Health systems strengthening

Press Release
Global health organizations commit to new ways of working together for greater impact
16 October 2018 16 October 2018BERLIN, GERMANY, 16 October 2018—Eleven heads of the world’s leading health and development organizations today signed a landmark commitment to find new ways of working together to accelerate progress towards achieving the United Nations’ Sustainable Development Goals.
Coordinated by the World Health Organization, the initiative unites the work of 11 organizations, with others set to join in the next phase.
The commitment follows a request from Chancellor Angela Merkel of Germany, President Nana Addo Dankwa Akufo-Addo of Ghana, and Prime Minister Erna Solberg of Norway, with support from United Nations Secretary-General Antonio Guterres, to develop a global plan of action to define how global actors can better collaborate to accelerate progress towards the health-related targets of the 2030 Sustainable Development Agenda.
“Healthy people are essential for sustainable development – to ending poverty, promoting peaceful and inclusive societies and protecting the environment. However, despite great strides made against many of the leading causes of death and disease, we must redouble our efforts or we will not reach several of the health-related targets,” the organizations announced today at the World Health Summit in Berlin. “The Global Action Plan for Healthy Lives and Well-being for All represents an historic commitment to new ways of working together to accelerate progress towards meeting the 2030 goals. We are committed to redefine how our organizations work together to deliver more effective and efficient support to countries and to achieve better health and well-being for all people.”
The group has agreed to develop new ways of working together to maximize resources and measure progress in a more transparent and engaging way. The first phase of the plan’s development is organized under three strategic approaches: align, accelerate and account.
- Align: The organizations have committed to coordinate programmatic, financing and operational processes to increase collective efficiency and impact on a number of shared priorities such as gender equality and reproductive, maternal, newborn, child and adolescent health.
- Accelerate: They have agreed to develop common approaches and coordinate action in areas of work that have the potential to increase the pace of progress in global health. The initial set of seven “accelerators” include community and civil society engagement, research and development, data and sustainable financing.
- Account: To improve transparency and accountability to countries and development partners, the health organizations are breaking new ground by setting common milestones for nearly 50 health-related targets across 14 Sustainable Development Goals. These milestones will provide a critical checkpoint and common reference to determine where the world stands in 2023 and whether it is on track to reach the 2030 goals.
The Global Action Plan will also enhance collective action and leverage funds to address gender inequalities that act as barriers to accessing health, and to improve comprehensive quality health care for women and girls, including sexual and reproductive health services.
The organizations that have already signed up to the Global Action Plan for Healthy Lives and Well-being for All are: Gavi the Vaccine Alliance, the Global Fund to Fight AIDS, Tuberculosis and Malaria, the Global Financing Facility, UNAIDS, UNDP, UNFPA, UNICEF, Unitaid, UN Women, the World Bank and WHO. The World Food Programme has committed to join the plan in the coming months.
The final plan will be delivered in September 2019 at the United Nations General Assembly.
For more information, www.who.int/sdg/global-action-plan
Media enquiries
- Gavi, the Vaccine Alliance: Frédérique Tissandier; +41 79 300 8253; ftissandier@gavi.org
- Global Financing Facility: Melanie Mayhew; +1 202-459-7115; mmayhew1@worldbankgroup.org
- Global Fund: Ibon Villelabeitia; +41 79 292 5426; ibon.Villelabeitia@theglobalfund.org
- UNAIDS: Sophie Barton-Knott; +41 79 514 6896; bartonknotts@unaids.org
- UNDP: Adam Cathro; +19179159725; adam.cathro@undp.org
- UNFPA: Omar Gharzeddine; +1 212 297 5028; gharzeddine@unfpa.org
- UNICEF: Sabrina Sidhu; +1 917 476 1537; ssidhu@unicef.org
- Unitaid: Andrew Hurst, +41795616807; hursta@unitaid.who.int
- UN Women: Maria Sanchez Aponte; +16467814507; maria.sanchez@unwomen.org
- World Bank Group: Maya Brahmam; +1 202 361 2594; mbrahmam@worldbankgroup.org
- WHO: Christian Lindmeier; +4179 500 6552; lindmeierch@who.int


