Health systems strengthening

Feature Story
Jamaica: tackling HIV-related stigma and discrimination
19 November 2019
19 November 2019 19 November 2019Rachel Allen (not her real name), who lives in Kingston, Jamaica, was coming to terms with testing positive for HIV and trying to get on with her life. When she decided to go to nursing school, she was horrified to discover that the school required her to take an HIV test as part of the application process.
Jane Williams and Paul Brown (not their real names) were in love and wanted to start a family. But when health-care workers learned that Ms Williams was living with HIV, they expressed their disapproval. One nurse told her she shouldn’t have a child because of her status. One doctor called her “wicked”.
These are experiences that are all too common among people living with HIV, according to Jumoke Patrick, Executive Director of the Jamaica Network of Seropositives. The organization was set up in 2005 as a mechanism for people living with HIV to report rights violations. Now, the Jamaican Anti-Discrimination System (JADS) provides a system for the formal reporting of incidents and as well as a system of redress.
It’s an essential service, says Mr Patrick. He says that providing a channel for people to identify stigma and discrimination is a first step to allowing people living with HIV to access services and live full and productive lives.
“The fact that people are not accessing services has to do with stigma and discrimination,” Mr Patrick said. “That is why we have a fall-off in access to services. Stigma and discrimination is the main reason we are not where we are supposed to be in terms of getting people onto treatment. I have to know that when I disclose my status, you will not use it against me.”
People who have experienced prejudice in the health-care, education and employment sectors can report it to a JADS Redress Officer. Clients are often referred through a community facilitator in their health region, other civil society organizations or the Ministry of Health’s client complaint mechanism. Complainants fill out a form and are interviewed by one of the four redress officers in their district. A panel reviews each case and makes recommendations regarding an investigation. Agency and confidentiality are key. Some people opt out of seeing their complaints through, but those willing to go the distance have the benefit of an advocate.
“If you want redress you have to make a complaint, and you don’t have to be alone,” said Nadine Lawrence, a JADS Redress Officer. “It makes a lot of difference when you become empowered. You are able to get back into society and live a positive life.”
The most common cases are about treatment in health-care settings, breach of confidentiality and workplace harassment. Ms Lawrence has supported clients whose work colleagues disclosed their HIV status to their bosses. Others have had health workers from their community disclose their status.
What would she say to someone who has suffered an injustice but is reluctant to make a report? “Our organization exists so people who are HIV-positive can be more empowered. We sign a code of confidentiality. Trust the system,” she said. “Because it works.”
It worked for Ms Allen. JADS redress officers contacted the Ministry of Health to challenge the practice of requiring an HIV test to enrol in nursing school. The Ministry’s Legal Department intervened, sending a letter to the school advising it that the policy was illegal. The school’s board ultimately removed the HIV test requirement from its intake form.
The system also worked for Ms Williams and Mr Brown, who received a written apology. In addition, their complaint initiated a training programme for medical staff about the sexual and reproductive health rights of people living with HIV.
Focus on
Region/country
Related




