the world safer from other pandemics.
At UNAIDS, efforts to support Member States in the pandemic treaty negotiations are rooted in evidence. At UNAIDS, we adhere always and only to facts, science, data and the lived experience of the people in the communities and countries where we work to support and guide the HIV response. We resolutely urge that all who are engaging in the negotiations do the same, standing for evidence, and categorically rejecting any misinformation, mischaracterization, or misattribution. The systematic use of facts and data in the HIV response has built public trust, and hugely contributed to advances in HIV prevention, testing, treatment and care.
Important lessons from the HIV response that can strengthen broader pandemic prevention, preparedness and response include:
- The infrastructure built up and strengthened to respond to the HIV pandemic – from lab systems, surveillance and health information systems, procurement and supply chain management through to community infrastructure and governance approaches – is vital for addressing other pandemics. For example, this infrastructure was widely deployed and played an essential role in helping countries to respond to the COVID-19 pandemic.
- Enabling equitable and timely access to scientific solutions, health technologies and medical countermeasures to all those in need is critical for saving lives and ending a pandemic. The role of regulation in ensuring the sharing of technology and know-how for generating local capacities in addressing pandemics is key.
- Tackling the inequalities which drive HIV and other pandemics is key to overcoming them. Closing social and economic gaps within and between countries will help the world to avoid the millions of preventable deaths the AIDS pandemic has seen from being repeated in future pandemics.
- Pandemic prevention, preparedness and response cannot succeed without mobilizing and enabling communities to lead themselves. Investing in community-led mechanisms is critical for successful prevention and response to pandemics.
- Human rights must be at the centre of all actions to prevent and respond to HIV and all other pandemics. The 2021 United Nations Political Declaration on HIV and AIDS, notes the need to “respect, promote, protect, and fulfil all human rights, which are universal, indivisible, interdependent and interrelated.”
- HIV has shown us that beyond being a health issue, a pandemic is a gender, social, economic, security, legal and human rights issue. Whole-of-government, whole-of-society approaches have driven progress in the HIV response. They should be employed at all levels of governance in pandemic preparedness and response.
The gains made and the lesson learnt in the global response to AIDS can help the world to be better prepared for the pandemics to come.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.


Press Statement
Pandemic Accord: UNAIDS offers lessons from the AIDS pandemic on Bureau’s text
24 July 2023 24 July 2023UNAIDS offers lessons from the AIDS pandemic on the Intergovernmental Negotiating Body Pandemic Accord Bureau text
GENEVA, 24 July 2023—The Joint United Nations Programme on HIV/AIDS (UNAIDS) offers lessons learnt from the HIV/AIDS pandemic to strengthen and sharpen the bureau text of the Pandemic Accord to ensure a truly robust response to current pandemics, and to prevent, prepare for and respond to pandemics of the future.
UNAIDS and the global response to AIDS have unique experience and insight over the past forty years in responding to pandemics. The global AIDS response has shown how effective a pandemic response can be which it outlined recently in its Global AIDS Update 2023 – The Path that Ends AIDS.
While COVID-19 increased HIV vulnerability and disrupted HIV service access for millions of people around the world, the AIDS response, systems, infrastructure and governance model also helped countries respond to both HIV and COVID-19. UNAIDS has a critical interest in protecting the gains in the HIV response, preventing future pandemics and health emergencies which impact people living with and affected by HIV and which could set back efforts to end AIDS by 2030.
Drawing on the more than a quarter-century as a global leader of the fight to end AIDS as a public health threat, UNAIDS offers the following lessons learned for strengthening the current bureau text of the Pandemic Accord:
General language
The current draft could be amended to incorporate much clearer, stronger language on the obligations of high-income countries (HICs) to ensure worldwide access to pandemic products and to proactively provide financial and technical support to enable pandemic responses in low- and middle-income countries (LMICs). The frequent use of “as appropriate” language could be replaced by clear language that conveys the obligation of states to act. In the current draft, much of the burden for prevention and surveillance falls on LMICs, without communicating clear obligations of HICs to assist and support LMICs. It could also have text that commits all countries to prioritise health and medical research.