Feature Story
Better integration of mental health and HIV services needed
10 October 2018
10 October 2018 10 October 2018World Mental Health Day is observed on 10 October each year. This year, UNAIDS is highlighting that governments need to do more to integrate mental health and HIV services.
People living with HIV are at a greatly increased risk of developing mental health conditions, often suffering from depression and anxiety as they adjust to their diagnosis and adapt to living with a chronic infectious disease.
People living with mental health problems can also be at higher risk of HIV. The risks are exacerbated by low access to information and knowledge of HIV, including how to prevent it, injecting drug use, sexual contact with people who inject drugs, sexual abuse, unprotected sex between men and low use of condoms.
“HIV affects the most vulnerable and marginalized in society, who are also disproportionally affected by mental health issues,” said Michel Sidibé, Executive Director of UNAIDS. “By integrating HIV and mental health services we will be able to reach more people with the specialist care and life-saving support they urgently need.”
Currently, very few health services are addressing the HIV-related needs of people living with mental health issues or the mental health issues of people living with HIV. This situation needs to change. Studies conducted over five continents have estimated that HIV prevalence among people living with severe mental disorders could be between 1.5% in Asia and up to 19% in Africa.
People living with HIV can experience mental health issues that can affect quality of life and stop them seeking health care, adhering to treatment and continuing in care. Studies across 38 countries show that 15% of adults and 25% of adolescents living with HIV reported depression or feeling overwhelmed, which could be a barrier to adherence to antiretroviral therapy.
In addition, treatment itself can cause a wide range of side-effects on the central nervous system, including depression, nervousness, euphoria, hallucinations and psychosis. Studies in Africa found a 24% prevalence of depression among people living with HIV.
Identifying mental health issues among people living with HIV is critical; however, far too often those go undiagnosed and untreated. There are many reasons for this, all of which need to be addressed. People may not want to reveal their psychological state to health-care workers for fear of stigma and discrimination and health-care workers may not have the skills or training to detect psychological symptoms or may fail to take the necessary action for further assessment, management and referral if symptoms are detected.
Mental health services should ensure access to voluntary and confidential HIV testing and counselling for people who may be at increased risk of HIV. Primary health-care providers must be trained to recognize and treat common mental health and substance-use disorders and refer people to expert care.
Prevention, testing, treatment and care services must meet the complex medical, psychological and social needs of people affected by HIV and mental health issues, which can be best managed through integrated programmes. Integrated approaches need to be across sectors and involve social, legal, health-care and educational services and engage community-based organizations.
Integrating mental health and HIV programming prevents new HIV infections and improves the health and well-being of people living with and affected by HIV.


Feature Story
Learning lessons from the AIDS response to control NCDs
27 September 2018
27 September 2018 27 September 2018Noncommunicable diseases (NCDs) are by far the biggest killers of people worldwide, responsible for 71% of all deaths globally. Defined by the World Health Organization as diseases of long duration and generally slow progression, the four main types of NCDs, which account for 80% of all NDC premature deaths, are cardiovascular diseases, cancer, chronic respiratory diseases and diabetes.
People of all ages can be affected by NCDs, but they tend to affect older people. With increasing numbers of people living with HIV accessing treatment and hence living longer, people living with HIV are increasingly falling ill with NCDs. Being HIV-positive, however, also increases the risk of developing NCDs, either because of the infection itself or owing to side-effects of the medicines used to treat HIV. The care that people living with HIV receive therefore increasingly needs to include care for NCDs.
Since people in many low- and middle-income countries are smoking more, drinking alcohol more and becoming less active, and their diets are changing, rates of NCDs are increasing. Age-adjusted death rates from NCDs are nearly twice as high in low- and middle-income countries as in high-income countries.
However, the successes to date in the AIDS response show what can be done if countries take decisive action. It is becoming increasingly clear that if the world is to control NCDs, the lessons of the AIDS response need to be learned and applied to the response to NCDs.
Health-care systems in regions that are home to most people living with HIV were designed to primarily address acute, rather than chronic, illnesses. However, HIV programmes in those same countries can be good models for how to step up services for NCDs, showing how to provide continuity of care, support adherence to treatment and engage communities.
The AIDS response has had a huge impact on global health. The impact of early diagnosis and treatment, HIV services being in many countries the entry point for broader health services, the importance of tackling poverty and other social determinants of health, raising community awareness and creating demand for services, the importance of putting civil society and communities in the centre, with their engagement, activism, advocacy and mobilization—these are all key lessons from the AIDS response that can guide the response to NCDs.
“The response to HIV has shown that the impossible is possible,” said Michel Sidibé, the Executive Director of UNAIDS. “UNAIDS will work with our partners in the United Nations system to share best practices from the AIDS response to guide countries, communities and other partners.”
As part of the world’s effort to combat NCDs, on 27 September countries will come together in New York, United States of America, at the United Nations for the Third High-Level Meeting on the Prevention and Control of Noncommunicable Diseases. UNAIDS is a part of the United Nations Interagency Task Force on the Prevention and Control of Noncommunicable Diseases and will be sharing its knowledge at the high-level meeting.