Feature Story
Five years on: 300 Fast-Track cities come together
10 September 2019
10 September 2019 10 September 2019More than 700 delegates from cities around the world have gathered in London, United Kingdom, for the first Fast-Track cities conference. The meeting, hosted by the International Association of Providers of AIDS Care (IAPAC) in partnership with UNAIDS and the Global Network of People Living with HIV (GNP+), is focusing on the efforts and progress that cities have made as well as the challenges and lessons learned over the past five years.
On World AIDS Day 2014, the Fast-Track cities initiative was launched in Paris, France, with 26 cities signing up to the initiative. It has now expanded to more than 300 cities and municipalities.
In a dialogue on the imperative of ending health inequalities in cities, a high-level panel of mayors, governors, civil society organizations, parliamentarians, United Nations agencies and other stakeholders addressed health and social inequalities in cities big and small.
Speaking at the opening of the conference, Sadiq Khan, the Mayor of London, confirmed his commitment to the HIV Fast-Track response in his city, which accounts for 38% of all people living with HIV in the United Kingdom.
“I am proud of what we have achieved, but we need to go further,” Mr Khan said. “I wholeheartedly support the United Kingdom’s bold ambition to get to zero new HIV infections, zero AIDS-related deaths and zero discrimination.”
London was one of the first cities to exceed the 90–90–90 and 95–95–95 targets, with recent figures confirming that 95% of all people living with HIV know their status, 98% of those are on treatment and 97% of people on treatment have suppressed viral loads. He also advocated for making pre-exposure prophylaxis (PrEP) widely available, saying, “No ifs, no buts, PrEP needs to be made available to everyone ... it works.”
In addition to London and Amsterdam, Netherlands, which were the first two cities to reach 90–90–90, two other cities in the United Kingdom, Manchester and Brighton and Hove, have also achieved the 90–90–90 targets. In an analysis of data from 61 cities, it was reported that 14 cities have surpassed the first 90, another 16 cities have surpassed the second 90 and 23 cities have surpassed the third 90.
UNAIDS Executive Director, a.i., Gunilla Carlsson said, “The AIDS response can be a pathfinder for fostering resilience in cities. We need continued inclusive leadership from mayors working hand in hand with communities to address the many structural and social factors that contribute to people being left behind with no access to health services.”
Other cities highlighted examples of how innovation and creating an enabling environment can increase the scale-up of services. In Melbourne, Australia, for example, the response began early with bipartisan political support at all levels of government, galvanizing a partnership between political, community and scientific leaders. This has driven the virtual elimination of mother-to-child transmission of HIV and transmission among sex workers. And in Nairobi, Kenya, the city has reached antiretroviral therapy coverage levels of close to 100% among people who have been diagnosed with HIV. The city credits the success to better data gathering, which helped to identify the needs of key populations and young people living in informal settlements.
IAPAC President and Chief Executive Officer José Zuniga reiterated the importance of cities, where more than 50% of the world’s population live. “The Fast-Track cities calculus for success requires political will and commitment, community engagement, data-driven planning and equity-based approaches so that no one is left behind,” he said.
Fast-Track Cities 2019
Related press release
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025