Human rights and equity
While the draft identifies human rights and equity as core principles of pandemic preparedness, the draft could clarify language regarding the member states’ commitment to protect human rights and ensure equity in all aspects of pandemic prevention, preparedness and response (PPR). The accord could: reconsider the definition of “persons in vulnerable situations” (Art. 1); explicitly reference States obligations to protect and fulfil human rights within its “general principles” (Art. 3.1); mainstream concern for equity throughout provisions of the accord; emphasize formal and substantive equality, alongside non-discrimination, as general principles (Art. 3.1)
Equitable access
With respect to equitable access to pandemic-related products, the bureau draft uses language that suggests that recommended actions are advisory rather than obligatory. UNAIDS recommends that the draft :
- Clearly commit countries that possess pandemic-related medical technologies and knowhow to share it with LMICs in a timely and meaningful manner, including requirements in funding and purchasing agreements for institutions and companies in HICs to share intellectual property rights, technologies and knowhow with researchers and capable manufacturers in LMICs.
- Commit to provide robust financial and technical support for collaborative research between institutions in the North and South to build R&D capacity in LMICs – not only for pandemics and not only for manufacturing, but to enable LMICs to contribute to progress in science and technology for all of humanity.
- Countries to make full use of TRIPS flexibilities to address public health needs during a health emergency.
- Commit all states to waive intellectual property provisions for all pandemic-related products during pandemic and recovery periods.
- Commit Member States to provide political leadership and robust financial and technical support to build strong, flexible medical manufacturing capacity in LMICs before the next pandemic emerges. With future pandemics, surge support will be essential to adapt this capacity in LMICs to manufacture pandemic-relevant products.
- If and when demand for pandemic-relevant products outstrips supply during future pandemics, all Member States must commit to abide by WHO product allocation prioritization recommendations to ensure equitable access, with particular attention to the most vulnerable populations.
Access and benefit sharing
Although the draft specifies obligations among LMICs for actions pertaining to surveillance and the timely sharing of pathogens and data, the draft should be revised to commit Member States to ensure equitable access, including sharing the benefits and profits from the sale of these pathogens. Draw lessons from the Ebola where pathogens from Africa were shared but the medicines were stockpiled in the north leaving people in Africa waiting for charitable donations. The Accord should build on the precedence of the Pandemic Influenza Preparedness agreement (PIP) which facilitates sharing of pathogens and benefits both in terms of vaccines and profit.
Common but differentiated responsibility
While PPR is a shared responsibility of Member States, the draft could make clear that the nature and extent of responsibilities are differentiated based on each country’s financial and technological resources and capacities. As the effects of epidemics are felt most heavily in poor and vulnerable populations, countries that are home to these populations require additional assistance.
Inclusion of community and civil society
Community-led responses play critical roles in reaching marginalized communities with essential health messages and services during a pandemic – as both HIV and COVID-19 have shown – but communities remain under-resourced and inadequately integrated as key partners in national PPR efforts. The Pandemic Accord must acknowledge the central role of community-led responses and commit member states to include communities and civil society in decision-making, planning, preparation, implementation and monitoring.
Sustainable investments in health systems and infrastructure
Sustainable, resilient, well-resourced, equitable, human rights-based and people-centred health systems are essential to PPR and to efforts to achieve Universal Health Coverage. The HIV response has shown clearly how it is possible to leverage HIV investments to build stronger, inclusive, sustainable health and social service systems that respond to both HIV and other health threats. Drawing on previously recommended language on differentiated responsibilities based on national financial and technical capacity, the draft could clearly commit countries to invest major new public financing in health systems – ensuring a well-trained, well-remunerated health workforce (including community health workers); strengthening primary health care; ensuring access to health technologies (including those that are locally produced); and strengthening and effectively using health information systems.
Multisectoral governance
HIV has pioneered inclusive, accountable, participatory health governance across multiple sectors and with community, but there is a risk that PPR governance will be devised as a technocratic, top-down enterprise that does not include the central contributions of communities and civil society. The draft could insist that PPR governance mechanisms be fully inclusive of key stakeholders and integrated at national and regional levels to deal with current pandemics and future health crises. Language on whole-of-government and whole-of-society approaches should be strengthened.