Feature Story
Leaders from China and Africa come together to build stronger and healthier communities
10 September 2018
10 September 2018 10 September 2018Leaders from African countries and China met in Beijing, China, during the 2018 Beijing Summit of the Forum on China–Africa Cooperation (FOCAC) on 3 and 4 September to accelerate the social and economic development of Africa. Under the theme of “China and Africa: toward an even stronger community with a shared future through win–win cooperation”, the two-day summit served to further enhance Africa–China collaboration in eight key areas: industrial promotion, infrastructure connectivity, trade facilitation, green development, capacity-building, health care, people-to-people exchanges and peace and security. China’s President, Xi Jinping, also announced a US$ 60 billion package of aid, investments and loans to Africa.
During the official opening, the President of China emphasized that Africa has a lot of potential and is a continent full of hope. He said that China would launch a health-care initiative and that information cooperation and exchange on public health would be intensified. Cooperation programmes will be launched on the prevention and control of emerging and re-emerging communicable diseases, schistosomiasis, HIV and malaria.
The current Co-Chair of FOCAC, Cyril Ramaphosa, the President of South Africa, welcomed the new FOCAC initiatives, which will have a significant and lasting impact on peace, stability and sustainable development on the African continent. The current Chairperson of the African Union, Paul Kagame, the President of Rwanda, said that African countries will intensify work on industry, infrastructure and trade. Antonio Guterres, the United Nations Secretary-General, described FOCAC as an embodiment of two major priorities of the United Nations: to pursue fair globalization and to promote development that leaves no one behind. The Chairperson of the African Union Commission, Moussa Faki Mahamat, highlighted the need to further create synergy between the African Union’s Agenda 2063 and China’s Belt and Road Initiative.
Leaders agreed the Beijing Declaration and the Beijing Action Plan, which will serve as a blueprint for further cooperation between China and Africa in the next three years. The outcome documents, which list ending AIDS and halting and reversing HIV (together with tuberculosis and malaria) as part of the China–Africa health cooperation, also focus on sustainability in health and included the local production of medicines in Africa, strengthening systems and developing public health worker capacity as essential to achieving universal health care.
In bilateral meetings with the Presidents of Côte d’Ivoire, Equatorial Guinea, Mali and Sierra Leone, Michel Sidibé, the Executive Director of UNAIDS, highlighted the important contribution that China–Africa health cooperation can make to improving access to medicines and local pharmaceutical production in Africa.
The African Union endorsed the 2 million community health workers for Africa initiative, which was raised in the bilateral meeting with the President of Sierra Leone. Explaining to Mr Sidibé that he had recently visited a maternity hospital and learned that there are just two gynaecologists in the entire country, the President sees the community health worker approach as a key way to ensure that people are reached with essential health services.
Mr Sidibé met with the China–Africa Business Council, which also chairs the China–Africa Health Industry Alliance. China–Africa cooperation can generate transformational changes in health and provide a platform to find people-centred solutions for ending AIDS and expanding universal health coverage.
Resources
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025