Press Release
Global leaders unite to tackle health inequalities
09 September 2019 09 September 2019Delegates from more than 300 municipalities join global Fast-Track Cities conference on urban HIV, tuberculosis, and viral hepatitis
LONDON, UNITED KINGDOM, 9 September 2019 — London Mayor Sadiq Khan today welcomed city, municipal, and global leaders to Fast-Track Cities 2019, the inaugural conference of more than 300 cities and municipalities prioritizing their responses to urban HIV, tuberculosis (TB), and viral hepatitis. Speaking at the conference, Mayor Khan highlighted the problem of health inequalities across the world, as well as the need to end the stigma still associated with HIV. He also reiterated the bold ambition for London to achieve the target of no new HIV infections, deaths, and stigma by 2030.
“I’m honoured that city and health leaders from all around the world are uniting today in London. The first international gathering of Fast-Track Cities will be a truly historic event in our fight against HIV and health inequalities,” said Mayor Khan. “I’m also proud of the work London is doing to tackle HIV and inequality, and am pleased that we will be able to share our knowledge and experience with others. But despite our progress, there is still much more to be done as too many people continue to catch the virus. To truly end all new cases of HIV in London, it’s high time the Government made PrEP available via the NHS for all those who need it. No ifs, no buts, and no more pilots – we know it works, it stops the spread of infection and saves money in the long run.”
More than half of the world’s population currently lives in urban centers where the risk of contracting HIV, TB, and hepatitis is significantly higher due to urban dynamics such as social behavior, migration, unemployment, and social and economic inequalities. However, cities and municipalities also have inherent advantages and offer important opportunities to accelerate health responses and take transformative action to ensure that equitable access to health services is available to everyone.
“We have seen that for an effective response to HIV it is critical to remove inequalities, power imbalances, marginalization, and discrimination,” said Gunilla Carlsson, Executive Director a.i., of UNAIDS, one of four core partners of the Fast-Track Cities initiative. “Cities must use their advantages to leverage innovation, create social transformation, and build equitable societies that are inclusive, responsive, resilient, and sustainable,” she added.
Organized by the International Association of Providers of AIDS Care (IAPAC), in collaboration with the Joint United Nations Programme on HIV/AIDS (UNAIDS) and other partners, the Fast-Track Cities 2019 conference is being held from September 9-11, 2019, at the Barbican Centre. The conference’s aim is to highlight successes achieved across the Fast-Track Cities network, address cross-cutting challenges faced by local stakeholders, and share best practices in accelerating urban AIDS responses, inclusive of co-infectious diseases such as TB and viral hepatitis. The conference features plenary sessions, panel discussions, and abstract presentations by representatives from more than 300 Fast-Track Cities.
“Health inequalities are preventing people living with HIV, TB, and viral hepatitis, notably from disenfranchised and minority ethnic communities, from accessing the services they need to live longer, healthier lives," said Dr. José M. Zuniga, President/CEO of the International Association of Providers of AIDS Care (IAPAC), one of the core partners of the Fast-Track Cities initiative and the conference’s organizer. “We are convening in London because the city’s high level of political commitment, public health leadership, support from clinical and service providers, and engagement with affected communities have enabled the city to surpass the Fast-Track Cities’ programmatic HIV targets. We are here to shine a light on London’s efforts to reduce and eliminate health inequalities that contravene the principles of social justice.”
When London joined the Fast-Track Cities initiative in January 2018, the city had already met the UNAIDS 90-90-90 targets, which are defined as 90% of people living with HIV knowing their status, 90% of people who know their status accessing HIV treatment, and 90% of people accessing HIV treatment achieving viral suppression. FTC London, a pan-city group of stakeholders steering the city’s Fast-Track Cities engagement, has made outreach to the black, Asian, and minority ethnic (BAME) community a priority in their “London Getting to Zero” strategy.
The “High-Level Panel on Health Inequalities,” which was the official opening of the Fast-Track Cities 2019 conference, included the following elected officials:
- Kostas Bakoyannis (Mayor, Athens, Greece)
- Josefina Belmonte (Mayor, Quezon City, Philippines)
- Winston Ennis (Deputy Mayor, Kingston, Jamaica)
- Simone Kukenheim (Deputy Mayor, Amsterdam, Netherlands)
- Fernando Medina (Mayor, Lisbon, Portugal)
- Svante Myrick (Mayor, Ithaca, NY, USA)
- Robb Pitts (Chairman, Fulton County, Atlanta, GA, USA)
- Mykola Povoroznyk, (First Deputy Mayor, Kyiv, Ukraine)
- Gennadiy Trukhanov (Mayor, Odesa, Ukraine)
In addition to IAPAC’s Dr. Zuniga, and UNAIDS’ Ms. Carlsson, several global public health leaders also participated in the “High Level Panel on Health Inequalities,” including:
- Amb. Deborah L. Birx (US Global AIDS Coordinator, PEPFAR)
- Cary James (CEO, World Hepatitis Alliance)
- Suvanand Sahu (Deputy Executive Director, Stop TB Partnership)
- Maimunah Mohd Sharif (Executive Director, UN-Habitat)
- Trevor Stratton (Board Member, GNP+)
- Marijke Wijnroks (Chief of Staff, Global Fund to fight AIDS, TB and Malaria)
The panel was moderated by UK-based broadcaster and former BBC journalist Henry Bonsu.
Press passes for Fast-Track Cities 2019 are available by contacting IAPAC Director of Communications Zack Pesavento at zpesavento@iapac.org.
The conference program is available at: https://www.iapac.org/conferences/fast-track-cities/#program
About the International Association of Providers of AIDS Care (IAPAC)
With more than 30,000 members globally, IAPAC is the largest association of clinicians and allied health professionals working to end AIDS as a public health threat by 2030. For more information about IAPAC and our global activities, please visit: https://www.iapac.org/
About the Fast-Track Cities Initiative
Fast-Track Cities is a global partnership between almost 300 cities and municipalities, the International Association of Providers of AIDS Care (IAPAC), the Joint United Nations Programme on HIV/AIDS (UNAIDS), the United Nations Human Settlements Programme (UN-Habitat), and the City of Paris that are collaborating to end the epidemics of HIV, TB, and viral hepatitis by 2030. The initiative was launched on World AIDS Day 2014 in Paris. For more information please visit: https://www.iapac.org/fast-track-cities/about-fast-track/
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Documents
Global Partnership for Action to Eliminate All Forms of HIV-Related Stigma and Discrimination
15 June 2023
Without addressing HIV-related stigma and discrimination, the world will not achieve the goal of ending AIDS as a public health threat by 2030. Related: Operational guidance with checklist for tracking progress at country level. This document is also available in Portuguese.
Related
 How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them
How the shift in US funding is threatening both the lives of people affected by HIV and the community groups supporting them

