
Feature Story
Tuberculosis deaths among people living with HIV are declining globally, but worrying gaps in TB care persist
24 March 2021
24 March 2021 24 March 2021Globally, the number of people living with HIV who died from tuberculosis (TB), a curable and preventable disease, has fallen from almost 600 000 deaths in 2010 to just over 200 000 in 2019, a fall of 63%. In 2016, a global target was set by the United Nations to reduce TB deaths among people living with HIV by 75% between 2010 and 2020. Nine countries (Djibouti, Eritrea, Ethiopia, India, Malawi, South Africa, Sudan, Thailand and Togo) achieved or exceeded the global target by the end of 2019, one year ahead of schedule.
Further progress towards the global targets has been made in making TB preventive treatment more available to people living with HIV. TB preventive treatment greatly reduces their risk of falling ill and dying from TB. In just two years—2018 and 2019—5.3 million people living with HIV received life-saving TB preventive treatment. That is already 88% of the 6 million target set for 2022 in the 2018 United Nations Political Declaration to End TB.
While progress in some countries is to be applauded, these successes mask the many inequalities and gaps that remain in providing the best integrated care for people living with HIV and TB. These gaps resulted in an estimated 208 000 preventable TB-related AIDS deaths in 2019—about one in three AIDS-related deaths.
“One of the greatest disparities in the global response to HIV and TB is in reaching children,” said Shannon Hader, UNAIDS Deputy Executive Director for Programme. “Much better tools to prevent, diagnose and treat TB and drug-resistant TB for young children are now available, but they are still not enough. Too many children are still not being reached with these new tools. Some health-care workers lack the confidence to manage TB among children living with HIV and, for fear of causing harm and a desire to be protective, they don’t always act. Children are being “protected to death”. We need to build confidence to manage TB and HIV in young children and reach transformational goals.”
TB is especially difficult to diagnose among the youngest infants and children living with HIV—those less than two years of age. The most severe forms of TB—disseminated TB and TB meningitis—are common among this age group and they are life-threatening without prompt diagnosis and treatment. Major advances have been made in improving TB diagnosis for children. Child-friendly medicines for the treatment and prevention of TB are available at low cost from the Stop TB Partnership Global Drug Facility. The challenge is to take these innovations to the scale and quality needed to reach all children living with HIV in need.
The Rome Paediatric HIV & TB Action Plan, part of the UNAIDS and United States President’s Emergency Plan for AIDS Relief Faith Initiative, is closing the gaps for children living with HIV. It is a unique multistakeholder partnership that has stimulated unprecedented collaboration among the faith community, private sector, regulators, donors and others to accelerate the development and implementation of better diagnostic tests, preventive measure and treatments for HIV and TB among children living with HIV.
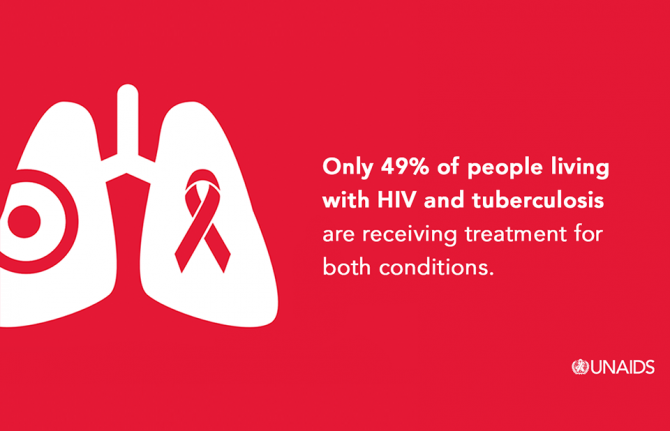
In 2019, less than half (49%) of the estimated 815 000 people living with HIV who also have TB disease were reported to be receiving both HIV treatment and TB treatment. This demonstrates that large gaps remain in screening, testing and treatment for both HIV and TB. To address this, national programmes need to go beyond traditional health facilities to find the missing millions of people who are still in need of treatment for HIV, TB or both. An integrated, community-based and person-centred approach is needed. Multidisease family and community screening for TB, HIV, COVID-19, high blood pressure, diabetes and other common conditions can be de-stigmatizing and can reduce costs for programmes and people. It is critical to encourage all people recently diagnosed with HIV, TB or COVID-19 to allow confidential screening of their family, household and community contacts, including children and young people.
Already, the clock is ticking for us to reach the ambitious new 2025 targets for TB and HIV laid out in the new global AIDS strategy for 2021–2026. Achieving these targets will place the world back on track to end AIDS and TB by 2030. A collaborative and integrated response to the pandemics of TB, HIV and COVID-19 is needed. The response must be rooted in affected communities and centred on the needs of the most affected people. Addressing the inequalities that drive TB and HIV will help to close the “deadly divide” between global commitments and the lived reality of TB- and HIV-affected communities. By ending inequalities, we can stop adults, young people and children living with HIV from dying of TB.