Feature Story
Situation rooms bring actionable data to decision-makers
27 August 2018
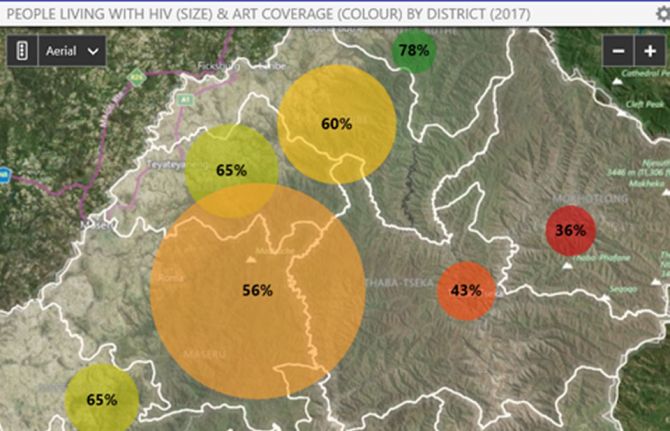
27 August 2018 27 August 2018Health situation rooms—software platforms designed to support decision-making on countries’ health responses—are opening up across Africa, bridging data and decision-making in order to improve the health and lives of tens of millions of the world’s most vulnerable people.
Data integration, data warehousing and data visualization are the core of the situation room concept, providing transparent and improved information on a range of diseases. While situation rooms are virtual working space, some countries also use physical rooms in which the analytics can be discussed and acted upon.
The idea of a health situation room is that data—whether on the availability of HIV medicines, the effects of a strike by health-care workers or diagnoses of cervical cancer—are centralized, yet accessible to everyone. Whereas in the past health data on different diseases would be spread around several databases in assorted government ministries, disease-specific organizations, etc., situation rooms collect the data in one place, on one system, in a form that is easily shared. The information held by the situation room can be utilized on tablets or computers throughout the country.
“We must continue to innovate in our response to HIV,” said Michel Sidibé, the UNAIDS Executive Director. “Having reliable and up-to-date information is vital if the world is to meet its commitment to end AIDS and reach the Sustainable Development Goals.”
By pooling the health data in the virtual situation room, better and more focused health services can be made available to the people who need them. For example, having data on specific parts of a city helps to drive a location–population approach to HIV prevention services, ensuring that the right people are reached in the right place with the right services.
Through combining data on, for example, HIV, tuberculosis and cervical cancer, interlinkages between the diseases can be seen and responded to. Data can be viewed in real time, so, for example, levels of HIV medicines can be monitored in order to anticipate and respond to medicine stock-outs. Studying the effects of HIV test and treat campaigns in Uganda, the effectiveness of cervical cancer screening in Côte d’Ivoire and malaria testing and new diagnoses in Zambia are other examples how health situation rooms are benefiting health responses.
Five countries—Côte d’Ivoire, Kenya, Lesotho, Zambia and Uganda—have launched situation rooms. Data on indicators, including on HIV, tuberculosis, malaria, noncommunicable diseases and reproductive, maternal, newborn and child health are gathered, with different countries collecting different information depending on the local situation. Namibia, Mozambique and Zimbabwe are preparing to launch situation rooms, and several other countries are in the planning stage.
As part of its work, UNAIDS has been helping countries to set up their situation rooms, with UNAIDS working with countries to select the specific indicators and connecting data in the country to their situation room. Countries with existing data collection systems, that collect data separated by age and sex and at the local level, that have good Internet connectivity and that have qualified local staff are best placed to establish their own situation rooms.
The situation room programme has resulted in UNAIDS’ support to countries being enhanced, with UNAIDS able to support health information systems in a way unique in the United Nations system. UNAIDS is therefore supporting country and programmatic monitoring in a more meaningful way in those countries that have invested in situation rooms.
“For us, its strength is in bringing multiple data sets together, and sharing powerful analytics in a visual and understandable way,” said Andrew Kashoka, Deputy Director of Information Technology, Zambia Ministry of Health.
For the future, UNAIDS plans to ensure that countries have technical support so that they can continue to operate their situation rooms without support from UNAIDS. UNAIDS will also work with partners, including the Africa Centres for Disease Control and Prevention, the private sector and others, to reduce the dependency of countries on UNAIDS’ support in setting up and running the platforms.
Such investments in technology and collaboration between UNAIDS, governments and partners are driving innovative approaches to responding to AIDS and to ultimately ending the AIDS epidemic as a public health threat by 2030.
Resources