18 February 2025
Impact of community-led and community-based HIV service delivery beyond HIV: case studies from eastern and southern Africa
30 January 2025
 Zambian football star Racheal Kundananji named UNAIDS Goodwill Ambassador for Education Plus in Zambia
Zambian football star Racheal Kundananji named UNAIDS Goodwill Ambassador for Education Plus in Zambia

23 January 2025
A shot at ending AIDS — How new long-acting medicines could revolutionize the HIV response
21 January 2025
Indicators and questions for monitoring progress on the 2021 Political Declaration on HIV and AIDS — Global AIDS Monitoring 2025
17 December 2024
Joint Evaluation of the Global Action Plan for Healthy Lives and Well-being for All (SDG 3 GAP)
16 December 2024
 To end AIDS, communities mobilize to engage men and boys
To end AIDS, communities mobilize to engage men and boys

04 December 2024


Feature Story
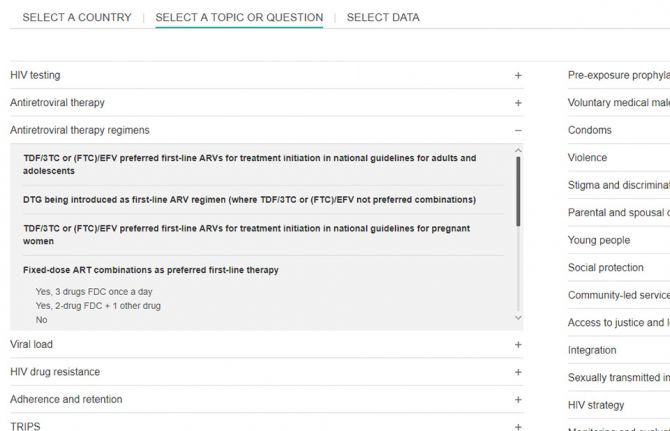
Mapping HIV laws and policies
31 July 2019
31 July 2019 31 July 2019A new website that enables people to identify national laws and policies related to the AIDS response has been launched by UNAIDS.
Covering areas as diverse as a country’s ability to diagnose HIV among young babies, the existence of laws that discriminate against transgender people and whether people are prosecuted for carrying condoms, the Laws and Policies Analytics website aims to give a full overview of a country’s laws and policies related to the HIV response. It also allows to view policy data jointly with other data on the HIV epidemic and response.
“We must better understand legal and policy environments to drive effective responses to the HIV epidemic. This new tool will provide access to data on national laws and policies and allow for joint analysis with data on the epidemic and response, so that we can drive more deeply-informed decision-making,” said Shannon Hader, UNAIDS Deputy Executive Director, Programme.
Under the 2016 United Nations Political Declaration on HIV and AIDS, countries committed to accelerate efforts to significantly increase the availability of high-quality data on HIV. The information used on the new website was reported since 2017 and most recently in 2019 through the National Commitments and Policy Instrument (NCPI), a part of the Global AIDS Monitoring mechanism through which countries report their progress against the commitments they made in the 2016 Political Declaration.
Data were provided by national authorities, civil society organizations and other nongovernmental partners engaged in the AIDS response. Data on HIV-related laws and policies compiled from other external official documents complement the nationally supplied data. UNAIDS carries out a thorough validation of all policy data included to ensure their accuracy. Data will be updated annually.
The website hosts data from over 140 countries. Users can search by country or region through an interactive map or can select a specific topic.
Through making policy data widely available, UNAIDS seeks to promote transparency and an increased use of policy data in analyses of the HIV epidemic and the response to HIV in countries worldwide.
The Laws and Policies Analytics website can be accessed at lawsandpolicies.unaids.org.
Laws and Policies Analytics website