Conclusion
Pandemics continue to exact enormous costs on societies across the world – an estimated 630,000 people died of AIDS-related causes in 2022, and long COVID will has lasting effects on human health and well-being and health infrastructure. In responses to HIV and COVID-19, too many countries and communities have been left to fend for themselves. Responding effectively to current and future pandemics requires the global community to summon the principles of solidarity, equity and people-centred action at the heart of the 2030 Agenda for Sustainable Development. Through learning by doing over decades, the HIV response has shown how it is possible to respond effectively to a pandemic. UNAIDS strongly encourages countries to take on board UNAIDS lessons learned when negotiating revisions to the bureau draft of the Pandemic Accord.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Documents
Synergies and sensemaking from pandemics—A comparative analysis of the proposed IHR amendments and the INB CA+ text
23 May 2023
Opening remarks by UNAIDS Executive Director Winnie Byanyima for the World Health Assembly 2023 side event Synergies and sensemaking from pandemics—A comparative analysis of the proposed IHR amendments and the INB CA+ text organised by Wits University, Open Society Foundations, the Permanent Mission of South Africa and UNAIDS
Documents
Dangerous inequalities: World AIDS Day report 2022
29 November 2022
This report, which marks World AIDS Day 2022, unpacks the impact that gender inequalities, inequalities faced by key populations, and inequalities between children and adults have had on the AIDS response. It is not inevitable, however, that these inequalities will slow progress towards ending AIDS. We know what works—with courage and cooperation, political leaders can tackle them. Read press release. Report introduction available in languages, including Arabic, French, Russian, Spanish.




Feature Story
Eastern Europe and Central Asia may face an accelerated increase in new HIV infections and AIDS-related deaths because of the humanitarian crisis gripping the entire region
28 October 2022
28 October 2022 28 October 2022Global shocks, including the COVID-19 pandemic and the war in Ukraine, have further exacerbated risks for the HIV response in Eastern Europe and Central Asia. The growing HIV epidemic and several waves of migration and refugee crises in the region require urgent and considerable efforts to ensure access to essential HIV services for all people in need. Officials and community representatives from several countries of the region have discussed how to address those challenges using the recommendations of the new Global AIDS Report “In Danger’ during the launch of the Report in Almaty, Kazakhstan.
When the Republic of Moldova faced the first wave of refugees from the war in Ukraine, with 500 000 people passing through within the first few months, there was not much time to prepare.
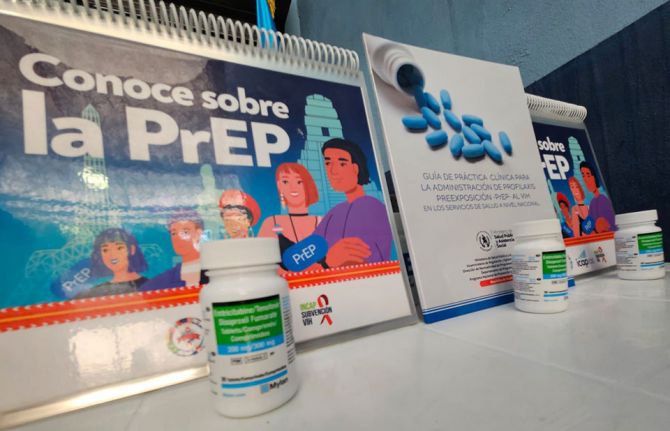
Svetlana Popovichi, National Treatment Coordinator in the Republic of Moldova, explained: “The Government prepared a legislative framework so that all people, regardless of their residence and available documents, have access to necessary HIV services. Civil society and community organizations worked day and night to connect us to people in need. Together with partners, despite the huge flow, we provided all the necessary services, including PrEP and treatment for pregnant women. We were able to quickly redesign our treatment plans so that everyone—our people and refugees—living with HIV had equal access to treatment and services.”
“This is our universal recommendation for countries in crisis,” said Gabriel Ionascu, UNAIDS Country Director in Kazakhstan. “All people, including foreigners, have to have access to HIV services, otherwise the infection will spread further.”
According to Azamat Dysenov, Director of the Treatment Department in the Ministry of Health of Kazakhstan, the availability of antiretroviral medicines for Kazakhstan citizens living with HIV in the country is 100%. Treatment and prevention programmes are funded from the state budget and available for all Kazakh people free of charge. He said: “Today we are facing new challenges, including active migration movements. We are ready to strengthen cooperation with neighbouring countries, maximize the potential of civil society, and work together to remove barriers to access to HIV services for all who need them.”