Feature Story
Sustaining the HIV response in Latin America
26 July 2018
26 July 2018 26 July 2018Antiretroviral stock-outs are a serious public health problem in the Latin America region and represent an important risk to the sustainability of the HIV response, according to participants at AIDS2018.
On July 26, a session titled Sustainability of the response to HIV in Latin America; factors that impact access to drugs and health supplies addressed and analyzed the magnitude, the structural causes and the impact of stock-outs on the sustainability of the HIV response in Latin America. Participants discussed strategies to pave the way forward and highlighted best practices on joint purchases of antiretroviral (ARV) treatment like the PAHO/OMS strategic fund, which has helped prevent stock-outs.
In Latin America, one of the most important achievements in the HIV response has been the recognition that accessing HIV treatment is part of the right to health in the public health system, resulting in an increased number of people receiving antiretroviral treatment in recent years. However, a major challenge to fulfill the right to health is to guarantee uninterrupted supplies of ARV drugs and other essential health commodities.
According to the Pan American Health Organization (PAHO), in 2012 45% of the countries reported at least one stock-out episode; the figure had been 54% in 2010. Although some improvements are seen from 2010 to 2012, the region is still experiencing a high frequency of stock-outs.
Shortages of ARVs and other essential supplies result in changes and interruptions in patient treatment, threaten the lives of people with HIV and hamper the reduction of new HIV infections and AIDS-related deaths.
Participants at the session stressed the need for greater health system strengthening and joint procurement processes, including the incorporation of TRIPS flexibilities to reduce ARV costs, aligned with policies for simplified treatment regimens. According to participants, all these factors are essential to prevent and respond to stock-outs of ARVs and medical supplies.
Quotes
“Situations of stock affect the adherence to treatment, and consequently increases morbidity and mortality through opportunistic infections/diseases. It is fundamental and urgent the increase of public financing to increase the budget for prevention and treatment. The purchase mechanisms should be efficient and timely”
“Latin America continues to be the region with the highest coverage rate of antiretroviral treatment. About 1.1 million people in the region were accessing treatment in 2017, which represents 61% of people living with HIV. To close the gaps, it is key to Improve the management of national programs and planning so there are no stock-outs of medication.”
“Policies on access to generic medicines continue to be one of the key strategies for improving access to medicines, together with the strengthening of systems for the management and use of regional drug procurement mechanisms, including the PAHO Strategic Fund.”
"70% of countries have been or have been at risk of interruptions in delivery of drugs and / or supplies in the past 2 years. The main identified causes were related to the management of supplies "
“Civil society has been playing a key role in the monitoring and auditing public management and procurement in order to ensure universal access to health. And we can improve this work by using several tools that are available in different countries of our region such as the law that guarantees access to public information, follow-up of public procurement (including e-procurement) and open parliament.“
Region/country
Related