Feature Story
“The staff at the clinic are very friendly. I am an old client so they all know me very well”
02 July 2019
02 July 2019 02 July 2019This story was first published by UNFPA
Windhoek, NAMIBIA - Sometimes it is best to go where everyone does not know your name, but where you feel welcome just the same. It is that way for many sex workers and men who have sex with men (MSM) in Namibia, who bear the brunt of criticism, repulsion and stigmatism in almost all aspects of their daily lives.
As a result, these men and women shy away from accessing essential health services, such as HIV testing/treatment, prophylaxis (PrEP), condoms, lubricants and contraceptives.
According to the first ever integrated bio-behavioral surveillance study (IBBSS) 2014, among MSM in Namibia, HIV prevalence among MSM was estimated to be 10.2 per cent in Keetmanshoop, 7.1 per cent in Oshakati, 10.1 per cent in Swakopmund/Walvis Bay, and 20.9 per cent in Windhoek the capital city.
The estimated HIV prevalence estimated among MSM in Oshakati and Swakopmund/Walvis Bay approximated that of the general population of adult males in the surrounding Oshana and Erongo regions, as measured by the Namibia Demographic and Health Survey, 2013.
HIV prevalence among MSM in Keetmanshoop was slightly lower than that of the general population of adult males in Karas Region, while HIV prevalence among MSM in Windhoek was nearly twice as high as HIV prevalence among adult males of the general population in Khomas Region.
Non-judgemental care
In 2018, the Namibia Planned Parenthood Association (NAPPA) with support from United Nations Population Fund (UNFPA) Namibia convened several advocacy meetings with key partners aimed at establishing a drop in centre at the Out Right Namibia offices.
Out Right Namibia is a Namibian organisation working with the lesbian, gay, bisexual, transgender and intersex (LGBTI) community aimed at advancing the rights, interests and expectations of the LGBTI community in Namibia.
Both the drop in centre and NAPPA Okuryangava clinic had flexible working hours to allow key population to access sexual and reproductive health (SRH) and HIV services at their convenient times, it also involved opening the clinic on Saturdays to allow key population to access services without fear of stigma and discrimination.
All service providers and staff at the drop in centre and clinic were trained and sensitised on the importance of quality, non-judgemental service provision to key population. The staff at Outright Namibia were also mobilised to build awareness and information about the services being provided at the drop in centre and clinic.
Pleasant experience
“I have had a very pleasant experience visiting NAPPA. As a sex worker, it is important that I feel comfortable and go to clinics where I’m free of judgement. NAPPA has opened their doors for me and I feel at home. There are no complications here as the services are free and I prefer this clinic over local hospitals,” said sex worker, Martha Keto (not her real name).
Keto, 30, has been a sex worker for almost 12 years and has been receiving PrEP treatment at the clinic since October 2017. ”I come regularly for my tests and for PrEP treatment which keeps me protected from contracting HIV. The testing I receive here not only keeps me updated on my HIV or STI status, but it keeps up with my overall health. I am informed about a lot of health information including my liver and the nurses are even able to tell if my alcohol consumption is too high,” she said.
“The staff at the clinic are very friendly. I am an old client so they all know me very well. I would recommend NAPPA services to my colleagues who are also workers. Their doors are always open for us, even during weekends we are able to come in if needed. There is a large number of sex workers in Namibia and I hope the services provided by NAPPA could be exposed so that more sex workers will be informed of the free services that are offered here,” she said.
Keto’s sentiments are shared by Cinton Nati and Gideon Markus, (not their real names) who are both homosexual males receiving services at the NAPPA clinic.
“If it had not been for the friendly staff at the NAPPA clinic and their constant support and encouragement, I would have not visited the clinic as recommended by the nurse,” said Nati. He said this made it easy for him to develop a personal relationship with the clinic’s staff because they were very encouraging and as a result, he was able to see major improvements not only in his health but also his confidence.
Prior to visiting NAPPA, Nati experienced emotional and mental difficulties associated with being newly diagnosed with HIV. As a result, he would often miss his appointments as he found it difficult to accept the reality of being newly diagnosed with HIV.
“Since the very first time my partner and I went to the NAPPA clinics, both at Out Right Namibia and at Okuryangava, we have been treated very well and the staff have gone out of their way to make us feel safe. I have had counselling sessions to make sure that I am doing alright and also checkups to make sure the medication is not having any side effects on my body and that I remain healthy. The staff at the clinics have also regularly checked that we understand how to look after ourselves and that we practice sound sexual health guidelines,” said Markus.
“Each time we visited the clinic at Okuryangava, Sister Fungai Bhera (Senior Registered Nurse) would first make time to chat to us about how we have been. This might sound like a small thing to others, but to me, it means the world as I know she cares about us and that I am taken care of and in safe hands,” said Van Den Berg.
He alluded: “LGBTI community in Namibia has never had proper support from our country’s leaders and as a result, there is still a lot of LGBTI people that get discriminated against and live in fear of their communities as we do not enjoy the same legal rights. Hence we live very secretive lives, sometimes even double lives. I think it is these secret lives that make it easy for LGBTI people in Namibia to land in situations where they are highly vulnerable to getting infected with HIV and other sexually transmitted infections.”
More KPs accessing services
In 2018, a total of 523 KPs were reached with sexual and reproductive health services at the two sites. This included 233 sex workers, 188 men who have sex with men 70 truck drivers and 32 women who have sex with women. A total of ten outreach events were held targeting KPs at various hotspots in Windhoek.
The comprehensive service package provided at the two sites included: HIV testing and counselling, those who tested positive were immediately enrolled for treatment; PrEP services, those who tested negative were also counselled and informed about PrEP services and those who agreed were enrolled on PrEP; family planning services including condoms; sexually transmitted infections (STIs) screening and treatment; and information education related to SRH, HIV and gender-based violence.
Region/country
Related
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025
 Status of HIV Programmes in Botswana
Status of HIV Programmes in Botswana