“Stigma and discrimination towards people living with HIV and other vulnerable groups, which are worsening during the humanitarian crisis, continue to be the major block to an effective response to the HIV epidemic in this region,” said Eamonn Murphy, UNAIDS Deputy Executive Director and Regional Director for Eastern Europe and Central Asia. “HIV transmission, exposure and nondisclosure are criminalized in all countries. While the majority of countries have decriminalized same-sex sexual relations, stigma against gay men and other men who have sex with men remains common.”
According to the UNAIDS Global AIDS Update: In Danger, in 2021, 160 000 [130 000–180 000] people were newly infected with HIV in Eastern Europe and Central Asia, a 48% increase since 2010. The number of AIDS-related deaths in the region in 2021, at 44 000 [36 000–53 000], is 32% higher than in 2010, despite expanding HIV treatment coverage and availability of new prevention methods and measures to control opportunistic infections. According to UNAIDS, in 2020, 54% of new HIV diagnoses in the region were detected at the late stage (CD4+ <350 cells), which is 10% more than in 2018.
Amir Shaikezhanov, an activist and AmanBol Project Director in Kazakhstan, said it is important to remember “there are people behind these facts and figures. Stigma is difficult to measure, but it hugely impacts access to HIV services for different groups. My friend just recently died from AIDS because he was not ready to disclose his gay status and HIV-positive status, even to doctors.”
The “transgender community has been excluded and not visible for a long time. It is great that the report pays attention to this group, including to a high level of stigma towards transgender people,” said Victoria Primak, a transgender activist in Kazakhstan.
According to the UNAIDS report, COVID-19 exposed an epidemic of violence against women across the region. Baktygul Ismailova, Director of the Network of Women Living with HIV in Kyrgyzstan, emphasized that women living with HIV need protection from violence at all levels.
The report’s recommendations for the region include maximizing the availability of community-led, people-centred services; removing punitive and discriminatory laws, especially those criminalizing HIV and people from key populations; national action; and international solidarity in providing sustainable financing.
“Over the past two years, community organizations have proven their ability to adapt quickly to new challenges, address problems quickly in crisis situations, and provide people with the necessary HIV services. We are ready to take on all the work of providing services to key groups. We have people, experience, knowledge and understanding of what exactly and how exactly needs to be done. Give us this opportunity!” urged Nurali Amanzholov, Leader of the Central Asian Association of People Living with HIV.
Recent developments in the region, including the war in Ukraine, massive waves of refugees and migration, humanitarian challenges and economic slowdown, bring additional challenges in providing HIV and other health-care services to all people in need and ensure sustainable financing. Domestic funding for the HIV response in the region may slow down, and countries that still depend on international resources will not be able to ensure the sustainability of AIDS programmes.
“Consolidated efforts of countries and increased support from the international community are urgently needed,” said Eamonn Murphy.
Watch: launch event (English interpretation)
Watch: launch event (Russian)
Region/country
- Eastern Europe and Central Asia
- Albania
- Armenia
- Azerbaijan
- Belarus
- Bosnia and Herzegovina
- Bulgaria
- Croatia
- Cyprus
- Czechia
- Estonia
- Georgia
- Hungary
- Kazakhstan
- Kyrgyzstan
- Latvia
- Lithuania
- Montenegro
- Poland
- Republic of Moldova
- Romania
- Russian Federation
- Serbia
- Slovakia
- Slovenia
- Tajikistan
- North Macedonia
- Türkiye
- Turkmenistan
- Ukraine
- Uzbekistan
Related


Press Release
UNAIDS warns that HIV, COVID and other health investments are in danger due to a looming debt crisis in Africa and the developing world
13 October 2022 13 October 2022In 2020 highly indebted countries already used four times more of their revenues on debt repayments than on health investments, reveals UNAIDS report A Pandemic Triad. The report was presented at an event hosted by Georgetown University in Washington DC during the Annual meetings of the International Monetary Fund (IMF) and the World Bank
WASHINGTON/GENEVA, 13 October 2022—COVID-19 and the debt crisis, now aggravated by the consequences of the war in Ukraine, have created an unprecedented setback in global health, and put the global response to AIDS in jeopardy, risking 7.7 million deaths to AIDS-related causes by 2030, according to a new report by UNAIDS.
The report, A Pandemic Triad, shows that the debt crisis and the war in Ukraine have deepened the fiscal crisis of developing countries, severely undermining their capacity to invest in health. It also shows that the countries most affected in economic terms by COVID-19 are the countries deepest in debt—they are also the countries most affected by HIV. In 2020, for every US$ 10 available, US$ 4 was spent on debt servicing and only US$ 1 was invested in health.