Feature Story
Catalysing zero discrimination in health-care settings in Thailand and Viet Nam
23 July 2018
23 July 2018 23 July 2018Stigma and discrimination in health-care settings is a major obstacle to ending AIDS. Widespread across the world, stigma and discrimination seriously reduces the quality of life of people who experience it and hinders their access to health and HIV services.
How to catalyse country initiatives and reduce stigma and discrimination in health-care facilities was the focus of a session at the International AIDS Conference on 23 July in Amsterdam, Netherlands. The session, Catalyzing Thailand and Regional Initiatives on Zero Discrimination in Healthcare Settings and Building Bridges Towards a Global Compact to Eliminate all Forms of HIV-Related Stigma and Discrimination, brought together representatives of the Governments of Thailand, Viet Nam and the Netherlands and representatives of regional civil society networks, the United States Centers for Disease Control and Prevention and UNAIDS.
Thailand is acknowledged as a pioneer in reducing stigma and discrimination in health-care settings in Asia through its innovative system-wide response. The event heard that the Thai stigma and discrimination reduction package is based on global measuring tools and contains a permanent monitoring system, evidence-informed actions at health facilities and community engagement at all levels.
Viet Nam piloted a stigma and discrimination reduction programme in Ho Chi Minh. At the session, Huu Thuy Do, Head of the Information, Education and Communication Department of the Viet Nam Administration for AIDS Control, explained how Viet Nam learned from cooperation with Thailand and how the Thai model was translated to the city level in Viet Nam.
Based on the experiences of Thailand and Viet Nam, speakers encouraged countries to foster cross-border links on stigma and discrimination reduction efforts in health-care settings in order to achieve more effective and efficient joint global action.
The participants also learned from the Dutch approach, which directs attention to the inequality of access to HIV prevention and treatment services while promoting an enabling legal environment to prevent stigma and discrimination.
The participants heard that the greater engagement of communities, people living with HIV and key populations in the development and monitoring of programmes against stigma and discrimination is a core element for successful stigma and discrimination reduction programmes. Their participation not only increases access by hard-to-reach communities, but also helps ensure that a rights-based approach is used.
The event concluded with the presentation of the Global Framework for Action, an initiative led by civil society that aims to catalyse and accelerate the implementation of commitments made to end HIV-related stigma and discrimination in different settings.
Quotes
“Thailand is a pioneer in the Asia region in developing a comprehensive programme to create health-care settings free from stigma and discrimination, leading to better health outcomes that go beyond HIV. In Thailand, we developed an intervention package that adapted global tools to our local context to stop stigma and discrimination. Stigma and discrimination is now systematically measured through surveys as part of that intervention package. The collected data are subsequently used to increase awareness, inform interventions and serve as a catalyst for system-wide actions.”
“What we should do is talk with religious leaders and talk with traditional leaders to make them see that discrimination and stigmatization is also a threat to society.”
“Discrimination at work links with health care. We find that people living with HIV all over the world face huge fears about disclosure, losing their jobs. Young people living with HIV have extremly high levels of unemployment.”
“Human rights, including stigma and discrimination and gender related vulnerabilities, are among the reasons for the serious HIV prevention gap and the insufficient progress that has been made in reducing new HIV infections in many regions of the world.”
"While HIV related stigma and discrimination are far from over, our experiences show that stigma and discrimination are both measurable and actionable. Reduction tools are available and when combined with collective leadership from key stakeholders and partners, we can end HIV related stigma through evidence based monitoring and effective interventions. Vision without action is just a dream but with action can make a difference. The world should unite to eradicate stigma and discrimination in all its forms."
"In the Thai model, the involvement of CSOs, PLHIV and KP’s goes beyond just an invitation to speak at a S&D reduction training. Communities are significantly involved in the entire process, from the programme consultation, planning over the implementation to the monitoring of progress."
Region/country
Related
 Status of HIV Programmes in Indonesia
Status of HIV Programmes in Indonesia