20 February 2025


Update
Out-of-pocket expenses hamper access to HIV services
06 May 2019
06 May 2019 06 May 2019User fees and other out-of-pocket expenses―defined as direct payments made by people to health-care providers at the time of service use―are a major barrier to people getting tested for HIV, to people living with HIV being treated and to people living with HIV being retained in treatment and care.
Even if antiretroviral medicines are available free of charge, fees for diagnostic tests, consultations and medicines for opportunistic infections have a huge impact on people living on a lower income. User fees have also been shown to reduce access to health services more broadly among the more vulnerable within society. Out-of-pocket payments make up substantial proportions of total health expenditure in all regions, and in some low- and middle-income countries private out-of-pocket spending is estimated to account for more than 60% of total health expenditure.
According to the World Bank, around 3.4 billion people globally who earn US$ 5.50 a day or less are just one medical bill away from sinking into poverty.
Related information
Related





Feature Story
Africa — Achieving health coverage without compromising on quality
08 March 2019
08 March 2019 08 March 2019Momentum for Universal Health Coverage (UHC) in Africa is building and many African countries have already integrated UHC into their national health strategies. But with 11 million Africans pushed into extreme poverty each year because of out-of-pocket health expenses, how can Africa achieve UHC which delivers a quality package of care for people living in Africa?
The UHC debate was buzzing in Rwanda’s capital Kigali this week during one of the largest health gatherings in Africa, the Africa Health Agenda International conference 2019. Co-hosted by the Ministry of Health of Rwanda and the African Medical and Research Foundation (Amref Health Africa), 1500 health leaders shared new ideas and home-grown solutions to the continent’s most pressing health challenges.
Participants discussed the need for countries to embrace the concept of UHC and do their utmost to make it work. They stressed that good health allows children to learn and adults to contribute to societies and the economy. They also underscored that it can allow people to emerge from poverty and provides the basis for long-term economic security, essential for the future of the continent.
Host country President, Paul Kagame was awarded the honour of excellence in recognition of his political leadership on UHC. In a tweet he thanked Amref saying, “We owe this progress to partners like you who have joined forces with us in our journey to deliver a dignified and healthy life for all Rwandans.” The Minister of Health of Ethiopia also received an award for Ethiopia’s work in promoting primary health care.
Ensuring that everyone has access to basic health services is a challenge and the key to the success of UHC will be ensuring that the quality of services is good enough to improve the health of the people who access them.
“We need to track the impact of UHC,” said Michel Sidibé, co-moderating a high-level ministerial panel. “Coverage is not enough, we need to be delivering quality, affordable, accessible services to all. The ultimate measure of success for UHC will be whether the poorest, the marginalized and the most vulnerable people are able to benefit.”
During the conference Mr Sidibé participated in a townhall with young people. He spoke to them about their meaningful engagement in the UHC process saying that young people need to ‘claim and own the space.’ He also talked to civil society groups about the remarkable progress towards achieving the UNAIDS 90-90-90 treatment targets across Africa and of the critical need of their continued engagement on HIV within UHC.
The first ever United Nations High-Level Meeting on Universal Health Coverage will take place on 23 September 2019 during the United Nations General Assembly under the theme ‘Universal Health Coverage: Moving Together to Build a Healthier World.’
Region/country
Related
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025
 Status of HIV Programmes in Botswana
Status of HIV Programmes in Botswana