“The multilateral system cannot fail again,” said Winnie Byanyima, Executive Director of UNAIDS. “The response to COVID was dramatically inadequate, from very limited vaccination in developing countries to no permanent debt relief, and scarce fresh resources to countries with severe health and social problems—there can be no mistakes this time.”
The World Bank is forecasting that, without even including the latest numbers, 110 countries will have health spending in 2027 either under 2019 levels or slightly over, with only 67 countries. going above 2019 pre-COVID health investment levels.
The 2020 data show that there was a temporary increase in health spending, but it was focused predominately on the COVID emergency, leaving other health priorities behind. Latest forecasts from the IMF predict slower economic growth, higher inflation and worsening debt risks, leaving health and HIV investments under severe threat.
“We need a brave multilateral response to enable developing countries to respond to current pandemics and prevent future ones, while tackling the urgent food crises,” said Ms Byanyima. “Growing development cooperation, closing tax loopholes and promoting progressive taxation, providing fast and effective debt cancellation and relief, and avoiding the resource to austerity that would mean less doctors, nurses, midwives, is the way to go. New resources and resources freed from debt or tax dodging should be invested wisely to end AIDS by 2030 and respond effectively to future pandemics.”
A Pandemic Triad shows that of the 38 million people estimated to be living with HIV, 26 million are in developing countries and two thirds are in countries that received absolutely no debt relief at all despite the deep health and economic crisis brought by COVID.
The HIV response in low- and middle-income countries is US$ 8 billion short of the amount needed by 2025. In 2021, international resources for HIV were 6% lower than in 2010. It is estimated that the reduced availability of resources to finance access to HIV services could cost 7.7 million lives over the next decade.
The Global Fund to Fight AIDS, Tuberculosis and Malaria is seeking additional resources for countries´ investments in the fight against the three diseases.
Kalipso Chalkidou, Head of Health financing at the Global Fund said, “As the latest IMF World Economic Outlook figures illustrate, the outlook is dire for donor and recipient countries alike, with debt servicing severely constraining especially poorer nations' ability to spend in health and social causes. In this environment, Global Fund views debt swaps for health as a promising tool for creating badly needed fiscal space to invest in health systems and the three diseases."
On average, public debt levels in low- and middle-income countries rose from 55% to 63.8% of GDP between 2019 and 2020 equivalent to a staggering US$ 2.3 trillion and continue spiraling. Meanwhile currency depreciation to the US dollar of over 10%, and escalating interest rates payments are creating a perfect debt storm. For low-income countries (LICs), total debt is estimated at 87% of GDP. As a consequence, the proportion of LICs in debt distress, or at high risk of debt distress, has doubled to 60% from 2015 levels.
OXFAM presented the update of the commitment to Reduce Inequality Index at the Annual meetings and presented the latest data around inequalities in access to health.
Max Lawson, Head of Inequality Policy and Advocacy at Oxfam International said, “Our analysis shows that half of the poorest countries cut health spending, despite the worst health crisis in century. They are spending far more on repaying their huge debts to rich creditors in New York and London than they are able to spend on protecting their people from dying from diseases. This is an appalling situation, made more appalling because it does not have to be this way. Inequality is a policy choice, not an inevitability”.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Documents
Pandemic triad: HIV, COVID-19 and debt in developing countries
11 October 2022
This report analyses the intersection of HIV, COVID-19 and public debt in developing countries. The collision between COVID-19 and a crippling debt crisis have reversed decades of progress - putting present and future investments in health and HIV at risk. Pragmatic options to address the pandemic triad are proposed.




Feature Story
Pandemics are not fate: Concrete actions to tackle inequalities can overcome AIDS, Monkeypox and COVID-19
10 August 2022
10 August 2022 10 August 2022We do not need to accept pandemics as fate, experts gathered at the International AIDS Conference concurred. By taking specific, well-evidenced, concrete actions to tackle the inequalities driving them, today’s health threats can all be overcome.
As the latest data reveals that progress in the HIV response is stalling, putting millions of lives in danger, as the COVID-19 crisis drags on, and as Monkeypox presents new risks, all are being held back by inequalities, and all three viruses are in turn further exacerbating those inequalities. However, a focus on tackling underlying drivers of pandemic risk can enable a successful response, scientists, economists and heads of AIDS programmes concurred.