24 February 2025






Feature Story
Health is made at home, hospitals are for repairs
22 May 2018
22 May 2018 22 May 2018Calls to increase the number of trained and paid community health workers and reach more people with primary health care have been made for decades. However, countries are still struggling to expand the number of health workers serving in their own communities. This is despite overwhelming evidence of the gains made through such programmes in improving overall health, particularly maternal health and child health.
Rwanda’s investment in a combination of community-based insurance and community health workers led to the lowest maternal mortality in history for the country, showing that investments save lives.
“Africa bears 25% of the global disease burden, but has barely 3% of all health workers,” said Michel Sidibé, Executive Director of UNAIDS. “We need a shift in perspective to invest in community health workers to ensure healthy families and health security and to reach the people left behind.”
Forty years after the Declaration of Alma-Ata, which identified primary health care as the key to attaining health for all, global health leaders came together at an event to promote the effectiveness of community health workers by sharing their experiences and looking at ways of advancing the agenda on a global scale.
The event, convened by Ecuador and Ethiopia, was held on the sidelines of the 71st World Health Assembly in Geneva, Switzerland, on 21 May and joined together community health workers, ministers of health, programme managers, the Director-General of the World Health Organization, Tedros Adhanom Ghebreyesus, Graça Machel, a co-founder of the Elders, and Mr Sidibé.
Sunil Kumar, a community health worker in India, gave his account of how important medical services are to people in remote communities. He explained how he managed to reach a pregnant woman in a remote area of India in the rainy season. Despite a dangerously overflowing river, he and his colleague went the extra mile to ensure that her baby was delivered safely—a stark reminder of the unique added value of community health workers.
The Ministers of Health of Ecuador, Ethiopia and Namibia and the Permanent Secretary of the United Republic of Tanzania talked about the successes and challenges they are facing in trying to expand the number of community health workers in their countries.
The State Minister of Health of Ethiopia shared a successful model that has been scaled up in the country. Ethiopia now has more than 38 000 paid and trained health extension workers following the 2004 launch of the health extension programme, financed by a mix of government and international donor funds. The programme has made significant contributions to declines in maternal mortality, improvements in hygiene and sanitation and a reduction in major communicable diseases.
“We are seeing momentum for universal health coverage,” said Mr Tedros. “Primary health care is both promotion and prevention and community health workers are the backbone.”
In July 2017, the African Union Commission launched an initiative to recruit, train and deploy 2 million community health workers by 2020, an initiative championed by UNAIDS. UNAIDS, in close collaboration with the World Health Organization and the United Nations Children’s Fund (UNICEF), recently supported the African Union Commission to undertake the first stocktaking exercise on the status of community health workers across the whole of Africa. The findings and recommendations will be submitted to heads of state during the African Union Summit in June 2018. UNAIDS is supporting countries to implement this important initiative.
Although positive steps have been made, many countries are still struggling to scale up. “In Namibia, we adopted the Ethiopian model, as it has been so successful,” said the Minister of Health of Namibia. “We trained 2000 people, which is small for a population of 2.3 million, and not all have been deployed due to budget cuts, inefficiencies and fraudulent use of resources.”
Other challenges cited by the speakers include transport issues, a lack of technology and communications support, such as smart phones, and political leadership at the very top levels.
“Health systems need to be built from the bottom up,” said Bent Høie, Norwegian Minister of Health and Care Services. “And that starts with community health workers.”
Stefan Swartling Peterson, Chief of Health at UNICEF, embodied the sentiment of the meeting by sharing a saying his professor, Francis Omaswa, former Minister of Health of Uganda, often reminded him of, “Health is made at home, hospitals are for repairs,” and stressed that community health workers cannot be alone, that systems, supply chains and data management are needed to make the programmes a true success.
Urging for a global movement with every country making a commitment to increase the number of trained and paid community health workers, Graça Machel concluded by saying, “Let us not come back in 2030 and say we promised but we failed … it is not allowed.”