20 February 2025


Press Statement
Message on the occasion of Universal Health Coverage Day
12 December 2018 12 December 2018Health is everyone’s concern. The world has been striving for access to quality and affordable health services since the Declaration of Alma-Ata, which called for health for all more than 40 years ago.
We have come a long way since then—improvements in access to, and the quality of, health-care services have increased life expectancy globally from 62 to 72 years. Yet progress is far from equal. Today, more than half of the world’s population do not have full access to essential health services, because they are unaffordable, inadequate, inaccessible for certain groups or simply unavailable.
There is increasing inequity around the world, with the richest 1% of the population now owning half of the world’s wealth. Life expectancy in the poorest countries of the world is appreciably lower than in the wealthiest, and living in areas blighted by poverty can mean a shorter life span and a lost future. The disparity is observed between countries and between different communities within countries, with the most vulnerable, marginalized and stigmatized being left behind.
Making progress towards universal health coverage that is truly universal means making progress towards equity, inclusion and social justice. It means a people-centred, human rights-based approach and community-led service delivery, as well as a recognition of the need to address the social determinants of health, including necessary reforms of laws and policies and removing stigma and discrimination and gender inequity.
The global response to HIV has illustrated the critical measures—decisive political leadership and commitment, community engagement and a response informed by scientific evidence—that can change the course of a global epidemic.
Reaching time-bound HIV prevention and treatment targets will make an important contribution to achieving the universal health coverage targets, and together will significantly accelerate progress towards realizing the Sustainable Development Goals.
In recognition of the theme of this year’s Universal Health Coverage Day, “Unite for universal health coverage: now is the time for collective action”, I call on everyone to embrace and contribute to the universal health coverage movement. United, we can make universal health coverage a reality for all.
12 December 2018
Michel Sidibé
Executive Director of UNAIDS
UNAIDS
The Joint United Nations Programme on HIV/AIDS (UNAIDS) leads and inspires the world to achieve its shared vision of zero new HIV infections, zero discrimination and zero AIDS-related deaths. UNAIDS unites the efforts of 11 UN organizations—UNHCR, UNICEF, WFP, UNDP, UNFPA, UNODC, UN Women, ILO, UNESCO, WHO and the World Bank—and works closely with global and national partners towards ending the AIDS epidemic by 2030 as part of the Sustainable Development Goals. Learn more at unaids.org and connect with us on Facebook, Twitter, Instagram and YouTube.
Press centre
Download the printable version (PDF)




Feature Story
New commitment to primary health care
01 November 2018
01 November 2018 01 November 2018Countries reaffirmed the fundamental right of every human being to the enjoyment of the highest attainable standard of health and committed to strengthen primary health-care services at the Global Conference on Primary Health Care. The Declaration of Astana, unanimously endorsed at the conference by all World Health Organization Member States, makes pledges in four key areas: making bold political choices for health across all sectors; building sustainable primary health care; empowering individuals and communities; and aligning stakeholder support to national policies, strategies and plans.
HIV disproportionately affects populations that are in many countries marginalized, stigmatized, discriminated against and criminalized. The new commitment to primary health care presents a timely and unique opportunity to step up efforts to address the many barriers that those populations face in accessing HIV and primary health-care services. Addressing such barriers requires having the courage to respond to issues that are often considered sensitive or taboo—around gender, sexuality, identity, exclusion and power.
“UNAIDS is proud to be leading on community and civil society engagement, as part of our contribution to the Global Action Plan for Healthy Lives and Well-Being for All. Only by taking AIDS out of isolation can we can save lives holistically, not disease by disease, issue by issue,” said Vinay P. Saldanha, Director of the UNAIDS Regional Support Team for Eastern Europe and Central Asia.
UNAIDS’ contribution to the event, The AIDS response and primary health care: linkages and opportunities, sets out examples of how to integrate HIV services into primary health care and, conversely, how to use the AIDS response to further leverage primary health care. It calls for urgent attention to be given to the structural and root causes of ill health and for sexual and reproductive health and rights to be central to primary health care.
The Global Conference on Primary Health Care took place in Astana, Kazakhstan, on 25 and 26 October.
Read the declaration
Region/country
Related
 Three Years On: From crisis to prospective recovery
Three Years On: From crisis to prospective recovery

20 February 2025