“There are Monkeypox vaccine doses in Europe but none in Africa. Most people at risk of dying from COVID-19 in lower-income countries have still not received a COVID-19 vaccine. New game changing prevention medicines for HIV will not be widely available in lower income counties for years unless there is a dramatic course correction,” said Winnie Byanyima, Executive Director, UNAIDS, and Under-Secretary-General of the United Nations. “An effective response to disease outbreaks and pandemics means tackling inequalities. That means empowering women and girls to shift power relations between men and women. It means tackling inequalities in access to health services between rich and poor. And it means removing punitive laws that push away from life-saving services LGBTQI+ people, people who use drugs, and sex workers.”
The application of scientific advancements is currently being undermined by inequalities, delegates at the International AIDS Conference noted. They recalled how, at the turn of the millennium, civil society and generic manufacturers teamed up to demand access to antiretrovirals for people living with HIV and their victory against the odds helped save millions of lives. But whilst that battle was won, delegates highlighted that the overall process of research and development, innovation and how that translates into manufacturing, pricing and distribution has remained untransparent and heavily skewed to the interests of rich countries. This played out during the COVID-19 pandemic as tests, vaccines and now antivirals are widely available in rich countries while still scarce in lower-income countries. And now this is repeating again with Monkeypox.
Inequality is not only about differential risks but is about cycles of power, the imbalance in how laws and policies are implemented, who is empowered by these policies, and who is disempowered.
“The AIDS movement is one of the best examples of how groups of people experiencing intersecting inequalities can unite to overcome them, leading to millions of lives being saved,” said Professor Joseph Stiglitz, Nobel laureate in economics. “But those gains were not permanent. Now a heating world combined with systemic inequalities mean that new disease outbreaks are becoming more frequent and while technological advancement is important, if there’s not a serious move to tackle inequality, the pattern of prolonged pandemics will only continue.” Professor Stiglitz was speaking at the AIDS Conference’s flagship session entitled “How Inequalities Perpetuate Pandemics: Why We Need a New Approach to End AIDS.”
New HIV infections occurred disproportionately among young women and adolescent girls, with a new infection every two minutes in this population in 2021. The gendered HIV impact, particularly for young African women and girls, occurred amidst disruption of key HIV treatment and prevention services, millions of girls out of school due to pandemics, and spikes in teenage pregnancies and gender-based violence. In sub-Saharan Africa, adolescent girls and young women are three times as likely to acquire HIV as adolescent boys and young men.
Worldwide, only half (52%) of children living with HIV have access to life-saving medicine, and the inequality in HIV treatment coverage between children and adults is increasing rather than narrowing.
Racial inequalities drive HIV too. In the United Kingdom and the United States, declines in new HIV diagnoses have been smaller among Black populations than among White. In Australia, Canada and the United States, HIV acquisition rates are higher in Indigenous communities than in non-Indigenous communities.
Sbongile Nkosi, Co-Executive Director of the Global Network of PLHIV stated “Our experiences to date remind us that responding to pandemics such as HIV and COVID-19 is not just about dealing with a medical condition, it’s also about the environment in which we live and how my social status will determine the care I receive. It means centering interventions around the needs of people, listening to people. When we talk about key populations, we tend to group people. But then we misunderstand inequalities. People live intersecting lives and inequalities affect them differently.” During the disruptions of the last few years, key populations have been particularly affected in many communities – with rising prevalence in many locations. UNAIDS data have shown increasing risk of new infections faced by gay men and other men who have sex with men (MSM) globally. As of 2021, UNAIDS key populations data show MSM have 28 times the risk of acquiring HIV compared to people of the same age and gender identity while people who inject drugs have 35 times the risk, sex workers 30 times the risk, and transgender women 14 times the risk.
Just as tackling inequalities has been key to progress in tackling HIV, so it is in tackling COVID-19. But too many COVID-19 responses have ignored this. “We have failed to learn a lot of the lessons from HIV/AIDS in the way we responded to COVID-19. And we need to be honest about that and reflect on where we go from here,” noted Executive Director of the Global Fund, Peter Sands.
“It's time not only to know your gaps but to close those gaps,” said Ambassador John Nkengasong, US Global AIDS Coordinator and Special Representative for Global Health Diplomacy.