Feature Story
South Africa tests ATMs for medicine
03 May 2018
03 May 2018 03 May 2018People living with HIV and other chronic illnesses are getting faster, simpler access to essential medicines thanks to new medicine dispensing machines being piloted in Johannesburg, South Africa.
The non-profit organization Right to Care is testing three pharmacy dispensing units at a shopping mall and two hospitals. Most of the people using the new machines are accessing repeat prescriptions for HIV medicines.
The machines connect users to pharmacy assistants by video for remote consultations in any of the 11 official languages of South Africa. The entire process, from consultation to the release of the medicines from the machine, takes only a few minutes.
The machines are integrated with public health facilities responsible for patients with chronic conditions, in order to ensure that patients receive and adhere to effective treatments. The users of the machines get a printed receipt with the date of their next visit and receive a reminder by SMS. The system alerts pharmacists if patients are late to collect their medicines.
The device could be a game-changer for expanding access to HIV treatment. The South Africa UNAIDS Country Director, Mbulawa Mugabe, said, “One of our biggest challenges today in most countries in Africa is that health facilities are packed. We need to find ways in which we can relieve the congestion in the interest of patients themselves and also for the health systems.”
People living with HIV can often wait several hours to have their prescription filled at a local clinic. The process also takes up valuable time for skilled pharmacists. Now those tasks are being handled by junior pharmacists, who work with a robotic system to dispense pills in a matter of minutes.
The pharmacy dispensing units were engineered by Right to Care’s subsidiary Right e-Pharmacy in collaboration with the German company Mach4 and supported by German and American development agencies GIZ and USAID. The current trials are being conducted in collaboration with the Gauteng Department of Health and Right to Care hopes to expand the trial to two other African countries in the near future.
South Africa has the highest rate of HIV prevalence in the world and provides free treatment to 4.2 million people. The President of South Africa, Cyril Ramaphosa, recently set a target of expanding HIV treatment to an additional 2 million people by 2020. With millions of South Africans accessing medicines from clinics and hospitals, innovations such as these dispensing machines promise to help South Africa achieve its ambitious targets.
South Africa tests potential game-changer in HIV treatment
Zaheer Cassim reports for VOA from Alexandra township in Johannesburg.
Related
 U=U can help end HIV stigma and discrimination. Here’s how
U=U can help end HIV stigma and discrimination. Here’s how

27 February 2025
 Comprehensive update on HIV programmes in South Africa
Comprehensive update on HIV programmes in South Africa

25 February 2025
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025




Feature Story
Advocating for zero discrimination in health-care settings in Kenya
08 May 2018
08 May 2018 08 May 2018Like many women in sub-Saharan Africa, women in Kenya are disproportionately affected by HIV. In 2016, 34 000 adult women became newly infected with HIV, compared with 22 000 adult men, and adult women accounted for 910 000 of the 1.6 million people living with HIV in the country.
Women also face challenges with sexual and reproductive health issues, such as limited access to family planning, as well as stigma and discrimination when they seek services.
To identify solutions to such challenges facing women in Kenya, the nongovernmental organization Women Fighting AIDS in Kenya (WOFAK) recently held a two-day workshop on 25 and 26 April in Nairobi, Kenya, on advancing the sexual and reproductive health and rights of women living with HIV. More than 30 women living with HIV from across the country met with representatives of the government, civil society and United Nations agencies to take stock and agree a pathway to implement the World Health Organization’s (WHO) Consolidated guideline on sexual and reproductive health and rights of women living with HIV.
“A woman-centered approach must guide a more responsive delivery of services for women living with HIV,” said Dorothy Onyango, co-founder of WOFAK, at the start of the meeting.
To guide effective implementation of the guideline at the country level, the Salamander Trust, with support from WHO, developed a checklist to support women living with HIV to organize and coordinate their own advocacy and ensure their meaningful engagement. The checklist was first used in Kenya and will be rolled out to other countries.
During the meeting, Rukia Ahmed, founder and chairperson of a support network for Kenyan Muslim women living with HIV in north-eastern Kenya, said, “Most women only find out about their HIV status when they are pregnant or very ill. Confidentiality is an issue. When their status is disclosed, some are not accepted by their family afterwards, leading to isolation.”
Ms Ahmed is now going to advocate for discrimination-free health-care settings. “I’m going to visit district hospitals and raise awareness among health-care workers and support groups on the right to stigma-free health care. Change is possible,” she said.
“What stood out for me was the message that as women living with HIV we need to accept ourselves and love ourselves first and as a result we will be able to fight for our rights,” said Joyce Ouma, from Sauti Skika, a network of young people living with HIV.
It is a message Ms Ouma hopes to bring to her peers. “Initially, I did my advocacy out of obligation. Now I want to do it because I have the drive and I know it is important for me first,” she said.
At the conclusion of the meeting, Jantine Jacobi, the UNAIDS Country Director for Kenya, said, “We need to listen to the lived experiences of women living HIV to ensure that services meet their needs.”
Related
 Zambia - an HIV response at a crossroads
Zambia - an HIV response at a crossroads

24 February 2025
 Status of HIV Programmes in Botswana
Status of HIV Programmes in Botswana

20 February 2025