Today’s inequalities are bleak. But the most important message is a hopeful one. We know how to end AIDS by 2030 and also how to overcome Monkeypox, COVID-19 and other current and future health threats: when we tackle the inequalities which drive health risks, we can keep everyone safe.
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.





Feature Story
Meet a Vaccine Champion overcoming vaccine hesitancy in Ghana
14 July 2022
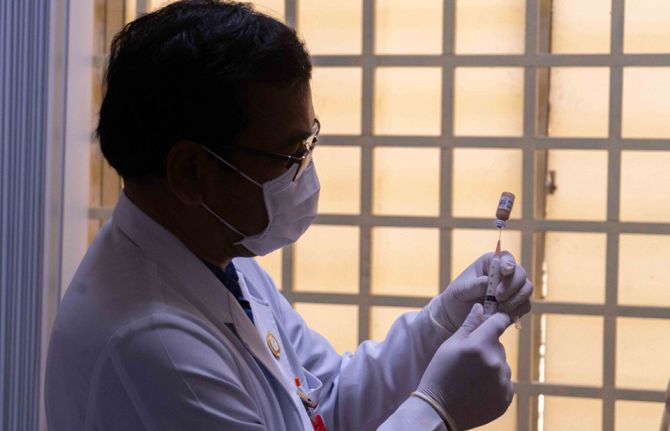
14 July 2022 14 July 2022On 24 February 2021, Ghana became the first recipient of a shipment of 600 000 COVID-19 vaccines under the COVAX initiative, a global effort to provide access to vaccination and curtail transmission of the virus in developing countries.
Joshua Appiah, who is living with HIV, was apprehensive about getting the Covid vaccine because he had been influenced by misinformation: “Some of what was circulating on social media frightened me. I was scared the jab would compromise my immune system and kill me!”.
After coming to learn that it is a lack of vaccination which poses a threat to health, particularly for people living with HIV, Joshua is angry at those who have promoted “misleading stories about the vaccine, its effects, the motivations behind its creation”. That is why Joshua decided to play his part. In June this year, he became one of 40 Vaccine Champions to undergo COVID-19 vaccination advocacy training, aimed at reinforcing their capacity to spread positive messaging and debunk “fake news”, myths and lies in their discussions with local community members. In turn, the programme hopes to increase vaccine uptake in local communities and among people living with HIV at ART sites, as Ghana continues to battle vaccine hesitancy.
The two-day training for Vaccine Champions was organised by Hope for Future Generations (HFFG), in partnership with the National Association of Persons Living with HIV (NAP+) Ghana, Young Health Advocates Ghana (YHAG), and the Ghana Red Cross Society (GRCS), with technical support from the Ghana Health Service. This activity falls under the Partnership for Accelerated COVID-19 Testing (PACT) 2.0 project, supported by UNAIDS and funded by the Government of Germany.
For Joshua, the topics covered, such as public sensitization on COVID-19, debunking myths and misconceptions, developing effective communication strategies, investigating the role of Vaccine Champions and working with data collection tools, have been enlightening and have empowered him to spread the word on vaccine uptake. “I took particular interest in the sessions on COVID-19 vaccine myths and misconceptions. I am now convinced that vaccines do not contain microchips, nor render people infertile, and I also feel comfortable spreading scientifically sound facts among the communities I am in contact with.”
In her opening remarks for the training in Accra, Executive Director of HFFG, Cecilia Senoo, described the current state of vaccine hesitancy as worrying, reinforcing the urgency of the project. She commended the Vaccine Champions for embarking on a “worthy cause” and encouraged the Vaccine Champions to remain devoted to their mandate. UNAIDS Ghana Youth Programs Officer, Eric Sinayobye, stated that, “vaccine hesitancy is a stumbling block to achieving mass immunity in Ghana, hence the need for Vaccine Champions to help educating members of the community”.
After the training, the 40 Vaccine Champions were deployed at ART sites and inside communities to provide education on the importance of getting vaccinated, as well as to help debunk myths surrounding the vaccines in the next three months. With funding from the Government of Germany, UNAIDS continues to work with the Africa Centers for Disease Control (Africa CDC) to strengthen community-led response against COVID-19 and HIV in Africa.
Region/country
Related
 Impact of US funding cuts on HIV programmes in Ghana
Impact of US funding cuts on HIV programmes in Ghana

08 April 2025